Abstract
Clinical management of Clostridium difficile infection is still far from satisfactory as bacterial spores are resistant to many chemical agents and physical treatments. Certain types of nanoparticles have been demonstrated to exhibit anti-microbial efficacy even in multi-drug resistance bacteria. However, most of these studies failed to show biocompatibility to the mammalian host cells and no study has revealed in vivo efficacy in C. difficile infection animal models. The spores treated with 500 µg/mL Fe3-δO4 nanoparticles for 20 minutes, 64% of the spores were inhibited from transforming into vegetative cells, which was close to the results of the sodium hypochlorite-treated positive control. By cryo-electron micro-tomography, we demonstrated that Fe3-δO4 nanoparticles bind on spore surfaces and reduce the dipicolinic acid (DPA) released by the spores. In a C. difficile infection animal model, the inflammatory level triple decreased in mice with colonic C. difficile spores treated with Fe3-δO4 nanoparticles. Histopathological analysis showed a decreased intense neutrophil accumulation in the colon tissue of the Fe3-δO4 nanoparticle-treated mice. Fe3-δO4 nanoparticles, which had no influence on gut microbiota and apparent side effects in vivo, were efficacious inhibitors of C. difficile spore germination by attacking its surface and might become clinically feasible for prophylaxis and therapy.
Similar content being viewed by others
Introduction
Nanomaterials have attracted significant interest in medicine. Certain microorganism-reactive nanomaterials have been used as alternative bactericides1, namely, silver, zinc oxide, and titanium oxide nanoparticles, all of which have remarkable antibacterial properties2, 3. The antibacterial mechanisms of nanoparticles may be attributable to their generation of reactive oxygen species, disruption of cell membranes, ability to bind thiol groups, and their release of toxic ions4. Spore-formation enables bacteria to survive nutritional deprivation and harsh environments. They can resist ultraviolet radiation, desiccation, high temperatures, extreme freezing, and chemical disinfectants5. Spores can reactivate themselves to the vegetative state when the environment becomes favorable. Therefore, Clostridium species, spore-forming pathogens, usually challenge clinical disease management and prevention. Clostridium difficile, a pathogen associated with healthcare-facility-related (nosocomial) infections, is a major cause of antibiotic-treatment-related diarrhea, pseudomembranous colitis, abdominal pain, fever, and death6. The normal flora in the gut can inhibit the growth of C. difficile and therefore protect patients from developing C. difficile infection7. C. difficile infection usually occurs in patients on a long-term regimen of antibiotics, and it is often initiated by the spores acquired from healthcare workers8, 9. Once a patient develops C. difficile infection, there are only a few antibiotics available to control it10. Moreover, the failure rate of first-line antibiotics and the C. difficile infection relapse rate are both dramatically high10, 11. Consequently, about two decades ago, the attributable post-diagnosis mortality rate was 6.9% at 30 days and 16.7% at 1 year12. The spores of C. difficile are the major cause of C. difficile infection. Compared with oxygen-sensitive vegetative bacteria, C. difficile spores survive for up to several months in room air and in low-pH gastric contents13. As the spores enter the human digestive tract, they germinate after they have been exposed to bile salts and their derivatives, and then they are colonized in the colon14. The virulence of C. difficile depends upon the gene expression of tcdA-encoded toxin A, an enterotoxin, and tcdB-encoded toxin B, a cytotoxin15. Both cause intestinal inflammation and neutrophil infiltration in the infected foci16, 17.
The incidence of C. difficile infection has significantly increased in the past 15 years18. C. difficile infection has become a major cause of nosocomial-associated infection in the world9. Antibiotic-resistant C. difficile is not only potentially fatal, but it also causes healthcare-associated economic burdens19. The available present antibiotics are targeted to vegetative bacterium, however, the infective form is the spore. Current C. difficile infection clinical management is still far from satisfactory because the spores are resistant to many chemical agents and physical treatments, which makes effective management of the spores an important problem20. Therefore, anti-germination approach could lead to the prevention of C. difficile infection. Some newly designed cholate derivatives show promise against C. difficile infection; however, they are still under pre-clinical study21, 22. Sodium hypochlorite, a standard disinfectant, has outstanding antimicrobial activity but undesirable side effects: it is corrosive and irritates tissue5. To control spore germination and C. difficile infection, it is important to develop an efficacious and biocompatible spore-control strategy.
There are various well-known antibacterial nanomaterials, e.g., silver (Ag) and zinc oxide (ZnO) nanoparticles23, 24, and zero-valent iron nanoparticles, which are prominently bactericidal against Escherichia coli 25. The nanotechnology even has been reported that it could overcome the problem of multi-drug resistant bacteria26. However, most current antibacterial nanomaterials are primarily multifunctional generic biocidal agents against vegetative cells; their sporicidal activity at high concentrations has been explored in only a few studies27, 28. Many studies demonstrated the excellent antibacterial ability of nanoparticles, but their impacts to the gut microbiota were not clear. The healthy gut microbiota prevent the host from colonic pathogen29. Therefore, an ideal antibacterial nanomaterial should exhibit the specific pathogen targeting capability without causing disruption of healthy gut microibota.
The toxicity of various bactericidal nanoparticles to mammalian cells has become an increasing concern. Iron-containing particles are generally recognized as highly biocompatible nanomaterials. A few specific iron oxide nanoparticles have recently been reported to be antibacterial; they were synthesized and showed therapeutic potential for cancer therapy30, 31. In this study, we evaluated whether such single-crystal nonstoichiometric Fe3-δO4 magnetite nanoparticles could inhibit C. difficile spore germination in vivo. The potential mechanisms were explored from both material science and molecular biology perspectives.
Results
Testing the sporicidal activity of Fe3-δO4 nanoparticles against C. difficile
We used a previously described method32 to explore the inhibitory efficacy of Fe3-δO4 nanoparticles to spores. After they had been incubated with sodium hypochlorite for 20 minutes, inactivated spores were used as positive controls, as described elsewhere33. After they had been incubated with nanomaterials of various concentrations (5, 50, and 500 μg/mL) for 20 minutes, the treated spores were then stimulated using 10 mM taurocholate to induce germination.
