Abstract
The retina requires adequate oxygenation to maintain cellular metabolism and visual function. Inner retinal oxygen metabolism is directly related to retinal vascular oxygen tension (PO2) and inner retinal oxygen extraction fraction (OEF), whereas outer retinal oxygen consumption (QO2) relies on oxygen availability by the choroid and is contingent upon retinal tissue oxygen tension (tPO2) gradients across the retinal depth. Thus far, these oxygenation and metabolic parameters have been measured independently by different techniques in separate animals, precluding a comprehensive and correlative assessment of retinal oxygenation and metabolism dynamics. The purpose of the current study is to report an innovative optical system for dual oxyphor phosphorescence lifetime imaging to near-simultaneously measure retinal vascular PO2 and tPO2 in rats. The use of a new oxyphor with different spectral characteristics allowed differentiation of phosphorescence signals from the retinal vasculature and tissue. Concurrent measurements of retinal arterial and venous PO 2 , tPO2 through the retinal depth, inner retinal OEF, and outer retinal QO 2 were demonstrated, permitting a correlative assessment of retinal oxygenation and metabolism. Future application of this method can be used to investigate the relations among retinal oxygen content, extraction and metabolism under pathologic conditions and thus advance knowledge of retinal hypoxia pathophysiology.
Similar content being viewed by others
Introduction
The retinal tissue requires an adequate supply of oxygen for cellular metabolism and function. Retinal ischemia due to reduced blood flow has been implicated in the development of vision threatening pathologies such as neovascularization and macular edema1, 2. Furthermore, inadequate oxygen availability can lead to hypoxic injury and eventual cell death. Therefore, assessment of retinal oxygenation is essential to improve knowledge of disease pathophysiology and advance treatments that target alleviation of hypoxia-induced pathologies.
Several techniques have become available for quantitative assessment of oxygen content within the retinal vasculature or tissue. Specifically, retinal oximetry for measurement of hemoglobin oxygen saturation (SO2) has been performed by spectrophotometry3,4,5, photoacoustic ophthalmoscopy6, and visible optical coherence tomography7, 8. Additionally, retinal vascular oxygen tension (PO2) has been reported using phosphorescence lifetime imaging9,10,11. Direct depth-resolved measurements of retinal tissue oxygen tension (tPO2) have been provided by the oxygen-sensitive microelectrode technique at single point locations12,13,14 and by phosphorescence lifetime imaging at multiple contiguous locations15. Furthermore, information about the metabolic activity of the retinal tissue has become available by calculation of inner retinal oxygen extraction fraction (OEF) based on retinal vascular oxygen content5, 16 and by estimation of outer retinal oxygen consumption (QO 2 ) from retinal tPO2 depth profiles14, 17, 18.
To date, these parameters of retinal oxygenation and metabolism have been measured independently in separate animals. Thus, current techniques precluded the assessment of relations among these parameters in the same animal under physiological or pathological conditions which is essential to improve understanding of retinal ischemia pathophysiology. Retinal hypoxia is implicated in the development of vision-threatening retinal pathologies, yet there are currently no direct methods to measure tPO2 in humans. Alterations in inner retinal OEF due to hypoxia16 and retinal disease19 have been demonstrated, but the relationship between tPO2 and OEF is not known. Furthermore, although presumed, a correspondence between inner retinal tPO2 and venous PO2 has not been established. Measurements of these parameters in separate animals cannot accurately determine the association between them due to physiological variations among animals. Therefore, concurrent measurements of retinal vascular PO2 and tPO2 in the same animals are necessary to infer reduced tPO2 based on altered OEF or venous PO2 under retinal ischemic conditions. These findings may be translated to humans to assess retinal hypoxia and identify OEF thresholds necessary to sustain tPO2. The purpose of the current study is to report an innovative optical system for dual oxyphor phosphorescence lifetime imaging to near-simultaneously measure retinal vascular PO2 and tPO2 in rats, derive OEF and QO 2 , and determine associations among these parameters.
