Abstract
A multicenter prospective surveillance on dialysis events was carried in 33 dialysis centers in China. Maintenance hemodialysis (HD) outpatients who were dialyzed on the first two days of each month during 2014 were monitored for dialysis events and other infections. During the one-year period, 52,680 patient-months were monitored. Fistula and tunneled or non-tunneled central line were used for 73.70%, 15.70% and 8.85% of vascular access, respectively. There were 773 dialysis events occurred in 671 patients including 589 IV antimicrobial starts, 74 positive blood cultures and 110 local access site infections (LASI). The incidence of dialysis events was 1.47 per 100 patient-months. Among the 74 cases with bloodstream infection (BSI), 38 were access-related BSI (ARB) and there were therefore 148 cases with vascular-related infection (VAI; 38 ARB and 110 LASI). There were 740 cases (1.40 per 100 patient-months) with infections other than BSI and LASI, most (79.19%) of which were respiratory tract infections. For those with dialysis events, there were 425 cases (425/671, 63.34%) admitted to hospital and 12 cases of death (12/671, 1.79%). In conclusion, the surveillance revealed a relatively low incidence of dialysis events and the surveillance may be tailored to target those using central lines in resource-limited settings.
Similar content being viewed by others
Introduction
According to the data that Chinese Hospital Association collected from dialysis centers, the prevalence of end stage renal diseases in China was 79.1 million in 20081. There were about 270,000 registered hemodialysis (HD) patients in China in 2012, compared with only 30,000 patients receiving peritoneal dialysis2. Among HD patients in China, the average age was 53.8 ± 15.3 years old and the male/female ratio was 1.45:13. Cardiovascular diseases (31.0%), stroke (20.3%) and infection (19.9%) were the main causes of death for HD patients in China3. The number of HD patients is estimated to increase rapidly in light of the aging population and the improved access to medical services in recent years2. A total of 3,696 HD centers were registered in China by 20113, most of which were affiliated to hospitals. A set of guidance and standards for preventing infections among HD patients has been established in China since 20104. However, the compliance of the prevention measures varied significantly in HD centers4 and a number of outbreaks of hepatitis C virus infections have been reported in China5.
HD patients are often in immunocompromised status and require frequent or long-term vascular access and they are therefore at risk for developing infections of the vascular access site and bloodstream infections (BSI)6,7,8. BSI and localized infections of the vascular access site cause substantial morbidity and mortality in HD patients9, 10. Both the American Center of Disease Prevention and Control (CDC) and the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) recommend monitoring infections in dialysis patients11, 12. Surveillance has long been recognized as a critical component in the prevention and control of healthcare-associated infections (HAIs)13. However, the infection incidence among HD outpatients in China remains unknown. The National Healthcare Safety Network (NHSN) of the CDC has developed a protocol for surveillance on several types of infection-related adverse events associated with HD called dialysis events14, which has the potential to be adopted or adapted for monitoring patients in China. We performed a prospective multi-center surveillance to investigate the incidence and the spectrum of dialysis events among HD outpatients in China, which is reported here.
Methods
A prospective surveillance for dialysis events was performed for all the maintenance HD outpatients in 33 outpatient HD centers in 11 provinces in China in 2014. These centers voluntarily participated in the surveillance. There were 1,285 HD beds in total for the 33 centers with 10 to 105 beds (median, 35 beds) for each center. These centers were all affiliated to tertiary hospitals with the facility for blood culture and in vitro susceptibility test. Maintenance HD outpatients, including transient patients, were eligible for the surveillance if they received HD on the first two working days of the month. A total of seven dialysis events were reported and definitions for these events developed by the NHSN14 were applied (Table 1). Three types of dialysis events including IV antimicrobial start, positive blood culture, and pus, redness, or increased swelling at the vascular access site (Table 1) were monitored throughout the entire month. Four additional types of events, i.e. BSI, local access site infection (LASI), access-related bloodstream infection (ARB), and vascular access infection (VAI), were determined from the aforementioned three events for these patients. In addition to IV antimicrobial start, oral antimicrobial start that was not a dialysis event of NHSN was recorded in this surveillance as patients may use oral agents without prescriptions in China. Infections of a site other than BSI and LASI such as pneumonia, other respiratory tract infection and urinary tract infection were also monitored using the definitions issued by the Ministry of Health, China (Table 1)15. Of note, for HD patients with a BSI secondary to other infections, they were recorded as having BSI rather than other infections. For HD patients with dialysis events, admission to hospitals and deaths were recorded as the outcome. Other rules defined by NHSN such as the 21 day rule were also applied in the surveillance.