Spores treated with 50 and 500 μg/mL of Fe3-δO4 nanoparticles showed significantly (**P < 0.01 and ***P < 0.001) inhibited germination (Fig. 1), but spores treated with 5 μg/mL did not. There were no significant differences between the sodium hypochlorite-treated positive controls and the Fe3-δO4 nanoparticle-treated (500 μg/mL) spores (Fig. 1). Intriguingly, there was no significant difference in germination inhibition between spores treated with 14-nm and 22-nm Fe3-δO4 nanoparticles (Fig. 2A). In Supplementary Table 1, the germination kinetic results show that the Michaelis-Menten constant (Km) for taurocholate-treated C. difficile CCUG 37780 spores increased from 4.34 to 8.43 M in mice treated with 50 μg/mL of Fe3-δO4 nanoparticles. The kinetic analysis suggested that Fe3-δO4 nanoparticles have an inhibiting constant (Ki) of approximately 62 μg/mL. To confirm the sporicidal property of 500 μg/mL of Fe3-δO4, the number of Fe3-δO4- and 3%-sodium hypochlorite-treated colony-forming unit (CFU) spores was counted. Compared with the negative control set, the number of CFUs of Fe3-δO4-treated and 3%-sodium hypochlorite-treated spores was ~60% lower (Fig. 2B). Furthermore, the inhibition rates of CFUs in Fe3-δO4-treated and in 3%-sodium hypochlorite-treated spores were not significantly different.
C. difficile spore germination was significantly inhibited in spores treated with Fe3-δO4 nanoparticles. Purified CCUG 37780 spores were incubated in BHIS medium containing Fe3-δO4 nanoparticles ([500 µg/mL (▲), 50 µg/mL ( ), or 5 μg/mL (▵)]), or 3% sodium hypochlorite as a positive control. The kinetics of spore germination was analyzed using spectrometric absorption referenced to the starting point. OD600(T) = different time points after taurocholate treatment; OD600(T0) = time zero. Spore germination was significantly inhibited in spores treated with Fe3-δO4 nanoparticles. (***P < 0.001; one-way analysis of variance [ANOVA] followed by Tukey’s Multiple Comparison test).
), or 5 μg/mL (▵)]), or 3% sodium hypochlorite as a positive control. The kinetics of spore germination was analyzed using spectrometric absorption referenced to the starting point. OD600(T) = different time points after taurocholate treatment; OD600(T0) = time zero. Spore germination was significantly inhibited in spores treated with Fe3-δO4 nanoparticles. (***P < 0.001; one-way analysis of variance [ANOVA] followed by Tukey’s Multiple Comparison test).
The viability and germination inhibition of C. difficile CCUG 37780 spores by Fe3-δO4 nanoparticles were dose-dependent rather than size-dependent. (A) The spores were first treated for 20 minutes with 500 μg/mL of 22-nm Fe3-δO4 (■), 500 μg/mL of 14-nm Fe3-δO4 (▲), 50 μg/mL of 22-nm Fe3-δO4 (□), 50 μg/mL of 14-nm Fe3-δO4 (▵), or 3% sodium hypochlorite (●) and then were treated with taurocholate to induce germination. Both 14-nm and 22-nm Fe3-δO4 nanoparticles had a similar dose-dependent effect on spore germination. (B) After C. difficile spores and 500 μg/mL of 22-nm Fe3-δO4 nanoparticles or 3% sodium hypochlorite had been incubated for 20 minutes, the spores were plated on BHIS agar for a colony formation assay the next day. The level of colony-forming unit inhibition was similar for Fe3-δO4 nanoparticle- and sodium hypochlorite-treated spores. (C) The spores were treated for 20 minutes with 500 μg/mL of 22-nm Fe3-δO4 and then stimulated using 10 mM taurocholate. After 15 minutes, the phase contrast of the spores was recorded under a phase contrast microscope. (D) The DPA-release assay showed that Fe3-δO4 nanoparticles-treated spores released less DPA than did the control group. Data are mean ± SEM. (***P < 0.001; one-way analysis of variance (ANOVA) followed by Tukey’s Multiple Comparison test).
Phase-contrast microscopy showed that in the positive controls, to which taurocholate was added for 15 minutes, but not in the negative controls, the contrast of the spores transitioned from bright to dark (Fig. 2C). The contrasts of the spores treated with 500 μg/mL Fe3-δO4 nanoparticles were not significantly different. The luminescence signal that accompanies DPA release was significantly higher during taurocholate-induced spore germination (Fig. 2D). However, the luminescence signal was less intense and less abundant in the Fe3-δO4-treated group than in the taurocholate-treated group. No luminescence signal was detected in the group of spores not treated with taurocholate because the spores did not release DPA.
Inhibitory effect of Fe3-δO4 nanoparticles on virulent strains of C. difficile
C. difficile strain CCUG 37780 does not have the tcdA and tcdB genes34. To determine what doses of Fe3-δO4 nanoparticles affect the spore germination of C. difficile, CCUG 19126 and BAA-1805 tcdA- and tcdB-positive strains were treated for 20 minutes with 5, 50, and 500 μg/mL doses of Fe3-δO4 nanoparticles, and then treated with 10 mM taurocholate. The germination of C. difficile CCUG 19126 spores and of C. difficile BAA-1805 spores was not significantly different between those treated with 500 μg/ml of Fe3-δO4 nanoparticles and those treated with sodium hypochlorite, but CCUG 19126 was relevantly resistant to treatment with 50 μg/mL of Fe3-δO4 nanoparticles (Fig. 3A).
Spore germination was significantly inhibited in Fe3-δO4-treated pathogenic strains of C. difficile. Spores from two pathogenic strains of C. difficile (CCUG 19126 and ATCC BAA-1805) were treated for 20 minutes with various concentrations of Fe3-δO4 nanoparticles and then with 10 mM taurocholate to induce spore germination. Spore germination was effectively inhibited in the two Fe3-δO4-treated pathogenic strains, as it was in the nonpathogenic CCUG 37780 strain. (***P < 0.001, *P < 0.05; one-way analysis of variance [ANOVA] followed by Tukey’s Multiple Comparison test).