Methods
Animals
All experimental procedures were in compliance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research and approved by the Animal Care Committee of the University of Illinois at Chicago. The study was performed in 10 Long Evans pigmented rats. Rats were anesthetized with intraperitoneal injections of ketamine (100 mg/kg) and xylazine (5 mg/kg) and additional injections were given as required to maintain anesthesia. One day prior to imaging, oxyphor G2 (Oxygen Enterprises, Philadelphia, PA) was constituted at 1.5 μM and administered as a 5 μL intravitreal bolus injection for retinal tPO2 imaging. Immediately prior to imaging, oxyphor R0 (Frontier Scientific, Logan, Utah) was administered intravenously (20 mg/kg) for retinal vascular PO2 imaging. Before imaging, pupils were dilated with 2.5% phenylephrine and 1% tropicamide, and a glass cover slip with 1% hydroxypropyl methylcellulose was placed on the cornea to minimize corneal refractive power and prevent dehydration. Rats were placed on an animal holder with a closed-loop water heater to maintain body temperature at 37 °C and were spontaneously breathing during imaging. One eye of each rat was imaged in temporal or nasal regions within three-disk diameters (600 microns) from the edge of the optic nerve head.
Phosphorescence Lifetime Imaging
Our previously established optical imaging system9, 15 for either retinal vascular PO2 or tPO2 measurement was modified for near-simultaneous measurement of both parameters by dual oxyphor phosphorescence lifetime imaging (Fig. 1). The use of two oxyphors (R0 and G2) with different absorption and emission spectra allowed differentiation of phosphorescence signal from within the retinal vasculature and tissue. Two diode lasers at 532 nm (Lasermate Group, Inc. MGM-10) and 635 nm (Lasermate Group, Inc. LTC6358AH) were incorporated into the imaging system for excitation of R0 and G2 oxyphors, respectively. The power of each laser was adjusted to 120 µW at the cornea. Both lasers were projected at an oblique angle to the imaging axis and focused to a co-localized 1 mm vertical line on the retina. Since the incident lasers were not coaxial with the imaging path, phosphorescence emission through the retinal depth appeared laterally displaced on the optical section phosphorescence image. A high pass (>650 nm; Thorlabs, Inc.) or bandpass filter (810 ± 25 nm; Midwest Optical Systems, Inc.) was placed interchangeably in the imaging path to selectively image the phosphorescence emission of R0 (within the retinal vasculature) or G2 (within the retinal tissue), respectively. Both lasers were modulated by an optical chopper at 1.6 kHz. Optical section phosphorescence images were acquired by an intensified charge-coupled device (ICCD) camera, while the gain of the intensifier was modulated by the camera software at the same frequency. The optical chopper frequency, ICCD gain modulation frequency and temporal delay increments between the two were selected to produce phase shifts between 0° and 180°. Phosphorescence lifetime was measured from 10 phase-delayed optical section phosphorescence images, as previously described9, 15.
Image acquisition consisted of imaging G2 and R0 phosphorescence sequentially. First, three repeated phase-delayed optical section phosphorescence images from the retinal tissue were acquired. Then, the excitation laser and emission filter were changed manually (within two seconds) and three repeated phase-delayed optical section phosphorescence images from the retinal vasculature were acquired at exactly the same retinal location. The total time for image acquisition was less than 60 seconds.
Vascular PO2 and Inner Retinal OEF
Vascular PO2 in major retinal arteries and veins was measured from the phosphorescence lifetime using the Stern-Volmer equation and the R0 oxyphor’s quenching constant and lifetime in a zero-oxygen environment, as previously described9, 20. PO2 in each blood vessel was calculated by averaging three repeated measurements. A mean arterial and venous PO2 (PO2A and PO2V) was determined for each rat by averaging measurements in each vessel type. Inner retinal OEF was calculated from PO2A and PO2V and using the oxyhemoglobin dissociation curve in rat21, as previously described16. Inner retinal OEF is the fraction of oxygen supplied by the retinal circulation that is extracted by the inner retinal tissue for metabolism, or equivalently, the ratio of inner retinal oxygen metabolism to inner retinal oxygen delivery.
