Abstract
End-stage renal disease is associated with mineral and bone disorders. Guidelines recommending therapies should be based on serial assessments of biomarkers, and thus on variations (Δ), rather than scattered values. We analyzed the correlations between ΔPTH and Δbone biomarkers such as bone-specific alkaline phosphatase (b-ALP), Beta-CrossLaps (CTX), osteocalcin, intact serum procollagen type-1 N-propeptide (P1NP), and tartrate-resistant acid phosphatase 5B (TRAP-5B) at different time-points. In this prospective observational analysis, variations of biomarkers were followed after 6-week (n = 129), 6-month (n = 108) and one-year (n = 93) period. Associations between variations were studied by univariate linear regression. Patients followed for one-year period were classified (increaser or decliner) according to variations reaching the critical difference. Over the 6-week period, only ΔCTX was correlated with ΔPTH (r = 0.38, p < 0.0001). Over the one-year period, correlations between ΔPTH and Δbone biomarkers became significant (r from 0.23 to 0.47, p < 0.01), except with ΔTRAP-5b. Correlations between Δbone biomarkers were all significant after one-year period (r from 0.31 to 0.68, p < 0.01), except between Δb-ALP and ΔTRAP-5b. In the head-to-head classifications (decliners/increasers), the percentage of concordant patients was significantly higher over the one-year than the 6-week period. A concordance between ΔPTH and Δbone biomarkers is observed in dialysis patients, but only after a long follow-up.
Similar content being viewed by others
Introduction
Chronic Kidney Disease (CKD) is associated with mineral and bone disorders (MBD). If bone health includes important concepts such as bone mineralization and bone volume, abnormalities in bone turnover remain key and specific to the dialysis population1. The gold standard for bone turnover diagnosis is bone biopsy2. However, such an invasive technique is difficult to apply in daily practice in every patient. Also, it is cumbersome to repeat such biopsies for bone turnover monitoring3. Therefore, nephrologists rely on bone biomarkers to monitor CKD-MBD1. The recent 2017 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines recommend to measure serum parathyroid hormone (PTH) and bone-specific alkaline phosphatase (b-ALP)4,5. However, the interpretation of these two parameters is not easy, notably because of lack of standardization in the dosages6,7,8. In cross-sectional studies, a good correlation is found between the two biomarkers3,9,10,11. However, their performance to predict bone turnover assessed by bone biopsies in transversal studies remains actually disappointing3,12,13,14. For this reason, the revised 2017 KDIGO guidelines suggest that potential CKD-MBD therapies should be based on serial assessments of biomarkers, and thus on trends or variations (Δ), more than on one-single transversal result. In a previous work, we suggested that the correlations between variations of PTH (ΔPTH) and b-ALP (Δb-ALP) were poor11. This study was however retrospective and sample size was limited. In the current work, we prospectively followed variations of PTH and other bone biomarkers on a 6-week, 6-month and one-year period.
Materials and Methods
Serum PTH and bone biomarker concentrations were measured in hemodialysis patients from three independent hospitals in Liège (Belgium) and surrounding areas (Centre Hospitalier Universitaire du Sart Tilman, Centre Hospitalier Regional de La Citadelle, Centre Hospitalier du Bois de l’Abbaye de Seraing) in 2013. All procedures performed in the current study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol was approved by the Ethics Committee of our institution “Comité d’éthique hospitalo-facultaire universitaire de Liège” (Belgian number study: B707201215885). Informed signed consent was obtained from all participants.
Samples were drawn in participating patients at baseline, then after 6 weeks, 6 months, and one year. Blood samples were collected before the first dialysis session of the week. Samples were immediately centrifuged and kept frozen at −80 °C until determination. Third-generation PTH (DiaSorin-Liaison, Stillwater, MN), intact serum procollagen type 1 N propeptide (P1NP), tartrate-resistant acid phosphatase 5B (TRAP-5B), osteocalcin, and Beta-CrossLaps (CTX)(IDS-iSYS, Boldon, UK) were measured in the same batch and in the same laboratory (department of Clinical Chemistry, University of Liège) accredited for the ISO 15189 Guideline. Inter-assay coefficients of variation were below 10% for all measurements15. Serum calcium, phosphorus, C-reactive protein and albumin were also measured at baseline and after one-year period (Roche Cobas, Mannheim, Germany).
