Abstract
Acute kidney injury (AKI), which is a common complication of acute illnesses, affects the health of individuals in community, acute care and post-acute care settings. Although the recognition, prevention and management of AKI has advanced over the past decades, its incidence and related morbidity, mortality and health care burden remain overwhelming. The rapid growth of digital technologies has provided a new platform to improve patient care, and reports show demonstrable benefits in care processes and, in some instances, in patient outcomes. However, despite great progress, the potential benefits of using digital technology to manage AKI has not yet been fully explored or implemented in clinical practice. Digital health studies in AKI have shown variable evidence of benefits, and the digital divide means that access to digital technologies is not equitable. Upstream research and development costs, limited stakeholder participation and acceptance, and poor scalability of digital health solutions have hindered their widespread implementation and use. Here, we provide recommendations from the Acute Disease Quality Initiative consensus meeting, which involved experts in adult and paediatric nephrology, critical care, pharmacy and data science, at which the use of digital health for risk prediction, prevention, identification and management of AKI and its consequences was discussed.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common complication of acute illnesses and can occur in the community, and in acute or post-acute care settings. AKI is associated with considerable clinical outcomes and health care costs1,2,3. However, despite knowledge advances and technological innovations, improvements in the care and outcomes of patients with AKI worldwide have been limited. Digital innovation in medical technologies — digital health — is increasingly used in modern health care4,5. Digital health has been introduced and implemented in multiple domains and offers numerous opportunities to improve care throughout the AKI care continuum. This continuum comprises various interconnected states — AKI risk, kidney injury or dysfunction, and associated short- and long-term outcomes — and therefore encompasses AKI prevention, early recognition, management and recovery of patients, some of whom will be receiving dialysis6,7. Importantly, inequitable access to technology, also termed the ‘digital divide’, limits the potential benefits of digital health. The 27th Acute Disease Quality Initiative (ADQI) conference was convened to develop a framework for appropriate development, validation and implementation of digital health in AKI care (DHAKI).
Methods
The 27th ADQI Consensus Conference included a diverse panel of 30 participants who represented relevant disciplines, including paediatric and adult nephrology, critical care medicine, pharmacy, data science, ethics and digital law, from North America, South America and Europe. The consensus meeting followed the established ADQI process, using a modified Delphi method, as previously described8. The broad objective of ADQI is to assess current knowledge and provide expertise-based statements that can guide clinicians and investigators, and to identify clinical research priorities to address gaps in knowledge. The 27th ADQI consensus meeting focused on DHAKI and was held over 2.5 days in San Diego, California, USA, on 4–6 March 2022.
The activities at the consensus conference were divided into three parts. The pre-conference activities involved a comprehensive search of the literature for assessment of the current evidence related to the diagnostic and management strategies for the AKI continuum, including acute and post-acute care, as well as care in the community, using digital health solutions. Each workgroup was tasked with summarizing the scope, implementation and evaluation strategies currently used to develop, validate, and implement DHAKI-driven solutions. Using virtual meetings, each workgroup identified the current state of knowledge to enable the formulation of the main questions from which discussion and consensus would be developed before the panel meeting. The consensus meeting included several breakout sessions, during which each group created their consensus positions and recommendations, before sharing, debating and refining them in a plenary session, which involved the whole panel. This process (modified Delphi) was repeated three times during the conference before the final statements were formulated and shared with the entire group. After the meeting, the summary reports from each group were collated to generate a report and summary recommendations, followed by revision and approval by all ADQI participants.
Current digital health landscape
What is digital health?
Consensus statements
-
1.
Digital health can be described as a strategy to transform the quality of health care delivery and improve outcomes using digital solutions.
-
2.
Digital health solutions generate and analyse data from individuals, health systems and populations to connect patients, care partners and professionals across the health care continuum, create opportunities to foster shared decision-making, improve the quality of health care delivery and promote learning across health care systems.
According to the FDA, digital health can improve health care and health outcomes by unifying people, information, technology and connectivity9. People are the central focus and include all the stakeholders involved in the design, development, implementation, delivery and use of health care (that is, patients, caregivers, communities, health care workforce, technology developers and policymakers). Information encompasses traditional data (for example, data created through the process of care delivery, such as electronic health records (EHRs), and imaging or device data), as well as emerging data sources (for example, from wearables, or societal and environmental data). Technologies refer to existing and emerging computational and engineering methods that can be used to improve health care delivery, efficiency, experience and outcomes. Finally, digital health strengthens connectivity by enhancing relationships and interactions within the health care system to improve access, empower shared decision-making, enable patient engagement, foster quality improvement and improve health outcomes10.
