Abstract
Osteoradionecrosis of the mandible (ORNM) is one of the most dreaded complications of radiotherapy. The poor healing capacity of soft tissue after radiation may lead to surgical failure. The current study was designed to identify prognostic factors for postoperative infection (PPI) and propose corresponding prophylaxis and intervention protocols. A retrospective study was conducted concerning ORNM patients from 2000 to 2015. A risk-stratification score and nomogram model were established to predict the risk of PPI. A total of 257 patients were analyzed, and the total incidence of PPI was 23.3% (60/257). In multiple logistic regression analysis, radiation dose \(\geqslant \)80 Gy (versus <80 Gy, OR = 2.044, P = 0.035, 95% CI: 1.05–3.979), bilateral ORNM (versus unilateral, OR = 4.120, P = 0.006, 95% CI: 1.501–11.307), skin fistula (versus none, OR = 3.078, P = 0.040, 95% CI: 1.05–9.023), and implant utilization (versus none, OR = 2.115, P = 0.020, 95% CI: 1.125–3.976) were significantly associated with PPI. The susceptibility to PPI in patients with risk-stratification scores of 14–22 was 2.833 times that of patients with scores of 7–13, and 7.585 times that of cases defined as scores of 0–6. The discrimination capability of the nomogram model was estimated using a ROC curve with an AUC of 0.708, revealing potentially useful predictive abilities. In conclusion, current risk-stratification scores and nomogram models effectively predicted the risk of PPI in ORNM patients.
Similar content being viewed by others
Introduction
Radiotherapy is common among the multidisciplinary therapeutics used to treat head and neck cancers. Osteoradionecrosis of the mandible (ORNM) is a serious, radiation-induced complication characterized by sequestra or devitalized bone formations with soft tissue destruction1, 2. Without medical intervention, this disease can develop into skin fistulae, bone exposures, mouth opening limitations, and pathological fractures, imposing tremendous psychological and physical trauma on patients. Therapeutic methods, including conservative treatment, sequestrectomy, segmental resection and hemimandibulectomy with simultaneous reconstruction, are selected based on the severity of ORNM3,4,5. Because of radiation damage to soft tissue (fibrosis and scar) and microcirculation, ORNM patients experience a higher risk of postoperative morbidities, such as delayed wound healing, dehiscence, swelling, fistula and infection, relative to non-pre-radiated surgeries6, 7. Several factors, including mucositis, decreased salivary secretion, mucosal fibrosis and poor oral hygiene, may lead to wound infection and subsequent orocutaneous fistula; these are formidable complications for surgeons to address during the perioperative period7. Once an infected fistula evolves into titanium plate extrusion or even bone exposure, plate removal or bone resection combined with vascularized flap coverage should be performed to control this relapse8. Furthermore, postoperative infection (PPI) may facilitate disease progression in patients who have undergone surgery for ORNM, even if a radical resection was performed. Considering these challenges, we set postoperative infection of ORNM as the primary outcome; the objectives of the study are to establish a predictive model for susceptibility to PPI and to propose precautionary protocols. To our knowledge, our study has the largest sample size of all studies examining prognostic parameters for PPI of ORNM. Based on this study, we hope to provide meaningful recommendations for the treatment of ORNM.
Methods
Study design and sample
To address this clinical issue, we designed and implemented a retrospective study. We used the files of ORNM patients who received treatment at the Department of Oral Maxillofacial & Head and Neck Oncology between 2000 and 2015. We only conducted our study on patients who met the following criteria: (1) patients diagnosed with ORNM with no evidence of primary tumor recurrence; (2) patients who received surgical treatment, including sequester, sequestrectomy, segmental or partial resection, hemimandibulevtomy; (3) patients who received treatments in single institution; (4) patients who did not die during perioperative period (beginning at the time of hospital admission and ending at patient discharge); and (5) patients with complete treatment records and follow-up information. We confirmed that all methods were carried out in accordance with study guidelines and regulations; all experimental protocols were approved by the Ethic Committee of Shanghai 9th People’s Hospital, and informed consent was obtained from all subjects.
