Abstract
Post-traumatic epilepsy (PTE) accounts for 5% of all epilepsies. The incidence of PTE after traumatic brain injury (TBI) depends on the severity of injury, approaching one in three in groups with the most severe injuries. The repeated seizures that characterize PTE impair neurological recovery and increase the risk of poor outcomes after TBI. Given this high risk of recurrent seizures and the relatively short latency period for their development after injury, PTE serves as a model disease to understand human epileptogenesis and trial novel anti-epileptogenic therapies. Epileptogenesis is the process whereby previously normal brain tissue becomes prone to recurrent abnormal electrical activity, ultimately resulting in seizures. In this Review, we describe the clinical course of PTE and highlight promising research into epileptogenesis and treatment using animal models of PTE. Clinical, imaging, EEG and fluid biomarkers are being developed to aid the identification of patients at high risk of PTE who might benefit from anti-epileptogenic therapies. Studies in preclinical models of PTE have identified tractable pathways and novel therapeutic strategies that can potentially prevent epilepsy, which remain to be validated in humans. In addition to improving outcomes after TBI, advances in PTE research are likely to provide therapeutic insights that are relevant to all epilepsies.
Key points
-
Post-traumatic epilepsy (PTE) is highly prevalent after traumatic brain injury, impairing neurological recovery and leading to worse functional outcomes.
-
Current epilepsy therapeutics symptomatically treat seizures but do not modify epileptogenesis, the process by which brain tissue becomes prone to seizures.
-
The unique nature of PTE, occurring after a well-defined epileptogenic insult, makes it a promising model system for understanding epileptogenesis.
-
Future research in individuals with PTE populations might not only reveal novel mechanisms of epileptogenesis but also enable anti-epileptogenic therapies to be tested.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Popescu, C., Anghelescu, A., Daia, C. & Onose, G. Actual data on epidemiological evolution and prevention endeavours regarding traumatic brain injury. J. Med Life 8, 272–277 (2015).
Frieden, T. R., Houry, D. & Baldwin, G. Report to Congress on traumatic brain injury in the United States: epidemiology and rehabilitation. Centers for Disease Control and Prevention. https://www.cdc.gov/traumaticbraininjury/pdf/TBI_Report_to_Congress_Epi_and_Rehab-a.pdf (2015).
GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 56–87 (2019).
Farrell, J. S., Wolff, M. D. & Teskey, G. C. Neurodegeneration and pathology in epilepsy: clinical and basic perspectives. Adv. Neurobiol. 15, 317–334 (2017).
Sharma, R. et al. Neuroinflammation in post-traumatic epilepsy: pathophysiology and tractable therapeutic targets. Brain Sci. 9, 318 (2019).
Pease, M. et al. Association of posttraumatic epilepsy with long-term functional outcomes in individuals with severe traumatic brain injury. Neurology 100, e1967–e1975 (2023).
Burke, J. et al. Association of posttraumatic epilepsy with 1-year outcomes after traumatic brain injury. JAMA Netw. Open 4, e2140191 (2021).
Fordington, S. & Manford, M. A review of seizures and epilepsy following traumatic brain injury. J. Neurol. 267, 3105–3111 (2020).
Lucke-Wold, B. P. et al. Traumatic brain injury and epilepsy: underlying mechanisms leading to seizure. Seizure 33, 13–23 (2015).
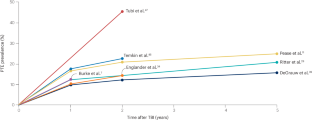
Annegers, J. F., Hauser, W. A., Coan, S. P. & Rocca, W. A. A population-based study of seizures after traumatic brain injuries. N. Engl. J. Med. 338, 20–24 (1998).
Pease, M. et al. Risk factors and incidence of epilepsy after severe traumatic brain injury. Ann. Neurol. 92, 663–669 (2022).
Schmidt, D., Friedman, D. & Dichter, M. A. Anti-epileptogenic clinical trial designs in epilepsy: issues and options. Neurotherapeutics 11, 401–411 (2014).
Pitkänen, A., Lukasiuk, K., Dudek, F. E. & Staley, K. J. Epileptogenesis. Cold Spring Harb. Perspect. Med. 5, a022822 (2015).
Löscher, W., Potschka, H., Sisodiya, S. M. & Vezzani, A. Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol. Rev. 72, 606–638 (2020).
Kehne, J. H., Klein, B. D., Raeissi, S. & Sharma, S. The National Institute of Neurological Disorders and Stroke (NINDS) Epilepsy Therapy Screening Program (ETSP). Neurochem. Res. 42, 1894–1903 (2017).
French, J. A. et al. Antiepileptogenesis and disease modification: clinical and regulatory issues. Epilepsia Open 6, 483–492 (2021).
Löscher, W. & Schmidt, D. Modern antiepileptic drug development has failed to deliver: ways out of the current dilemma. Epilepsia 52, 657–678 (2011).
World Health Organization. Epilepsy: a public health imperative. WHO. https://iris.who.int/bitstream/handle/10665/325440/WHO-MSD-MER-19.2-eng.pdf (2019).
Gugger, J. J. et al. Multimodal quality of life assessment in post-9/11 veterans with epilepsy: impact of drug resistance, traumatic brain injury, and comorbidity. Neurology 98, E1761–E1770 (2022).
Raymont, V. et al. Correlates of posttraumatic epilepsy 35 years following combat brain injury. Neurology 75, 224–229 (2010).
Vespa, P. M. et al. The epilepsy bioinformatics study for anti-epileptogenic therapy (EpiBioS4Rx) clinical biomarker: study design and protocol. Neurobiol. Dis. 123, 110–114 (2019).
Saletti, P. G. et al. Tau phosphorylation patterns in the rat cerebral cortex after traumatic brain injury and sodium selenate effects: an Epibios4rx Project 2 study. J. Neurotrauma 41, 222–243 (2024).
Saletti, P. G. et al. Early preclinical plasma protein biomarkers of brain trauma are influenced by early seizures and levetiracetam. Epilepsia Open 8, 586–608 (2023).
Engel, J. J. Epileptogenesis, traumatic brain injury, and biomarkers. Neurobiol. Dis. 123, 3–7 (2019).
Correa, D. J. et al. Applying participatory action research in traumatic brain injury studies to prevent post-traumatic epilepsy. Neurobiol. Dis. 123, 137–144 (2019).
Duncan, D. et al. Big data sharing and analysis to advance research in post-traumatic epilepsy. Neurobiol. Dis. 123, 127–136 (2019).
Christensen, J. The epidemiology of posttraumatic epilepsy. Semin. Neurol. 35, 218–222 (2015).
Thapa, A. et al. Post-traumatic seizures — a prospective study from a tertiary level trauma center in a developing country. Seizure 19, 211–216 (2010).
