Abstract
Fixed-dose combination (FDC) therapy, also known as polypill therapy, targets risk factors for atherosclerotic cardiovascular disease (ASCVD) and has been proposed as a strategy to reduce global ASCVD burden. Here we conducted a systematic search for relevant studies from 2016–2022 to assess the effects of FDC therapy for prevention of ASCVD. The studies selected include randomized trials evaluating FDC therapy with at least one blood pressure-lowering drug and one lipid-lowering drug. The study data were independently extracted, the quality of evidence was appraised by multiple reviewers and effect estimates were pooled using a fixed-effect meta-analysis when statistical heterogeneity was low to moderate. The main outcomes of the analysis were all-cause mortality, fatal and nonfatal ASCVD events, adverse events, systolic blood pressure, low-density lipoprotein cholesterol and adherence. Among 26 trials (n = 27,317 participants, 43.2% female and mean age range 52.9–76.0), FDC therapy was associated with lower low-density lipoprotein cholesterol and systolic blood pressure, with higher rates of adherence and adverse events in both primary and mixed secondary prevention populations. For studies with a mostly primary prevention population, FDC therapy was associated with lower risk of all-cause mortality by 11% (5.6% versus 6.3%; relative risk (risk ratio) of 0.89; 95% confidence interval 0.78 to 1.00; I2 = 0%; four trials and 16,278 participants) and risk of fatal and nonfatal ASCVD events by 29% (6.1% versus 8.4%; relative risk (risk ratio) of 0.71; 95% confidence interval 0.63 to 0.79; I2 = 0%; five trials and 15,503 participants). One adequately powered trial in an exclusively secondary prevention population showed that FDC therapy reduced the risk of major adverse cardiovascular events by 24%. These findings support adoption and implementation of polypills to lower risk for all-cause mortality and ASCVD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
We conducted the searches on MEDLINE (Ovid), Cochrane Library (Wiley), EMBASE (Elsevier), CINAHL Plus with Full Text (EBSCOhost) and Web of Science (Thomson Reuters). We sought additional studies from ClinicalTrials.gov and the World Health Organization International Clinical Trial Registry Platform. Search results were uploaded to EndNote (version 20) and subsequently Covidence (available from https://www.covidence.org/) for deduplication and screening. Data supporting the findings of this study are available within the manuscript, extended data and Supplementary Information. Any additional data are available from the corresponding author upon request by email.
Code availability
Custom code was developed using R version 4.0.5 (R Project for Statistical Computing) for analysis of data inputs. The statistical code used for this analysis is available at https://github.com/THUYE/FDC-Therapy-ASCVD.
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019 update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795–808 (2020).
The Global Cardiovascular Risk Consortium. Global effect of modifiable risk factors on cardiovascular disease and mortality. N. Engl. J. Med. 389, 1273–1285 (2023).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364, 937–952 (2004).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Cholesterol Treatment Trialists’ Consortium. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376, 1670–1681 (2010).
Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 362, 1527–1535 (2003).
Marcus, M. E. et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Glob. Health 10, e369–e379 (2022).
Nelson, A. J. et al. Use of lipid, blood pressure, and glucose-lowering pharmacotherapy in patients with type 2 diabetes and atherosclerotic cardiovascular disease. JAMA Netw. Open 5, e2148030 (2022).
Yusuf, S. et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet 378, 1231–1243 (2011).
Secondary prevention of noncommunicable diseases in low- and middle-income countries through community-based and health service interventions: World Health Organization–Wellcome Trust meeting report, 1–3 August 2001. World Health Organization https://apps.who.int/iris/handle/10665/42567 (2002).
Joseph, P. et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis. Lancet 398, 1133–1146 (2021).
Castellano, J. M. Polypill strategy in secondary cardiovascular prevention. N. Engl. J. Med. https://doi.org/10.1056/nejmoa2208275 (2022).