Retinal tPO2 and Outer Retinal QO2
Retinal tissue optical section phosphorescence images were first processed to minimize retinal curvature, then smoothed in vertical (y-axis) and axial (z-axis) dimensions using a 2D anisotropic averaging filter (6 × 4 pixels), corresponding to 18 μm in both axes. A depth-resolved tPO2 image was generated from the phosphorescence lifetime measured at each pixel using the Stern-Volmer equation and the G2 oxyphor’s quenching constant and lifetime in a zero-oxygen environment22, as previously described15. A mean depth-resolved retinal tPO2 image was generated from three repeated images.
Along the vertical dimension of each retinal tPO2 image (superior to inferior), 35 contiguous tPO2 depth profiles were generated by vertically averaging tPO2 over 10 pixels (30 microns) and plotting tPO2 as a function of retinal depth, as previously described15. The outer and inner retina were defined as 50% to 100% and 0% to 50% of the retinal depth, respectively. Maximum outer retinal tPO2, minimum outer retinal tPO2, and mean inner retinal tPO2 were calculated from each tPO2 depth profile. Mean inner retinal tPO2 was plotted along the vertical dimension of the image to demonstrate changes in this parameter with respect to retinal arteries and veins. Furthermore, mean values for each parameter were calculated from all profiles along the tPO2 image.
From each retinal tPO2 depth profile, outer retinal QO2 was calculated by fitting a three-layer, one-dimensional, steady-state oxygen diffusion model using a non-linear least squares technique, as previously described12, 14, 17, 23. In this model, oxygen diffuses in one dimension from the choroidal circulation across the outer retinal depth, which is divided into three layers14, based on their oxygen consumption properties. QO2 has been shown to be negligible in layers 1 and 323, which correspond to the photoreceptor outer segments and outer nuclear layer, respectively. In contrast, oxygen is consumed in layer 2 by mitochondria of the photoreceptor inner segments, yielding a quadratic relationship between tPO2 and retinal depth. A mean outer retinal QO2 was calculated by averaging measurements obtained from all tPO2 depth profiles along the vertical dimension of the tPO2 image.
Data availability
The data generated are available from the corresponding author on reasonable request.
Results
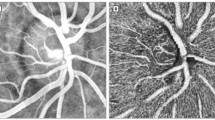
A representative example of a retinal vascular PO2 and tPO2 image obtained at the same location overlaid on the retinal reflectance image is shown in Fig. 2a. The vascular PO2 image displays measurements in two arteries and one vein, demonstrating higher PO2A than PO2V, as expected. The tPO2 image shows higher tPO2 near the chorioretinal interface compared to inner retina. Mean inner retinal tPO2 plotted along the vertical dimension (superior to inferior) is shown in Fig. 2b, displaying higher tPO2 near arteries than the vein.
(a) Combined depth-resolved retinal vascular oxygen tension (PO2) and tissue oxygen tension (tPO2) images overlaid on the retinal reflectance image in a rat. The vascular PO2 image displays measurements in two arteries and one vein (labeled), outlined by black circles. Color bar indicates PO2 in mmHg. (b) Inner retinal tPO2 plotted along the vertical dimension (superior to inferior) along the tPO2 image. Locations of the two arteries and one vein are marked.
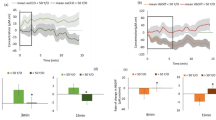
Compiled retinal vascular PO2 and tPO2 measurements in all rats are presented in Fig. 3. PO2A and PO2V were 41 ± 5 mmHg and 25 ± 4 mmHg, respectively (P < 0.001; N = 10). Inner retinal tPO2, minimum outer retinal PO2, maximum outer retinal PO2 were 23 ± 7 mm Hg, 22 ± 5 mm Hg and 33 ± 8 mm Hg, respectively. There was no significant difference between PO2V and mean inner retinal tPO2 (P = 0.4). Inner retinal OEF was 0.58 ± 0.11 and outer retinal QO2 was 0.57 ± 0.27 mLO2/100 g*min. There was no significant correlation between inner retinal OEF and mean inner retinal tPO2 (R2 = 0.05; P = 0.53; N = 10). As demonstrated in Fig. 4, there was a significant correlation between outer retinal QO2 and maximum outer retina tPO2 (R2 = 0.77; P < 0.001; N = 10).