Infection control link nurses in each dialysis center collected data manually from the patient chart using a self-design paper form after training and whether the HD outpatients had dialysis events or not was determined by infection control practitioners together with infection control link nurses in each HD center. The forms were input into database using EpiData (version 3.1)16. An auditor who was responsible for checking the quality and integrity of data and was usually an infection control practitioner other than that collected data was assigned for each participating centers. In addition, a one-month pilot study was performed on December 2013 to test the forms and the procedures before the start of the surveillance. The incidences of dialysis events were stratified by the vascular access type and were expressed by the number per 100 patient-months.
The surveillance was regarded as a performance improvement project and the ethical approval was not sought after consulting the Chinese Hospital Association. Nonetheless, the study protocol was approved by the Ethical Committee of West China Hospital, Sichuan University under a waiver of consent. This surveillance was conducted in accordance with the amended Declaration of Helsinki. Patient data were anonymized prior to analysis and investigators have no access to identifying patient information.
Statistical analysis was performed using the SPSS program (version 18.0; SPSS Inc., Chicago, IL). Percentiles were used to describe the numerical variables that fit a skewed distribution. The overall incidence of dialysis events, rate of hospitalization and mortality rate among the patients with fistula and central lines were compared using a chi square test. A p value below 0.05 was considered statistically significant.
Results
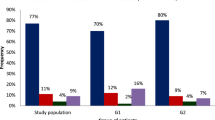
During the one-year surveillance period in 2014, a total of 52,680 HD cases, which include all eligible HD patients, were monitored, corresponding to 52,680 patient months. As for the type of vascular access for HD, fistula, tunneled central line, non-tunneled central line and graft were used for 73.70% (n = 38, 824), 15.70% (n = 8,272), 8.85% (n = 4,662) and 1.04% (n = 548) of the patients, respectively. In addition, 374 (0.71%) patients received direct peripheral venipuncture of the antecubital fossa for dialysis access.
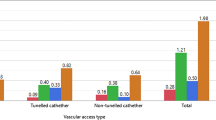
A total of 773 dialysis events occurred in 671 cases and the overall incidence of dialysis events was therefore 1.47 per 100 patient-months (773/52,680) during the surveillance period. Among the dialysis events, there were IV antimicrobial starts in 589 cases (proportion of dialysis events, 589/773, 76.20%; incidence, 1.12 per 100 patient-months), positive blood cultures in 74 (proportion, 9.57%; incidence, 0.14 per 100 patient-months) and pus, redness, or increased swelling at the vascular access site in 110 (proportion, 14.23%; incidence, 0.21 per 100 patient-months; Table 2). Among the 74 cases with BSI (positive blood cultures), 38 were ARB and the remaining 36 cases were either primary BSI without known infection sites (n = 15) or BSI secondary to other infections (n = 21; 12 cases were secondary to pneumonia, 3 to URTI, 2 to skin and sift tissue infections and one to each of LRTI other than pneumonia, liver infection, UTI and gastrointestinal infection. There were 110 cases with LASI (pus, redness, or increased swelling at the vascular access site) and the number of cases with VAI (i.e. either ARB or LASI) was therefore 148. Correspondingly, the incidences of BSI, ARB, LASI and VAI were therefore 0.14, 0.07, 0.21 and 0.28 per 100 patient-months, respectively. Among the 671 cases with dialysis events, 425 cases were admitted to hospital and the corresponding rate of hospitalization was 63.34% (425/671; Table 2). There were 12 death cases and the mortality rate was 1.79% (12/671).
When stratified by the vascular access type, the incidences of dialysis events among patients using fistulas, grafts, tunneled or non-tunneled central lines, and direct puncture were 0.98, 0.91 2.74, 3.37 and 0.80 per 100 patient-months, respectively (Table 2). The dialysis events were significantly more common among patients with central lines (either a tunneled or non-tunneled) compared to those with fistulas (χ2, 263.198; p, 0.000) or graft (χ2, 7.935; p, 0.005). The incidence of dialysis events varied among hospitals from 0.00 to 16.71 per 100 patient-months (Table 3).
