Abstract
Our perception of the world is remarkably stable despite of distorted retinal input due to frequent eye movements. It is considered that the brain uses corollary discharge, efference copies of signals sent from motor to visual regions, to compensate for distortions and stabilize visual perception. In this study, we tested whether patients with Alzheimer’s disease (AD) have impaired corollary discharge functions as evidenced by reduced compensation during the perception of optic flow that mimics self-motion in the environment. We asked a group of early-stage AD patients and age-matched healthy controls to indicate the perceived direction of self-motion based on optic flow while tracking a moving target with smooth pursuit eye movement, or keeping eye fixation at a stationary target. We first replicated the previous findings that healthy participants were able to compensate for distorted optic flow in the presence of eye movements, as indicated by similar performance of self-motion perception between pursuit and fixation conditions. In stark contrast, AD patients showed impaired self-motion perception when the optic flow was distorted by eye movements. Our results suggest that early-stage AD pathology is associated with disrupted eye movement compensation during self-motion perception.
Similar content being viewed by others
Introduction
In addition to the progressive loss of memory and cognitive functions, patients with Alzheimer’s disease (AD) at the early stage often exhibit declined visuospatial capabilities1, 2. At the behavioral level, it has been shown that AD patients have poor performance in spatial navigation tasks3 and impaired perception of optic flow that mimics self-motion in the environment4, 5. Comparing to healthy elderly individuals, AD patients possess elevated optic flow thresholds6 and are worse at perceiving and steering in the direction of self-motion based on the pattern of optic flows7. Consistent with these behavioral deficiencies, imaging studies have revealed that AD patients have noticeable atrophy in the superior parietal lobules8, 9 and they show reduced activations in dorsal visual stream areas that are implicated in visuosptial processing10,11,12. There is also evidence that AD patients have impaired ability to bind distinct visual features of a stimulus (e.g., color and motion) in a sensory integration task, implicating that AD pathology might be associated with declined cross-cortical connectivity in the cerebral cortex13, 14.
Corollary discharge, one special form of functional connectivity among cortical regions, is often referred to as efference copies of motor command signals sent from motor to sensory areas that are used to predict the sensory consequence of an impending movement15, 16. Corollary discharge is an integral part of cortical functions that allow the brain to monitor its own actions17 (e.g., during motor planning18 and motor executing19) and compensate for visual distortions to achieve perceptual stability in the presence of eye movements20, 21. There is growing evidence that corollary discharge functions might have failed in several clinical populations leading to neurologic symptoms22 and delusional experiences such as auditory hallucination23, mirror-touch synaesthete24, and schizophrenic disorders25. Up to date, there is little evidence of corollary discharge dysfunctions in AD pathology in the literature.
The purpose of this study is to address whether deficits in corollary discharge functions are present in patients at the early stage of AD. We will assess the influence of eye movements on optic flow perception in AD patients. Eye rotations during pursuit eye movement distort the optic flow by adding a rotational component to it26. Nevertheless, previous findings have shown that healthy human observers barely experience a twisted visual representation27, 28, owing to pursuit compensation mechanisms which are widely believed to rely on corollary discharge signals sent from pursuit areas to visual areas to cancel the distortion29, 30 (for an alternative view, please see31). In this study we will exploit the pursuit compensation effects to examine the potential dysfunction of corollary discharge in AD patients. To this end, we will compare the performance of optic flow perception between a group of AD patients and age-matched healthy elder participants, under the condition of either smooth pursuit eye movements or pure fixations.
Material and Methods
Subjects
Two groups of participants took part in the current study. The first group consisted of 15 early-stage AD patients who were selected based on two criteria: (1) They had to met the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association criteria for the diagnosis of AD32; and (2) According to the assessment of the Mini-Mental State Exam (MMSE)33, they had a MMSE score less than 25 but larger than 18, hence classified as mild cognitive impairment patients. The second group involved 15 age- and sex- matched healthy elderly, most of whom were the spouse or relatives of AD patients tested in the current study. All participants had passed the ophthalmologic exams to be free of other neurologic, ophthalmologic, or psychiatric illnesses. All participants had given informed consent for their participation in the current study prior to the experimentation. All the experiments were performed in accordance with the guidelines and regulations approved by the Ethics Committee of Liaocheng People’s Hospital, China.