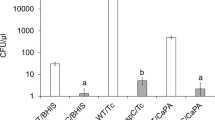
To evaluate the bactericidal effect of Fe3-δO4 nanoparticles on vegetative cells in different strains, three groups of vegetative cells—CCUG 37780, CCUG 19126, and BAA-1805—were first treated for 20 minutes with 500 μg/mL of Fe3-δO4 nanoparticles, spread on BHIS agar plates, and their CFUs were counted. The growth behavior of the Fe3-δO4-treated vegetative cells was not significantly different from that of the negative control groups; however, almost all the vegetative cells treated with 3% sodium hypochlorite died (Fig. 4). Treatment with Fe3-δO4 nanoparticles did not damage C. difficile vegetative cells.
The viability of C. difficile vegetative cells was not significantly affected by Fe3-δO4-treatment. Fe3-δO4 nanoparticles (500 µg/mL) did not inhibit the viability of vegetative C. difficile in all three test strains compared cells treated with 3% sodium hypochlorite. (***P < 0.001; Student’s t test).
The mechanisms underlying Fe3-δO4-inhibited spore germination
To determine whether any additional underlying mechanisms allow Fe3-δO4 nanoparticles to inhibit spore germination, we first excluded the sporicidal activity of the coating polymer poly-(styrene-alt-maleic acid) (PSMA) on Fe3-δO4 nanoparticles. At a concentration higher than that on PSMA-coated on Fe3-δO4 nanoparticles, PSMA did not inhibit spore germination (Supplementary Fig. 1). In addition, to verify whether Fe3-δO4 nanoparticles promoted or hindered the germination-inducing activity of taurocholate, 10 mM taurocholate was incubated for 20 minutes with different concentrations of Fe3-δO4 nanoparticles and then used to treat spores. The taurocholate incubated with Fe3-δO4 nanoparticles still induced C. difficile spore germination (Supplementary Fig. 2).
To identify any additional underlying mechanisms that allow Fe3-δO4 nanoparticles to inhibit spore germination, we took advantage of the magnetic property of Fe3-δO4. Some C. difficile BAA-1805 spores were incubated with 500 μg/mL of Fe3-δO4 nanoparticles for 20 minutes and then separated, using a magnet, into two parts: the nonmagnetic supernatant and the magnetic pellets (Fig. 5A). Each part was collected, and PCR was used to detect the tcdB gene. The tcdB gene was detected only in the supernatant (Fig. 5B) in the spores-alone groups. In the Fe3-δO4-treated spores, the tcdB gene was also detected in the magnetic pellets.
Fe3-δO4 nanoparticles bound to the surface of C. difficile (ATCC BAA-1805) spores, which allowed magnetic attraction. (A) Schematic illustration of the magnetic separation of spores with which Fe3-δO4 nanoparticles had bound: these spores were attracted by a magnet, but spores with which the nanoparticles had not bound were retained in the supernatant. (B) The spores were incubated for 20 minutes with Fe3-δO4 nanoparticles, and then tcdB genes were isolated from the supernatant or the magnetically concentrated precipitates were detected after PCR amplification. Lanes 1–3 are spores alone and lanes 4–6 are spores treated with 500 µg/mL of Fe3-δO4 nanoparticles. TcdB amplicons were detected in the supernatant of the control group, but they were found only in the magnetically concentrated fraction after they had been treated with Fe3-δO4 nanoparticles. (C) TEM images of the spores (upper panel: 10,000×; lower panel: 30,000×). The left image shows that native spores have a smooth coat; accumulated Fe3-δO4 nanoparticles on spore surfaces are evident after incubation. The spores treated with 500 µg/mL were completely covered by the Fe3-δO4 nanoparticles.
To clarify the interaction between Fe3-δO4 and spores, the Fe3-δO4-treated spores were examined under a TEM. The TEM images showed that spores treated with 50 μg/mL of Fe3-δO4 nanoparticles were only spotted with Fe3-δO4 nanoparticles, but that spores treated with 500 μg/mL were almost fully surrounded (Fig. 5C). To reconfirm that Fe3-δO4 nanoparticles were simply attached to the surface of the spores instead of diffused into the spores, the spores were examined using cryo-electron tomography. The rotated dynamic video (Supplementary Video 1) revealed that Fe3-δO4 nanoparticles were directly and dose-dependently bound to the surface of C. difficile spores.
Fe3-δO4 nanoparticles as an in vivo sporicidal agent against C. difficile infection
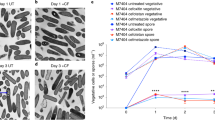
Before the mouse experiments, the cytotoxicity of Fe3-δO4 nanoparticles was evaluated using a methylthiazol tetrazolium (MTT) assay. The colorectal cells were treated with various concentrations of Fe3-δO4 nanoparticles (5 to 500 μg/mL) for 24 hours. The viability of C2BBe1 cell line were decreased at the 500 μg/mL of Fe3-δO4 nanoparticles. However, the cell viability assay showed no significant cytotoxicity of the Fe3-δO4 nanoparticles in HT-29 cell line compared with the control group (Supplementary Fig. 3). To investigate the feasibility of Fe3-δO4 nanoparticles as an in vivo sporicidal agent, we used a C. difficile infection mouse model. The inflammatory signal peaked 3 days after C. difficile infection had been induced (Supplementary Fig. 4). Therefore, in the mouse experiment, we examined the C. difficile infection pathology 3 days after the mice had been treated with spores. Mice treated with Fe3-δO4 nanoparticles plus spores lost significantly less body weight than did the mice treated with spores alone (P = 0.0119, Student’s t test) (Fig. 6A). The cecum weight of the Fe3-δO4-treated mice was significantly higher than that of the mice treated with spores alone (P = 0.0024, Student’s t test) (Fig. 6B), which showed minor inflammation under an in vivo imager (P = 0.0406, Student’s t test) (Fig. 6C). The histopathological images also showed that neutrophil infiltration was lower in the mice treated with Fe3-δO4 nanoparticles plus spores (Fig. 6D) than in the control mice treated with spores alone. A real-time reverse transcription quantitative polymerase chain reaction (RT-qPCR) was used to determine the expression of the proinflammatory genes TNF-α, IFN-γ, and IL-1β, compared with the spores-alone groups (Fig. 6E). The level of inflammation caused by the spores was significantly lower (P = 0.0088 for TNF-α, P = 0.0276 for IFN-γ, and P = 0.0097 for IL-1β, Student’s t test) at the molecular level in the mice treated with Fe3-δO4 nanoparticles plus spores than in the mice treated with spores alone. To verify whether treatment with 500 μg/mL Fe3-δO4 nanoparticles alone induces any adverse side effects in vivo, we fed the mice with nanoparticles alone and monitored the biochemistry markers (Supplementary Fig. 5). Based on the ratio of Firmicutes to Bacteroidetes, we found this nanoparticle does not altered the gut microbiota (Supplementary Fig. 6A), suggesting that this particle did not has the toxicity to the mice.