Notably, despite this positive potential, digital health can also have unintended negative consequences, such as provider or patient dissatisfaction, and increased resource utilization. Such potential negative outcomes should therefore be anticipated, recognized and addressed. Moreover, the ethical, legal and social implications (ELSIs) of digital health, which are relevant to all areas of its development, use and regulation, must also be considered. For example, the interplay between inequities and algorithm bias, regulatory aspects (data protection, security, privacy and consent), liability, accountability and trust. Of note, the rapid pace of innovation in digital health solutions demands the use of a simplified and well-defined language that can be used to describe them and their unintended ELSIs (Supplementary Table 1).
What are the categories of digital health solutions?
Consensus statements
-
1.
Digital health tools include the technologies (for example, computing platforms, connectivity, software, hardware and sensors), infrastructure and various applications, upon which digital health strategy is built and deployed. Most digital health solutions can be classified into broad categories, including health information technology (HIT), artificial intelligence (AI), telehealth and virtual care, mobile health applications (mHealth), wearables and devices, and digitally-enabled therapeutics (DTx). These categories are neither exhaustive nor mutually exclusive.
-
2.
Digital health solutions can be customized for different contexts (for example, specific country or health jurisdictions) and across the care continuum. This customization is enabled by core infrastructure and technologies such as standardized and interoperable data, AI, cloud computing platforms, cybersecurity, sensors and communication channels.
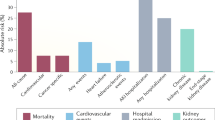
The expansion of digital health is driven by the promise of access (through remote monitoring and management) to efficient and high-quality health care services (point-of-care access and clinical decision support). The integration of digital health into current standard of care should therefore lead to improved personalized health care, with greater health autonomy (through better patient engagement and shared decision-making) and empowerment for individuals to enable informed health decisions, and improved population-level interventions (that is, public health initiatives)11,12. Digital health could therefore improve clinical care and outcomes in several domains (Fig. 1).
A digital health strategy centres around the patient and involves digital health tools deployed with intention across different settings. Importantly, because digital health can have unintended consequences, ethical, legal and social principles must be embedded into digital health solutions as they mature. Adapted from the Acute Dialysis Quality Initiative143, CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/). AI, artificial intelligence; FAIR, findable, accessible, interoperable and reusable.
Health information technology
HIT involves the processing, storing and exchanging of health information in an electronic environment. EHRs are a vital part of HIT as they contain the medical and treatment histories of patients. These records can be integrated with clinical-decision support tools that health care professionals and patients can use to make health care decisions, and that enable automation and streamlining of health care professional workflows.
Artificial or augmented intelligence
Although health systems are increasingly turning to artificial intelligence (AI) to accelerate the informed decision process, we must emphasize that the judgment of health care professionals still has a crucial role in the decision-making process13. AI is an umbrella term that encompasses machine learning (ML) techniques, algorithms and software applications that mirror and support human decision-making by integrating, analysing and using health care data. Augmented intelligence uses AI to assist, facilitate, nudge and enhance human decision-making by leveraging computational methods such as machine or deep learning.
Telehealth and virtual care
Telehealth, also termed telemedicine, enables health care professionals to provide health care through electronic information and telecommunication technologies. Telehealth strategies came to the fore during the COVID-19 pandemic and have been used successfully to improve kidney care14.
Mobile health
mHealth is defined as medical and public health practice that is facilitated by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants and other wireless tools15.
Wearable sensors and devices
Innovations in wearables, hearables (that is, in-ear devices), and nearables (that is, neighbouring devices that interact with wearables) are transforming health care delivery, especially given the widespread availability of smartphones16. In addition, continuous progress in the miniaturization of integrated electronics has lowered the prices, size, weight and energy consumption of electronic sensors, while increasing their processing power, memory and wireless connectivity. Combined, these factors have boosted opportunities for wearable medical sensors to improve patient care across the care continuum. Notably, wearable biosensor technologies can be used to influence human behaviour, provide enhanced care at home, facilitate remote consults, patient education and connection with peer networks.
