Abstract
An innovative natriuretic peptide analog named CNAAC (structurally consisting of the C-terminus and ring of ANP and the N-terminus of CNP) that has been shown to exhibit potent vasodilatory, diuretic, and hypotensive effects in our previous study was evaluated for the treatment of left ventricular dysfunction following myocardial infarction. The temporal relaxation effect and metabolic status of CNAAC were determined. A myocardial ischemic model was established. Rats were randomly divided into Sham, MI, MI-ANP, MI-CNP, MI-VNP, and MI-CNAAC groups. Humoral factors were measured; echocardiography and hemodynamics methods were employed to assess the cardiac function at the fourth week after modeling. The results showed that CNAAC had a potent relaxant effect and longer duration of action than ANP, CNP, or VNP. The stability of CNAAC in blood was higher than other three NPs. Four weeks of NP administration ameliorated diastolic and systolic dysfunction, the hypertrophic index, myocardial fibrosis, and infarct size; it also restored the abnormal changes in humoral factors. These results demonstrate that CNAAC has a potent cardioprotective effect against left ventricular dysfunction after myocardial infarction. The results may lay the foundation for the clinical application of this newly designed NP chimera in the treatment and prevention of heart failure.
Similar content being viewed by others
Introduction
Chronic heart failure is a clinical syndrome that is characterized by diastolic and systolic dysfunction and ejection function damage that result in an insufficient cardiac output that cannot fulfill the body’s needs. Chronic heart failure has also been associated with high morbidity and mortality1. The traditional treatment for heart failure is to strengthen cardiac function by administering several drugs, but the result is unsatisfactory. Recently, researchers realized that an adjustment of neurohormone activation is key in the treatment of heart failure. One of the adjustments is to restrain the function of positive regulation factors, such as the use of angiotensin-converting enzyme inhibitors (ACEI), to decrease the effects of angiotensin II and aldosterone, which will then alleviate the cardiac load and improve the coronary blood-supply. Another method is to strengthen the function of negative regulation factors and utilize the vasorelaxant, natriuretic, diuretic, and renin-angiotensin-aldosterone system (RAAS) inhibiting effects of natriuretic peptides to postpone the development of heart failure and myocardial remodeling2.
Natriuretic peptides (NPs) are a group of structurally similar but genetically distinct peptides that exert potent diuretic, natriuretic, vasorelaxant, antifibrotic, and antihypertrophic effects and play crucial roles in cardiovascular homeostasis2, 3. The study of natriuretic peptides began 50 years ago4. Earlier studies identified members of the NP family. After atrial natriuretic peptide (ANP) was found in atrial cells in the early 1980s, brain natriuretic peptide (BNP) and C-type natriuretic peptide (CNP) were identified in porcine brain between 1988 and 19905, 6. Dendroaspis natriuretic peptide (DNP) was then identified in the venom of the green mamba in 19927. Other peptides, including urodilatin and ventricle natriuretic peptide, were identified from the distal tubules of the kidney or ventricles of rainbow trout and eel and exhibited similar cardiovascular effects8, 9.
Although natriuretic peptides exert important effects in the cardiovascular system, the circulating half-life of ANP is only 3–5 min, the half-life of BNP is approximately 23 min4, and the half-life of CNP is only 2–3 min. Although designed-ANP and BNP analogs have been widely used to treat experimental heart failure, the clinical application of natriuretic peptides has been limited10, 11 due to the low chemical synthetic efficiency, expensive fabrication cost, and vulnerability to degradation in vivo.
In recent studies, synthetic chimeric natriuretic peptides, such as VNP, CD-NP, and CU-NP, were shown to maximize the beneficial properties of their donor natriuretic peptides12,13,14,15, and the extension of natural natriuretic peptide applications has become a research hotspot. In our previous study, we innovatively designed and synthesized a chimera peptide named CNAAC 16 (the C-terminus and ring of ANP was combined with the N-terminus of CNP), which has potent vasorelaxant, diuretic and hypotensive effects. These actions of CNAAC imply that it may be applicable in the treatment of heart failure.
Therefore, the present study was designed to determine whether CNAAC has a longer duration of action and higher stability than ANP, CNP or VNP and whether it can be used to treat left ventricular dysfunction after myocardial infarction in rats.