C. difficile infection-induced colitis was attenuated in mice treated with Fe3-δO4 nanoparticles. Purified CCUG 19126 spores were incubated for 20 minutes with Fe3-δO4 nanoparticles, and then the mice were injected with them. Three days later, the mice were killed. (A) The mean bodyweight-loss of the Fe3-δO4 nanoparticle-treated mice was significantly lower than that of the spores-alone control mice. (B) The mean weight-loss of the cecums of the Fe3-δO4 nanoparticle-treated mice was also significantly lower than that of spores-alone control mice. (C) The inflammation of the isolated colon from 11FNL/FVB/NJ transgenic mice with NF-κB-signal-activated bioluminescence was detected. The left image shows a spores-alone control colon and the right image a Fe3-δO4-nanoparticle-treated colon. C. difficile infection-induced inflammation was significantly lower in the Fe3-δO4 nanoparticle-treated colon (right panel). (D) A histopathological examination of the isolated colon tissue shows prominent infiltration of neutrophils (black arrows in left 400× panel) in the control group, but attenuated inflammation in the Fe3-δO4 nanoparticle-treated group (right 400× panel). Neutrophils were morphometrically counted in 10 randomly selected fields in the tissue sections. The number of neutrophils in the control group was 16 ± 5 per 170 m × 130 µm field; the number in the Fe3-δO4 nanoparticles-treated group was 2 ± 1 per 170 m × 130 µm field. (E) A reverse transcription-quantitative polymerase chain reaction (RT-QPCR) shows that the total RNA extracted from the Fe3-δO4-nanoparticle-treated spores expressed significantly lower levels of proinflammatory genes than did the spores in the control group. (*P < 0.05, **P < 0.01; Student’s t test) (n = 6).
Discussion
Based on our review of the literature, this is the first study which shows Fe-based nanoparticles that strongly inhibited the germination of C. difficile spores despite the growth inhibitory effect of other type of iron oxide nanoparticles to other bacteria vegetative cells was recently reported.
Iron oxide nanoparticles have existed in the earth’s stratum and some organisms35. Due to the iron oxide nanoparticles are widely used in medical applications. The iron oxide nanoparticles not only can be the MRI T2 contrast material but also be conjugated to other dyes as detection reagents for different imaging systems35. The iron oxide nanoparticles could be used as hyperthermia-based cancer therapeutic reagent when combined to radiofrequency. The iron oxide nanoparticles could even be modified with different materials to become the multi-functional nanoparticles, e.g., targeting, drug releasing, and imaging abilities36. We performed the new function of iron oxide nanoparticles that could be a C. difficile spore germination inhibition reagent in the study. The 22-nm-Fe3-δO4 nanoparticles presented as unique octahedron single crystals, and the ratio of iron to oxide was 2.966:4, similar to our previously reported 6-nm Fe3O4 nanoparticles30. The differences between Fe3-δO4 and Fe3O4 include size, surface chemistry, and the presence of minor non-oxidized Fe voids in the Fe3-δO4 particles. There was no significant difference between the inhibitory ability of the 22-nm and the 14-nm Fe3-δO4 doses. The amount of DPA released from the spores was significantly lower in the Fe3-δO4-treated group than in the positive controls. The transition of spores from bright to dark can be observed with a phase-contrast microscope after the DPA has been released37. In the present study, because Fe3-δO4 nanoparticles inhibited spore germination, there was no transition of spores into phase-dark. However, DPA could be detected, but not in as great abundance as with the taurocholate-treated spores, after the spores had been exposed to Fe3-δO4 nanoparticles. Thus, it is conceivable that there is an underlying mechanism that enables Fe3-δO4 nanoparticles both to induce DPA release and to inhibit spore germination. We hypothesized that taurocholate can be caught by Fe3-δO4 nanoparticles and block the interaction between taurocholate and CspC. CspC is a bile salt germination receptor in C. difficile and transmits the signal to the downstream signaling molecule. However, we later discovered that taurocholate does not bind with Fe3-δO4 nanoparticles, and that taurocholate supernatant without Fe3-δO4 nanoparticles was able to trigger C. difficile spore germination. Therefore, we now hypothesize that Fe3-δO4 nanoparticles inhibit bacterial growth without directly interacting with taurocholate. We also hypothesize that Fe3-δO4 nanoparticles do not penetrate spores based on our cryo-TEM Supplementary Video 1. The details of the molecular mechanisms of Fe3-δO4 nanoparticles require additional study.
Zero-valent iron (ZVI) has recently been reported38 to be involved in the selective inhibition of cancerous cells while sparing noncancerous cells because it depletes mitochondrial membrane potential. Because mitochondria share distinct structural and biochemical similarities as well as evolutionary links to bacteria, we hypothesize that the nonstoichiometric non-oxidized Fe of Fe3-δO4 also inhibits spore germination. In fact, one study25 reported a prominent bactericidal effect of ZVI-based nanoparticles on E. coli because they effectively caused oxidative damage to bacterial membranes. Our study showed that Fe3-δO4-treatment significantly inhibited the germination of C. difficile spores by damaging spore membranes but not the vegetative cells and therefore did not damage the balance of intestinal normal flora. Thus the specific activity to spore germination must go through other yet to be discovered mechanisms.
It is well known that the expression of the tcdA and tcdB genes is closely associated with the virulence of C. difficile infection. We found that Fe3-δO4 nanoparticles inhibited germination in both the tcdA(−)tcdB(−) strain and the more virulent tcdA(+)tcdB(+) strain. In an in vivo C. difficile infection mouse experiment, we found that Fe3-δO4 significantly reduced the inflammation indices in the groups treated with spores +Fe3-δO4, and that it effectively inhibited C. difficile spore germination, thus controlling in vivo the virulence of C. difficile. Intriguingly, treatment with 500 μg/mL of Fe3-δO4 nanoparticles did not kill vegetative cells.