Ritter, A. C. et al. Incidence and risk factors of posttraumatic seizures following traumatic brain injury: a Traumatic Brain Injury Model Systems Study. Epilepsia 57, 1968–1977 (2016).
Haltiner, A. M., Temkin, N. R. & Dikmen, S. S. Risk of seizure recurrence after the first late posttraumatic seizure. Arch. Phys. Med. Rehabil. 78, 835–840 (1997).
Ngugi, A. K., Bottomley, C., Kleinschmidt, I., Sander, J. W. & Newton, C. R. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia 51, 883–890 (2010).
Thijs, R. D., Surges, R., O’Brien, T. J. & Sander, J. W. Epilepsy in adults. Lancet 393, 689–701 (2019).
Angeleri, F. et al. Posttraumatic epilepsy risk factors: one-year prospective study after head injury. Epilepsia 40, 1222–1230 (1999).
Englander, J. et al. Analyzing risk factors for late posttraumatic seizures: a prospective, multicenter investigation. Arch. Phys. Med. Rehabil. 84, 365–373 (2003).
Ferguson, P. L. et al. A population-based study of risk of epilepsy after hospitalization for traumatic brain injury. Epilepsia 51, 891–898 (2010).
Laing, J. et al. Risk factors and prognosis of early posttraumatic seizures in moderate to severe traumatic brain injury. JAMA Neurol. 79, 334–341 (2022).
Christensen, J. et al. Long-term risk of epilepsy after traumatic brain injury in children and young adults: a population-based cohort study. Lancet 373, 1105–1110 (2009).
Karlander, M., Ljungqvist, J. & Zelano, J. Post-traumatic epilepsy in adults: a nationwide register-based study. J. Neurol. Neurosurg. Psychiatry 92, 617–621 (2021).
DeGrauw, X. et al. Epidemiology of traumatic brain injury-associated epilepsy and early use of anti-epilepsy drugs: an analysis of insurance claims data, 2004–2014. Epilepsy Res. 146, 41–49 (2019).
Annegers, J. F. et al. Seizures after head trauma: a population study. Neurology 30, 683–689 (1980).
Mahler, B. et al. Unprovoked seizures after traumatic brain injury: a population-based case–control study. Epilepsia 56, 1438–1444 (2015).
Santos, S., Murphy, G., Baxter, K. & Robinson, K. M. Organisational factors affecting the quality of hospital clinical coding. Heal. Inf. Manag. 37, 25–37 (2008).
O’Malley, K. J. et al. Measuring diagnoses: ICD code accuracy. Health Serv. Res. 40, 1620–1639 (2005).
Langlois, J. A., Rutland-Brown, W. & Wald, M. M. The epidemiology and impact of traumatic brain injury: a brief overview. J. Head Trauma Rehabil. 21, 375–378 (2006).
Pugh, M. J. V. et al. The prevalence of epilepsy and association with traumatic brain injury in veterans of the Afghanistan and Iraq wars. J. Head Trauma Rehabil. 30, 29–37 (2015).
Lolk, K., Dreier, J. W. & Christensen, J. Repeated traumatic brain injury and risk of epilepsy: a Danish nationwide cohort study. Brain 144, 875–884 (2021).
Tubi, M. A. et al. Early seizures and temporal lobe trauma predict post-traumatic epilepsy: a longitudinal study. Neurobiol. Dis. 123, 115–121 (2019).
Salazar, A. M. et al. Epilepsy after penetrating head injury. I. Clinical correlates: a report of the Vietnam Head Injury Study. Neurology 35, 1406–1414 (1985).
The World Bank. World bank country and lending groups. Worldbank.org. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (2023).
Ogunrin, O. A. & Adeyekun, A. A. Profile of post-traumatic epilepsy in Benin City, Nigeria. West Afr. J. Med. 29, 153–157 (2011).
Rabiu, T. B. & Adetunmbi, B. Posttraumatic seizures in a rural Nigerian neurosurgical service. World Neurosurg. 104, 367–371 (2017).
Wang, X. P. et al. Development and external validation of a predictive nomogram model of posttraumatic epilepsy: a retrospective analysis. Seizure 88, 36–44 (2021).
Espinosa-Jovel, C., Toledano, R., Aledo-Serrano, Á., García-Morales, I. & Gil-Nagel, A. Epidemiological profile of epilepsy in low income populations. Seizure 56, 67–72 (2018).
Gennarelli, T., Champion, H., Copes, W. & Sacco, W. Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J. Trauma 37, 962–968 (1994).
Eagle, S. R., Pease, M., Nwachuku, E., Deng, H. & Okonkwo, D. O. Prognostic models for traumatic brain injury have good discrimination but poor overall model performance for predicting mortality and unfavorable outcomes. Neurosurgery 92, 137–143 (2023).
Eagle, S. R. et al. Performance of CRASH and IMPACT prognostic models for traumatic brain injury at 12 and 24 months post-injury. Neurotrauma Rep. 4, 118–123 (2023).
Hanna Siig Hausted, J. F. N. & Odgaard, L. Epilepsy after severe traumatic brain injury: frequency and injury severity. Brain Inj. 34, 889–894 (2020).
Ritter, A. C. et al. Prognostic models for predicting posttraumatic seizures during acute hospitalization, and at 1 and 2 years following traumatic brain injury. Epilepsia 57, 1503–1514 (2016).
Xu, T. et al. Risk factors for posttraumatic epilepsy: a systematic review and meta-analysis. Epilepsy Behav. 67, 1–6 (2017).
Temkin, N. R. Risk factors for posttraumatic seizures in adults. Epilepsia 44, 18–20 (2003).
Arefan, D., Pease, M., Eagle, S. R., Okonkwo, D. O. & Wu, S. Comparison of machine learning models to predict long-term outcomes after severe traumatic brain injury. Neurosurg. Focus 54, E14 (2023).
Dijkland, S. A. et al. Prognosis in moderate and severe traumatic brain injury: a systematic review of contemporary models and validation studies. J. Neurotrauma 37, 1–13 (2020).
Steyerberg, E. W. et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med 5, 1251–1261 (2008).
Immonen, R. et al. Imaging biomarkers of epileptogenecity after traumatic brain injury — preclinical frontiers. Neurobiol. Dis. 123, 75–85 (2019).
Garner, R. et al. Imaging biomarkers of posttraumatic epileptogenesis. Epilepsia 60, 2151–2162 (2019).
Prince, D. A. et al. Epilepsy following cortical injury: cellular and molecular mechanisms as targets for potential prophylaxis. Epilepsia 50, 30–40 (2009).
Jennett, W. B. & Lewin, W. Traumatic epilepsy after closed head injuries. J. Neurol. Neurosurg. Psychiatry 23, 295–301 (1960).