Data are expressed as mean ± standard deviation (SD) when distribution was normal and as median with interquartile range [IQR] when not. Normality was assessed by the Shapiro-Wilk test. In the transversal analysis, Pearson’s coefficients of correlation were calculated between PTH and bone biomarkers at baseline and after one-year. Then, three different analyses were done to study the variations of PTH and bone biomarkers over time. First, coefficients of correlation were calculated focusing on the variations of PTH (ΔPTH, in %) and bone biomarkers (Δbone biomarkers, in %). Correlations between ΔPTH and Δbone biomarkers over a 6-week, 6-month and one-year period were thus calculated. Second, the concept of critical difference (CD) or least significant change was introduced in the analysis. In the field of Clinical Chemistry, CD represents the threshold from which a relative change between two consecutive measurements in the same patient is considered as significant. CD was previously determined for PTH, b-ALP, P1NP and TRAP-5b in the dialysis context15: 43%, 23%, 32% and 24%, respectively. As an example, a relative difference between two PTH consecutive results in the same patient can be considered as clinically relevant if it reached 43%. Patients were then classified according to these significant variations (stable, increaser or decliner). Classifications were compared by exact χ². Third, the slopes of different biomarkers were compared over one-year period (using the 4 available concentrations). Slopes were built and compared by simple linear regression and Pearson correlation. A p value of 0.008 was considered as significant after Bonferroni correction.
Results
Characteristics of the population
One hundred thirty-one patients signed the informed consent. Two patients were excluded from the analysis because of extreme PTH variations (from 36 to 1140 and from 1020 to 67 pg/mL). Median age was 73.3 [18.1] year-old and 55.8% were men. During the follow-up, 36 patients dropped-out the analysis because of death (n = 18), loss of follow-up (n = 8), renal transplantation (n = 8) or hospitalization (n = 2). The total sample at baseline, after 6-week, 6-month and one-year was 129, 123, 108 and 93, respectively. Clinical and biological characteristics at baseline and over one-year period are summarized in Table 1.
Pearson correlations
In the transversal analysis, a significant positive correlation was found between PTH and different bone biomarkers (except no correlation with TRAP-5B), both at baseline (r ranging from 0.42 to 0.72, p < 0.0001) and after one-year follow-up (r ranging from 0.51 to 0.72, p < 0.0001) (Table 2). Significant positive correlations were also found between the different bone biomarkers at baseline (r ranging from 0.22 to 0.81, p < 0.01) and after one-year follow-up (r ranging from 0.22 to 0.82, p < 0.01).
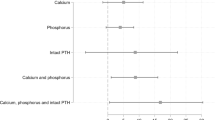
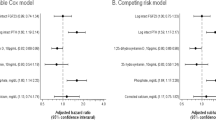
By contrast, when the variations of concentrations are considered (ΔPTH and Δbone biomarkers), associations were much less solid than in the transversal analyses. Over the 6-week period (Table 3), only CTX was correlated with ΔPTH (r = 0.38, p < 0.0001). Also, several correlations between Δbone biomarkers were not significant. However, over the 6-month period (Table 3) and still more for the one-year period (Table 3), correlations between ΔPTH and Δbone biomarkers became significant (r ranging from 0.23 to 0.47, p < 0.01 after one year), except for the absence of correlation between ΔPTH and ΔTRAP-5b. Also, correlations between Δbone biomarkers were all significant (and stronger than between ΔPTH and Δbone biomarkers) after one-year period (r ranging from 0.31 to 0.68, p < 0.01 after one year), except that no correlation existed between Δb-ALP and ΔTRAP-5b.
Critical difference
In this analysis, only the patients who fulfilled the entire one-year period (n = 93) were included. According to the respective CD of markers, the patients were classified as “stable”, “increaser” or “decliner”, at 6-week and one-year. As expected, the percentage of stable patients was higher after 6-week than one-year for all biomarkers (exact χ², p < 0.05), except for TRAP-5b. Head-to-head classifications (stable/decliners/increasers) of different biomarkers are given over the 6-week and one-year period in Table 4. Globally, biomarkers similarly classified the patients in 38 to 72% of patients. Severe discordances (meaning that one biomarker significantly increased whereas the other actually significantly decreased) were found in 1 to 13% of patients. Results of head-to-head comparisons including TRAP-5b were systematically less good than with other bone biomarkers. Concordances in classifications were slightly better between b-ALP and CTX than between PTH and b-ALP or PTH and intact P1NP. Concordances over a six-week period are better than over one-year period, but this analysis must be adjusted by the much higher percentage of stable patients in the 6-week period. Excluding stable patients and focusing on increasers and decliners, the percentage of concordant patients (i.e. the percentage of patients classified as decliners or increasers) was significantly higher over the one-year period in the head-to-head comparisons of biomarkers.