Because antibiotics are overused everywhere in the world, multidrug-resistant microbes have emerged as a major public health threat39. Nanomedicines have inspired various new strategies to control microbes without allowing them to develop drug resistance40. Bacterial spores are even more resistant than are the bacteria themselves to harsh environments and antibiotics, but nanoparticle-spore interaction and potential clinical applications are rarely discussed. The germination of Bacillus subtilis spores is greatly compromised by treatment with polyionic polymers and then silica nanoparticles41. Such treatment, however, does not affect spore viability. We also found that excess PSMA alone did not significantly inhibit the germination of spores; therefore, PSMA must not be important for inhibiting spore germination. In the present study, 500 μg/mL of Fe3-δO4 nanoparticles were sufficient to significantly, and almost as efficaciously as 3% sodium hypochlorite, inhibit spore germination, which indicated the potential of Fe3-δO4 nanoparticles for clinical development as a novel and effective treatment for managing and perhaps even preventing C. difficile infection.
Many studies showed their materials existed excellent antibacterial activity, but sometimes the impact of the materials on the normal flora and biocompatibility were rarely discussed. The guts normal flora plays a vital role in animals, because it attend the metabolism and pathogenic colonization prevention in the host29. Therefore, we should have to understand the potential adverse effect of Fe3-δO4 nanoparticles on normal flora and biocompatibility. We found that Fe3-δO4 nanoparticles at a concentration of 500 μg/mL inhibited spore germination but did not damage their vegetative cells. Another study42 reported that a high concentration (3 mg/mL) of Fe3O4 nanoparticles inhibited the growth of Staphylococcus aureus. After mice were fed with Fe3-δO4 nanoparticles for 72 hours, RT-qPCR was used to analyze the results of normal flora population changes. The two main phyla of bacteria in the gut are Firmicutes and Bacteroidetes 43. We found that the Fe3-δO4 nanoparticles did not change the ratio of Firmicutes to Bacteroidetes in the mice (Supplementary Fig. 6A). Bacteroides fragilis and Enterococcus faecalis are the common bacteria in the large intestine44, 45. Our results showed that Fe3-δO4 nanoparticles did not cause damage to the two bacteria (Supplementary Fig. 6B). According to our results we hypothesize that Fe3-δO4 nanoparticles do not cause imbalance of gut microbiota. The Fe3-δO4 nanoparticles will not be an issue in the normal flora destruction after administering to human and other animals. We also found excellent biocompatibility between Fe3-δO4 nanoparticles and a variety of colorectal cells. We previously reported30, 31 that Fe3-δO4 nanoparticles used with MRI scans and cancer therapy were safe. Although the safe dosages are different in these three studies, we have shown that Fe3-δO4 nanoparticles are biocompatible and safe in vivo.
Metronidazole and vancomycin are antibiotics frequently used to treat patients with C. difficile infection, but the some clinical isolates are metronidazole-resistant46. Antibiotics unselectively damage pathogens as well as normal flora and might trigger a highly contagious state of super-shedding C. difficile spores, thus increasing the risk of infection47. Spores can survive for many years in harsh environments and wait to be ingested by animals48. The imbalance of normal flora and spore germination might be the major cause of a C. difficile infection relapse. Moreover, bowel inflammation has long been recognized as an important index for C. difficile infection severity and prognosis. Therefore, we quantitatively assessed C. difficile infection by directly injecting mice with spores, which is most relevant to the pathogenesis of clinical C. difficile infection. Transgenic mice with NF-κB-dependent luciferase reporter enabled us to visualize bowel inflammation using the IVIS imaging system. Because of their unique ability to selectively kill spores without damaging normal flora, mammalian cells, or the mouse gastrointestinal tract, Fe3-δO4 nanoparticles offer a new strategy for controlling infectious clinical diseases. Fe3-δO4 nanoparticle treatment not only inhibited the germination of different clinical strains of C. difficile spores in vitro, but also reduced the virulence of spores that induced C. difficile infection in vivo. We also report the first relatively low-dose but efficacious Fe-based nanoparticle inhibition of spore germination, one which uses a novel mechanism that does not interfere with the growth of healthy vegetative flora, which is an important clinical consideration in C. difficile infection management. We hypothesize that coating the surfaces of medical devices with Fe3-δO4 nanoparticles will reduce the threat of spores in hospitals. Additional research on improving the design of Fe3-δO4 nanoparticles should help nanoparticle-based therapeutics become safer and more effective, and should contribute to the development of new therapeutics for C. difficile infection and other emerging infectious diseases.
Methods
Ethics statement and animals
All NF-κB-dependent reporter mice (FVB/NJNarl genetic background) were obtained from the National Laboratory Animal Center in Taiwan and housed in a pathogen-free barrier facility. All animal experiments were approved and in accordance with the relevant guidelines and regulations required by the Institutional Animal Care and Use Committee of National Cheng Kung University (NCKU-IACUC-102-296).
Bacterial culture and spore purification
C. difficile CCUG 37780 (tcdA−, tcdB−) and CCUG 19126 (tcdA+, tcdB+) were purchased from the Culture Collections of the University of Göteborg (Göteborg, Sweden), and BAA-1805 (tcdA+, tcdB+) from American Type Culture Collection (Manassas, VA). All strains were incubated in brain-heart infusion-supplemented medium (BHIS; BD Difco, Franklin Lakes, NJ), with 0.5% yeast extract (BD Difco) and 0.1% L-cysteine (Amresco, Solon, OH), at 37 °C under anaerobic conditions. The spores were prepared and purified as previously described32 with a slight modification. Briefly, C. difficile in BHIS medium was diluted in fresh BHIS medium to an optical density (OD) (600 nm) of 0.2. The diluted bacterial suspension (900 μL) was added to a 6-well dish with BHIS agar, and then the dish was incubated at 37 °C in an anaerobic jar (Thermo Fisher, Oxoid Ltd., Basingstoke, England) for 4 days. The whole cells were washed 5 times with ice-cold sterile water, the bacteria were resuspended with 3 mL of ice-cold sterile MQ water. The suspension was spread on top of a 10-mL 50% (wt/vol) sucrose solution (J.T. Baker Chemical, Phillipsburg, PA) in a centrifuge tube, and then centrifuged at 3500 g for 20 minutes to separate spores from vegetative cells. The purified spores at the bottom of the centrifuge tube were washed 5 times with ice-cold sterile water to remove sucrose, and then stored at 4 °C.