Al-Haddad, S. A. & Kirollos, R. A 5-year study of the outcome of surgically treated depressed skull fractures. Ann. R. Coll. Surg. Engl. 84, 196–200 (2002).
De Reuck, J. Risk factors for late-onset seizures related to cerebral contusions in adults with a moderate traumatic brain injury. Clin. Neurol. Neurosurg. 113, 469–471 (2011).
La Rocca, M. et al. Distribution and volume analysis of early hemorrhagic contusions by MRI after traumatic brain injury: a preliminary report of the Epilepsy Bioinformatics Study for Antiepileptogenic Therapy (EpiBioS4Rx). Brain Imaging Behav. 15, 2804–2812 (2021).
Messori, A., Polonara, G., Carle, F., Gesuita, R. & Salvolini, U. Predicting posttraumatic epilepsy with MRI: prospective longitudinal morphologic study in adults. Epilepsia 46, 1472–1481 (2005).
Gupta, P. K. et al. Subtypes of post-traumatic epilepsy: clinical, electrophysiological, and imaging features. J. Neurotrauma 31, 1439–1443 (2014).
Won, S. Y. et al. A systematic review of epileptic seizures in adults with subdural haematomas. Seizure 45, 28–35 (2017).
La Rocca, M. et al. Multiplex networks to characterize seizure development in traumatic brain injury patients. Front. Neurosci. 14, 591662 (2020).
Lutkenhoff, E. S. et al. Early brain biomarkers of post-traumatic seizures: initial report of the multicentre epilepsy bioinformatics study for antiepileptogenic therapy (EpiBioS4Rx) prospective study. J. Neurol. Neurosurg. Psychiatry 91, 1154–1157 (2020).
Manninen, E. et al. Acute thalamic damage as a prognostic biomarker for post-traumatic epileptogenesis. Epilepsia 62, 1852–1864 (2021).
Graham, N. S. N., Cole, J. H., Bourke, N. J., Schott, J. M. & Sharp, D. J. Distinct patterns of neurodegeneration after TBI and in Alzheimer’s disease. Alzheimers Dement. 19, 3065–3077 (2023).
Dinkel, J. et al. Long-term white matter changes after severe traumatic brain injury: a 5-year prospective cohort. Am. J. Neuroradiol. 35, 23–29 (2014).
Zelano, J. & Westman, G. Epilepsy after brain infection in adults. Neurology 95, e3213–e3220 (2020).
Yu, T., Liu, X., Sun, L., Wu, J. & Wang, Q. Clinical characteristics of post-traumatic epilepsy and the factors affecting the latency of PTE. BMC Neurol. 21, 301 (2021).
Candy, N., Tsimiklis, C., Poonnoose, S. & Trivedi, R. The use of antiepileptic medication in early post traumatic seizure prophylaxis at a single institution. J. Clin. Neurosci. 69, 198–205 (2019).
DJohn, J., Ibrahim, R., Patel, P., DeHoff, K. & Kolbe, N. Administration of levetiracetam in traumatic brain injury: is it warranted? Cureus 12, e9117 (2020).
Pease, M. et al. Multicenter and prospective trial of anti-epileptics for early seizure prevention in mild traumatic brain injury with a positive computed tomography scan. Surg. Neurol. Int. 13, 241 (2022).
Lee, S. T., Lui, T. N., Wong, C. W., Yeh, Y. S. & Tzaan, W. C. Early seizures after moderate closed head injury. Acta Neurochir. 137, 151–154 (1995).
Temkin, N. R. et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N. Engl. J. Med. 323, 497–502 (1990).
Gugger, J. J. & Diaz-Arrastia, R. Early posttraumatic seizures — putting things in perspective. JAMA Neurol. 79, 325–326 (2022).
Jennett, B. Early traumatic epilepsy: incidence and significance after nonmissile injuries. Arch. Neurol. 30, 394–398 (1974).
Glaser, A. C. et al. The effect of antiseizure medication administration on mortality and early posttraumatic seizures in critically ill older adults with traumatic brain injury. Neurocrit. Care 37, 538–546 (2022).
Zhao, Y., Wu, H., Wang, X., Li, J. & Zhang, S. Clinical epidemiology of posttraumatic epilepsy in a group of Chinese patients. Seizure 21, 322–326 (2012).
Bakr, A. & Belli, A. A systematic review of levetiracetam versus phenytoin in the prevention of late post-traumatic seizures and survey of UK neurosurgical prescribing practice of antiepileptic medication in acute traumatic brain injury. Br. J. Neurosurg. 32, 237–244 (2018).
Carney, N. et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 80, 6–15 (2017).
Wilson, C. D. et al. Early and late posttraumatic epilepsy in the setting of traumatic brain injury: a meta-analysis and review of antiepileptic management. World Neurosurg. 110, e901–e906 (2018).
Sundararajan, K., Milne, D., Edwards, S., Chapman, M. J. & Shakib, S. Anti-seizure prophylaxis in critically ill patients with traumatic brain injury in an intensive care unit. Anaesth. Intensive Care 43, 646–651 (2015).
Sun, Y. et al. Early post-traumatic seizures are associated with valproic acid plasma concentrations and UGT1A6/CYP2C9 genetic polymorphisms in patients with severe traumatic brain injury. Scand. J. Trauma Resusc. Emerg. Med 25, 85 (2017).
Temkin, N. R. et al. Valproate therapy for prevention of posttraumatic seizures: a randomized trial. J. Neurosurg. 91, 593–600 (1999).
Wang, B. C. et al. Comparative efficacy of prophylactic anticonvulsant drugs following traumatic brain injury: a systematic review and network meta-analysis of randomized controlled trials. PLoS ONE 17, e0265932 (2022).
Kwon, S. J. et al. Lacosamide versus phenytoin for the prevention of early post traumatic seizures. J. Crit. Care 50, 50–53 (2019).
Herman, S. T. et al. Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J. Clin. Neurophysiol. 32, 87–95 (2015).
Vespa, P. et al. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann. Neurol. 79, 579–590 (2016).
Khor, D. et al. Early seizure prophylaxis in traumatic brain injuries revisited: a prospective observational study. World J. Surg. 42, 1727–1732 (2018).
Inglet, S. et al. Seizure prophylaxis in patients with traumatic brain injury: a single-center study. Cureus 8, 6–8 (2016).
Hazama, A. et al. The effect of Keppra prophylaxis on the incidence of early onset, post-traumatic brain injury seizures. Cureus 10, e2674 (2018).
Pingue, V., Mele, C. & Nardone, A. Post-traumatic seizures and antiepileptic therapy as predictors of the functional outcome in patients with traumatic brain injury. Sci. Rep. 11, 4708 (2021).
Zaccara, G. et al. Do antiepileptic drugs increase the risk of infectious diseases? A meta-analysis of placebo-controlled studies. Br. J. Clin. Pharm. 83, 1873–1879 (2017).