Discussion
A novel optical imaging method for near-simultaneous imaging of retinal vascular PO2 and tPO2 was demonstrated by phosphorescence lifetime imaging of dual oxyphors delivered intravenously and intravitreally. For the first time, concurrent assessment of oxygen content across the retinal depth and oxygen metabolism metrics of the inner and outer retina was demonstrated. Future application of this method can provide knowledge of relations among these parameters under experimental pathologic conditions and thus yield a comprehensive understanding of retinal oxygenation and metabolism dynamics.
Measurements of retinal PO2A and PO2V were in general agreement with those from previous studies24, 25. Depth-resolved retinal tPO2 images displayed maximum tPO2 near the choroid, consistent with normal physiology. Inner retinal tPO2 measurements using the G2 oxyphor were similar to our previously published data with the R2 oxyphor15 and those reported by the oxygen microelectrode technique14. Alterations in inner retinal tPO2 were consistent with the nearby presence of arteries and veins. Inner retinal OEF was 0.58, on average, indicating 58% of the oxygen delivered by the retinal circulation was extracted for metabolism by the inner retinal tissue. The mean inner retinal OEF was higher as compared to our previous study16 and maximum outer retinal tPO2 in the current study was slightly lower than previous reports14, 15. Both of these results are consistent with the presence of reduced systemic oxygenation26, which likely resulted from the effect of anesthesia while the rats were under spontaneous breathing conditions27. Furthermore, the variability of tPO2 adjacent to the chorioretinal interface along the tPO2 image may, at least in part, be attributed to presumed anesthesia-induced systemic hypotension. This may have resulted in reduced choroidal blood flow, thus altering tPO2 gradients within the retinal depth. Overall, the results demonstrate the ability of the optical imaging system to measure retinal vascular PO2, tPO2 and inner retinal OEF.
Measurements of outer retinal QO2 obtained in the current study were similar to our previously reported values17, but lower than those obtained by the oxygen microelectrode technique in light-adapted rats12, 14, 18. This difference is likely due to intraretinal phosphorescence scattering which decreases the depth resolution, minimizes the curvature of tPO2 profiles and calculated values of QO2. Nevertheless, outer retinal QO2 was significantly associated with maximum outer retinal tPO2, in agreement with a previous study14, though a small portion of oxygen utilized by the photoreceptors is supplied by the retinal vasculature14. This result suggests a dependence of the photoreceptor metabolic function on the level of oxygen supplied by the choroidal circulation.
Simultaneous measurements of retinal vascular PO2 and tPO2 coupled with derivation of inner retina OEF and outer retinal QO2 can advance knowledge of retinal oxygen dynamics. For example, we demonstrated here, for the first time, that there was no significant correlation between inner retinal OEF and mean inner retinal tPO2 under healthy condition. This result suggests that despite physiological variations, tPO2 is well-maintained due to compensatory alterations in OEF and oxygen delivery, and implies the presence of highly effective regulatory mechanisms. Previous studies have shown alterations in OEF under experimental hypoxia in rats16. In future studies, by relating inner retinal tPO2 with OEF under graded hypoxia/ischemia, diabetes or light flicker stimulation, the OEF threshold necessary to sustain tPO2 may be identified. Additionally, data obtained under graded levels of ischemia may be used to establish a relationship between inner retinal tPO2 and PO2V. Furthermore, combined retinal blood flow measurements with the current method can be used to determine the inner retinal oxygen delivery threshold necessary to maintain retinal tPO2 with direct relevance to retinal ischemic diseases. These thresholds can only be accurately determined with concurrent retinal vascular PO2 and tPO2 measurements in the same animal.
One potential limitation of this method is the scattering of phosphorescence light within the retina and vitreous which can degrade image quality. However, compared to the R2 oxyphor, less scattering is expected from the G2 oxyphor due to its longer phosphorescence emission wavelength. The quenching constants used to calculate PO2 were obtained from literature and may be different within the retinal tissue environment. Phototoxicity may affect data derived from images acquired repeatedly at the same location with R0 oxyphor28, but any effect of phototoxicity on measurements derived using the G2 oxyphor is not known. Although, the laser irradiance was below the threshold for tissue damage, repeatability of measurements obtained at the same location with the use of dual oxyphors will need further evaluation. The feasibility of the method was demonstrated in a limited number of rats and future studies using larger sample sizes are needed to fully establish the utility of the method.