Preparation of the nanoparticles
Fe3-δO4 nanoparticles (22 nm and 14 nm) were synthesized using thermal decomposition, as previously described30. Briefly, 1.42 g of iron acetylacetonate was mixed with 0.57 mL of oleic acid and 20 mL of trioctylamine (all 3: Sigma-Aldrich, St. Louis, MO). The solution was refluxed at 325 °C in an argon environment for 30 minutes. After the solution had cooled down to room temperature, the precipitates were collected with a magnet and washed 3 times with toluene. The Fe3-δO4 nanoparticles were collected with a magnet and then transferred to chloroform solutions (Merck, Whitehouse Station, NJ) containing 0.4 mg/mL of PSMA (Sigma-Aldrich) and were left there for 6 hours at 55 °C. The Fe3-δO4 nanoparticles were collected, washed 3 times with MQ water, and then stored at 4 °C.
Optical density based spore germination test
Spores were germinated as previously described32. Before the germination experiments, the spore suspension was incubated at 60 °C for 30 minutes. The heat-treated spores were then moved to ice. The C. difficile spores (concentration: OD600 0.5) were co-incubated with various nanoparticles or at different concentrations (5 to 500 μg/mL) in BHIS in a 96-well plate for 20 minutes. The concentration of Fe3-δO4 nanoparticles was measured based on the total particle weight per 1 mL of solution. Fe3-δO4 (22-nm) nanoparticles were used here. Spores treated with 3% bleach (Wako, Osaka, Japan) were the positive controls to inhibit germination, and spores treated with BHIS only were the negative controls. After the spore + nanoparticle co-incubation, the spores were treated with 10 mM taurocholate (Sigma-Aldrich) to induce germination. The OD600 of treated spores was kinetically determined at 1 minute intervals using a spectrophotometer (TECAN, Grödig, Austria) at room temperature for 12 minutes. The OD at different time points was used to plot the spore germination curve.
Phase-contrast microscopy observation of spore germination
The images of spore germination were recorded using phase-contrast optical microscopy described elsewhere49. The purified spores were incubated at 60 °C for 30 minutes. The spores were co-incubated for 20 minutes with 500 μg/mL of Fe3-δO4 nanoparticles or with buffer alone. Taurocholate was then added to the samples to a final concentration of 10 mM in BHIS. Five microliters of samples were then dropped onto the 0.7% agarose surface on the glass slide. After 15 minutes, phase-contrast images of the spores were captured (Nikon Eclipse 80i; Tokyo, Japan). Six random fields of view were obtained for each experimental group.
Dipicolinic acid (DPA) release assay
The DPA release was estimated by modified method from a previous study50. Briefly, the spores were heated as described and washed with distilled water then resuspended in spore germination buffer (10 mM Tris [pH 7.5], 150 mM NaCl, and 100 mM glycine). The spores were treated with MQ water or 500 μg/mL of Fe3-δO4 nanoparticles for 20 minutes in a black 96-well plate before taurocholate (10 mM) and terbium (III) chloride (TbCl3) (100 μM) were added. The total DPA of the spores was extracted by boiling the samples for 30 minutes. The spores treated with TbCl3 only were negative controls. The DPA-Tb signal was monitored immediately in real-time using a microplate reader (FlexStation 3 Multi-Mode; Molecular Devices, CA) with excitation/emission at 270 nm and 545 nm, and a cutoff at 530 nm.
Spore viability analysis
After the spore germination curves had been recorded, each aliquot was removed from the 96-well plate and plated on BHIS agar dishes and serially diluted. The plate-counts (CFU/mL) at each dilution were done after 48 hours of incubation in an anaerobic environment. The inhibition rates were calculated using the following formula:
Nanoparticle-spore binding analysis
C. difficile BAA-1805 spores at a concentration of OD600 0.5 were co-incubated with Fe3-δO4 nanoparticles (500 μg/mL) in BHIS in a 96-well plate for 20 minutes. The spore samples without Fe3-δO4 treatment were controls. The samples were placed next to a magnet for 5 minutes and then all supernatant was removed to other tubes. The magnet-attracted parts and supernatant were washed 3 times with 1× phosphate-buffered saline. All samples were resolved in distilled deionized water, and the tcdB DNA in samples was detected using a polymerase chain reaction (PCR). Spore and nanoparticle images were captured using a transmission electron microscope (TEM) (JEM-1400; JEOL, Tokyo, Japan).
In vivo analysis of C. difficile infection
To directly monitor the colonic inflammation, we infected mice with C. difficile spores in a previously generated NF-κB-dependent reporter mouse model containing the luciferase transgene under the transcriptional control of NF-κB (NF-κB-RE-luciferase)51. Before the mice were fed the spores with NF-κB reporter, they were given an antibiotic cocktail (0.4 mg/mL of kanamycin, 0.035 mg/mL of gentamicin, and 0.057 mg/mL of colistin) in their drinking water for 48 hours and a refreshed cocktail every 24 hours for 2 days. The mice were gavaged with a 200-μL proton pump inhibitor (PPI) (2 mg/mL) every 12 hours for 2 days before the C. difficile spore infection. C. difficile CCUG 19126 spores (2 × 105 CFUs) were co-incubated with or without 500 μg/mL of Fe3-δO4 nanoparticles for 20 minutes before they were gavaged with 100 L of sample solution. While the spores and Fe3-δO4 nanoparticles were incubating, all the mice were gavaged with a 50- μL PPI (2 mg/mL) and then intraperitoneally injected with clindamycin (4 mg/kg). The antibiotic cocktail water was replaced with normal water after the C. difficile infection. All mice were monitored for C. difficile infection symptoms, e.g., diarrhea, weight loss, hunched posture, and death. Seventy-two hours post-infection, the mice were intraperitoneally injected with 150 mg/kg of luciferin (PerkinElmer, Waltham, MA) to show NF-κB activation-mediated luminescence. The mice were anesthetized with isoflurane and oxygen, and then images were collected for 5 minutes using an imaging system (Xenogen IVIS® Spectrum; Advanced Molecular Vision, Grantham, Lincolnshire, UK). Data were analyzed (Xenogen Living Image®), and luciferase activity was presented in photons/sec/cm2/steradian (p/s/cm2/sr). After the IVIS images had been obtained, a reagent (TRI; Sigma-Aldrich) was used to extract RNA from colon tissue samples. The levels of inflammatory gene expression were estimated using a real-time PCR assay (StepOnePlus; Applied Biosystems).