Carpay, J. A., Aldenkamp, A. P. & van Donselaar, C. A. Complaints associated with the use of antiepileptic drugs: results from a community-based study. Seizure 14, 198–206 (2005).
Lu, X. & Wang, X. Hyponatremia induced by antiepileptic drugs in patients with epilepsy. Expert Opin. Drug Saf. 16, 77–87 (2017).
Aarabi, B., Taghipour, M., Haghnegahdar, A., Farokhi, M. & Mobley, L. Prognostic factors in the occurrence of posttraumatic epilepsy after penetrating head injury suffered during military service. Neurosurg. Focus 8, e1 (2000).
Galanopoulou, A. S. et al. Antiepileptogenesis and disease modification: progress, challenges, and the path forward — Report of the Preclinical Working Group of the 2018 NINDS-sponsored antiepileptogenesis and disease modification workshop. Epilepsia Open 6, 276–296 (2021).
Pingue, V. et al. Impact of seizures and their prophylaxis with antiepileptic drugs on rehabilitation course of patients with traumatic or hemorrhagic brain injury. Front. Neurol. 13, 1060008 (2022).
Pugh, M. J. et al. The military injuries: understanding post-traumatic epilepsy study: understanding relationships among lifetime traumatic brain injury history, epilepsy, and quality of life. J. Neurotrauma 38, 2841–2850 (2021).
Juengst, S. B. et al. Post-traumatic epilepsy associations with mental health outcomes in the first two years after moderate to severe TBI: a TBI Model Systems analysis. Epilepsy Behav. 73, 240–246 (2017).
Mazzini, L. et al. Posttraumatic epilepsy: neuroradiologic and neuropsychological assessment of long-term outcome. Epilepsia 44, 569–574 (2003).
Semple, B. D., Zamani, A., Rayner, G., Shultz, S. R. & Jones, N. C. Affective, neurocognitive and psychosocial disorders associated with traumatic brain injury and post-traumatic epilepsy. Neurobiol. Dis. 123, 27–41 (2020).
Ngadimon, I. W. et al. An interplay between post-traumatic epilepsy and associated cognitive decline: a systematic review. Front. Neurol. 13, 827571 (2022).
Mukherjee, S. et al. Neuroinflammatory mechanisms of post-traumatic epilepsy. J. Neuroinflammation 17, 193 (2020).
La Rocca, M. et al. Functional connectivity alterations in traumatic brain injury patients with late seizures. Neurobiol. Dis. 179, 106053 (2023).
Pease, M. et al. Outcome prediction in patients with severe traumatic brain injury using deep learning from head CT scans. Radiology 304, 385–394 (2022).
Lutkenhoff, E. S. et al. The subcortical basis of outcome and cognitive impairment in TBI: a longitudinal cohort study. Neurology 95, E2398–E2408 (2020).
Walker, W. C. et al. Global outcome and late seizures after penetrating versus closed traumatic brain injury: a NIDRR TBI Model Systems study. J. Head Trauma Rehabil. 30, 231–240 (2015).
Bushnik, T., Englander, J., Wright, J. & Kolakowsky-Hayner, S. A. Traumatic brain injury with and without late posttraumatic seizures: what are the impacts in the post-acute phase: a NIDRR traumatic brain injury model systems study. J. Head Trauma Rehabil. 27, 36–44 (2012).
Yu, T. et al. Predicting global functional outcomes among post-traumatic epilepsy patients after moderate-to-severe traumatic brain injury: development of a prognostic model. Front. Neurol. 13, 874491 (2022).
Uski, J., Lamusuo, S., Teperi, S., Löyttyniemi, E. & Tenovuo, O. Mortality after traumatic brain injury and the effect of posttraumatic epilepsy. Neurology 91, e878–e883 (2018).
Karlander, M., Ljungqvist, J., Sörbo, A. & Zelano, J. Risk and cause of death in post-traumatic epilepsy: a register-based retrospective cohort study. J. Neurol. 269, 6014–6020 (2022).
Englander, J., Bushnik, T., Wright, J. M., Jamison, L. & Duong, T. T. Mortality in late post-traumatic seizures. J. Neurotrauma 26, 1471–1477 (2009).
Rayner, G., Jackson, G. D. & Wilson, S. J. Two distinct symptom-based phenotypes of depression in epilepsy yield specific clinical and etiological insights. Epilepsy Behav. 64, 336–344 (2016).
Ponsford, J. Anxiety and depression following TBI. in Neurobehavioural Disability and Social Handicap Following Traumatic Brain Injury 2nd edn (eds McMillan, T. M. & Wood, R. L. L.) 167–177 (Taylor & Francis, 2017).
Foreman, B. et al. Seizures and cognitive outcome after traumatic brain injury: a post hoc analysis. Neurocrit. Care 36, 130–138 (2022).
Lee, H. et al. Continuous electroencephalography after moderate to severe traumatic brain injury. Crit. Care Med 47, 574–582 (2019).
He, X. et al. Resective surgery for drug-resistant posttraumatic epilepsy: predictors of seizure outcome. J. Neurosurg. 133, 1568–1575 (2019).
Chartrain, A. G. et al. Antiepileptics for post-traumatic seizure prophylaxis after traumatic brain injury. Curr. Pharm. Des. 23, 6428–6441 (2017).
Zimmermann, L. L., Martin, R. M. & Girgis, F. Treatment options for posttraumatic epilepsy. Curr. Opin. Neurol. 30, 580–586 (2017).
Hamed, R., Hussein, R., Ibraheem, S. & Jumaily, M. Comparative study between leviteracetam, phenytoin & carbamazepine in treating post traumatic epilepsy. NeuroQuantology 18, 1–5 (2020).
Scheffer, I. E. et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 58, 512–521 (2017).
Hitti, F. L. et al. Surgical outcomes in post-traumatic epilepsy: a single institutional experience. Oper. Neurosurg. 18, 12–18 (2020).
Marks, D. A., Kim, J., Spencer, D. D. & Spencer, S. S. Seizure localization and pathology following head injury in patients with uncontrolled epilepsy. Neurology 45, 2051–2057 (1995).
Hakimian, S. et al. Long-term outcome of extratemporal resection in posttraumatic epilepsy. Neurosurg. Focus 32, E10 (2012).
Schuele, S. U. & Lüders, H. O. Intractable epilepsy: management and therapeutic alternatives. Lancet Neurol. 7, 514–524 (2008).
Ferreira, L. D., Tabaeizadeh, M. & Haneef, Z. Surgical outcomes in post-traumatic temporal lobe epilepsy: a systematic review and meta-analysis. J. Neurotrauma 41, 319–330 (2024).
Wiebe, S., Blume, W. T., Girvin, J. P. & Eliasziw, M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N. Engl. J. Med. 345, 311–318 (2001).