Apparatus and optical flow
Subjects seated in a dimly lit room. They rested their chins on a chinrest which helps to stabilize head position. They faced a CRT monitor (screen resolution: 800 × 600; refresh rate: 100 Hz) which was 57 cm away from the chinrest. We used the Psychophysical Toolbox34, 35 to generate the visual optic flow and design the control of experimental flow as described below. The optic flow was made of a cloud of moving dots, consisted of 2000 white dots (each 0.2 deg in diameter) on a black background (0.7 cd/m2) and distributed in a virtual trapezoidal volume. Dots moving outside the trapezoidal volume were randomly assigned to locations on the furthest base as the new starting locations. The speed and luminance gradients of moving dots within this column resemble the visual experience of forward translation in the environment at a speed of 2.5 m/s. Specifically, the focus of expansion (FOE) in the optic flow corresponds to the direction of self-motion, which was interleaved from trial to trial along an imaginary horizontal line, locating at one of the six possible positions (±6.4 degrees, ±3.2 degrees, and ±1.6 degrees), relative to the straight ahead direction (“dead ahead’).
Each trial begun with an initial ocular fixation at the cross (+) for 500 ms. Then the optic flow was presented for 1000 ms, and after a fixed delay of another 500 ms following optic flow offset, participants were required to report the perceived self-motion direction (either left or right relative to the straight ahead direction) by means of keyboard presses (Fig. 1). There were two task conditions. In the fixation condition, the central cross remained stationary during the visual stimulus presentation, and subjects’ task was to fixate their gaze at the cross. In the pursuit condition, during stimulus presentation the cross moved along the horizontal line at a speed of 5 degree/s (either leftward or rightward), and participants were asked to make smooth pursuit eye movements to keep track of the cross. Fixation and pursuit trials were randomly interleaved on a trial-by-trial basis. We used the method of constant stimuli and repeated each combination of conditions 10 trials to obtain the psychometric curve of self-motion perception as a function of FOE angles.
Optic flow perception task and experimental conditions. Participants faced a CRT monitor displaying a cloud of moving dots mimicking the observer’s forward translation on a straight path. The focus of expansion (FOE), which determines the direction of self-motion, could be at one of the six potential positions in a single trial. Participants were asked if perceived direction is to the left- or right- side of the dead ahead. In the fixation condition participants kept their gaze constant whereas in the pursuit conditions they made pursuit eye movements to track the moving cross.
The logic in our design was, if the brain is able to compensate for visual distortions caused by pursuit eye movements, we should expect similar performance of self-motion perception between fixation and pursuit conditions. Many previous studies have already demonstrated that healthy observers can precisely judge self-motion directions in the presence of eye movements27, 28. So, the critical aspect in the current study was to see how the AD patients would behave in these two task conditions. Comparing the performance of optic flow perception between AD patients and healthy controls will then allow us to infer the functionality of corollary discharge signals in AD pathology.
Data analysis
All data analysis was performed with custom-made MatLab scripts (The MathWorks, Natick, MA). To quantitatively characterize the performance of optic flow perception, we fitted a logistic function to the psychometric curve obtained for each subject. The logistic function was formulated as the following:
where x was the FOE angle and f(x) was the proportion of rightward choice. Of the parameters derived from the fitted function, μ represented the FOE angle at which the subjects show equal left/right choice probability and was defined as the point of subjective equality (PSE), also known as the perceptual bias. The scaling factor σ (sigma) was inversely related to the slope of the psychometric function and was an index of perceptual sensitivity.