Study variables and estimation model
The demographic and comorbidity features included age at surgical treatment, gender, smoking, alcohol consumption and systemic disease; ORNM-related characteristics before surgery included primary tumor, mandibular surgery prior to radiotherapy, radiotherapy (the dose and the time interval between radiation completion and the onset of ORNM, which was counted by month), tooth extraction and hyperbaric oxygen therapy; and ORNM clinical manifestations included morphological changes, spontaneous pain, numbness, mucosal defects, skin fistulae, orocutaneous fistulae, bone exposure, titanium plate exposure, purulent discharge, limitation of mouth opening (categorized as mild, moderate, severe or trismus) and pathological fracture. Particular emphasis was placed on ORNM classification and stage1. Data regarding treatment consisted of different surgical therapies and titanium plate utilization. All aforementioned variables were defined as primary predictive factors, and the outcome variable was postoperative infection. Follow-up began at the time-point when patients finished surgical treatment to three months after surgery. An association study of primary predictive factors with the outcome variable was performed to filter the factors with predictive roles; these factors were then recombined to establish a risk-stratification score and nomogram model to predict the PPI of ORNM.
Statistical analysis
Sociodemographic and clinical variables were analyzed using descriptive statistics. The association between primary predictive factors and PPI was tested in a univariate analysis (Chi-square tests, P < 0.05 was deemed statistically significant). Those factors with P < 0.05 were then entered into multiple logistic regression analysis to eliminate the reciprocal influence and determine the final predictive role. P value, odds ratio and 95% confidence intervals were recorded. For the risk-stratification score, the score was assigned to predictors filtered from multivariate analysis according to the regression coefficient obtained from the logistic model. This score was subsequently analyzed in Chi-square tests to clarify its predictive role of PPI. For better analysis, we also established a nomogram model to show the odds ratio of patients with different risks and scores. We further assessed the model’s performance via discrimination (ROC curve, area under curve, AUC), and model fitness was tested using bias-corrected calibration curve with 1000-sample bootstrapping for the prediction of PPI. Bootstrapping was used as internal validation. Statistical analyses were performed with SPSS software (version 21.0; SPSS, Chicago, IL) and R version of 3.3.1 (http://www.rproject.org).
Results
Clinical characteristics of study cohort
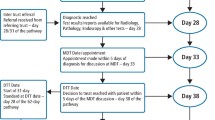
Twenty-four patients were excluded according to the inclusion criteria, and a total of 257 patients were analyzed in the study (Fig. 1). Three patients died during the hospital-stay period: one as the result of an electrolyte disturbance, one as the result of a carotid hemorrhage, and one as the result of heart disease. Thus, we failed to determine the PPI information within the first three months after surgical treatment for their deaths during the hospital-stay period. The age distribution ranged from 24 to 92 years (mean: 55.7, median: 55), with 170 (66.1%) patients younger than 60 years old. The group was mostly composed of male patients (n = 202, 78.6%). Other demographical characteristics are summarized in Table 1.
Among 257 cases, the most common primary tumor was nasopharyngeal carcinoma (n = 96, 37.4%), followed by tongue cancer (n = 49, 19.1%) and buccal malignancy (n = 18, 7.0%) (Table 2). Among patients receiving extended resections of malignant neoplasms, 54 cases (21.0%) underwent simultaneous marginal resections of the mandible, and an additional 11 patients (4.3%) received segmental resections. Subsequent X-ray radiation, ranging from 35 to 144 Gy (mean: 75.35; median: 70), was performed in all patients (Fig. 2A).