Among 74 positive blood cultures, 57 (77.03%) isolates were recovered from patients using central lines and 17 (22.97%) were from patients with fistulas (Table 4). Of the 74 isolates from blood, 64.86% (48/74) were Gram-positive and 35.14% (26/74) were Gram-negative (Table 4). Staphylococcus aureus was most common microorganism, accounting for 37.84% (n = 28) of all isolates recovered. Among S. aureus isolates, 5 (17.86%, 5/28) were methicillin-resistant S. aureus (MRSA).
IV antimicrobial start was the most common type of dialysis events and accounted for 76.20% (589/773) of all events. The majority (87.10%, 513/589) of IV antimicrobial start was used to treat infections other than BSI and LASI such as respiratory or urinary tract infections based on patient chart review. Most patients (72.16%, 425/589) receiving IV antimicrobial agents were admitted to hospital afterwards and the mortality rate of those receiving IV antimicrobial start was 2.04% (12/589). The majority (88.46%, 521/589) of those receiving IV antimicrobial start used a single agent. Cephalosporins, penicillins and fluoroquinolones were the most commonly-used agents with being used in 38.75%, 31.61% and 14.89% of those receiving IV antimicrobial start, respectively.
In addition, 340 HD patients received oral antimicrobial agents instead of IV ones, corresponding to 0.65 per 100 patient-months. Most (66.76%, 227/340) of oral antimicrobial agents were used to treat infections other than BSI and LASI. The hospitalization rate of those receiving oral antimicrobial agents was 20.29% (69/340), which was significantly lower than those receiving IV antimicrobial agents (72.16%; χ2, 232.86; p, 0.000). The mortality rate (0.59%; 2/340) of those receiving oral antimicrobial agents appeared to be much lower than those receiving IV antimicrobial agents (2.04%) but the difference was not statistically significant (χ2, 3.050; p, 0.081), which was likely due to the small sample size of death cases. A single agent was used in almost all (96.47%, 328/340) cases. The most commonly-used agents were cephalosporins, penicillins, macrolides and fluoroquinolones, which accounted for 40.28%, 23.66%, 16.34% and 14.37% of all use, respectively.
There were 740 patients who had an infection other than BSI and LASI with an incidence of 1.40 (740/52,680) per 100 patient-months. The majority (79.19%, 586/740) of these infections were pneumonia or other respiratory tract infections (Table 2). Other relatively common infections included urinary tract infection (n = 38), skin and soft tissue infection (n = 31), gastrointestinal infection (n = 30), and eye, ear, nose, throat, or mouth infection (n = 25).
Discussion
To the best of our knowledge, this is the first surveillance on dialysis events in China. This surveillance generated the baseline information of infections and associated events among HD outpatients in China. In general, to counter dialysis events in China, the awareness among healthcare workers and HD patients should be raised and more efforts on prevention such as establishing a national initiative should be taken. The surveillance did generate useful information to guide the prevention in practice. First, previous studies have shown that vascular access is one of the most important risk factors for infection in HD patients17,18,19 and it has been reported that the use of fistula is associated with less incidence of complications including infections compared to the use of central lines20. This surveillance confirms the use of fistula for vascular access was indeed associated with lower dialysis events, hospitalization and morality than the use of central line. In light of the advantage of using fistula, it has been a core prevention measure for dialysis events. The NKF KDOQI set a goal of using fistula for vascular access in more than 65% of HD patients in 200621 and subsequently the Breakthrough Initiative of Centers for Medicare and Medicaid Services (CMS) increased the goal to 66% by June 200922. Although the >66% target has been achieved in the facilities participating in this study, the use of fistula should be continuously promoted and the use of central line should be minimized. Second, IV antimicrobial start accounted for the majority of dialysis events and was mainly used to treat infections other than VAI, particularly respiratory tract infections including pneumonia. Based on evidence of limited data, the intervention of dialysis events could therefore include measures to prevent respiratory tract infections such as keeping warm during the dialysis23, 24 and more exercises afterwards25, 26. Prospective interventional studies are warranted to investigate the preventability of dialysis events and the efficacy of prevention measures. Third, there were still 31 cases of ARB among those using central lines as the vascular access. Bundles targeting central line associated bloodstream infection (CLABSI) should be implemented to prevent ARB. Fourth, previous studies have identified coagulase-negative staphylococci and S. aureus as the major pathogens causing HD-associated infections6, 7. This surveillance also found that staphylococci, most of which were S. aureus, accounted for almost a half of all microorganisms recovered from blood cultures. However, methicillin-resistant S. aureus (MRSA) only accounted for 17.9% of all S. aureus in this surveillance, while 42% of all S. aureus isolates from dialysis centers participating in the NHSN were MRSA27. Although it still lacks large-scale and multi-center studies to screen the prevalence of MRSA in China, it appears that the carriage of MRSA was low among inpatients in this country based on several small-scale single center surveillances, e.g. 0.5% for inpatients with diabetes28, 1.0% for tumor patients receiving chemotherapy29 and 4.8% for ICU patients30. The relatively low prevalence of ARB due to MRSA among HD patients in this surveillance and the low carriage of MRSA among various patients in previous studies28,29,30 suggest that active screening for MRSA for HD patients may not be a cost-efficient measure in China.