Results
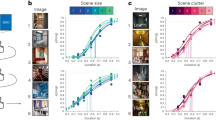
We assessed the behavioral performance of optic flow perception in both pursuit and fixation conditions in AD patients and healthy elderly respectively, as illustrated in Fig. 2A,B. It was clear that the perception of optic flow differed dramatically between AD and elderly groups in the pursuit conditions. Specifically, we found that healthy individuals can accurately judge the direction of self-motion in the presence of pursuit eye movements. This was evident from the similar performances between pursuit and fixation conditions in the elderly group (Fig. 2B), which was consistent with previous studies27, 28. In sharp contrast, eye movements affected the perception of self-motion in AD participants (Fig. 2A). They performed poorly in the pursuit conditions comparing to the fixation condition. They were more likely to perceive a leftward self-motion in trials when the eyes move to the left (triangles), and vice versa for rightward pursuit movements (squares). In other words, self-motion perception in the presence of pursuit movements was biased in the same direction as the shift of FOE in the distorted optic flow. This means, AD patients exhibited disrupted eye movement compensation during optic flow perception.
To quantitatively characterize these effects, we fitted a logistic function to the psychometric data and we did this for each task condition and for each observer, before we average them across participants (see Methods). Of the derived parameters, the absolute value of point of subjective equality (PSE) denotes the magnitude of perceptual bias whereas sigma measures the perceptual sensitivity. Figure 3A,B summarized the cross-participant mean and SEM of PSE and sigma values for each task condition in each group. Firstly, the perceptual biases in the pursuit conditions were significantly larger in AD patients (Mean ± SEM: 8.26 ± 1.14 degree) than those in the control group (0.69 ± 0.08 degree) (Fig. 3A). Unpaired t-test revealed that there was a significant difference between the two groups (p < 0.001). In contrast, the perceptual biases in the fixation condition were both very low (AD: 0.83 ± 0.35 degree; Elderly: 0.24 ± 0.17 degree) and they were not statistically different between groups (unpaired t-test, p > 0.05). Meanwhile, analysis of sigma also showed a similar pattern of results (Fig. 3B). AD patients had significantly larger sigma values than healthy controls in the presence of pursuit eye movements (p = 0.003, unpaired t-test). When there was no pursuit movement (fixation condition), mean sigma became statistically indistinguishable between groups (p > 0.05, unpaired t-test).
To sum it up, our results revealed that AD patients possessed larger biases and weaker sensitivity during the perception of distorted optic flow in the presence of eye movements, comparing to healthy elderly participants. When there was no distortion in the optic flow (fixation condition), self-motion judgments were not different between groups.
Discussion
The current study revealed that AD pathology is associated with disrupted eye movement compensation during the perception of optic flow. We showed that both the sensitivity and bias of optic flow perception were impaired in AD patients in the presence of pursuit eye movement. However, AD patients did not exhibit deficits in the perception of optic flow when there was no eye movement. These findings add to the notion that non-cognitive impairments, such as sensory and motor dysfunctions, are increasingly evident in early-stage AD patients.
Optic flow perception is one commonly used perceptual task in AD research2, 9. Most previous studies focused primarily on the perception of optic flow during ocular fixation (without eye movements), that is, no corollary discharge is involved. For example, studies from Duffy laboratory report that AD patients show elevated optic flow coherence thresholds during passive viewing5, 36. Here we examined optic flow perception in AD patients in the presence of pursuit eye movements as well as during passive viewing (fixation condition). By comparing results across participant groups and task conditions, we can infer if corollary discharge of pursuit compensation during optic flow perception is intact in AD patients. To our knowledge, this is the first study that links corollary discharge dysfunction to AD pathology. We showed that AD patients exhibited impaired pursuit compensation during optic flow perception as comparing to healthy controls. In contrast, the performance of optic flow perception (both bias and selectivity) in the passive viewing condition (fixation trials) did not differ between groups. This ruled out a general decline of low level processing as the explanation for the observed results. Instead, the between-group difference in the optic flow perception was specific to eye movement compensations (pursuit trials). It should be noted that, our results of similar self-motion performance between AD patients and healthy controls during passive viewing are seemingly contradictory with previous studies showing that AD is associated with elevated optic flow threshold5, 36. However, this difference may well be explained by the methodological differences between studies. More precisely, the previous studies varied the coherence levels of optic flow (by adding randomly-moving dots) and took the coherence threshold as a measure of perceptual capability. In contrast, in the current study we did not incorporate visual noise into the optic flow. Instead, we varied the angle of optic flow to obtain the psychometrical performance. To what extent the perceptual performance based on these two different measures are related is still unknown.