Slopes
Mean slopes were +0.77 ± 16.4 pg/mL/month, +1.13 ± 2.8 µg/L/month, +7.91 ± 158 ng/L/month, +5.93 ± 16.4 ng/mL/month, +4.58 ± 17.2 ng/mL/month, −0.04 ± 0.25 U/L/month/month for PTH, b-ALP, CTX, osteocalcin, P1NP and TRAP-5B, respectively. PTH slope was significantly correlated to CTX (r = 0.5, p < 0.0001), b-ALP (r = 0.41, p < 0.0001), and P1NP (r = 0.29, p = 0.004) slopes whereas no correlation was found between PTH slope and osteocalcin or TRAP-5b slopes. Apart from PTH, several pairs of biomarkers’ slopes displayed significant correlations. P1NP, b-ALP, CTX and osteocalcin slopes were significantly correlated, with a positive Pearson’s coefficient in every combination. TRAP-5B slope was only correlated to CTX. Pairs combinations are displayed in Table 5 and Fig. 1.
Correlation (Pearson) plot between pairs of biomarkers’ slopes calculated on 4 points. The Pearson’s coefficient is proportional to the area of each circle and the intensity of the color. The blue color represents a positive coefficient. Beta-CrossLaps, CTX, intact serum procollagen type 1 N propeptide P1NP, osteocalcin, OSC, PTH, parathormone, tartrate-resistant acid phosphatase 5B, TRAP.
Discussion
Variations of biomarkers, more than one-point result, are recommended by the KDIGO to assess the bone turnover of hemodialysis patients4. Indeed, cross-sectional studies showed that the performance of PTH, bone biomarkers or even combinations of both is poor to predict the turnover determined by bone biopsy3,12,13,14. Changes in biomarkers over time are associated with mortality in dialysis patients16,17 and could also be better predictive of bone turnover observed by bone biopsy3. In the current analysis, we studied the evolution and, more specifically, the concordance between variations of biomarkers over time. If we confirmed that baseline or one-year results of PTH and bone biomarkers are highly correlated in cross-sectional analyses3,9,10,11, the correlations are much less relevant if the variations or changes of biomarkers are considered, suggesting that PTH and bone biomarkers give different information8. In this analysis, the variable “time” seems particularly important. Over a short period of time (6-week), no correlation can be found between PTH and bone biomarkers variations (except for CTX). The correlations between variations of PTH and bone biomarkers became however significant (except for TRAP-5b) after one year of follow-up. This point is confirmed both by considering two points comparison (baseline – 6 weeks and baseline – one year) or comparison of slopes built with four points (baseline, 6 weeks, 6 months and one year). Similarly, the correlations between bone biomarkers are stronger over one-year than 6-week period, suggesting that the variations of bone biomarkers between them and still more variations of bone biomarkers and PTH must be interpreted on a relatively long period of time.
The classification of patients as stable, increasers or decliners is based on the critical difference of biomarkers, this variable having been previously determined for PTH, b-ALP, P1NP and TRAP-5b15. At first glance, it could be concluded that the concordance of classifications is better over a 6-week period than over one-year of follow-up. However, it must be reminded that most patients remain stable over the 6-week period. If stable patients are excluded from the analysis, it is clear that the concordance of both decliners and increasers are higher over the one-year period.
Globally, the results support a better concordance between variations of “true” bone biomarkers (P1NP, CTX, and b-ALP,) than between PTH and bone biomarkers, which is not fully unexpected as PTH is actually an indirect bone biomarker, since it is mainly influenced by calcium concentration8,18. Moreover, PTH concentrations rapidly follow any modification of calcium concentration, although other bone biomarkers take more time because their concentration will depend on the bone-remodelling process, which is about six months in healthy individuals. In the same view, the half-life of bone biomarkers in serum is expressed in days, whereas the half-life of PTH is only a few minutes8,19. Differences between the kinetics of the “minute to minute” calcium regulation by PTH, which has a short half-life, and the time needed for bone to be altered or improved, which is sometimes over 1 year have been illustrated in peritoneal dialysis patients moving to low calcium dialysate20 and in hemodialyzed patients treated by cinacalcet14,21.
Globally, the concordances are better between bone biomarkers, with the exception of TRAP-5b. Variations of P1NP and b-ALP over time seem particularly concordant. Moreover, concentrations of these two biomarkers (at least the intact form of P1NP) are not influenced by CKD status8,22, contrary to CTX3,8,23,24. The choice of one biomarker could be dependent on the availability of the biomarker in the laboratory and/or some specific characteristics of the patients (for instance, it has been suggested that severe hepatic dysfunction could interfere with b-ALP measurement)8,25. Also from an analytical point of view, intact P1NP seems more robust than b-ALP6 and is considered as the formation marker of choice by the International Osteoporosis Foundation26. The lower concordance observed with TRAP-5b could be explained by the fact that this biomarker is the only bone biomarker of osteoclastic activity (or, even more, a marker of osteoclasts number), the other being markers of bone formation8,27,28. In this context, it must be underlined that TRAP-5b classified many patients as decliners whereas decliners are minority with P1NP and b-ALP. TRAP-5b has also be proposed as an interesting biomarker for bone mass monitoring29.