Clinical presentations and staging of ORNM
The time interval between radiotherapy completion and the onset of ORNM varied from 1 month to 456 months (mean: 46.9; median: 36); cases diagnosed within 36 months accounted for 60.3% (n = 155) (Fig. 2B). With regards to the lesion site of the mandible, most cases (n = 237, 92.2%) were found unilaterally in the mandible (116 in left and 121 in right), and the remaining 20 patients were diagnosed with bilateral ORNM. From anatomic analysis, bone destruction mostly occurred in the mandibular body combined with the angle and the ramus (n = 129, 50.2%) (Fig. 3).
ORNM in its early stage is easily overlooked because it is symptomless and shows little change in both radiographic and clinical examinations. The patients sought outpatient service after experiencing obvious symptoms or symptoms beyond their tolerance, such as morphological changes, spontaneous pain, numbness, mucosal defects, skin fistulae, orocutaneous fistulae, bone or titanium plate exposure, pyorrhea, and pathological fracture. Detailed information on this topic is provided in Fig. 4. The majority of patients (n = 240, 93.4%) complained of limitations in mouth opening; this limitation was mild in 19 patients, moderate in 74 patients, severe in 140 patients, and trismus in 7 patients. All patients were categorized into variable stages per the staging system mentioned above. Most of the cases were classified as Stage II (178/257, 69.3%), followed by Stage III (55/257, 21.4%) and Stage I (24/257, 9.3%).
Surgical treatments and postoperative infection
Surgery was performed on all cases in our study, and the resection margin adhered to the criteria for the appearance of well-vascularized and infection-free bone. Twenty-nine patients (11.3%, Grade I = 24, Grade II = 5) were treated with curettage/sequestrectomy and primary closure of the wound. The remaining 228 patients (88.7%; Grade II = 171, Grade III = 55) received extended resection; of these, 156 patients (68.4%) underwent simultaneous flap tissue transfer: 71 patients from the pectoralis major myocutaneous flap, 63 from the fibular flap and 11 from the anterolateral thigh flap. Titanium plates were used in 106 patients (41.2%) to maintain the anatomic arch of the mandible after segmental resection or to fix the binding interface between the remaining mandible and bone graft (Table 3).
During the postsurgical period (3 months), infection was found in 60 patients with an incidence of 23.3% and was categorized into five types: 1) swelling and pyometra in 15 patients (25%), who were treated with conservative therapeutics consisting of debridement (removal of the necrotic soft tissues), daily dressing changes that continued for about two weeks, and antibiotic prescription, which achieved good outcomes; 2) soft tissue split with infection in 13 patients (21.7%), of whom 10 patients received conservative therapeutics, and the remaining three patients underwent extended resections in conjunction with flap re-coverage; 3) fistula formation with titanium plate exposure (n = 16, 26.7%) where removal of titanium plates was adequate for 12 patients, and the other four patients needed extra flap coverage; 4) fistula formation with bone exposure in seven patients (11.7%), five of whom received curettage of the necrotic bone and subsequent conservative treatment, and the remaining two patients received bone ablation and flap reconstruction; and 5) partial necrosis of the vascularized flap with infection (n = 9, 15%), for which seven patients received conservative treatment, and the remaining two patients needed new flap coverage (Table 4). All infection cases were treated with surgical intervention.
Predictors for postoperative infection in univariate and logistic analysis
A total of 257 patients were included in the predictive analysis. All predictive factors were analyzed to identify their correlation with PPI. In the univariate analysis, six factors demonstrated a significant association with PPI with p-values less than 0.05 (Table 5). Other factors failed to show a statistically significant association with PPI in the chi-square test. When these six factors were further entered into the logistic model, only four variables maintained their predictive role in multiple logistic regression analysis. The patients who received a radiation dose \(\geqslant \)80 Gy were 2.044 times more likely to develop PPI than those who received a dose <80 Gy (p = 0.035, 95% CI: 1.050–3.979). Patients diagnosed with bilateral ORNM were 4.120 times more likely to develop PPI than those with unilateral ORNM (p = 0.006, 95% CI: 1.501–11.307). The odds of susceptibility to PPI in patients with a skin fistula were 3.078 times the odds of cases without infection (P = 0.040, 95% CI: 1.023–9.203). The risk of PPI increased abruptly with an OR of 2.115 (P = 0.020, 95% CI: 1.125–3.976) when an implant (titanium plate) was used for fixation during the operation (Table 6).