Results
Temporal Course of Natriuretic Peptide-Induced Relaxation
Figure 1 illustrates the effect of a single concentration (10−6 M) of NPs on NE-induced contractility. Control strips were steady during the observation time and were not significantly different from the basal level. The relaxation induced by ANP or CNP decreased after 10 min, relaxation induced by VNP decreased after 15 min, and relaxation induced by CNAAC increased steadily over the entire 25 min. Relaxation in response to all the peptides remained significantly greater than the basal level throughout the 25-min study period (P < 0.01).
During the first 5 min, the magnitude of the relaxation induced by CNAAC or ANP was greater than that produced by CNP (P < 0.05). During 10, 15, 20, and 25 min, the magnitude of the relaxation induced by CNAAC, VNP, or ANP was greater than that induced by CNP (P < 0.01). The relaxation effect of CNAAC was greater than that of VNP at 10, 15, 20, and 25 min (P < 0.01) and was also greater than ANP at 20 and 25 min (P < 0.01).
Stability of CNAAC in the Circulation of Rats
To further investigate the stability of CNAAC, NPs were administered, the rat serum was separated, and the remaining NPs were detected.
In the first 5 min, 52.2% of CNP, 39.9% of ANP, 20.3% of VNP, and 9.9% of CNAAC were degraded (Fig. 2a). The remaining levels of VNP and CNAAC were greater than those of ANP or CNP (P < 0.01). At 10 min, only 19.1% of CNP and 32.7% of ANP remained, and the remaining VNP and CNAAC levels were higher than those of ANP or CNP (P < 0.05 or P < 0.01) (Fig. 2b); the remaining level of CNAAC was greater than that of VNP (P < 0.05). Less than 10% of ANP or CNP remained at 20 min (Fig. 2c), and the compounds were completely degraded at 30 min. More than 30% of VNP and CNAAC remained at 20 min, the remaining level of CNAAC was greater than that of VNP (P < 0.01) at 20 min. At 30 min, the remaining VNP and CNAAC levels were still detectable, the remaining level of CNAAC was greater than VNP (P < 0.05) (Fig. 2d).
Effect of CNAAC on Cardiac Hypertrophy after Myocardial Infarction
After 4 weeks, body weights were decreased in the MI group compared to the sham group (P < 0.05) and lung weights were similar among groups (Table 1). The left ventricular weight, heart weight, ratios of the left ventricular weight to body weight (LVW/BW), heart weight to body weight (HW/BW), and lung weight to body weight (LW/BW) in the MI group were higher than in the sham group (P < 0.01). The MI-NP groups showed significantly reduced LVW/BW and HW/BW compared with the MI group (P < 0.05 or P < 0.01), and only the CNAAC-treated group showed significantly reduced LW/BW (P < 0.05).
Effect of CNAAC on Hemodynamics and Left Ventricular Remodeling
Hemodynamics examinations revealed that the heart rate did not change in each group, LVSP and ± dp/dtmax were significantly decreased (P < 0.01) (Table 2), and LVEDP was significantly increased in the MI group (P < 0.01). After NP administration, left ventricular function, as reflected by these parameters, was reversed (P < 0.05, P < 0.01) (Table 2). These results suggest that natural NP and CNAAC elicited a significant protective effect on cardiac function.
After 4 weeks, the impulses of the ventricular anterior wall in the MI group weakened significantly and the heart volume enlarged, which were detected by echocardiography (Fig. 3a); cardiac function also improved in the NP-treated groups. Compared with the Sham group, EF and FS in the MI group decreased significantly (P < 0.01) (Fig. 3b,c) and the LVEDD, LVESD, LVEDV, and LVESV increased significantly (P < 0.01) (Fig. 3d,e). In addition, all the MI-NPs groups showed elevated EF and FS (P < 0.01). Only the MI-CNAAC group showed decreased LVEDD and LVESD compared with the MI group (P < 0.01), and the effect of CNAAC was stronger than the other three NPs (P < 0.05 or P < 0.01) (Fig. 3d). LVEDV and LVESV were decreased in all four NP groups (P < 0.01), and the effect of CNAAC was more potent than the other NPs (P < 0.05 or P < 0.01) (Fig. 3e).