Bahiru, E. et al. Fixed‐dose combination therapy for the prevention of atherosclerotic cardiovascular diseases. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.cd009868.pub3 (2017).
Cates, et al. Fixed‐dose combination therapy for the prevention of cardiovascular disease. Cochrane Database Syst. Rev. CD009868 https://doi.org/10.1002/14651858.cd009868.pub2 (2014).
Zamorano, J. et al. Proactive multiple cardiovascular risk factor management compared with usual care in patients with hypertension and additional risk factors: the CRUCIAL trial. Curr. Med. Res. Opin. 27, 821–833 (2011).
Neutel, J. M. et al. The use of a single‐pill calcium channel blocker/statin combination in the management of hypertension and dyslipidemia: a randomized, placebo‐controlled, multicenter study. J. Clin. Hypertens. 11, 22–30 (2009).
Castellano, J. M. et al. A polypill strategy to improve adherence results from the FOCUS project. J. Am. Coll. Cardiol. 64, 2071–2082 (2014).
Selak, V. et al. Effect of fixed dose combination treatment on adherence and risk factor control among patients at high risk of cardiovascular disease: randomised controlled trial in primary care. Br. Med. J. 348, g3318 (2014).
Patel, A. et al. A pragmatic randomized trial of a polypill-based strategy to improve use of indicated preventive treatments in people at high cardiovascular disease risk. Eur. J. Prev. Cardiol. 22, 920–930 (2014).
Malekzadeh, F. et al. A pilot double‐blind randomised placebo‐controlled trial of the effects of fixed‐dose combination therapy (‘polypill’) on cardiovascular risk factors. Int. J. Clin. Pr. 64, 1220–1227 (2010).
Park, J.-S. et al. Efficacy and safety of fixed-dose combination therapy with olmesartan medoxomil and rosuvastatin in Korean patients with mild to moderate hypertension and dyslipidemia: an 8-week, multicenter, randomized, double-blind, factorial-design study (OLSTA-D RCT: OLmesartan rosuvaSTAtin from Daewoong). Drug Des. Dev. Ther. 10, 2599–2609 (2016).
PILL Collaborative Group. An international randomised placebo-controlled trial of a four-component combination pill (‘polypill’) in people with raised cardiovascular risk. PLoS ONE 6, e19857 (2011).
Soliman, E. Z. et al. A polypill for primary prevention of cardiovascular disease: a feasibility study of the World Health Organization. Trials https://doi.org/10.1186/1745-6215-12-3 (2011).
The Indian Polycap Study (TIPS). Effects of a polypill (polycap) on risk factors in middle-aged individuals without cardiovascular disease (TIPS): a phase II, double-blind, randomised trial. Lancet 373, 1341–1351 (2009).
Grimm, R. et al. Simultaneous treatment to attain blood pressure and lipid goals and reduced CV risk burden using amlodipine/atorvastatin single-pill therapy in treated hypertensive participants in a randomized controlled trial. Vasc. Health Risk Manag. 6, 261–271 (2010).
Thom, S. et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD: the UMPIRE randomized clinical trial. JAMA 310, 918–929 (2013).
Wald, D. S., Morris, J. K. & Wald, N. J. Randomized polypill crossover trial in people aged 50 and over. PLoS ONE 7, e41297 (2012).
Kim, S.-H. et al. Blood pressure and cholesterol-lowering efficacy of a fixed-dose combination with irbesartan and atorvastatin in patients with hypertension and hypercholesterolemia: a randomized, double-blind, factorial, multicenter phase III study. Clin. Ther. 38, 2171–2184 (2016).
Oh, G. C. et al. Efficacy and safety of fixed-dose combination therapy with telmisartan and rosuvastatin in Korean patients with hypertension and dyslipidemia: TELSTA-YU (TELmisartan-rosuvaSTAtin from YUhan), a multicenter, randomized, 4-arm, double-blind, placebo-controlled, phase III study. Clin. Ther. 40, 676–691.e1 (2018).