There is a possibility that between-group difference of optic flow perception in pursuit conditions was a consequence of differences in the qualities of pursuit movements per se. This explanation is also compatible with the apparent lack of between-group difference in fixation trials. Since we did not conduct simultaneous eye-tracking to monitor gaze positions in parallel to the psychophysical measurements, we cannot completely exclude this possibility. More-carefully designed experiments are needed to better determine the nature of these compensation differences. Another limitation of the current study is that, due to a lack of sufficient variability in MMSE scores, we could not know whether the amounts of pursuit compensation impairment are correlated with the severity of AD pathologies. Future studies should recruit more AD patients with larger MMSE variability (from early to late stages) to explore the correlative relationships between compensation deficits and AD pathology.
The current study has implications on the cortical dysfunctions in AD pathology. Optic flow is generally believed to be processed by the dorsal subdivision of medial superior temporal area (MSTd) and ventral intraparietal area (VIP)37. Neurons in these two areas received not only visual information about the optic flow38,39,40 but also extra-retinal information including signals related to pursuit eye movements41,42,43. Single-unit neurophysiologic studies in monkeys have shown that neural responses in MSTd and VIP are stable despite of distorted retinal optic flow in the presence of eye movements44,45,46, indicating the involvement of these two areas in movement compensation. Our results of impaired pursuit compensation during optic flow perception in AD patients suggest that AD pathology is probably associated with the progressive cell death and/or synaptic loss in these two parietal areas. However, this does not exclude the possibility of structural and functional alterations of cerebral white matter in AD, as the integrity of white matter is also pivotal for normal brain functions47, 48. Further studies with animal models of AD are needed to advance our understanding of its underlying cortical and white matter pathology and to explore the relevance of eye movement compensation deficits in AD.
References
Cronin-Golomb, A., Corkin, S. & Growdon, J. H. Visual dysfunction predicts cognitive deficits in Alzheimer’s disease. Optom Vis Sci 72, 168–176 (1995).
Albers, M. W. et al. At the interface of sensory and motor dysfunctions and Alzheimer’s disease. Alzheimers Dement 11, 70–98, doi:10.1016/j.jalz.2014.04.514 (2015).
Monacelli, A. M., Cushman, L. A., Kavcic, V. & Duffy, C. J. Spatial disorientation in Alzheimer’s disease: the remembrance of things passed. Neurology 61, 1491–1497 (2003).
Tetewsky, S. J. & Duffy, C. J. Visual loss and getting lost in Alzheimer’s disease. Neurology 52, 958–965 (1999).
Kavcic, V., Vaughn, W. & Duffy, C. J. Distinct visual motion processing impairments in aging and Alzheimer’s disease. Vision Res 51, 386–395, doi:10.1016/j.visres.2010.12.004 (2011).
Kavcic, V. & Duffy, C. J. Attentional dynamics and visual perception: mechanisms of spatial disorientation in Alzheimer’s disease. Brain 126, 1173–1181 (2003).
Mapstone, M., Logan, D. & Duffy, C. J. Cue integration for the perception and control of self-movement in ageing and Alzheimer’s disease. Brain 129, 2931–2944, doi:10.1093/brain/awl201 (2006).
Prvulovic, D. et al. Functional imaging of visuospatial processing in Alzheimer’s disease. NeuroImage 17, 1403–1414 (2002).
von Gunten, A., Bouras, C., Kovari, E., Giannakopoulos, P. & Hof, P. R. Neural substrates of cognitive and behavioral deficits in atypical Alzheimer’s disease. Brain Res Rev 51, 176–211, doi:10.1016/j.brainresrev.2005.11.003 (2006).
Thulborn, K. R., Martin, C. & Voyvodic, J. T. Functional MR imaging using a visually guided saccade paradigm for comparing activation patterns in patients with probable Alzheimer’s disease and in cognitively able elderly volunteers. AJNR. American journal of neuroradiology 21, 524–531 (2000).