Effects of NPs on left ventricular remodeling after myocardial infarction. (a) Echocardiography in each group. (b,c,d) Effects of NPs on cardiac function (n = 6). EF: Left ventricular ejection fraction, FS: Left ventricular fractional shortening, LVEDD: left ventricular end diastolic diameter, LVESD: left ventricular end systolic diameter, LVEDV: left ventricular end-diastolic volume, LVESV: left ventricular end-systolic volume. Data are expressed as the mean ± the SEM. **P < 0.01 vs. Sham, ## P < 0.01 vs. MI, $ P < 0.05, $$ P < 0.01 vs. MI-ANP, && P < 0.01 vs. MI-CNP, vs. ^ P < 0.05, ^^ P < 0.01 vs. MI-VNP.
Examination of the Infarct Size and Collage Volume Fraction after Myocardial Infarction
As shown in Masson’s trichrome stain (optical microscopy), the MI group showed a diffused brick-red staining in the cytoplasm, with large scales of blue collagen, and less blue collagen was observed in the MI-NP groups (Masson’s trichrome stain, 40 × , 400 × , Fig. 4a). Compared with the Sham group, the infarct size and collage volume fraction (CVF) in the MI group were significantly increased (P < 0.01) (Fig. 4b,c). The infarct size and CVF decreased significantly after NP administration (P < 0.01). The effects of VNP and CNAAC on the infarct size were stronger than those of ANP or CNP (P < 0.01). The effect of VNP on CVF was stronger than that of ANP, and the effect of CNAAC was stronger than other three NPs (P < 0.01) (Fig. 4c).
Effect of NPs on myocardial infarct size and collagen volume fraction. (a) Representative images of Masson’s trichrome stained blue collagen in each group (original magnification, 40× , 400× ). The scale bars in 40 × magnification pictures represent 200 μm, the scale bars in 400× magnification pictures represent 20 μm. The cytoplasm appears dark-red and collagen fibers are blue; (b) Effect of NPs on myocardial infarct size; (c) Effect of NPs on collagen volume fraction. Gross size in the MI group was larger than that in the Sham group. Wall thinning and the whitish color of the infarcted areas in left ventricle were detected with Masson’s trichrome stain, and thick blue colored fibrosis was found (original magnification, 400× ). CVF: collagen volume fraction. Data are expressed as the mean ± the SEM; n = 5 in each experimental group. **P < 0.01 vs. Sham; ## P < 0.01 vs. MI; $ P < 0.05, $$ P < 0.01 vs. MI-ANP; && P < 0.01 vs. MI-CNP; ^^ P < 0.01 vs. MI-VNP.
Examination of Humoral Factors in Serum
At 4 weeks after surgery, the serum BNP, Ang II, ALD and ET-1 levels in the MI group increased significantly compared with those of the sham group (P < 0.01) (Fig. 5). The serum level of BNP decreased only after VNP or CNAAC administration (P < 0.01) (Fig. 5a); the serum level of Ang II and ET-1 decreased after ANP, CNP, VNP or CNAAC administration (P < 0.05 or P < 0.01) (Fig. 5b and d); and the serum level of ALD decreased after ANP, VNP, and CNAAC administration (P < 0.05 or P < 0.01) (Fig. 5c). The serum level of cGMP in the MI group decreased dramatically compared with that in the sham group, whereas it was increased after ANP, CNP, VNP or CNAAC administration (P < 0.05 or P < 0.01) (Fig. 5e).
Effect of NPs on humoral factors in the serum of rats. (a) Effect of NPs on serum BNP levels in rats; (b) Effect of NPs on serum Ang II levels in rats; (c) Effect of NPs on plasma ALD levels in rats; (d) Effect of NPs on serum ET-1 levels in rats; (e) Effect of NPs on serum cGMP levels in rats (n = 6). Data are expressed as the mean ± the SEM; n = 6 in each experimental group. **P < 0.01 vs. Sham; # P < 0.05, ## P < 0.01 vs. MI.
Discussion
In our previous study, we confirmed that the new chimera CNAAC had potent vasorelaxant, diuresis and hypotensive effects. Based on these cardiorenal effects, we further demonstrated that CNAAC elicited inhibitory effects on left ventricular remodeling in the present study. A continuous infusion of CNAAC for four weeks improved the systolic and diastolic function, ameliorated myocardial infarction and fibrosis, and even normalized plasma biomarkers of heart failure.