Of note, the incidence of dialysis events was much lower among HD outpatients in China than those in the USA in 200627, in Ireland in 201031 and in Kuwait in 201232 (Table 3). The incidence of BSI as a dialysis event in the USA in 2014 is also available (https://www.cdc.gov/nhsn/pdfs/dialysis/bsi-rate-vat-de-2014.pdf). The BSI incidence in the present surveillance study is still lower than that in USA in 2014 (Table 3). The exact reasons for the lower incidence of dialysis events in Chinese outpatients have not been fully understood. However, comparisons of the dialysis event incidence among different countries are complicated due to differences in the patient characteristics (e.g. underlying diseases, severity of kidney diseases, ages and personal hygiene), the access to dialysis care, staff performance in practice and the infection control policy and compliance. Nonetheless, there were several possible reasons contributing to the low incidence of dialysis events in this study. First, the utilization incidence of fistula for the vascular access among of HD patients was much higher (73.70% vs. 43%) than that in the 2006 NHSN report27 and as mentioned above the use of fistula is associated with lower incidence of complications. Second, the data of NHSN report on dialysis events were from 10 years ago, which is likely to be outdated. It would be more meaningful to compare our data with newer data of the NHSN but such data except those for BSI are not available yet. Third, patients with high severity of underlying or kidney diseases in China were prone to be admitted to the hospital and then receive HD during their hospitalization rather than were dialyzed in outpatients. It will be useful to perform a surveillance of dialysis events for those receiving HD during hospitalization in China. Fourth, the Ministry of Health, China, has initiated a nationwide campaign to strictly restrict the use of antimicrobial agents since May 2011, which may have significantly reduced IV antimicrobial use among HD outpatients and therefore contributes to the low incidence of dialysis events.
The low incidence of dialysis events in this study suggests that the surveillance is needed to be tailored to identify patients at high risks of infection in a resource efficient manner and therefore could be more suitable in resource-limited settings like ours. As the use of fistula was associated with lower incidences of dialysis events, we propose that the continuous surveillance of dialysis events should target those using central lines only, which are associated with higher incidence of dialysis events, more hospitalizations and increased mortality32. In addition, a one- or two-day point prevalence survey on dialysis events for all HD outpatients regardless of the type of vascular access could be performed several times a year, e.g. every three months, in resource-limited settings. If the point prevalence survey identified high prevalence of dialysis events in a certain type (e.g. vascular access, age and underlying diseases) of patients, targeted surveillance for those patients may be initiated.
The findings in this report are subject to several limitations and should be interpreted with cautions. First, all participating dialysis centers were in tertiary hospitals and the results in this surveillance might not be generalizable to other centers, particularly those in non-tertiary hospitals. Second, we did not specially investigate the risk factors to develop dialysis events, the interventions implemented in each center to prevent HAIs and the preventability of dialysis events due to the restrain of the manpower, material and financial resources. Third, we did not collect the data about the timing of drawing blood for culture. It was therefore likely that blood culture samples were collected after antimicrobial start, which would reduce the rate of positive cultures. Fourth, we did not monitor hospitalization and death for all HD patients but only for those with dialysis events, which was a deficiency of our study design. Therefore, we were unable to determine whether patients with dialysis events were associated with higher hospitalization and mortality rates. Nonetheless, most patients with dialysis events were admitted to hospitals, suggesting that the surveillance on dialysis events was able to identify patients with poor outcomes.
In conclusion, this first multi-site surveillance of dialysis events in China revealed a relatively low incidence of dialysis events among HD outpatients. The use of fistula was associated with lower incidence of dialysis events compared to the use of central line. IV antimicrobial start accounted for the majority of dialysis events but was mainly used to treat respiratory tract infections rather than VAI. The intervention of dialysis events could include measures to prevent respiratory tract infections in addition to those to prevent VAI including BSI and LASI. The surveillance of dialysis events may be tailored to target those using central line for vascular access in resource-limited settings.