Nomogram model establishment and its performance
Based on the results obtained from multiple logistic regression analysis, a nomogram model was established to predict PPI in ORNM patients. A score was assigned to the four identified factors according to their regression coefficients (Table 6). The score sum of each predictor was calculated for each patient to form a risk-stratification score that was then separated into three categories: 1) 0–6; 2) 7–13; and 3) 14–22. We found that PPI risk increased with the stratification score. The susceptibility to PPI in patients with scores of 14–22 was 2.833 times that of patients with scores of 7–13 and 7.585 times that of patients with scores of 0–6 (Table 7). Figure 5 outlines the nomogram model in which the total points and corresponding risk of every patient were calculated in a more convenient way. We plotted the ROC curve to estimate the discriminative ability of this nomogram model depending on the AUC with an area of 0.708 (95% CI: 0.646–0.798, and the p-value of the hypothesis test of the AUC of 0.5 was <0.001), which indicated that the probability that a patient with PPI had a higher score than a patient without PPI was 70.8%, showing the power of this predictive model (Fig. 6). The calibration curve also revealed strong goodness of fit (Fig. 7).
Discussion
Mandibular osteoradionecrosis is a radiation-induced late toxicity that is among the most terrible side effects affecting the quality of life of survivors of head and neck cancers. Thus far, most investigations have dealt with the modality of ORNM therapeutics and risk factors related to the causation of ORNM1, 3,4,5,6, 9, 10. Few studies have probed the postoperative complications of ORNM7, 11,12,13,14, and almost no literature has systemically identified the prognostic factors for PPI or proposed corresponding prophylaxis and intervention protocols. This imbalance in research calls for in-depth evaluation of PPI to standardize therapeutics and minimize postoperative morbidities. Our sample size of 257 patients is the largest of any ORNM investigation to date11, 15. Through data review and analysis, we found that four factors (radiation dose, skin fistula, unilateral/bilateral involvement, and implant utilization) were predictors for PPI of ORNM. Other factors failed to demonstrate a statistical association with PPI. Based on these findings, we established a risk-stratification score and nomogram model to predict the risk of PPI occurrence; these tools can be used to improve clinical evaluation. The nomogram model was evaluated for discrimination capability and found to have an AUC of 0.708. Previous studies have reported a PPI incidence ranging from 11.1% to 22.2% in reconstruction of ORNM with a vascularized flap11, 14, 16, 17. In the current study, the total incidence of PPI was 23.3%, and in patients reconstructed with a free flap, it was 21.7%, which is in accordance with other studies.
In our study, the average radiation dose was 75.35 Gy, which is comparable with the mean dose that was used in previous studies17,18,19. This high dosage may be attributed to the high proportion of patients with nasopharyngeal carcinoma (96/257, 37.4%), who require higher doses for primary control or local relapse. It was common for a patient to receive a cumulative dose higher than 100 Gy when malignancy was recurrent4. Another situation was when a patient had undergone prior surgery with radiotherapy at another institution but was referred to our department and diagnosed with tumor recurrence, thus a second course of irradiation was inevitable. For the aforementioned reasons, we set the cut-off for the radiation dose at 80 Gy and performed further analysis. Controversy persists among investigations as to whether the radiation dose is directly proportional to the development or severity of ORNM18, 20,21,22; nevertheless, no coherent conclusion has been drawn because the distinct grading system used in previous investigations made comparison baseless and meaningless. Mucke et al.12 failed to prove the predictive role of the radiation dose on postsurgical infection. In the current study, we demonstrated that the radiation dose was statistically associated with PPI in both univariate and multiple logistic regression analyses. Radiation damage to skin and connective tissue that is marked by fibrosis reduces vascularity and ultimately causes necrosis, as has been proven through histological analysis23. Radiation damages the immunological barrier of the skin and its self-renewing property, resulting in hypovascularized tissue that is susceptible to trauma or infection24.