There are limitations to our study. First, the study is purely observational and was neither designed nor powered to determine why and for which patients’ discrepant results are observed, notably according to their therapies. Analyses were repeated after excluding 9 patients who changed their therapy (regarding cinacalcet or active vitamin D therapy) during the follow-up and the same conclusions remained (data not shown). The number of patients with changing therapy was definitively too low to be analyzed separately. A study with a similar design but focusing on patients starting cinacalcet or active vitamin D would be of interest. Second, in the absence of bone biopsy data, only a description of concordances and discrepancies in bone biomarkers evolution can be done but the potential superiority of one biomarker over another one to assess turnover cannot be proved. Third, because relative differences were used, the results could be too largely influenced by low PTH concentrations at baseline. Analyses were thus repeated excluding patients with low turnover at baseline (defined as PTH lower than two-times the upper normal value) (n = 12) and the results remained the same (see supplements), suggesting that the level of PTH at baseline did not modify the conclusions. Lastly, our follow-up remains limited (one-year) and our population contains only prevalent dialysis patients. Further analyses in incident patients and with a still longer follow-up could be of interest.
Bone biomarkers have been suggested as of interest to detect bone turnover abnormalities in dialysis patients. A dynamic view and a focus on bone biomarkers modifications is promoted3,8. However, as illustrated in the present study, there are frequently discrepancies between the evolution of these different markers. One can recommend that results must be analyzed on a relatively long period of time because these bone biomarkers have certainly not the same reactivity to reflect bone activity, and this is especially true comparing PTH with bone biomarker. Moreover, a better concordance is observed between “true” bone formation biomarkers than between bone biomarkers and PTH (or marker of osteoclastic activity).
References
Moorthi, R. N. & Moe, S. M. Recent advances in the noninvasive diagnosis of renal osteodystrophy. Kidney Int 84, 886–894 (2013).
Torres, P. U., Bover, J., Mazzaferro, S., de Vernejoul, M. C. & Cohen-Solal, M. When, how, and why a bone biopsy should be performed in patients with chronic kidney disease. Semin Nephrol 34, 612–625 (2014).
Vervloet, M. G. & Brandenburg, V. M. Circulating markers of bone turnover. J Nephrol. in press (2017).
KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl S1–130 (2009).
Ketteler, M. et al. Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney Int 92, 26–36 (2017).
Cavalier, E. et al. Inter-method variability in bone alkaline phosphatase measurement: clinical impact on the management of dialysis patients. Clin Biochem 47, 1227–1230 (2014).
Souberbielle, J. C. et al. Inter-method variability in PTH measurement: implication for the care of CKD patients. Kidney Int 70, 345–350 (2006).
Delanaye, P., Souberbielle, J.-C., Lafage-Proust, M.-H., Jean, G. & Cavalier, E. Can we use circulating biomarkers to monitor bone turnover in CKD haemodialysis patients? Hypotheses and facts. Nephrol Dial Transplant 29, 997–1004 (2014).
Cavalier, E., Delanaye, P., Collette, J., Krzesinski, J.-M. & Chapelle, J.-P. Evaluation of different bone markers in hemodialyzed patients. Clin Chim Acta 371, 107–111 (2006).
Reichel, H., Esser, A., Roth, H. J. & Schmidt-Gayk, H. Influence of PTH assay methodology on differential diagnosis of renal bone disease. Nephrol Dial.Transplant 18, 759–768 (2003).
Delanaye, P. et al. Parathormone and bone-specific alkaline phosphatase for the follow-up of bone turnover in hemodialysis patients: is it so simple? Clin Chim.Acta 417, 35–38 (2013).
Sprague, S. M. et al. Diagnostic Accuracy of Bone Turnover Markers and Bone Histology in Patients With CKD Treated by Dialysis. Am J Kidney Dis 67, 559–566 (2016).
Torres, A. et al. Bone disease in predialysis, hemodialysis, and CAPD patients: evidence of a better bone response to PTH. Kidney Int 47, 1434–1442 (1995).
Behets, G. J. et al. Bone histomorphometry before and after long-term treatment with cinacalcet in dialysis patients with secondary hyperparathyroidism. Kidney Int 87, 846–56 (2015).