References
Zuo, L. & Wang, M. & Chinese Association of Blood Purification Management of Chinese Hospital, A. Current burden and probable increasing incidence of ESRD in China. Clin Nephrol 74 (Suppl 1), S20–22 (2010).
Liu, Z. H. Nephrology in China. Nat Rev Nephrol 9, 523–528 (2013).
Chen, X. The currect status and countermeasures of blood purification in China. An expert seminar. (Chinese Society of Nephrology, http://www.csnchina.org/cn/news.asp?id=39.html, 2012).
Deng, M. & Wu, Y. Current status of control of nosocomial infections in hemodialysis centers. Chin J Nosocomiol 24, 4391–4393 (2014).
Li, L. Thinking about HCV infection events of hemodalysis patients. Chinese Nursing Management 10, 36–39 (2010).
Eleftheriadis, T., Liakopoulos, V., Leivaditis, K., Antoniadi, G. & Stefanidis, I. Infections in hemodialysis: a concise review - Part 1: bacteremia and respiratory infections. Hippokratia 15, 12–17 (2011).
Betjes, M. G. Prevention of catheter-related bloodstream infection in patients on hemodialysis. Nat Rev Nephrol 7, 257–265 (2011).
Schweiger, A., Trevino, S. & Marschall, J. Nosocomial infections in dialysis access. Contrib Nephrol 184, 205–221 (2015).
Rojas, L. et al. Bloodstream infections in patients with kidney disease: risk factors for poor outcome and mortality. J Hosp Infect 85, 196–205 (2013).
van Diepen, A. T. et al. The association between dialysis modality and the risk for dialysis technique and non-dialysis technique-related infections. Nephrol Dial Transplant 29, 2244–2250 (2014).
Centers for Disease, C. & Prevention. Infection control requirements for dialysis facilities and clarification regarding guidance on parenteral medication vials. MMWR Morb Mortal Wkly Rep 57, 875–876 (2008).
National Kidney, F. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis 60, 850–886 (2012).
Haddad, N. J., Winoto, J., Shidham, G. & Agarwal, A. K. Hemodialysis access monitoring and surveillance, how and why? Front Biosci (Elite Ed) 4, 2396–2401 (2012).
Center of Disease Prevention and Control. NHSN Dialysis Event Protocol (2012).
Ministry of Health of the People’s Republic of China. Diagnostic standards of nosocomial infections (2001).
EpiData - Comprehensive Data Management and Basic Statistical Analysis System (EpiData Association, Odense, Denmark, 2010).
Alexander, E. L. et al. Prevalence, persistence, and microbiology of Staphylococcus aureus nasal carriage among hemodialysis outpatients at a major New York Hospital. Diagn Microbiol Infect Dis 70, 37–44 (2011).
Rojas-Moreno, C. A. et al. Catheter-Related Bloodstream Infections in Patients on Emergent Hemodialysis. Infect Control Hosp Epidemiol 37, 301–305 (2016).
Lata, C., Girard, L., Parkins, M. & James, M. T. Catheter-related bloodstream infection in end-stage kidney disease: a Canadian narrative review. Can J Kidney Health Dis 3, 24 (2016).
Pantelias, K. & Grapsa, E. Vascular access today. World J Nephrol 1, 69–78 (2012).
Nelson, R. G. & Tuttle, K. R. The new KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and CKD. Blood Purif 25, 112–114 (2007).
Spergel, L. & Vickie, P. In Endovascular Today 46–48 (2007).
Davis, R. E., Dougherty, E., McArthur, C., Huang, Q. S. & Baker, M. G. Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza Other Respir Viruses 10, 310–313 (2016).
Eccles, R. & Wilkinson, J. E. Exposure to cold and acute upper respiratory tract infection. Rhinology 53, 99–106 (2015).
Wilkinson, T. J., Shur, N. F. & Smith, A. C. “Exercise as medicine” in chronic kidney disease. Scand J Med Sci Sports (2016).
Barcellos, F. C., Santos, I. S., Umpierre, D. & Bohlke, M. & Hallal, P. C. Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin Kidney J 8, 753–765 (2015).