Lee, H.-O. et al. Effect of vagus nerve stimulation in post-traumatic epilepsy and failed epilepsy surgery: preliminary report. J. Korean Neurosurg. Soc. 44, 196–198 (2008).
Shen, C.-C. & Jiang, J.-F. Auricular electroacupuncture for late posttraumatic epilepsy after severe brain injury: a retrospective study. Evid. Based Complement Altern. Med. 2019, 5798912 (2019).
Chen, Y. et al. Quantitative epileptiform burden and electroencephalography background features predict post-traumatic epilepsy. J. Neurol. Neurosurg. Psychiatry 94, 245–249 (2023).
Kim, J. A. et al. Epileptiform activity in traumatic brain injury predicts post-traumatic epilepsy. Ann. Neurol. 83, 858–862 (2018).
Faghihpirayesh, R. et al. Automatic detection of EEG epileptiform abnormalities in traumatic brain injury using deep learning. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2021, 302–305 (2021).
Di Sapia, R. et al. ECoG spiking activity and signal dimension are early predictive measures of epileptogenesis in a translational mouse model of traumatic brain injury. Neurobiol. Dis. 185, 106251 (2023).
Kumar, U., Li, L., Bragin, A. & Engel, J. J. Spike and wave discharges and fast ripples during posttraumatic epileptogenesis. Epilepsia 62, 1842–1851 (2021).
Li, L. et al. Spatial and temporal profile of high-frequency oscillations in posttraumatic epileptogenesis. Neurobiol. Dis. 161, 105544 (2021).
Pease, M. et al. Predicting post-traumatic epilepsy using admission electroencephalography after severe traumatic brain injury. Epilepsia 64, 1842–1852 (2023).
Ghaith, H. S. et al. A literature review of traumatic brain injury biomarkers. Mol. Neurobiol. 59, 4141–4158 (2022).
Misra, S. et al. Common pathways of epileptogenesis in patients with epilepsy post-brain injury: findings from a systematic review and meta-analysis. Neurology 101, e2243–e2256 (2023).
Cotter, D., Kelso, A. & Neligan, A. Genetic biomarkers of posttraumatic epilepsy: a systematic review. Seizure 46, 53–58 (2017).
Nam, J.-W. et al. Global analyses of the effect of different cellular contexts on microRNA targeting. Mol. Cell 53, 1031–1043 (2014).
Yu, Y. et al. The role of exosomal microRNAs in central nervous system diseases. Mol. Cell. Biochem. 476, 2111–2124 (2021).
Gitaí, D. L. G. et al. Extracellular vesicles in the forebrain display reduced miR-346 and miR-331-3p in a rat model of chronic temporal lobe epilepsy. Mol. Neurobiol. 57, 1674–1687 (2020).
Chen, S.-D. et al. Circulating microRNAs from serum exosomes may serve as a putative biomarker in the diagnosis and treatment of patients with focal cortical dysplasia. Cells 9, 1867 (2020).
Brennan, G. P. & Henshall, D. C. microRNAs in the pathophysiology of epilepsy. Neurosci. Lett. 667, 47–52 (2018).
Wang, Y. et al. Circulating microRNAs from plasma small extracellular vesicles as potential diagnostic biomarkers in pediatric epilepsy and drug-resistant epilepsy. Front. Mol. Neurosci. 15, 823802 (2022).
Heiskanen, M. et al. Discovery and validation of circulating microRNAs as biomarkers for epileptogenesis after experimental traumatic brain injury — the EPITARGET Cohort. Int. J. Mol. Sci. 24, 2823 (2023).
Kumar, P. miRNA dysregulation in traumatic brain injury and epilepsy: a systematic review to identify putative biomarkers for post-traumatic epilepsy. Metab. Brain Dis. 38, 749–765 (2023).
Karnati, H. K. et al. Neuronal enriched extracellular vesicle proteins as biomarkers for traumatic brain injury. J. Neurotrauma 36, 975–987 (2019).
Lin, Z. et al. Serum exosomal proteins F9 and TSP-1 as potential diagnostic biomarkers for newly diagnosed epilepsy. Front. Neurosci. 14, 737 (2020).
Karttunen, J., Heiskanen, M., Lipponen, A., Poulsen, D. & Pitkänen, A. Extracellular vesicles as diagnostics and therapeutics for structural epilepsies. Int. J. Mol. Sci. 20, 1259 (2019).
Upadhya, D. & Shetty, A. K. Promise of extracellular vesicles for diagnosis and treatment of epilepsy. Epilepsy Behav. 121, 106499 (2021).
Redell, J. B., Moore, A. N., Ward, N. H. III, Hergenroeder, G. W. & Dash, P. K. Human traumatic brain injury alters plasma microRNA levels. J. Neurotrauma 27, 2147–2156 (2010).
Qin, X. et al. Expression profile of plasma microRNAs and their roles in diagnosis of mild to severe traumatic brain injury. PLoS ONE 13, e0204051 (2018).
Ko, J. et al. Diagnosis of traumatic brain injury using miRNA signatures in nanomagnetically isolated brain-derived extracellular vesicles. Lab Chip 18, 3617–3630 (2018).
Hicks, S. D. et al. Overlapping microRNA expression in saliva and cerebrospinal fluid accurately identifies pediatric traumatic brain injury. J. Neurotrauma 35, 64–72 (2018).
Di Pietro, V. et al. MicroRNAs as novel biomarkers for the diagnosis and prognosis of mild and severe traumatic brain injury. J. Neurotrauma 34, 1948–1956 (2017).
Bhomia, M., Balakathiresan, N. S., Wang, K. K., Papa, L. & Maheshwari, R. K. A panel of serum miRNA biomarkers for the diagnosis of severe to mild traumatic brain injury in humans. Sci. Rep. 6, 28148 (2016).
Yan, S. et al. Altered microRNA profiles in plasma exosomes from mesial temporal lobe epilepsy with hippocampal sclerosis. Oncotarget 8, 4136–4146 (2017).
Raoof, R. et al. Dual-center, dual-platform microRNA profiling identifies potential plasma biomarkers of adult temporal lobe epilepsy. eBioMedicine 38, 127–141 (2018).
Medel-Matus, J.-S. et al. Susceptibility to epilepsy after traumatic brain injury is associated with preexistent gut microbiome profile. Epilepsia 63, 1835–1848 (2022).
Medel-Matus, J.-S. et al. Modification of post-traumatic epilepsy by fecal microbiota transfer. Epilepsy Behav. 134, 108860 (2022).
French, J. A. et al. Characteristics of medial temporal lobe epilepsy: I. Results of history and physical examination. Ann. Neurol. 34, 774–780 (1993).
Löscher, W. The search for new screening models of pharmacoresistant epilepsy: is induction of acute seizures in epileptic rodents a suitable approach? Neurochem. Res. 42, 1926–1938 (2017).