In conclusion, for the first time, near-simultaneous measurement of retinal vascular and tissue oxygen tension by phosphorescence lifetime imaging was demonstrated. Future application of this method under challenged physiologic or pathologic conditions permits correlation of retinal vascular and tissue oxygen content and can potentially elucidate retinal oxygenation dynamics.
References
Campochiaro, P. A. Molecular pathogenesis of retinal and choroidal vascular diseases. Progress in retinal and eye research 49, 67–81, doi:10.1016/j.preteyeres.2015.06.002 (2015).
Kurihara, T., Westenskow, P. D. & Friedlander, M. Hypoxia-inducible factor (HIF)/vascular endothelial growth factor (VEGF) signaling in the retina. Advances in experimental medicine and biology 801, 275–281, doi:10.1007/978-1-4614-3209-8_35 (2014).
Olafsdottir, O. B., Eliasdottir, T. S., Kristjansdottir, J. V., Hardarson, S. H. & Stefansson, E. Retinal Vessel Oxygen Saturation during 100% Oxygen Breathing in Healthy Individuals. PloS one 10, e0128780, doi:10.1371/journal.pone.0128780 (2015).
Hammer, M., Vilser, W., Riemer, T. & Schweitzer, D. Retinal vessel oximetry-calibration, compensation for vessel diameter and fundus pigmentation, and reproducibility. Journal of Biomedical Optics 13, doi:10.1117/1.2976032 (2008).
Felder, A. E., Wanek, J., Blair, N. P. & Shahidi, M. Inner Retinal Oxygen Extraction Fraction in Response to Light Flicker Stimulation in Humans. Invest Ophthalmol Vis Sci 56, 6633–6637, doi:10.1167/iovs.15-17321 (2015).
Song, W. et al. A combined method to quantify the retinal metabolic rate of oxygen using photoacoustic ophthalmoscopy and optical coherence tomography. Sci Rep 4, 6525, doi:10.1038/srep06525 (2014).
Yi, J. et al. Visible light optical coherence tomography measures retinal oxygen metabolic response to systemic oxygenation. Light, science & applications 4, doi:10.1038/lsa.2015.107 (2015).
Soetikno, B. T. et al. Inner retinal oxygen metabolism in the 50/10 oxygen-induced retinopathy model. Scientific reports 5, 16752, doi:10.1038/srep16752 (2015).
Shahidi, M., Shakoor, A., Blair, N. P., Mori, M. & Shonat, R. D. A method for chorioretinal oxygen tension measurement. Curr Eye Res 31, 357–366, doi:10.1080/02713680600599446 (2006).
Blair, N. P., Wanek, J. M., Mori, M. & Shahidi, M. Abnormal retinal vascular oxygen tension response to light flicker in diabetic rats. Invest Ophthalmol Vis Sci 50, 5444–5448, doi:10.1167/iovs.09-3465 (2009).
Wanek, J., Teng, P. Y., Albers, J., Blair, N. P. & Shahidi, M. Inner retinal metabolic rate of oxygen by oxygen tension and blood flow imaging in rat. Biomed Opt Express 2, 2562–2568, doi:10.1364/BOE.2. (2011).
Cringle, S. J., Yu, D. Y., Yu, P. K. & Su, E. N. Intraretinal oxygen consumption in the rat in vivo. Invest Ophthalmol Vis Sci 43, 1922–1927 (2002).
Wangsa-Wirawan, N. D. & Linsenmeier, R. A. Retinal oxygen: fundamental and clinical aspects. Arch Ophthalmol 121, 547–557, doi:10.1001/archopht.121.4.547 (2003).
Lau, J. C. & Linsenmeier, R. A. Oxygen consumption and distribution in the Long-Evans rat retina. Exp Eye Res 102, 50–58, doi:10.1016/j.exer.2012.07.004 (2012).
Shahidi, M., Wanek, J., Blair, N. P., Little, D. M. & Wu, T. Retinal Tissue Oxygen Tension Imaging in Rat. Investigative ophthalmology & visual science 09–4710 (2010).