Our previous study demonstrated that CNAAC had more potent vasorelaxant effects than ANP and CNP16. To better understand whether CNAAC had a longer effect time than the other NPs, the abdominal aorta was obtained and a temporal examination was performed. We found that the vasorelaxant effect of CNAAC lasted for a long time and steadily increased over the entire examination. By contrast, the relaxation induced by ANP or CNP began to decrease at 10 min, and the relaxation induced by VNP began to decrease at 15 min. The results suggested that CNAAC has a longer duration of action than ANP, CNP, or VNP. To further confirm the stability of CNAAC in circulation, the remaining NPs in the serum were detected after NPs were administered. The remaining NPs were detected at 5, 10, 20, and 30 min. It has been reported that the half-life of ANP and CNP is very short, almost 2–3 min4. The results of the present study are in accordance with previous results. The levels of CNP and ANP decreased by almost half in the first 5 min, while the levels of VNP and CNAAC were stable. Over time, VNP and CNAAC were degraded slowly, and at 30 min, some VNP and CNAAC were still present. This result suggests that chimeric natriuretic peptides are stable in circulation and have longer durations of action than natural natriuretic peptides.
Cardiac dysfunction and pathophysiologic adaption were observed in rats subjected to ligation of the coronary artery17, 18. In the current study, the left ventricular dysfunction model was established via ligation of the coronary artery for 4 weeks. After 4 weeks, MI rats showed increased LVW/BW, HW/BW, and LW/BW, indicating that MI rats exhibited severely cardiac hypertrophy and pulmonary congestion; these results were consistent with others19. The four MI-NP groups showed reduced LVW/BW and HW/BW, and the CNAAC-treated group showed reduced left ventricular weight, heart weight and LW/BW, indicating a satisfactory reversal of cardiac hypertrophy.
Diastolic dysfunction caused by coronary artery ligation always appears earlier than systolic dysfunction20. MI rats displayed increased LVEDP, LVEDD, LVESD, LVEDV and LVESV and decreased LVSP, ± dp/dtmax, EF and FS; all these changes reflect serious diastolic and systolic dysfunction of the left ventricle in rats. Many studies have demonstrated the effect of NPs and their analogs in the treatment of myocardial ischemia and infarction15, 21,22,23. Our data showed that a 4-week intraperitoneal injection of natriuretic peptides (20 nmol/kg/2 d) apparently ameliorates both cardiac systolic (LVSP, EF, FS, + dp/dtmax) and diastolic function (LVEDP, −dp/dtmax). In particular, CNAAC significantly decreased LVEDD, LVESD, LVEDV, and LVESV, and these effects were greater than with the other three natriuretic peptides, suggesting that CNAAC significantly improves cardiac function and the effect of CNAAC is more potent than its donor or homology natriuretic peptide in some respects.
CNAAC has more potent relaxation effect than ANP, CNP, and VNP, thus our previous study showed that CNAAC has more potent hypotensive and diuretic effects in normal rats16. The peripheral vascular resistance (after-loading) and blood volume were reduced due to the vasodilation and diuresis caused by CNAAC, therefore CNAAC exerts potent cardioprotective effect in the present study, and shows more efficacious than other peptides in some parameters. Because CNAAC has more potent vasorelaxant effect, the venous return in the MI-CNAAC group was reduced relatively compare with other NP-treated groups. On the other hand, MI-CNAAC group showed more potent effect to reduce the LVEDV and LVESV, it means the myocardial contractility was improved in the MI-CNAAC group. Combine these two aspects, the EF may remain unchanged compared with other NP-treated groups.
Histological analysis demonstrated that myocardial fibrosis and infarct size were significantly decreased after administration of the four natriuretic peptides (i.p. for 4 weeks). The effect of VNP or CNAAC was greater than that of ANP or CNP. These results suggest that CNAAC may have a potent cardioprotective effect.
In the present study, besides consulting the typical operation method from other researchers24, 25, operation was conducted by same laboratory technician, ligation was carried out at the same position of coronary artery, and the same age and weight of rats were adopted, and above all, the survival rats which undergone surgery were randomly divided into MI or MI-NP groups. All these steps should objectively ensure that there are no significant differences among groups before NPs treatment. However, very recent study has reported that serum concentration of troponin I should be measured 24 h after coronary artery ligation to indirectly estimate myocardial infarct size and confirm that there are no differences among groups26. We totally agree that this is really a more effective method to avoid between-group variance and is valuable to be used in the future study.