Dudek, F. E. & Staley, K. J. The time course and circuit mechanisms of acquired epileptogenesis. in Jasper’s Basic Mechanisms of the Epilepsies 4th edn (eds Noebels, J. L. et al.) (Oxford Univ. Press, 2012).
Santhakumar, V., Ratzliff, A. D., Jeng, J., Toth, Z. & Soltesz, I. Long-term hyperexcitability in the hippocampus after experimental head trauma. Ann. Neurol. 50, 708–717 (2001).
Dudek, F. E. & Spitz, M. Hypothetical mechanisms for the cellular and neurophysiologic basis of secondary epileptogenesis: proposed role of synaptic reorganization. J. Clin. Neurophysiol. 14, 90–101 (1997).
Cantu, D. et al. Traumatic brain injury increases cortical glutamate network activity by compromising GABAergic control. Cereb. Cortex 25, 2306–2320 (2015).
Lowenstein, D. H., Thomas, M. J., Smith, D. H. & McIntosh, T. K. Selective vulnerability of dentate hilar neurons following traumatic brain injury: a potential mechanistic link between head trauma and disorders of the hippocampus. J. Neurosci. 12, 4846–4853 (1992).
Raible, D. J., Frey, L. C., Cruz Del Angel, Y., Russek, S. J. & Brooks-Kayal, A. R. GABA(A) receptor regulation after experimental traumatic brain injury. J. Neurotrauma 29, 2548–2554 (2012).
Gupta, A., Elgammal, F. S., Proddutur, A., Shah, S. & Santhakumar, V. Decrease in tonic inhibition contributes to increase in dentate semilunar granule cell excitability after brain injury. J. Neurosci. 32, 2523–2537 (2012).
Webster, K. M. et al. Inflammation in epileptogenesis after traumatic brain injury. J. Neuroinflammation 14, 10 (2017).
Hunt, R. F., Scheff, S. W. & Smith, B. N. Synaptic reorganization of inhibitory hilar interneuron circuitry after traumatic brain injury in mice. J. Neurosci. 31, 6880–6890 (2011).
Bolkvadze, T., Puhakka, N. & Pitkänen, A. Epileptogenesis after traumatic brain injury in Plaur-deficient mice. Epilepsy Behav. 60, 187–196 (2016).
Kumar, P. et al. Single-cell transcriptomics and surface epitope detection in human brain epileptic lesions identifies pro-inflammatory signaling. Nat. Neurosci. 25, 956–966 (2022).
Srinivasan, D., Yen, J.-H., Joseph, D. J. & Friedman, W. Cell type-specific interleukin-1beta signaling in the CNS. J. Neurosci. 24, 6482–6488 (2004).
Shiozaki, T. et al. Cerebrospinal fluid concentrations of anti-inflammatory mediators in early-phase severe traumatic brain injury. Shock 23, 406–410 (2005).
Fan, L. et al. Experimental brain injury induces expression of interleukin-1 beta mRNA in the rat brain. Brain Res. Mol. Brain Res. 30, 125–130 (1995).
Clausen, F. et al. Neutralization of interleukin-1beta modifies the inflammatory response and improves histological and cognitive outcome following traumatic brain injury in mice. Eur. J. Neurosci. 30, 385–396 (2009).
Scaffidi, P., Misteli, T. & Bianchi, M. E. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature 418, 191–195 (2002).
Shi, Y., Zhang, L., Teng, J. & Miao, W. HMGB1 mediates microglia activation via the TLR4/NF-κB pathway in coriaria lactone induced epilepsy. Mol. Med. Rep. 17, 5125–5131 (2018).
Chiavegato, A., Zurolo, E., Losi, G., Aronica, E. & Carmignoto, G. The inflammatory molecules IL-1β and HMGB1 can rapidly enhance focal seizure generation in a brain slice model of temporal lobe epilepsy. Front. Cell. Neurosci. 8, 155 (2014).
Semple, B. D., Kossmann, T. & Morganti-Kossmann, M. C. Role of chemokines in CNS health and pathology: a focus on the CCL2/CCR2 and CXCL8/CXCR2 networks. J. Cereb. Blood Flow Metab. 30, 459–473 (2010).
Gosselin, R. D. et al. Constitutive expression of CCR2 chemokine receptor and inhibition by MCP-1/CCL2 of GABA-induced currents in spinal cord neurones. J. Neurochem. 95, 1023–1034 (2005).
Patabendige, A. & Janigro, D. The role of the blood–brain barrier during neurological disease and infection. Biochem. Soc. Trans. 51, 613–626 (2023).
Marchi, N., Granata, T., Alexopoulos, A. & Janigro, D. The blood–brain barrier hypothesis in drug resistant epilepsy. Brain 135, e211 (2012).
Bargerstock, E. et al. Is peripheral immunity regulated by blood–brain barrier permeability changes? PLoS ONE 9, e101477 (2014).
Dadas, A. & Janigro, D. Breakdown of blood–brain barrier as a mechanism of post-traumatic epilepsy. Neurobiol. Dis. 123, 20–26 (2019).
Weissberg, I. et al. Albumin induces excitatory synaptogenesis through astrocytic TGF-β/ALK5 signaling in a model of acquired epilepsy following blood–brain barrier dysfunction. Neurobiol. Dis. 78, 115–125 (2015).
Ivens, S. et al. TGF-beta receptor-mediated albumin uptake into astrocytes is involved in neocortical epileptogenesis. Brain 130, 535–547 (2007).
Saletti, P. G. et al. In search of antiepileptogenic treatments for post-traumatic epilepsy. Neurobiol. Dis. 123, 86–99 (2019).
Kendirli, M. T., Rose, D. T. & Bertram, E. H. A model of posttraumatic epilepsy after penetrating brain injuries: effect of lesion size and metal fragments. Epilepsia 55, 1969–1977 (2014).
Takei, N. & Nawa, H. mTOR signaling and its roles in normal and abnormal brain development. Front. Mol. Neurosci. 7, 28 (2014).
Lee, D. Y. Roles of mTOR signaling in brain development. Exp. Neurobiol. 24, 177–185 (2015).
Butler, C. R., Boychuk, J. A. & Smith, B. N. Effects of rapamycin treatment on neurogenesis and synaptic reorganization in the dentate gyrus after controlled cortical impact injury in mice. Front. Syst. Neurosci. 9, 163 (2015).
Niu, L.-J., Xu, R.-X., Zhang, P., Du, M.-X. & Jiang, X.-D. Suppression of Frizzled-2-mediated Wnt/Ca2+ signaling significantly attenuates intracellular calcium accumulation in vitro and in a rat model of traumatic brain injury. Neuroscience 213, 19–28 (2012).