A skin fistula is one of the most typical symptoms of ORNM. During the development of ORNM, necrotic bone may suffer from infection, and irradiated soft tissue may easily split, thus forming a skin fistula with infection and hindering the healing capability of surrounding tissue even after an extended bone resection is performed7. In the current study, the presence of a skin fistula prior to surgical treatment was a major risk factor for PPI in both univariate and multiple logistic regression analyses. However, mucosal defects failed to show the same effect, and orocutaneous fistulae demonstrated significance in the univariate analysis but not in the multiple logistic regression analysis. These results indicate a decisive effect of skin fistulae on the significance of orocutaneous fistulae in the chi-square test, but that effect was absent in multivariate analysis when all factors were considered. Skin fistulae have a worse microenvironment and lower resistance after radiation than skin with an intact barrier, and this chronically infected tissue may increase the propensity of PPI24. Complications from infection are usually associated with necrotic wound tissue (ulcers of the mucosa, skin fistulae) before surgery11.
Bilateral ORNM may result from extensive irradiation covering both sides of the mandible. In our cases, ORNM with bilateral involvement accounted for 7.8% of cases (20/257), and these patients were more prone to suffer from PPI than those with unilateral ORNM (OR = 4.12, p = 0.006, 95% CI: 1.501–11.307). This correlation was not analyzed in the study of Mucke et al.12, who attempted to find prognostic factors for PPI. Extensive irradiation imposed damage not only on bone tissue but also on the surrounding soft tissue and vascular system. The metabolism and self-refreshing capability of these irradiated soft tissues were significantly depressed, with the consequence of lower resistance to infection24. In the current study, little evidence was gathered regarding the predictive role of the severity of ORNM on the onset of PPI; the result was similar to the findings of Mucke et al.12. However, the staging system used in our cases was not the same, indicating that even when different clinical staging systems were evaluated, PPI had no significant correlation with the severity of ORNM. It is easier to control necrotic bone than to address the extensive destruction of irradiated soft tissue. Postoperative infection may directly correlate with soft tissue damage rather than bony destruction.
Reconstruction plates are commonly used to stabilize both sides of the remaining mandible or bind the interface between the mandible and bone graft. The disadvantage of this biomaterial is that postsurgical plate exposure increases skin fistula formation, with an incidence of 7.1% to 46.1%14, 25. The ratio in the current study was 15.1% (16/106), and we found that reconstruction plate utilization was a predictor of PPI in both univariate and multiple logistic regression analyses. The reasons for this result are as follows: 1) rejection of the titanium plate; 2) shrinkage of the grafted flap and local movement of the residual mandible rendering plate tortuosity25; 3) pressure on the overlying soft tissue caused by a plate in a wound during contraction26; and 4) sites where screws were fixed in bone tissue within prior radiation fields, where the metabolism of the bone was lower than that in bone that did not receive preceding radiotherapy27.