The level of serum BNP has been shown to be elevated in patients with left ventricular dysfunction27, and has been widely used in the diagnosis of heart failure11. It was demonstrated in the present study that the BNP level was decreased after VNP or CNAAC was administered. The potential reason for this decrease is that the cardiac load was decreased and cardiac function was improved by VNP or CNAAC. In addition, the effect of precipitating factors that cause BNP release from the heart was decreased by CNAAC administration. RAAS has been shown to be activated in rats after myocardial infarction, and the serum Ang II and ALD levels were shown to be significantly increased in the MI group in the present study. Previous studies have shown that plasma ALD levels may be elevated significantly in HF patients, primarily due to an increased production by the adrenal glands following stimulation by the high plasma Ang II concentrations28, 29. Although ANP and BNP were released from the heart after MI, the amount was insufficient to resist the effect of the sympathetic nervous system, RAAS, and vasopressin. RAAS inhibitors are currently the cornerstone pharmacotherapy for chronic heart failure30, and the present study showed that the Ang II and ALD levels were significantly decreased by CNAAC. These results suggested that RAAS, a precipitating factor that causes BNP release from the heart, was inhibited by CNAAC.
ET-1 participates in the pathological process of heart failure or myocardial infarction31. Jandeleit-Dahm KA et al.20, 32, 33 found that natriuretic peptides promote cGMP production to inhibit the ET-1 synthesis caused by ischemia or hypoxia. In the present study, when rats were subjected to myocardial infarction, the serum ET-1 level increased significantly, and this elevated ET-1 was decreased by treatment with natriuretic peptides. In our previous study, abdominal aortic cGMP production was increased after incubation with natriuretic peptides; in the present study, serum cGMP was decreased in the MI group and the cGMP level was increased after natriuretic peptide administration, which are in accordance with previous studies34, 35.
Taken together, our results demonstrate that CNAAC, a newly designed NP chimera, exerts a longer duration of action and potent cardioprotective effects against left ventricular dysfunction. These findings may lay the foundation for future studies aimed at the clinical application of natriuretic peptide chimeras in the treatment and prevention of heart failure after myocardial infarction.
Methods
Peptide synthesis and Reagents
Human ANP, CNP, VNP and the designed CNAAC were synthesized by GL Biochem Ltd. (Shanghai, China) and were confirmed to have a purity of approximately 95% by high-performance liquid chromatography analysis. ACh and L-norepinephrine (NE) were purchased from Sigma-Aldrich Co. LLC (St. Louis, MO, USA). Rat BNP, angiotensin II (Ang II), aldosterone (ALD), endothelin-1 (ET-1), and cyclic guanosine monophosphate (cGMP) ELISA kits were purchased from Shanghai Lianshuo Biological Technology Co., Ltd. (Lianshuo, Shanghai, China).
Animals
Male Sprague-Dawley (SD) rats (250 ± 20 g body weight) from the animal center of the Fourth Military Medical University were housed under specific pathogen-free conditions, with free access to water and food and a 12 h light/12 h dark cycle. All experiments were conducted according to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85–23, revised 1985) and were approved by University Ethics (the Ethical Committee of the Fourth Military Medical University).
Although we identified that CNAAC has potent vasodilating, diuretic, and hypotensive effects, it was not clear whether it has a longer duration of action than its analog VNP or other natural NPs. Therefore, in vivo and in vitro experiments were conducted as follows.
Examination of the temporal relaxation effect of CNAAC
Rats were sacrificed and the abdominal aorta was obtained. The abdominal aorta, K-H solution, experimentation system, and the operational program were prepared and used as described in our previous study12. After a 30-min equilibration, NE (10−6 M) was added to induce a vasoconstriction effect. The contraction amplitude caused by NE (10−6 M) is approximately 1750 ± 250 mg in the control and the treatment group. To study the temporal relaxation effect of CNAAC, Normal Saline or NPs (10−6 M) were added when a stable contraction was reached. The effect of NPs on abdominal aorta contractility was measured as the activity during the 5-min period after their administration to the organ bath, and the data were recorded in 5-min intervals. Each maximal contraction induced by 10−6 M NE was arbitrarily set as 100%. Relaxation data are the reduced percentage of maximal contractile amplitudes16.