Mardones, M. D. & Gupta, K. Transcriptome profiling of the hippocampal seizure network implicates a role for Wnt signaling during epileptogenesis in a mouse model of temporal lobe epilepsy. Int. J. Mol. Sci. 23, 12030 (2022).
Gupta, K. & Schnell, E. Neuronal network remodeling and Wnt pathway dysregulation in the intra-hippocampal kainate mouse model of temporal lobe epilepsy. PLoS ONE 14, e0215789 (2019).
Raza, M. et al. Evidence that injury-induced changes in hippocampal neuronal calcium dynamics during epileptogenesis cause acquired epilepsy. Proc. Natl Acad. Sci. USA 101, 17522–17527 (2004).
Powell, K. L., Cain, S. M., Snutch, T. P. & O’Brien, T. J. Low threshold T-type calcium channels as targets for novel epilepsy treatments. Br. J. Clin. Pharm. 77, 729–739 (2014).
Conboy, K., Henshall, D. C. & Brennan, G. P. Epigenetic principles underlying epileptogenesis and epilepsy syndromes. Neurobiol. Dis. 148, 105179 (2021).
Dębski, K. J. et al. Etiology matters — genomic DNA methylation patterns in three rat models of acquired epilepsy. Sci. Rep. 6, 25668 (2016).
Nelson, E. D., Kavalali, E. T. & Monteggia, L. M. Activity-dependent suppression of miniature neurotransmission through the regulation of DNA methylation. J. Neurosci. 28, 395–406 (2008).
Machnes, Z. M. et al. DNA methylation mediates persistent epileptiform activity in vitro and in vivo. PLoS ONE 8, e76299 (2013).
Deutsch, S. I., Mastropaolo, J., Burket, J. A. & Rosse, R. B. An epigenetic intervention interacts with genetic strain differences to modulate the stress-induced reduction of flurazepam’s antiseizure efficacy in the mouse. Eur. Neuropsychopharmacol. 19, 398–401 (2009).
Perez-Pinera, P. et al. RNA-guided gene activation by CRISPR-Cas9-based transcription factors. Nat. Methods 10, 973–976 (2013).
Dominguez, A. A., Lim, W. A. & Qi, L. S. Beyond editing: repurposing CRISPR-Cas9 for precision genome regulation and interrogation. Nat. Rev. Mol. Cell Biol. 17, 5–15 (2016).
Sasa, M. A new frontier in epilepsy: novel antiepileptogenic drugs. J. Pharmacol. Sci. 100, 487–494 (2006).
Brady, R. D. et al. Modelling traumatic brain injury and posttraumatic epilepsy in rodents. Neurobiol. Dis. 123, 8–19 (2020).
Ford, I. & Norrie, J. Pragmatic trials. N. Engl. J. Med. 375, 454–463 (2016).
Casey, J. D., Beskow, L. M. & Brown, J. Use of pragmatic and explanatory trial designs in acute care research: lessons from COVID-19. Lancet Respir. Med. 10, 700–714 (2022).
Braun, R. It’s been a TRACK-TBI LONG time coming but well worth the wait. Neurology 101, 287–289 (2023).
McCrea, M. A. et al. Functional outcomes over the first year after moderate to severe traumatic brain injury in the prospective, longitudinal TRACK-TBI study. JAMA Neurol. 78, 982–992 (2021).
Andrews, P. J. et al. Therapeutic hypothermia to reduce intracranial pressure after traumatic brain injury: the Eurotherm3235 RCT. Health Technol. Assess. 22, 1–134 (2018).
Bastian, L. A. et al. Stakeholder engagement in pragmatic clinical trials: emphasizing relationships to improve pain management delivery and outcomes. Pain Med. 21, S13–S20 (2020).
Morain, S. & Largent, E. Think pragmatically: investigators’ obligations to patient-subjects when research is embedded in care. Am. J. Bioeth. 23, 10–21 (2023).
Diaz, V. Encouraging participation of minorities in research studies. Ann. Fam. Med. 10, 372–373 (2012).
Boden-Albala, B. et al. Use of community-engaged research approaches in clinical interventions for neurologic disorders in the United States. Neurology 101, S27–S46 (2023).
Griffith, D. M., Towfighi, A., Manson, S. M., Littlejohn, E. L. & Skolarus, L. E. Determinants of inequities in neurologic disease, health, and well-being: the NINDS Social Determinants of Health Framework. Neurology 101, S75–S81 (2023).
Danziger, J. et al. Temporal trends in critical care outcomes in U.S. minority-serving hospitals. Am. J. Respir. Crit. Care Med 201, 681–687 (2020).
Kanter, G. P., Segal, A. G. & Groeneveld, P. W. Income disparities in access to critical care services. Health Aff. 39, 1362–1367 (2020).
Nayfeh, A. & Fowler, R. A. Understanding patient- and hospital-level factors leading to differences, and disparities, in critical care. Am. J. Respir. Crit. Care Med 201, 642–644 (2020).
Brown, K. E., Fohner, A. E. & Woodahl, E. L. Beyond the individual: community-centric approaches to increase diversity in biomedical research. Clin. Pharmacol. Ther. 113, 509–517 (2023).
Benizri, N., Hallot, S., Burns, K. & Goldfarb, M. Patient and family representation in randomized clinical trials published in 3 medical and surgical journals: a systematic review. JAMA Netw. Open 5, e2230858 (2022).
Gill, M. et al. Patient and family member-led research in the intensive care unit: a novel approach to patient-centered research. PLoS ONE 11, e0160947 (2016).
Fairley, R. et al. Increasing clinical trial participation of Black women diagnosed with breast cancer. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-023-01644-z (2023).
Barrett, N. J. et al. Factors associated with biomedical research participation within community-based samples across 3 National Cancer Institute-designated cancer centers. Cancer 126, 1077–1089 (2020).
Miles, S. R. et al. Evolution of irritability, anger, and aggression after traumatic brain injury: identifying and predicting subgroups. J. Neurotrauma 38, 1827–1833 (2021).
Driver, S., Reynolds, M. & Kramer, K. Modifying an evidence-based lifestyle programme for individuals with traumatic brain injury. Brain Inj. 31, 1612–1616 (2017).
Sutton, K. M. et al. Engaging individuals with neurological conditions and caregivers in rural communities in a health research team. Prog. Community Health Partnersh. 13, 129–139 (2019).
Shimia, M. et al. A placebo-controlled randomized clinical trial of amantadine hydrochloride for evaluating the functional improvement of patients following severe acute traumatic brain injury. J. Neurosurg. Sci. 67, 598–604 (2023).
Morey, C. E., Cilo, M., Berry, J. & Cusick, C. The effect of Aricept in persons with persistent memory disorder following traumatic brain injury: a pilot study. Brain Inj. 17, 809–815 (2003).