Based on our predictive model and the manifestations of PPI, we proposed prophylaxis protocols as follows. (1) Preoperative assessment (risk-stratification score and nomogram model) of the hazard ratio for PPI is needed, thus preparing rigorous operative procedures and postoperative care. (2) Thorough excision of necrotic/infected soft tissues is needed, especially for skin or orocutaneous fistula and reconstruction defects with sufficient vascularized flap coverage to reduce the suture tension of binding interfaces between the flap and the remaining tissue. It is more difficult to define the excision margin of soft tissue than of necrotic bone. Under these circumstances, extensive resections of irradiated soft tissue should be advocated even if a large flap will be needed to recover the defect28. Inadequate debridement of residual infected tissue may cause PPI and even progression of ORNM. Suturing the flap without retortion and decreased tension was crucial during the healing process because this measure can prevent the wound from splitting or dehiscing and can protect it from further plate or bone exposure25. (3) Functional evaluation of recipient vessels is important, guaranteeing a high survival rate of the free flap and good conjunction between the flap and the remaining soft tissue. Radiation damnification of vessels manifests in two ways: (a) pathological changes, including endothelium destruction, adventitial fibrosis and vasa vasorum damage that lead to tissue hypoxia and atherosclerosis; (b) physiological changes that result from surrounding tissue fibrosis and smooth muscle vasoconstriction, leading to a decrease in blood flow and an increase in blood pressure29. It is of pivotal importance to evaluate blood flow and vascular structure in a “frozen” neck through radiographic techniques (Computed Tomographic Angiography or Doppler) to select ideal recipient vessels and furnish an ample blood supply to ensure flap survival. (4) We advocate the use of the mini-plate system to lessen plate-related complications. In a retrospective study of 544 patients with fibular grafts combined with mini-plate fixation, Liu et al.30 demonstrated that the exposure rate was 1.5%, and the total incidence of complications was 10.3%; these are much lower rates than those obtained using a reconstruction plate. (5) Exhaustive debridement of necrotic bone should be performed until bleeding bone is observed. In most cases, bone necrosis was inextricably linked with infection31. To be specific, bone necrosis may lead to infection of surrounding tissue, and secondary infection may facilitate the progression of necrosis. For this reason, extended resections should be carried out to prevent ORNM from continuing and to minimize the risk of PPI. (6) Prophylactic use of antibiotics during postoperative care is needed. Intravenous antibiotics with broad spectra were used in all cases, similar to the study by Chen et al.11. Although no evidence exists concerning the preventive role of antibiotics on the onset of PPI of ORNM, we recommended that the prophylactic use of antibiotics should be advocated for the following reasons: (a) most cases include infected wounds; and (b) irradiated tissue holds a lower capacity for spontaneous healing and a lower resistance to destructive stimuli. In addition, maintaining oral hygiene and using mouthwash with an antibiotic ingredient should also be advocated.
Different modalities should be used to address PPI, depending on its variable severity. There was no statistical association between different therapeutics (resection with reconstruction versus resection only, pedicle flap versus free flap, bone flap versus soft flap), and PPI. Chen et al.11 hold the view that most PPI following flap reconstruction is mild and heals well through treatment with intravenous antibiotics. In the current study, conservative therapy including local debridement, dressing changes and antibiotic prescription was performed in 53.3% (32/60) of cases and achieved positive outcomes. A previous study reported a plate removal rate of 21% and unsatisfactory cosmetic outcomes32. In our cases, the patients with plate exposure needing surgical removal accounted for 15.1% (16/106), and most of these patients (12/16) healed spontaneously following plate removal and local wound care; this result was in accordance with the treatment of plate problems in the study by Blackwell et al.26. However, contour deformity following primary wound closure for plate removal may be far from ideal, and primary wound closures were sometimes difficult as a result of large soft tissue defects and high tension. Previous studies8 have suggested that vascularized flaps should be used in the closure of large oropharyngocutaneous fistulae located in the submandibular region. For these reasons, we performed free flap coverage in four cases with plate exposure. The same situation was found in three cases that were diagnosed with soft tissue splits with infection, where two patients had local bone necrosis and two patients had partial necrosis of the flap. We concluded that, in patients with mild infections, conservative treatment should be sufficient. For patients with plate rejection and bone necrosis, modalities entailing the removal of the plate and necrotic bone combined with dressing changes and intravenous antibiotics should be advocated. More seriously, vascularized flaps should be used to reconstruct large soft tissue defects following plate removal, necrotic bone debridement or partial necrosis of the flap.