Fernandez, R., Kavcic, V. & Duffy, C. J. Neurophysiologic analyses of low- and high-level visual processing in Alzheimer disease. Neurology 68, 2066–2076, doi:10.1212/01.wnl.0000264873.62313.81 (2007).
Thiyagesh, S. N. et al. The neural basis of visuospatial perception in Alzheimer’s disease and healthy elderly comparison subjects: an fMRI study. Psychiatry Res 172, 109–116, doi:10.1016/j.pscychresns.2008.11.002 (2009).
Festa, E. K. et al. Neocortical disconnectivity disrupts sensory integration in Alzheimer’s disease. Neuropsychology 19, 728–738, doi:10.1037/0894-4105.19.6.728 (2005).
Wu, Y. et al. Distinct Changes in Functional Connectivity in Posteromedial Cortex Subregions during the Progress of Alzheimer’s Disease. Front Neuroanat 10, 41, doi:10.3389/fnana.2016.00041 (2016).
Helmholtz, H. Handbuck der physiologischen Optic. Vol. 3 (Voss, 1910).
Sperry, R. W. Neural Basis of the Spontaneous Optokinetic Response Produced by Visual Inversion. J Comp Physiol Psych 43, 482–489, doi:10.1037/H0055479 (1950).
Shadmehr, R., Smith, M. A. & Krakauer, J. W. Error correction, sensory prediction, and adaptation in motor control. Annual review of neuroscience 33, 89–108, doi:10.1146/annurev-neuro-060909-153135 (2010).
Kuang, S., Morel, P. & Gail, A. Planning Movements in Visual and Physical Space in Monkey Posterior Parietal Cortex. Cereb Cortex 26, 731–747, doi:10.1093/cercor/bhu312 (2016).
Kuang, S. & Gail, A. When adaptive control fails: Slow recovery of reduced rapid online control during reaching under reversed vision. Vision Res 110, 155–165, doi:10.1016/j.visres.2014.08.021 (2015).
Jeannerod, M., Kennedy, H. & Magnin, M. Corollary Discharge - Its Possible Implications in Visual and Oculomotor Interactions. Neuropsychologia 17, 241–258, doi:10.1016/0028-3932(79)90014-9 (1979).
Wurtz, R. H., Joiner, W. M. & Berman, R. A. Neuronal mechanisms for visual stability: progress and problems. Philosophical transactions of the Royal Society of London. Series B, Biological sciences 366, 492–503, doi:10.1098/rstb.2010.0186 (2011).
Kuang, S. Two Polarities of Attention in Social Contexts: From Attending-to-Others to Attending-to-Self. Front Psychol 7, 63, doi:10.3389/fpsyg.2016.00063 (2016).
Ford, J. M. & Mathalon, D. H. Corollary discharge dysfunction in schizophrenia: can it explain auditory hallucinations? International journal of psychophysiology: official journal of the International Organization of Psychophysiology 58, 179–189, doi:10.1016/j.ijpsycho.2005.01.014 (2005).
Kuang, S. Toward a Unified Social Motor Cognition Theory of Understanding Mirror-Touch Synaesthesia. Front Hum Neurosci 10, 246, doi:10.3389/fnhum.2016.00246 (2016).
Thakkar, K. N., Schall, J. D., Heckers, S. & Park, S. Disrupted Saccadic Corollary Discharge in Schizophrenia. J Neurosci 35, 9935–9945, doi:10.1523/JNEUROSCI.0473-15.2015 (2015).
Longuet-Higgins, H. C. & Prazdny, K. The interpretation of a moving retinal image. Proc.R.Soc.Lond B Biol.Sci. 208, 385–397 (1980).
Warren, W. H. & Hannon, D. J. Eye movements and optical flow. J. Opt. Soc. Am. A 7, 160–169 (1990).
Royden, C. S., Banks, M. S. & Crowell, J. A. The perception of heading during eye movements. Nature 360, 583–585 (1992).