Jha, A. et al. A randomized trial of modafinil for the treatment of fatigue and excessive daytime sleepiness in individuals with chronic traumatic brain injury. J. Head Trauma Rehabil. 23, 52–63 (2008).
Shultz, S. R. et al. Sodium selenate reduces hyperphosphorylated tau and improves outcomes after traumatic brain injury. Brain 138, 1297–1313 (2015).
Liu, S.-J. et al. Sodium selenate retards epileptogenesis in acquired epilepsy models reversing changes in protein phosphatase 2A and hyperphosphorylated tau. Brain 139, 1919–1938 (2016).
Li, Z. et al. Iron neurotoxicity and protection by deferoxamine in intracerebral hemorrhage. Front. Mol. Neurosci. 15, 927334 (2022).
Terrone, G., Balosso, S., Pauletti, A., Ravizza, T. & Vezzani, A. Inflammation and reactive oxygen species as disease modifiers in epilepsy. Neuropharmacology 167, 107742 (2020).
Serrano, G. E. et al. Ablation of cyclooxygenase-2 in forebrain neurons is neuroprotective and dampens brain inflammation after status epilepticus. J. Neurosci. 31, 14850–14860 (2011).
Desjardins, P. et al. Induction of astrocytic cyclooxygenase-2 in epileptic patients with hippocampal sclerosis. Neurochem. Int. 42, 299–303 (2003).
Löscher, W. & Friedman, A. Structural, molecular, and functional alterations of the blood–brain barrier during epileptogenesis and epilepsy: a cause, consequence, or both? Int. J. Mol. Sci. 21, 591 (2020).
Henshall, D. C. & Kobow, K. Epigenetics and epilepsy. Cold Spring Harb. Perspect. Med. 5, a022731 (2015).
Guo, D., Zeng, L., Brody, D. L. & Wong, M. Rapamycin attenuates the development of posttraumatic epilepsy in a mouse model of traumatic brain injury. PLoS ONE 8, e64078 (2013).
Galanopoulou, A. S., Gorter, J. A. & Cepeda, C. Finding a better drug for epilepsy: the mTOR pathway as an antiepileptogenic target. Epilepsia 53, 1119–1130 (2012).
Coulter, D. A. & Steinhäuser, C. Role of astrocytes in epilepsy. Cold Spring Harb. Perspect. Med. 5, a022434 (2015).
Acknowledgements
The authors thank Christopher Brown (Indiana University) for his contributions to the design of the figures for this manuscript.
Author information
Authors and Affiliations
Contributions
M.P., K.G., S.M., A.G., D.O.O., J.G.-M., L.S. and J.F.C. researched data for the article. All authors contributed substantially to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S.M. is the Charles Frost Chair in Neurosurgery and Neurology and partially funded by grants from NIH U54 NS100064 (EpiBioS4Rx), R01-NS43209 and R01-NS127524, the US Department of Defense (W81XWH-22-1-0510, W81XWH-22-1-0210), a pilot grant from the National Institute of Child Health and Human Development (NICHD) centre grant (P50 HD105352) for the Rose F. Kennedy Intellectual and Developmental Disabilities Research Center (RFK-IDDRC), the Heffer Family and the Segal Family Foundations, the Isabelle Rapin and Harold Oaklander Child Neurology Research Fund in the Isabelle Rapin Child Neurology Division and the Abbe Goldstein/Joshua Lurie and Laurie Marsh/Dan Levitz families. He is on the editorial boards of Brain and Development, Paediatric Neurology, Annals of Neurology, MedLink and Physiological Research. He receives compensation from MedLink for his work as Associate Editor; and royalties from books he co-edited. A.G. acknowledges research grant support from NINDS R01-NS127524, US Department of Defense (W81XWH-22-1-0210, W81XWH-22-1-0510, EP220067), a pilot grant from the NICHD centre grant (P50 HD105352) for the RFK-IDDRC, R01-DA019473, R01-AI164864, the Heffer Family and the Segal Family Foundations, the Isabelle Rapin and Harold Oaklander Child Neurology Research Fund in the Isabelle Rapin Child Neurology Division and the Abbe Goldstein/Joshua Lurie and Laurie Marsh/Dan Levitz families. She is the Editor-in-Chief of Epilepsia Open and associate editor of Neurobiology of Disease and receives royalties from Elsevier, Walters Kluwer and MedLink for publications. J.G.-M. receives consulting fees for Zimmer Biomet. D.C. receives compensation as lead editor for the Brain and Life podcast for the American Academy of Neurology and is co-editor of a new textbook on health equity among neurological disorders including chapters on traumatic brain injury and epilepsy. J.F.C. and K.G. accept fees from NeuroOne Medical Technologies Corporation for consulting. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks S. Shultz and D. Duncan for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Anti-epileptogenic medications
-
(AEMs). Therapies that ameliorate epileptogenesis, with lasting effects beyond the period of drug exposure.
- Anti-seizure medications
-
(ASMs). Medications that treat seizures but do not modify the process of epileptogenesis or alter the disease course of epilepsy.
- Cerebrospinal fluid shunting
-
A common neurosurgical procedure to drain cerebrospinal fluid, usually from the ventricular system, thereby decreasing intracranial pressure.
- Encephalomalacia
-
A radiological finding denoting an area of brain tissue that has undergone liquefactive necrosis.
- Engel Epilepsy Surgery Outcome Scale
-
A classification scheme of seizure outcomes after epilepsy surgery using four classes: 1, free of disabling seizures; 2, rare disabling seizures; 3, worthwhile improvement; and 4, no worthwhile improvement.
- Extended GOS
-
(GOSE). An extension of the Glasgow Outcome Scale that subdivides the categories of severe disability, moderate disability and good recovery into lower and upper categories.
- Glasgow Coma Scale
-
(GCS). A broadly utilized clinical scale describing the level of consciousness after traumatic injury.
- Glasgow Outcome Scale
-
(GOS). A global scale for functional outcome after brain injury that rates patient status using five categories: dead, vegetative state, severe disability, moderate disability and good recovery.
- Mild TBI
-
Traumatic brain injury with post-impact (may not need resuscitation) Glasgow Coma Scale score 13–15.
- Moderate TBI
-
Traumatic brain injury with post-resuscitation Glasgow Coma Scale score 9–12.
- Pathological posturing responses
-
Stereotypical movements of the trunk and extremities in response to stimuli, typically indicative of significant CNS injury.
- Severe TBI
-
Traumatic brain injury with post-resuscitation Glasgow Coma Scale score ≤ 8.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pease, M., Gupta, K., Moshé, S.L. et al. Insights into epileptogenesis from post-traumatic epilepsy. Nat Rev Neurol (2024). https://doi.org/10.1038/s41582-024-00954-y
Accepted:
Published:
DOI: https://doi.org/10.1038/s41582-024-00954-y