Examination of the metabolic status of CNAAC
To determine the metabolic status of NPs in circulation, blood was collected from rats after a bolus injection of NPs. Rats were anesthetized with pentobarbital sodium (40 mg/kg i.p). One microcatheter was inserted into the left jugular vein to administer NPs, and another one was inserted into the right carotid artery to collect blood. After the surgery was completed, rats were allowed to stabilize for 15 min. Human ANP, CNP, VNP, or CNAAC at a concentration of 40 nmol/kg was administered in a bolus fashion (0.1 ml). Blood (0.5 ml) was sampled 5, 10, 20, and 30 min after the bolus injection. The samples from the plasma were analyzed using LT-20AT High-Performance-Liquid-Chromatography (HPLC) (Shimadzu, Tokyo, Japan). A linear gradient (Buffer A: acetonitrile with 0.05% trifluoroacetic acid; Buffer B: double distilled water with 0.05% trifluoroacetic acid)36 was used for both analyses to separate peptides on an Inertsil OSD-3 (250 mm × 4.6 mm, 5 µm) chromatographic column (Shimadzu, Tokyo, Japan) and a Water Quatro-premier tandem quadrupole mass spectrometry and Alliance 2695 chromatographic system (Waters, Milford, Massachusetts, USA). Peak areas have been calculated with the Masslynx 4.1 software from Waters. Four independent experiments were performed. Each experiment was conducted in duplicate, whereby duplicates are defined as two different vials.
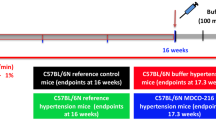
Examination of the cardioprotective effect of CNAAC
Animals were divided into six groups: Group 1: Sham (i.p. 0.5 ml 0.85% NaCl/2d; n = 6); Group 2: MI (i.p. 0.5 ml 0.85% NaCl/2d; n = 6); Group 3: MI-ANP (i.p. 0.5 ml ANP, 20 nmol/kg·2d; n = 6); Group 4: MI-CNP (i.p. 0.5 ml CNP, 20 nmol/kg·2d; n = 6); Group 5: MI-VNP (i.p. 0.5 ml VNP, 20 nmol/kg·2d; n = 6); Group 6: MI-CNAAC (i.p. 0.85% NaCl; 20 nmol/kg·2d; n = 6).
The Sham and MI animal model were established as described by Johns TN et al.24, 25 Rats were anesthetized with pentobarbital sodium (40 mg/kg i.p.), and then the left anterior descending coronary artery was ligated in the MI and MI-NP groups. The chest was closed immediately. Only a thoracotomy and closure were performed in the sham group. From the day of surgery, 0.85% NaCl or NPs (20 nmol/kg) were administered to these groups (i.p), one injection every two days and lasted for four weeks. Four weeks later, the cardiac function was measured by Doppler echocardiography under anesthesia with pentobarbital sodium (40 mg/kg i.p.). A 12 MHz linear probe (Vevo2100, VisualSonics, Inc., CAN) was used to perform the transthoracic echocardiography. Left ventricular (LV) ejection fraction (EF), LV fraction shortening (FS), LV end diastolic diameter (LVEDd), and left ventricular end systolic diameter (LVESd) were measured. All examinations were performed in a blinded state.
The day after echocardiography was performed; rats in each group were weighed and anesthetized via a peritoneal injection of pentobarbital sodium (40 mg/kg i.p.). Supplemental doses of sodium pentobarbital were given when needed to maintain uniform anesthesia. A micro catheter was inserted into the left ventricle through the right external jugular artery, and left ventricular systolic pressure (LVSP), left ventricular end diastolic pressure (LVEDP), and ± dp/dtmax were recorded by the BL-420F BioData Acquisition & Analysis Systems (TME Technology Co, Ltd, Chengdu, China). At the end of the experiment, blood was sampled and the following parameters were recorded: heart weight (HW), left ventricle weight (LVW), and lung weight (LW).
Analysis of humoral factors
Blood samples were centrifuged (4000 rpm, 15 min) and the serum was separated. Serum BNP, Ang II, ALD, ET-1, cGMP levels were detected with rat ELISA kits (Lianshuo, Shanghai, China).