Histopathology examination
Histopathological analysis was used to evaluate C. difficile infection-induced mucosal damage and inflammation. Resected colon tissue samples were fixed in 4% formaldehyde buffered with PBS and then embedded in paraffin. Deparaffinized 6-μm-thick sections were stained with hematoxylin and eosin. The results were captured using optical microscopy. Neutrophils were randomly counted in 10 fields for both the spores-alone group and the Fe3-δO4-treated-spores group.
Statistical analysis
GraphPad Prism 5.01 was used for all statistical analyses. All experiments were done in triplicate. Data are means ± standard error of the mean (SEM) from three independent experiments. One-way analysis of variance (ANOVA) and then Tukey’s Multiple Comparison test were used for spore germination curve analyses, and Student’s t test was used in the other CFU inhibition test.
References
Morones, J. R. et al. The bactericidal effect of silver nanoparticles. Nanotechnology 16, 2346 (2005).
Prucek, R. et al. The targeted antibacterial and antifungal properties of magnetic nanocomposite of iron oxide and silver nanoparticles. Biomaterials 32, 4704–4713 (2011).
Jones, N., Ray, B., Ranjit, K. T. & Manna, A. C. Antibacterial activity of ZnO nanoparticle suspensions on a broad spectrum of microorganisms. FEMS Microbiol Lett 279, 71–76 (2008).
Hajipour, M. J. et al. Antibacterial properties of nanoparticles. Trends Biotechnol 30, 499–511 (2012).
Barbut, F. et al. Comparison of the efficacy of a hydrogen peroxide dry‐mist disinfection system and sodium hypochlorite solution for eradication of Clostridium difficile spores. Infect Control Hosp Epidemiol 30, 507–514 (2009).
Hedge, D. D., Strain, J. D., Heins, J. R. & Farver, D. K. New advances in the treatment of Clostridium difficile infection (CDI). Ther Clin Risk Manag 4, 949 (2008).
Voelker, R. I. Clostridium difficile virulence demands new treatment approach. JAMA 303, 2017–2019 (2010).
Vardakas, K. Z. et al. Treatment failure and recurrence of Clostridium difficile infection following treatment with vancomycin or metronidazole: a systematic review of the evidence. Int J Antimicrob Agents 40, 1–8 (2012).
Loo, V. G. et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile–associated diarrhea with high morbidity and mortality. N Engl J Med 353, 2442–2449 (2005).
Jump, R. L., Pultz, M. J. & Donskey, C. J. Vegetative Clostridium difficile survives in room air on moist surfaces and in gastric contents with reduced acidity: a potential mechanism to explain the association between proton pump inhibitors and C. difficile-associated diarrhea? Antimicrob Agents Chemother 51, 2883–2887 (2007).
Wilson, K. H. & Perini, F. Role of competition for nutrients in suppression of Clostridium difficile by the colonic microflora. Infect Immun 56, 2610–2614 (1988).
Russell, A. Bacterial resistance to disinfectants: present knowledge and future problems. J Hosp Infect 43, S57–S68 (1999).
Owens, R. C., Donskey, C. J., Gaynes, R. P., Loo, V. G. & Muto, C. A. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin Infect Dis 46, S19–S31 (2008).
Burns, D. A., Heap, J. T. & Minton, N. P. Clostridium difficile spore germination: an update. Res Microbiol 161, 730–734 (2010).
Lyras, D. et al. Toxin B is essential for virulence of Clostridium difficile. Nature 458, 1176–1179 (2009).
Poutanen, S. M. & Simor, A. E. Clostridium difficile-associated diarrhea in adults. CMAJ 171, 51–58 (2004).
Hirota, S. A. et al. Intrarectal instillation of Clostridium difficile toxin A triggers colonic inflammation and tissue damage: development of a novel and efficient mouse model of Clostridium difficile toxin exposure. Infect Immun 80, 4474–4484 (2012).
Ananthakrishnan, A. N. Clostridium difficile infection: epidemiology, risk factors and management. Nat Rev Gastroenterol Hepatol 8, 17–26 (2010).
Sebaihia, M. et al. The multidrug-resistant human pathogen Clostridium difficile has a highly mobile, mosaic genome. Nat Genet 38, 779–786 (2006).
Wilcox, M. H. & Fawley, W. N. Hospital disinfectants and spore formation by Clostridium difficile. Lancet 356, 1324 (2000).
Howerton, A., Patra, M. & Abel-Santos, E. A new strategy for the prevention of Clostridium difficile infection. J Infect Dis 207, 1498–1504 (2013).
Howerton, A., Ramirez, N. & Abel-Santos, E. Mapping interactions between germinants and Clostridium difficile spores. J Bacteriol 193, 274–282 (2011).
Xiu, Z.-m, Zhang, Q.-b., Puppala, H. L., Colvin, V. L. & Alvarez, P. J. Negligible particle-specific antibacterial activity of silver nanoparticles. Nano Lett 12, 4271–4275 (2012).
Kumar, A., Pandey, A. K., Singh, S. S., Shanker, R. & Dhawan, A. Engineered ZnO and TiO2 nanoparticles induce oxidative stress and DNA damage leading to reduced viability of Escherichia coli. Free Radic Biol Med 51, 1872–1881 (2011).
Lee, C. et al. Bactericidal effect of zero-valent iron nanoparticles on Escherichia coli. Environ Sci Technol 42, 4927–4933 (2008).