The sample size of 257 in the current study is the largest in the literature concerning ORNM. This larger sample size made the statistical results more powerful and reliable. Therapeutic methods showed better coherence in single institution investigation, thus lessening the treatment bias. There were also several limitations in current study. First, it is difficult to entirely eliminate selection and document bias in a retrospective study, and unknown confounders may affect the statistical results. Second, 24 patients (including 3 patients died during hospital stay period) were excluded due to exclusion criteria, and missing data may cause bias. Third, the results from single institutions may be less generalizable than results from multicenter investigations. Finally, the nomogram model and risk-stratification score should be tested further in prospective studies. Fourth, the selection of predictors for the model in current study was based on statistical significance testing for bivariate association, and this may miss predictors that can improve the performance of multivariable model. Fifth, we used observational data as the basis for clinical recommendations for ORNM treatment, even though observational data by themselves do not provide a sufficient basis for causal inferences. Hence, readers should view these proposed recommendations on the basis of their own expert judgment.
References
He, Y. et al. Retrospective analysis of osteoradionecrosis of the mandible: proposing a novel clinical classification and staging system. Int J Oral Maxillofac Surg. 44, 1547–1557 (2015).
Owosho, A. A. et al. Radiographic osteoradionecrosis of the jaw with intact mucosa: Proposal of clinical guidelines for early identification of this condition. Oral Oncol. 51, e93–96 (2015).
Rice, N., Polyzois, I., Ekanayake, K., Omer, O. & Stassen, L. F. The management of osteoradionecrosis of the jaws–a review. Surgeon. 13, 101–109 (2015).
Notani, K. et al. Management of mandibular osteoradionecrosis corresponding to the severity of osteoradionecrosis and the method of radiotherapy. Head Neck. 25, 181–186 (2003).
Chrcanovic, B. R., Reher, P., Sousa, A. A. & Harris, M. Osteoradionecrosis of the jaws–a current overview–Part 2: dental management and therapeutic options for treatment. Oral Maxillofac Surg. 14, 81–95 (2010).
Nolen, D. et al. Comparison of complications in free flap reconstruction for osteoradionecrosis in patients with or without hyperbaric oxygen therapy. Head Neck. 36, 1701–1704 (2014).
Zhang, D. M. et al. Role of Negative-Pressure Wound Therapy in the Management of Submandibular Fistula After Reconstruction for Osteoradionecrosis. J Oral Maxillofac Surg. 74, 401–405 (2016).
You, H. Y., Chen, W. L. & Zhang, D. M. Closure of large oropharyngocutaneous fistulas using a folded extensive supraclavicular fasciocutaneous island flap. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology. 25, 310–313 (2013).
Nabil, S. & Samman, N. Risk factors for osteoradionecrosis after head and neck radiation: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 113, 54–69 (2012).
Cheriex, K. C., Nijhuis, T. H. & Mureau, M. A. Osteoradionecrosis of the jaws: a review of conservative and surgical treatment options. J Reconstr Microsurg. 29, 69–75 (2013).
Chen, S. H. et al. Reconstruction for osteoradionecrosis of the mandible: superiority of free iliac bone flap to fibula flap in postoperative infection and healing. Ann Plast Surg. 73, S18–26 (2014).
Mücke, T. et al. Surgical outcome and prognostic factors after treatment of osteoradionecrosis of the jaws. J Cancer Res Clin Oncol. 139, 389–394 (2013).
Lyons, A. J., Nixon, I., Papadopoulou, D. & Crichton, S. Can we predict which patients are likely to develop severe complications following reconstruction for osteoradionecrosis? Br J Oral Maxillofac Surg. 51, 707–713 (2013).
Lee, M., Chin, R. Y., Eslick, G. D., Sritharan, N. & Paramaesvaran, S. Outcomes of microvascular free flap reconstruction for mandibular osteoradionecrosis: A systematic review. J Craniomaxillofac Surg. 43, 2026–2033 (2015).
Raguse, J. D. et al. Patient and treatment-related risk factors for osteoradionecrosis of the jaw in patients with head and neck cancer. Oral Surg Oral Med Oral Pathol Oral Radiol. 121, 215–221 (2016).
Alam, D. S., Nuara, M. & Christian, J. Analysis of outcomes of vascularized flap reconstruction in patients with advanced mandibular osteoradionecrosis. Otolaryngol Head Neck Surg. 141, 196–201 (2009).