Histological analysis
Rats in each group were anesthetized with pentobarbital sodium (40 mg/kg i.p.). Their hearts were then separated and fixed in 4% formaldehyde for 48 hours, and Masson’s trichrome stain was performed. Myocardial infarction and fibrosis were observed by Masson staining. We calculated infarct size as follows: Infarct size (%) = Length of infarction area / (inner perimeter of left ventricle + outer perimeter of left ventricle) /2 × 100%. We randomly chose six segments, and then photomicrographs of each segment stained by Masson trichrome were acquired with a scanner. Imagin-Pro Plus (version 6.0) was used to calculate the collagen volume fraction (CVF): CVF (%) = collagen area / total area × 100%.
Statistical analysis
All data were expressed as the mean ± the SEM and analyzed with either t-tests (two groups) or ANOVAs (three or more groups). A Bonferroni correction was performed for post hoc t-tests. P values less than 0.05 were considered statistically significant. Graphpad prism 5 was used to create all artwork.
References
Yamazaki, T. et al. Tolvaptan improves left ventricular dysfunction after myocardial infarction in rats. Circ Heart Fail 6, 794–802 (2012).
Suzuki, T., Yamazaki, T. & Yazaki, Y. The role of the natriuretic peptides in the cardiovascular system. Cardiovasc Res 51, 489–494 (2001).
Abassi, Z., Karram, T., Ellaham, S., Winaver, J. & Hoffman, A. Implications of the natriuretic peptide system in the pathogenesis of heart failure: diagnostic and therapeutic importance. Pharmacol Ther 102, 223–241 (2004).
Woodard, G. E. & Rosado, J. A. Recent advances in natriuretic peptide research. J Cell Mol Med 11, 1263–1271 (2007).
Sudoh, T., Kangawa, K., Minamino, N. & Matsuo, H. A new natriuretic peptide in porcine brain. Nature 332, 78–81 (1988).
Sudoh, T., Minamino, N., Kangawa, K. & Matsuo, H. C-type natriuretic peptide (CNP): a new member of natriuretic peptide family identified in porcine brain. Biochem Biophys Res Commun 168, 863–870 (1990).
Schweitz, H., Vigne, P., Moinier, D., Frelin, C. & Lazdunski, M. A new member of the natriuretic peptide family is present in the venom of the green mamba (Dendroaspis angusticeps). J Biol Chem 267, 13928–13932 (1992).
Takei, Y. et al. Rainbow trout ventricular natriuretic peptide: isolation, sequencing, and determination of biological activity. Gen Comp Endocrinol 96, 420–426 (1994).
Forssmann, W. G., Richter, R. & Meyer, M. The endocrine heart and natriuretic peptides: histochemistry, cell biology, and functional aspects of the renal urodilatin system. Histochem Cell Biol 110, 335–357 (1998).
Burger, A. J. et al. Effect of nesiritide (B-type natriuretic peptide) and dobutamine on ventricular arrhythmias in the treatment of patients with acutely decompensated congestive heart failure: the PRECEDENT study. Am Heart J 144, 1102–1108 (2002).
Park, Y. H. et al. BNP as a marker of the heart failure in the treatment of imatinib mesylate. Cancer Lett 243, 16–22 (2006).
Wei, C. M., Kim, C. H., Miller, V. M. & Burnett, J. C. Jr. Vasonatrin peptide: a unique synthetic natriuretic and vasorelaxing peptide. J Clin Invest 92, 2048–2052 (1993).
McKie, P. M., Sangaralingham, S. J. & Burnett, J. C. Jr. CD-NP: an innovative designer natriuretic peptide activator of particulate guanylyl cyclase receptors for cardiorenal disease. Curr Heart Fail Rep 7, 93–99 (2010).
Rose, R. A. CD-NP, a chimeric natriuretic peptide for the treatment of heart failure. Curr Opin Investig Drugs 11, 349–356 (2010).
Kilic, A. et al. A novel chimeric natriuretic peptide reduces cardiomyocyte hypertrophy through the NHE-1-calcineurin pathway. Cardiovasc Res 88, 434–442 (2010).
Zhang, S. M. et al. Cardiovascular and renal effect of CNAAC: An innovativele designed natriuretic peptide. Eur J Pharmacol 761, 180–188 (2015).
Maki, T., Nasa, Y., Tanonaka, K., Takahashi, M. & Takeo, S. Beneficial effects of sampatrilat, a novel vasopeptidase inhibitor, on cardiac remodeling and function of rats with chronic heart failure following left coronary artery ligation. J Pharmacol Exp Ther 305, 97–105 (2003).