Crowell, J. A., Banks, M. S., Shenoy, K. V. & Andersen, R. A. Visual self-motion perception during head turns. Nature neuroscience 1, 732–737, doi:10.1038/3732 (1998).
Shenoy, K. V., Crowell, J. A. & Andersen, R. A. Pursuit speed compensation in cortical area MSTd. Journal of Neurophysiology 88, 2630–2647 (2002).
Wertheim, A. H. Motion Perception during Self-Motion - the Direct Versus Inferential Controversy Revisited. Behav Brain Sci 17, 293–311 (1994).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34, 939–944 (1984).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12, 189–198 (1975).
Brainard, D. H. The Psychophysics Toolbox. Spat.Vis 10, 433–436 (1997).
Pelli, D. G. The VideoToolbox software for visual psychophysics: transforming numbers into movies. Spat.Vis. 10, 437–442 (1997).
Velarde, C., Perelstein, E., Ressmann, W. & Duffy, C. J. Independent deficits of visual word and motion processing in aging and early Alzheimer’s disease. J Alzheimers Dis 31, 613–621, doi:10.3233/JAD-2012-112201 (2012).
Britten, K. H. Mechanisms of self-motion perception. Annual review of neuroscience 31, 389–410 (2008).
Duffy, C. J. & Wurtz, R. H. Sensitivity of MST neurons to optic flow stimuli. I. A continuum of response selectivity to large-field stimuli. Journal of neurophysiology 65, (1329–1345 (1991).
Bremmer, F., Duhamel, J. R., Ben, H. S. & Graf, W. Heading encoding in the macaque ventral intraparietal area (VIP). European Journal of Neuroscience 16, 1554–1568 (2002).
Britten, K. H. & Van Wezel, R. J. Area MST and heading perception in macaque monkeys. Cerebral cortex 12, 692–701 (2002).
Komatsu, H. & Wurtz, R. H. Relation of cortical areas MT and MST to pursuit eye movements. I. Localization and visual properties of neurons. Journal of Neurophysiology 60, 580–603 (1988).
Newsome, W. T., Wurtz, R. H. & Komatsu, H. Relation of cortical areas MT and MST to pursuit eye movements. II. Differentiation of retinal from extraretinal inputs. Journal of neurophysiology 60, 604–620 (1988).
Schlack, A., Hoffmann, K. P. & Bremmer, F. Selectivity of macaque ventral intraparietal area (area VIP) for smooth pursuit eye movements. J.Physiol 551, 551–561 (2003).
Bradley, D. C., Maxwell, M., Andersen, R. A., Banks, M. S. & Shenoy, K. V. Mechanisms of heading perception in primate visual cortex. Science 273, 1544–1547 (1996).
Shenoy, K. V., Bradley, D. C. & Andersen, R. A. Influence of gaze rotation on the visual response of primate MSTd neurons. Journal of Neurophysiology 81, 2764–2786 (1999).
Lee, B., Pesaran, B. & Andersen, R. A. Translation speed compensation in the dorsal aspect of the medial superior temporal area. Journal of Neuroscience 27, 2582–2591 (2007).
Kuang, S. Is reaction time an index of white matter connectivity during training? Cogn Neurosci 8, 126–128, doi:10.1080/17588928.2016.1205575 (2017).
Salat, D. H. et al. Regional white matter volume differences in nondemented aging and Alzheimer’s disease. NeuroImage 44, 1247–1258, doi:10.1016/j.neuroimage.2008.10.030 (2009).
Acknowledgements
This work was supported by the National Natural Science Foundation of Shandong Province, China (No: ZR2015HQ023).
Author information
Authors and Affiliations
Contributions
T.C. and W.Y. conceived and designed the experiment; J.W., X.G. and X.Z. collected data and performed data analysis; J.W., T.C., W.Y. wrote the first draft of the manuscript. All authors have discussed, reviewed, and approved the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, J., Guo, X., Zhuang, X. et al. Disrupted pursuit compensation during self-motion perception in early Alzheimer’s disease. Sci Rep 7, 4049 (2017). https://doi.org/10.1038/s41598-017-04377-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04377-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.