Baumann, D. P., Yu, P., Hanasono, M. M. & Skoracki, R. J. Free flap reconstruction of osteoradionecrosis of the mandible: a 10-year review and defect classification. Head Neck. 33, 800–807 (2011).
Chronopoulos, A. et al. Osteoradionecrosis of the mandible: A ten year single-center retrospective study. J Craniomaxillofac Surg. 43, 837–846 (2015).
Støre, G. & Boysen, M. Mandibular osteoradionecrosis clinical behaviour and diagnostic aspects. Clin Otolaryngol Allied Sci. 25, 378–384 (2000).
Chopra, S. et al. Factors predictive of severity of osteoradionecrosis of the mandible. Head Neck. 33, 1600–1605 (2011).
Glanzmann, C. & Grätz, K. W. Radionecrosis of the mandibular: a retrospective analysis of the incidence and risk factors. Radiother Oncol. 36, 94–100 (1995).
Epstein, J. B., Wong, F. L. & Stevenson-Moore, P. Osteoradionecrosis: clinical experience and a proposal for classification. J Oral Maxillofac Surg. 45, 104–110 (1987).
Marx, E. A new concept in the treatment of osteoradionecrosis. J Oral Maxillofac Surg. 41, 351–357 (1983).
Ryan, J. L. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol. 132, 985–993 (2012).
Wei, F. C. et al. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast Reconstr Surg. 112, 37–42 (2003).
Blackwell, K. E., Buchbinder, D. & Urken, M. L. Lateral mandibular reconstruction using soft-tissue free flaps and plates. Arch Otolaryngol Head Neck Surg. 122, 672–678 (1996).
Jereczek-Fossa, B. A. & Orecchia, R. Radiotherapy-induced mandibular bone complications. Cancer Treat Rev. 28, 65–74 (2002).
Chang, D. W., Oh, H. K., Robb, G. L. & Miller, M. J. Management of advanced mandibular osteoradionecrosis with free flap reconstruction. Head Neck. 23, 830–835 (2001).
Cannady, S. B. et al. Free flap reconstruction for osteoradionecrosis of the jaws outcomes and predictive factors for success. Head Neck. 33, 424–428 (2011).
Liu, S. P., Cai, Z. G., Zhang, J., Zhang, J. G. & Zhang, Y. Stability and complications of miniplates for mandibular reconstruction with a fibular graft: outcomes for 544 patients. Br J Oral Maxillofac Surg. 54, 496–500 (2016).
Hamilton, J. D., Lai, S. Y. & Ginsberg, L. E. Superimposed infection in mandibular osteoradionecrosis: diagnosis and outcomes. J Comput Assist Tomogr. 36, 725–731 (2012).
Santamaria, E., Wei, F. C. & Chen, H. C. Fibula osteoseptocutaneous flap for reconstruction of osteoradionecrosis of the mandible. Plast Reconstr Surg. 101, 921–929 (1998).
Acknowledgements
Doctor Chunyue Ma contributed to the current study through data collection and language editing. This work was supported by the National Natural Science Foundation of China (NSFC: 81271112, 81570949), Shanghai Municipal Education Commission – Gaofeng Clinical Medicine Grant Support (20152222), SMC Rising Star (2013A) Scholar of Shanghai Jiao Tong University.
Author information
Authors and Affiliations
Contributions
Yue He, Zhiyuan Zhang and Weiliu Qiu conceived the study design and contributed in manuscript revision; Zhonghe Wang participated in radiotherapy analysis and data extraction; Zhonglong Liu and Tianguo Dai participated in data collection, statistical analysis and manuscript preparation and writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Z., Dai, T., Wang, Z. et al. Nomogram model to predict postoperative infection after mandibular osteoradionecrosis surgery. Sci Rep 7, 3479 (2017). https://doi.org/10.1038/s41598-017-03672-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03672-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.