Yoon, N. et al. Preventive effects of the angiotensin-II receptor blocker on atrial remodeling in an ischemic heart failure model of rats. Korean Circ J 43, 686–693 (2013).
Aksentijević, D. et al. High-energy phosphotransfer in the failing mouse heart: role of adenylate kinase and glycolytic enzymes. Eur J Heart Fail 12, 1282–1289 (2010).
Jandeleit-Dahm, K. A. & Watson, A. M. The endothelin system and endothelin receptor antagonists. Curr Opin Nephrol Hypertens 21, 66–71 (2012).
Cohn, P. F., Herman, M. V. & Gorlin, R. Ventricular dysfunction in coronary artery disease. Am J Cardiol 33, 307–310 (1974).
Asanuma, H. et al. Carperitide induces coronary vasodilation and limits infarct size in canine ischemic hearts: role of NO. Hypertens Res 37, 716–723 (2014).
Zakeri, R. & Burnett, J. C. Designer natriuretic peptides: a vision for the future of heart failure therapeutics. Can J Physiol Pharmacol 89, 593–601 (2011).
Johns, T. N. & Olson, B. J. Experimental myocardial infarction. I. A method of coronary occlusion in small animals. Ann Surg 140, 675–682 (1954).
Patten, R. D. & Hall-Porter, M. R. Small animal models of heart failure: development of novel therapies, past and present. Circ Heart Fail 2, 138–144 (2009).
Santulli, G., Xie, W., Reiken, S. R. & Marks, A. R. Mitochondrial calcium overload is a key determinant in heart failure. Proc Natl Acad Sci USA 112, 11389–11394 (2015).
Maisel, A. S. et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347, 161–167 (2002).
Lymperopoulos, A. et al. An adrenal β-arrestin 1-mediated signaling pathway underlies angiotensin II-induced aldosterone production in vitro and in vivo. Proc Natl Acad Sci USA 106, 5825–5830 (2009).
Lymperopoulos, A., Rengo, G. & Koch, W. J. Adrenergic nervous system in heart failure: pathophysiology and therapy. Circ Res 113, 739–753 (2013).
Capote, L. A., Mendez Perez, R. & Lymperopoulos, A. GPCR signaling and cardiac function. Eur J Pharmacol 763, 143–148 (2015).
Yanagisawa, M. et al. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332, 411–415 (1988).
Emori, T. et al. Cellular mechanism of natriuretic peptides-induced inhibition of endothelin-1 biosynthesis in rat endothelial cells. Endocrinology 133, 2474–2480 (1993).
Fujisaki, H. et al. Natriuretic peptides inhibit angiotensin II-induced proliferation of rat cardiac fibroblasts by blocking endothelin-1 gene expression. J Clin Invest 96, 1059–1065 (1995).
Moltzau, L. R. et al. Different compartmentation of responses to brain natriuretic peptide and C-type natriuretic peptide in failing rat ventricle. J Pharmacol Exp Ther 350, 681–690 (2014).
Ozawa, T. et al. Effects of human atrial natriuretic peptide on myocardial performance and energetics in heart failure due to previous myocardial infarction. J Cardiol 66, 232–238 (2015).
Zhu, X., Wang, Y., Schwiebs, A. & Walther, T. Chimeric natriuretic peptide ACNP stimulates both natriuretic peptide receptors, the NPRA and NPRB. Mol Cell Endocrinol 366, 117–123 (2013).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81270402) and grants from Shaanxi Province of China (No. 2016JM3022, No. 2016KTCL03–11).
Author information
Authors and Affiliations
Contributions
J.-M.P. and W.-S.C. designed the research and approved the final version of the manuscript, S.-M.Z., H.-L.Z. and X.-M.G. performed the experiments, X.-M.G. and J.L. analyzed the results, S.-M.Z., H.-L.Z. and N.F. interpreted the results, Y.-M.W. and R.F. drafted and edited the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, SM., Zhao, HL., Gu, XM. et al. A New Chimeric Natriuretic Peptide, CNAAC, for the Treatment of Left Ventricular Dysfunction after Myocardial Infarction. Sci Rep 7, 10099 (2017). https://doi.org/10.1038/s41598-017-10748-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10748-6
This article is cited by
-
Cardiac natriuretic peptides
Nature Reviews Cardiology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.