Klevens, R. M. et al. Dialysis Surveillance Report: National Healthcare Safety Network (NHSN)-data summary for 2006. Semin Dial 21, 24–28 (2008).
Meng, J., Cui, J., Wang, R. & Zheng, C. Nasal carriage of Staphylococcus aureus and drug resistance in patients with diabetes mellitus. Chin J Nosocomiol 15, 830–831 (2005).
Huang, X., Li, J., Wu, A. & Li, C. The carriage state of Staphylococcus aureus in tumor patients with chemotherapy. Chin J Infect Control 8, 348–350 (2009).
Chen, Z., Liu, W., Zou, M., Wu, A. & Ai, Y. Colonization and drug-resistance of multidrug-resistant bacteria in intensive care unit. Chin J Infect Control 9, 155–159 (2010).
Bajwa, R. et al. Can the NHSN dialysis event protocol be implemented in an Irish dialysis unit? Int J Infect Control 8, 1–6 (2012).
Badawy, D. A., Mowafi, H. S. & Al-Mousa, H. H. Surveillance of dialysis events: 12-month experience at five outpatient adult hemodialysis centers in Kuwait. J Infect Public Health 7, 386–391 (2014).
Acknowledgements
This study was supported by a grant from the Hospital Infection Prevention And Control Capacity Building Project of Chinese Hospital Association, China (CHA-2012-XSPX-0629-1). We are grateful to many other investigators who participated in this project including Li Jiang and Yang Yang from Fuxing Hospital, Capital Medical University, Huixue Jia and Liuyi Li from First people’s Hospital of Beijing University, Xiayue Jie and Xiying Shan from Beijing Huaxin Hospital, Mingmei Du and Wensi Du from People’s Liberation Army General Hospital, Xia Cui and Fang Liu from Air Force General Hospital, Yu Zhang from Guangdong Provincial People’s Hospital, Dayue Liu from the First Affiliated Hospital of Sun Yet-sen University, Tong Chen and Yufei Zhang from First people’s Hospital of Zunyi, Yong Liu and Liekuan Li from Zunyi Medical College, Fuqin Li and Pei Wang from the first affiliated hospital of Zhengzhou University, Jinjuan Liang and Dan Qu from the second affiliated hospital of Zhengzhou University, Rui Wu and Yongshen Lu from the fifth affiliated hospital of Zhengzhou University, Xuelan Fan and Xinhong Shen from Xinxiang Central Hospital, Meili Huang and Li Zhang from Mawangdui Hospital of Hunan province, Yuan Yuan and Tian Huang from Xiangtan Central Hospital of Hunan province, Mei Chang and Chunjuan Shi from Gulou Hospital Affiliated to Medical College of Nanjing University, Wanjun Zhang and Yandong Zhang from People’s Liberation Army NO. 202 Hospital, Hui Gao and Man Liu from the First people’s Hospital of Jining City, Jihua Sun and Lin Wang from Binzhou Medical University Hosptial, Haijiao Zhang and Bo Dai from people’s Hospital of Liaocheng City, Xiaoling Zhang and Guohong Wang from Shanxi Province People’s Hospital, Jie Zhang and Ming Hui from Yuncheng Central Hospital, Suping Zhang and Xuemei Li from First people’s Hospital of Jinzhong City, Yun Yang and Junping Shen from Shanxi Dayi Hospital, Lizhen Guo from the second people’s Hospital of Changzhi City, Chao Li and Weijia Yin from West China Hospital of Sichuan University, Yue Hong and Huijun Zhou from the second people’s Hospital of Ningbo City, Yeli Dong and Huafang Xi from the second people’s Hospital of Jiaxing City, Xuefen He and Xiaomei Xu from First people’s Hospital of Dongyang City, Shuhua Ren and Yuying Ge from First people’s Hospital of Hangzhou City, Qunfang You and Muying Yang from the Second Affiliated Hospital of Zhejiang University School of Medicine.
Author information
Authors and Affiliations
Contributions
L.L., H.J., Y.L., J.W., A.W., Q.L., T.H., Y.Y., H.Y., W.L., and Z.Z. designed the study. H.Z. and Z.Z. wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, H., Li, L., Jia, H. et al. Surveillance of Dialysis Events: one-year experience at 33 outpatient hemodialysis centers in China. Sci Rep 7, 249 (2017). https://doi.org/10.1038/s41598-017-00302-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00302-9
This article is cited by
-
Surveillance of hemodialysis related infections: a prospective multicenter study
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.