Teng, P. Y., Wanek, J., Blair, N. P. & Shahidi, M. Inner retinal oxygen extraction fraction in rat. Invest Ophthalmol Vis Sci 54, 647–651, doi:10.1167/iovs.12-11305 (2013).
Wanek, J., Blair, N. P. & Shahidi, M. Outer retinal oxygen consumption of rat by phosphorescence lifetime imaging. Curr Eye Res 37, 132–137, doi:10.3109/02713683.2011.629071 (2012).
Yu, D. Y. & Cringle, S. J. Oxygen distribution and consumption within the retina in vascularised and avascular retinas and in animal models of retinal disease. Progress in retinal and eye research 20, 175–208 (2001).
Felder, A. E. et al. The Effects of Diabetic Retinopathy Stage and Light Flicker on Inner Retinal Oxygen Extraction Fraction. Invest Ophthalmol Vis Sci 57, 5586–5592, doi:10.1167/iovs.16-20048 (2016).
Lo, L. W., Koch, C. J. & Wilson, D. F. Calibration of oxygen-dependent quenching of the phosphorescence of Pd-meso-tetra (4-carboxyphenyl) porphine: a phosphor with general application for measuring oxygen concentration in biological systems. Anal Biochem 236, 153–160, doi:10.1006/abio.1996.0144 (1996).
Cartheuser, C. F. Standard and pH-affected hemoglobin-O2 binding curves of Sprague-Dawley rats under normal and shifted P50 conditions. Comparative biochemistry and physiology. Comparative physiology 106, 775–782 (1993).
Dunphy, I., Vinogradov, S. A. & Wilson, D. F. Oxyphor R2 and G2: phosphors for measuring oxygen by oxygen-dependent quenching of phosphorescence. Anal Biochem 310, 191–198 (2002).
Haugh, L. M., Linsenmeier, R. A. & Goldstick, T. K. Mathematical models of the spatial distribution of retinal oxygen tension and consumption, including changes upon illumination. Ann Biomed Eng 18, 19–36 (1990).
Wanek, J., Teng, P. Y., Blair, N. P. & Shahidi, M. Inner retinal oxygen delivery and metabolism under normoxia and hypoxia in rat. Invest Ophthalmol Vis Sci 54, 5012–5019, doi:10.1167/iovs.13-11887 (2013).
Yu, D. Y., Cringle, S. J., Alder, V. & Su, E. N. Intraretinal oxygen distribution in the rat with graded systemic hyperoxia and hypercapnia. Investigative ophthalmology & visual science 40, 2082–2087 (1999).
Teng, P. Y., Wanek, J., Blair, N. P. & Shahidi, M. Response of Inner Retinal Oxygen Extraction Fraction to Light Flicker Under Normoxia and Hypoxia in Rat. Investigative Ophthalmology & Visual Science 55, 6055–6058, doi:10.1167/iovs.13-13811 (2014).
Shakoor, A., Gupta, M., Blair, N. P. & Shahidi, M. Chorioretinal vascular oxygen tension in spontaneously breathing anesthetized rats. Ophthalmic Res 39, 103–107, doi:10.1159/000099246 (2007).
Stepinac, T. K. et al. Light-induced retinal vascular damage by Pd-porphyrin luminescent oxygen probes. Investigative ophthalmology & visual science 46, 956–966, doi:10.1167/iovs.04-0500 (2005).
Acknowledgements
This study was supported by NIH grants EY017918 and EY001792, Senior Scientific Investigator award (MS) and an unrestricted departmental grant from Research to Prevent Blindness.
Author information
Authors and Affiliations
Contributions
A.E.F.: experimental design, data acquisition, data analysis, data interpretation, writing. J.W.: data analysis, data interpretation, writing. M.R.T.: data acquisition. N.P.B.: data interpretation, writing. M.S.: experimental design, data analysis, data interpretation, writing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Felder, A.E., Wanek, J., Tan, M.R. et al. A Method for Combined Retinal Vascular and Tissue Oxygen Tension Imaging. Sci Rep 7, 10622 (2017). https://doi.org/10.1038/s41598-017-10955-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10955-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.