Cavassin, E. D. et al. Comparison of methods to detect the in vitro activity of silver nanoparticles (AgNP) against multidrug resistant bacteria. Journal of nanobiotechnology 13, 1 (2015).
Hamal, D. B. et al. A multifunctional biocide/sporocide and photocatalyst based on titanium dioxide (TiO2) codoped with silver, carbon, and sulfur. Langmuir 26, 2805–2810 (2009).
Gopinath, P. M. et al. Multi-functional nano silver: A novel disruptive and theranostic agent for pathogenic organisms in real-time. Sci Rep 6, 34058 (2016).
Jandhyala, S. M. et al. Role of the normal gut microbiota. World J Gastroenterol 21, 8787–8803 (2015).
Huang, C. C. et al. Size-control synthesis of structure deficient truncated octahedral Fe3−δO4 nanoparticles: high magnetization magnetites as effective hepatic contrast agents. J Mater Chem 21, 7472–7479 (2011).
Li, T. J. et al. In vivo anti-cancer efficacy of magnetite nanocrystal-based system using locoregional hyperthermia combined with 5-fluorouracil chemotherapy. Biomaterials 34, 7873–7883 (2013).
Sorg, J. A. & Sonenshein, A. L. Inhibiting the initiation of Clostridium difficile spore germination using analogs of chenodeoxycholic acid, a bile acid. J Bacteriol 192, 4983–4990 (2010).
Lawley, T. D. et al. Use of purified Clostridium difficile spores to facilitate evaluation of health care disinfection regimens. Appl Environ Microbiol 76, 6895–6900 (2010).
Kubota, H. et al. Development of TaqMan-based quantitative PCR for sensitive and selective detection of toxigenic Clostridium difficile in human stools. PLoS One 9, e111684 (2014).
Lee, N. et al. Iron oxide based nanoparticles for multimodal imaging and magnetoresponsive therapy. Chem Rev 115, 10637–10689 (2015).
Laurent, S. et al. Magnetic iron oxide nanoparticles: synthesis, stabilization, vectorization, physicochemical characterizations, and biological applications. Chem Rev 108, 2064–2110 (2008).
Yung, P. T. & Ponce, A. Fast sterility assessment by germinable-endospore biodosimetry. Appl Environ Microbiol 74, 7669–7674 (2008).
Wu, Y. N. et al. The anticancer properties of iron core–gold shell nanoparticles in colorectal cancer cells. Int J Nanomedicine 8, 3321 (2013).
Levy, S. B. & Marshall, B. Antibacterial resistance worldwide: causes, challenges and responses. Nat Med 10, S122–S129 (2004).
Pelgrift, R. Y. & Friedman, A. J. Nanotechnology as a therapeutic tool to combat microbial resistance. Adv Drug Deliv Rev 65, 1803–1815 (2013).
Balkundi, S. S., Veerabadran, N. G., Eby, D. M., Johnson, G. R. & Lvov, Y. M. Encapsulation of bacterial spores in nanoorganized polyelectrolyte shells. Langmuir 25, 14011–14016 (2009).
Tran, N. et al. Bactericidal effect of iron oxide nanoparticles on Staphylococcus aureus. Int J Nanomedicine 5, 277 (2010).
Mariat, D. et al. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol 9, 123 (2009).
Klein, G. Taxonomy, ecology and antibiotic resistance of enterococci from food and the gastro-intestinal tract. Int J Food Microbiol 88, 123–131 (2003).
Wexler, H. M. Bacteroides: the good, the bad, and the nitty-gritty. Clinical microbiology reviews 20, 593–621 (2007).
Chong, P. M. et al. Proteomic analysis of a NAP1 Clostridium difficile clinical isolate resistant to metronidazole. PLoS ONE 9, e82622 (2014).
Lawley, T. D. et al. Antibiotic treatment of Clostridium difficile carrier mice triggers a supershedder state, spore-mediated transmission, and severe disease in immunocompromised hosts. Infect Immun 77, 3661–3669 (2009).
Wilcox, M. H. Clostridium difficile infection and pseudomembranous colitis. Best Pract Res Clin Gastroenterol 17, 475–493 (2003).
Liu, R., Suárez, J. M., Weisblum, B., Gellman, S. H. & McBride, S. M. synthetic polymers active against Clostridium difficile vegetative cell growth and spore outgrowth. J Am Chem Soc 136, 14498–14504 (2014).
Francis, M. B., Allen, C. A. & Sorg, J. A. Spore cortex hydrolysis precedes dipicolinic acid release during Clostridium difficile spore germination. J Bacteriol 197, 2276–2283 (2015).
Hung, Y. P. et al. Proton pump inhibitor exposure aggravates Clostridium difficile colitis: evidences from a mouse model. J Infect Dis 212, 654–663 (2015).
Acknowledgements
This work was supported by grants from the Taiwan Ministry of Science and Technology (NSC102-2320-B-006-027, NSC101-2314-B-006-048-MY3, and NSC102-2120-M-006- 003); from the Taiwan Ministry of Health and Welfare (MOHW103-TDU-PB-211-113016); from the Taiwan National Research Program for Biopharmaceuticals; and from the Headquarters of University Advancement at National Cheng Kung University, which is sponsored by the Taiwan Ministry of Education. Finally, we thank i-MANI, the International Institute of Macromolecular Analysis and Nanomedicine Innovation, National Cheng Kung University, for providing invaluable technical support.
Author information
Authors and Affiliations
Contributions
D.-B. Shieh and P.-J. Tsai form the concept, designed the study and edited the manuscript. W.-T. Lee did most experiments and draft the manuscript. Y.-N. Wu helped the organization of the manuscript and perform the primary language editing. Y.-H. Chen participated in most animal tests. S.-R. Wu performed all TEM and cryo-EM imaging and interpretation. T.-M. Shih performed part of the spore germination test. T.-J. Li and L.-X. Yang participated in results discussion and part of the animal tests. C.-S. Yeh provided nanoparticles fabrication protocol and guided the synthesis detail.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, WT., Wu, YN., Chen, YH. et al. Octahedron Iron Oxide Nanocrystals Prohibited Clostridium difficile Spore Germination and Attenuated Local and Systemic Inflammation. Sci Rep 7, 8124 (2017). https://doi.org/10.1038/s41598-017-08387-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-08387-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.