Cho, K. I. et al. Efficacy and safety of a fixed-dose combination of candesartan and rosuvastatin on blood pressure and cholesterol in patients with hypertension and hypercholesterolemia: a multicenter, randomized, double-blind, parallel phase III clinical study. Clin. Ther. 41, 1508–1521 (2019).
Muñoz, D. et al. Polypill for cardiovascular disease prevention in an underserved population. N. Engl. J. Med. 381, 1114–1123 (2019).
Roshandel, G. et al. Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): a pragmatic, cluster-randomised trial. Lancet 394, 672–683 (2019).
Chung, S. et al. Effect of FIXed-dose combination of ARb and statin on adherence and risk factor control: the randomized FIXAR study. Cardiol. J. 29, 815–823 (2022).
Mariani, J. et al. Multicap to improve adherence after acute coronary syndromes: results of a randomized controlled clinical trial. Ther. Adv. Cardiovasc. Dis. 14, 1753944720912071 (2020).
Choi, J. et al. Central blood pressure lowering effect of telmisartan‐rosuvastatin single‐pill combination in hypertensive patients combined with dyslipidemia: a pilot study. J. Clin. Hypertens. 23, 1664–1674 (2021).
González-Juanatey, J. R. et al. Pharmacodynamic study of the cardiovascular polypill. Is there any interaction among the monocomponents? Rev. Esp. Cardiol. Engl. Ed. 74, 51–58 (2021).
Yusuf, S. et al. Polypill with or without aspirin in persons without cardiovascular disease. N. Engl. J. Med. 3, 216–228 (2021).
Merat, S. et al. Polypill for prevention of cardiovascular diseases with focus on non-alcoholic steatohepatitis: the PolyIran-Liver trial. Eur. Heart J. 21, 2023–2033 (2022).
Kim, W. et al. A randomized, double‐blind clinical trial to evaluate the efficacy and safety of a fixed‐dose combination of amlodipine/rosuvastatin in patients with dyslipidemia and hypertension. J. Clin. Hypertens. 22, 261–269 (2020).
Zhu, J. Z. et al. Medication use for cardiovascular disease prevention in 40 low- and middle-income countries. J. Am. Coll. Cardiol. 81, 620–622 (2023).
Yusuf, S. et al. Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N. Engl. J. Med. 374, 2032–2043 (2016).
Jahangiri, R. et al. Cost-effectiveness of fixed-dose combination pill (polypill) in primary and secondary prevention of cardiovascular disease: a systematic literature review. PLoS ONE 17, e0271908 (2022).
Lamy, A. et al. The cost implications of a polypill for primary prevention in the TIPS-3 trial. Eur. Hear. J. Qual. Care Clin. Outcomes 8, 899–908 (2021).
Abimbola, S. & Liu, H. Adoption and scale-up of the cardiovascular polypill: a realist institutional analysis. Health Policy Plan. 1, 15–27 (2023).
Huffman, M. D., Xavier, D. & Perel, P. Uses of polypills for cardiovascular disease and evidence to date. Lancet 389, 1055–1065 (2017).
Huffman, M. D., Salam, A. & Patel, A. Implementation strategies for cardiovascular polypills. JAMA 322, 2279–2280 (2019).
Huffman, M. D. & Yusuf, S. Polypills essential medicines for cardiovascular disease secondary prevention? J. Am. Coll. Cardiol. 63, 1368–1370 (2014).
Webster, R. et al. An electronic decision support‐based complex intervention to improve management of cardiovascular risk in primary health care: a cluster randomised trial (INTEGRATE). Med J. Aust. 214, 420–427 (2021).
Rao, S. et al. Association of polypill therapy with cardiovascular outcomes, mortality, and adherence: a systematic review and meta-analysis of randomized controlled trials. Prog. Cardiovasc. Dis. 73, 48–55 (2022).
Selak, V. et al. Reaching cardiovascular prevention guideline targets with a polypill-based approach: a meta-analysis of randomised clinical trials. Heart 105, 42 (2019).