Cavalier, E., Delanaye, P. & Moranne, O. Variability of new bone mineral metabolism markers in patients treated with maintenance hemodialysis: implications for clinical decision making. Am J Kidney Dis 61, 847–848 (2013).
Soohoo, M. et al. Changes in Markers of Mineral and Bone Disorders and Mortality in Incident Hemodialysis Patients. Am J Nephrol 43, 85–96 (2016).
Streja, E. et al. Mortality of combined serum phosphorus and parathyroid hormone concentrations and their changes over time in hemodialysis patients. Bone 61, 201–207 (2014).
Mundy, G. R. & Guise, T. A. Hormonal control of calcium homeostasis. Clin Chem 45, 1347–1352 (1999).
Garrett, G., Sardiwal, S., Lamb, E. J. & Goldsmith, D. J. PTH–a particularly tricky hormone: why measure it at all in kidney patients? Clin J Am Soc Nephrol 8, 299–312 (2013).
Sanchez, C. et al. Low vs standard calcium dialysate in peritoneal dialysis: differences in treatment, biochemistry and bone histomorphometry. A randomized multicentre study. Nephrol Dial Transplant 19, 1587–1593 (2004).
Jean, G., Chazot, C. & Charra, B. 12 months cinacalcet therapy in hemodialysis patients with secondary hyperparathyroidism: effect on bone markers. Clin Nephrol 68, 63–64 (2007).
Cavalier, E., Lukas, P., Carlisi, A., Gadisseur, R. & Delanaye, P. Aminoterminal propeptide of type I procollagen (PINP) in chronic kidney disease patients: the assay matters. Clin Chim Acta 425, 117–118 (2013).
Reichel, H., Roth, H. J. & Schmidt-Gayk, H. Evaluation of serum beta-carboxy-terminal cross-linking telopeptide of type I collagen as marker of bone resorption in chronic hemodialysis patients. Nephron Clin Pract 98, c112–c118 (2004).
Okabe, R. et al. Clinical evaluation of the Elecsys beta-CrossLaps serum assay, a new assay for degradation products of type I collagen C-tlopeptides. Clin Chem 47, 1410–1414 (2001).
Jean, G. et al. Total and bone-specific alkaline phosphatases in haemodialysis patients with chronic liver disease. Clin Biochem 45, 436–439 (2012).
Vasikaran, S. et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 22, 391–420 (2011).
Shidara, K. et al. Serum levels of TRAP5b, a new bone resorption marker unaffected by renal dysfunction, as a useful marker of cortical bone loss in hemodialysis patients. Calcif Tissue Int 82, 278–287 (2008).
Yamada, S. et al. Utility of serum tartrate-resistant acid phosphatase (TRACP5b) as a bone resorption marker in patients with chronic kidney disease: independence from renal dysfunction. Clin Endocrinol 69, 189–196 (2008).
Malluche, H. H., Davenport, D. L., Cantor, T. & Monier-Faugere, M. C. Bone Mineral Density and Serum Biochemical Predictors of Bone Loss in Patients with CKD on Dialysis. Clin J Am Soc Nephrol 9, 1254–1262 (2014).
Acknowledgements
Authors thank the data nurses who were involved in the study, Jean Barahira and Arnaud Borsu for CHU, Sart Tilman and Chadya Bouidane for CHR, La Citadelle.
Author information
Authors and Affiliations
Contributions
Pierre Delanaye wrote the manuscript, had the research idea and designed the study, Xavier Warling, Martial Moonen, Nicole Smelten and François Jouret participated in the data acquisition in different centers. They also participated to the data analysis and interpretation. Jean-Marie Krzesinski reviewed the manuscript as the head of department of Nephrology, Hans Pottel and Nicolas Maillard performed the statistical analyses, Etienne Cavalier designed the study, participated to the interpretation of data and reviewed the manuscript as the head of the department of Clinical Chemistry. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the.
Corresponding author
Ethics declarations
Competing Interests
Pierre Delanaye and Etienne Cavalier are consultants for IDS company. Etienne Cavalier is consultant for Diaosrin. These companies have not been involved in the current research. Other authors have no conflict of interest to declare.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Delanaye, P., Warling, X., Moonen, M. et al. Variations of parathyroid hormone and bone biomarkers are concordant only after a long term follow-up in hemodialyzed patients. Sci Rep 7, 12623 (2017). https://doi.org/10.1038/s41598-017-12808-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12808-3
This article is cited by
-
Bone turnover correlates with bone quantity but not bone microarchitecture in chronic hemodialysis
Journal of Bone and Mineral Metabolism (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.