Abushouk, A. I. et al. Fixed-dose combination (polypill) for cardiovascular disease prevention: a meta-analysis. Am. J. Prev. Med. 63, 440–449 (2022).
United States Preventive Services Task Forceet al. Aspirin use to prevent cardiovascular disease. JAMA 327, 1577–1584 (2022).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br. Med. J. 336, 924–926 (2008).
Agarwal, A. Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular diseases: a systematic review update. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=229735 (PROSPERO, 2021).
Higgins, J. P. T. et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3. www.training.cochrane.org/handbook (Cochrane, 2011).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br. Med. J. 366, l4898 (2019).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 315, 629 (1997).
Acknowledgements
We thank the investigators of the PolyIran-Liver trial for sharing selected disaggregated data to allow our team to standardize definitions of ASCVD events in this systematic review and meta-analysis. We thank A. Hively for his contributions in manuscript reviewing. The study received no funding. A.A. is supported by the NIH/NHLBI grant K99HL157687 and has received funding from grant 2020144 from the Doris Duke Charitable Foundation.
Author information
Authors and Affiliations
Contributions
A.A., A.N.d.C., S.E. and M.D.H. conceptualized the study and designed the systematic review protocol. Q.E.W. performed all database searches. A.A., P.M.M., T.J., N.S.S, J.Z., E.B. and M.D.H. contributed to screening, data extraction and quality of evidence assessment. J.Y. conducted the meta-analysis and provided statistical expertise. A.A. led writing of the original draft and P.M.M., T.J., N.S.S., J.Y., J.Z., Q.E.W., E.B., A.N.d.C., S.E., D.P., A.R. and M.D.H. contributed to revising the manuscript critically for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
M.D.H. has received travel support from the World Heart Federation. M.D.H. and A.R. have an appointment at The George Institute for Global Health, which has a patent, license and has received investment funding with intent to commercialize fixed-dose combination therapy through its social enterprise business, George Medicines. George Health Enterprises Pty Ltd, the social enterprise arm of the George Institute for Global Health (TGIGH), has received investment to develop fixed-dose combination products containing aspirin, statin and BP-lowering drugs. The George Institute for Global Health holds and have filed applications for combination products for the treatment of hypertension and diabetes, and A.R. is listed as one of the inventors (granted: US 10,369,15; US 10,799,487; US 10,322,117; US 11,033,544; and US 11,478,462 and pending: US 17/932,982; US 18/446,268; US 17/598,122; and US 17/317,614). A.R. is seconded part-time to George Medicines Pty Ltd, a subsidiary of George Health Enterprises. A.R. does not have a personal financial interest in these patents or products. M.D.H. and A.A. have pending patents for heart failure polypills. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks John McEvoy and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Michael Basson, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Sensitivity analyses of primary outcomes including only large studies with more than 500 participants.
Shown are risks of fatal or non-fatal ASCVD events in mostly primary prevention trials [N = 3 studies, N = 14,817 participants] (a). Shown are effects on systolic blood pressure in mostly primary prevention trials (b). Shown are effects on systolic blood pressure in mixed secondary prevention trials (c). Shown are effects on LDL cholesterol in mostly primary prevention trials (d). Shown are effects on LDL cholesterol in mixed secondary prevention trials (e). Shown are effects on adverse events in mostly primary prevention trials [N = 3 studies, N = 13,140 participants] (f). Shown are effects on adverse events in mixed secondary prevention trials [N = 5 studies, N = 6,301 participants] (g). Shown are effects on adherence in mostly primary, mixed, and secondary prevention trials [N = 6 studies, N = 11,280 participants] (h). In these forest plots, the risk ratio or mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall risk ratio or mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 2 Effects of fixed-dose combination therapy on diastolic blood pressure: primary analyses.
Shown are effects on diastolic blood pressure (mmHg) in mostly primary prevention trials (a) and mixed secondary prevention trials (b). In these forest plots, the mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 3 Effects of fixed-dose combination therapy on total cholesterol: primary analyses.
Shown are effects on total cholesterol (mmol/L) in mostly prevention trials (a), mixed secondary prevention trials (b), trials with comparator as usual care (c), and trials evaluating three-drug or more fixed-dose combination therapies (d). In these forest plots, the mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 4 Effects of fixed-dose combination therapy on discontinuation.
In this forest plot (N = 9 studies, N = 8,927 participants), the risk ratio for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall risk ratio is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 5 Effects of fixed-dose combination therapy on health-related quality of life using EQ-5D health state.
In this forest plot, the mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 6 Effects of fixed-dose combination therapy on the risk of all-cause mortality and atherosclerotic cardiovascular disease events: subgroup analyses.
Shown is the risk of all-cause mortality in trials with comparator as usual care [N = 7 studies, N = 16,171 participants] (a). Shown is the risk of all-cause mortality in trials evaluating three-drug or more fixed-dose combination therapies [N = 8 studies, N = 21,122 participants] (b). Shown is the risk of fatal and non-fatal ASCVD events in trials with comparator as usual care [N = 6 studies, N = 14,720 participants] (c). Shown is the risk of fatal and non-fatal ASCVD events in trials evaluating three-drug or more fixed-dose combination therapies [N = 9 studies, N = 21,603 participants] (d). In these forest plots, the risk ratio for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall risk ratio is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 7 Effects of fixed-dose combination therapy on systolic blood pressure: subgroup analyses.
Shown is the effect on systolic blood pressure (mmHg) in trials with comparator as usual care (a) and effect on systolic blood pressure (mmHg) in trials evaluating three-drug or more fixed-dose combination therapies (b). In these forest plots, the mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 8 Effects of fixed-dose combination therapy on LDL cholesterol: subgroup analyses.
Shown is the effect on LDL cholesterol (mmol/L) in trials with comparator as usual care (a). Shown is the effect on LDL cholesterol in trials evaluating three-drug or more fixed-dose combination therapies (b). In these forest plots, the mean difference for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall mean difference is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 9 Effects of fixed-dose combination therapy on adverse events as defined by study investigators: subgroup analyses.
Shown are effects on any adverse event in trials with the comparator as usual care [N = 7 studies, N = 13,308 participants] (a). Shown are effects on any adverse event in trials evaluating three-drug or more fixed-dose combination therapies [N = 13 studies, N = 19,697 participants] (b). Shown are effects on adverse event of myalgias [N = 12 studies, N = 11,204 participants] (c). Shown are effects on adverse event of increased liver enzymes [N = 6 studies, N = 2,280 participants] (d). Shown are effects on adverse event of cough [N = 7 studies, N = 10,967 participants] (e). Shown are effects on adverse event of dyspepsia/gastrointestinal irritation [N = 8 studies, N = 15,567 participants] (f). Shown are effects on adverse event of bleeding [N = 5 studies, N = 9,473 participants] (g). In these forest plots, the risk ratio for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall risk ratio is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Extended Data Fig. 10 Effects of fixed-dose combination therapy on adherence: subgroup analysis.
In this forest plot [N = 4 studies, N = 4,872 participants], the risk ratio for each individual study is represented with an orange dot surrounded by a dark blue square representing the weight assigned to each study in the model, with 95% confidence intervals represented by horizontal lines. The overall risk ratio is represented by a green diamond. All statistics were based on a two-sided z-test with no adjustments made for multiple comparisons.
Supplementary information
Supplementary Information
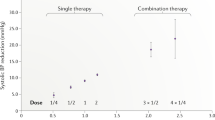
Supplementary Tables 1–4 and Figs.1–3.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agarwal, A., Mehta, P.M., Jacobson, T. et al. Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular disease. Nat Med 30, 1199–1209 (2024). https://doi.org/10.1038/s41591-024-02896-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-024-02896-w