Digitally enabled therapeutics
DTx are evidence-based therapeutic interventions delivered to patients through software programs17. Although the role of DTx in AKI is not yet well-defined, several DTx tools have been successfully implemented in clinical care18. A relevant example of DTx includes fully automated and individualized insulin dosing using real-time glycaemic status data in patients with insulin-dependent diabetes mellitus19.
Current DHAKI status
What is the evidence that digital health influences patient outcomes in the AKI continuum?
Consensus statements
-
1.
AKI alerts driven by concrete criteria improve early detection and prompt AKI management.
-
2.
Risk prediction models based on machine learning (ML) and/or AI might improve the identification of patients at a high risk of AKI who could benefit from tailored surveillance and primary prevention.
-
3.
The utility of ML- and/or AI-driven clinical decision support system (CDSS) tools to improve early recognition of AKI within the appropriate context, and to enable a multidisciplinary team to manage a patient through preventive and therapeutic interventions should be evaluated.
Most studies that evaluated electronic AKI alerts were retrospective and observational, although a few prospective observational quality improvement projects, quasi-experimental before-and-after studies and some randomized controlled trials (RCTs) have also been performed. These investigations were mostly directed at AKI recognition to facilitate timely patient management20,21,22,23. CDSS alert systems can recognize all stages of AKI. As most patients have stage 1 AKI at the time of detection, focusing on and implementing a directed intervention for patients with stage 1 AKI at a high risk of progression to stage 2 might be more useful than including all patients with stage 1 as most of these patients will only have transient kidney impairment. CDSS studies with patients at a high risk of AKI mainly include critically ill patients receiving nephrotoxins. The use of CDSS in these cases improved AKI documentation, recognition and response time21,24,25,26,27,28, and reduced nephrotoxin administration27,29,30,31. Of note, in most studies of such screening tools, the focus on achieving high alert sensitivity led to high numbers of false positives, which can cause alert fatigue and might dilute any improvements in relevant outcomes32.
Several kidney-related outcomes have also been evaluated, including AKI duration and progression, length of hospital stay, and the need for kidney replacement therapy (KRT)28,30,31,33,34,35. Among patients who have already developed AKI, digital health might also be used to guide the personalized prescription of medication or KRT36,37,38, or to manage complications associated with AKI and dialysis (for example, intradialytic hypotension39). However, findings on kidney-related outcomes have been inconsistent. Importantly, given that many of these CDSS alerts were designed for AKI recognition rather than as a clinical intervention, an effect on clinical and patient-centreed outcomes might have been unlikely28,30,32,33,40,41,42,43. Of note, prospective RCTs and quality improvement studies that demonstrated improvements in kidney-related outcomes focused on risk and recognition, and typically involved a multidisciplinary team equipped with informatic resources31,34,42. Improved management of multidisciplinary teams is a proposed solution to improve processes of care and might therefore have contributed to the success of these CDSS-related trials44. Importantly, successful DHAKI adoption and implementation will require stakeholder engagement, which rarely occurs in prospective evaluations45.
As risk-based models for generating CDSS evolve, ML and the increasing digitalization of patient data yield opportunities for greater accuracy and timely prediction of AKI risk. In predominantly retrospective settings, researchers have demonstrated the ability of ML to predict AKI up to 48 h before onset46,47,48,49,50,51,52,53,54 using routinely collected inpatient clinical data. Robust external validation55 and evidence of transportability across sites56 are promising, but the lack of prospective implementation and analysis of the clinical impact are significant gaps in the current literature. Any clinical benefits of digital health solutions will be more palpable as preventative or therapeutic strategies for AKI are developed and implemented. The potential successes of AKI prediction models in improving care processes or patient outcomes depend on the scale and scope of the datasets used to develop and validate these models. In addition, the explainability, adaptability and portability of these models affect their implementation and ability to guide feasible interventions that can affect relevant outcomes. However, nearly all current studies are limited by data inadequacy, whether in sample size or diversity, or by a lack of robust validation. Inadequate data transparency remains another substantial limitation. Furthermore, studies on the use of digital health solutions for the management of AKI are nearly impossible to replicate, as their findings are heavily dependent on the context of their development, applications and populations. Thus, drawing broad conclusions about these solutions is challenging without consensus standards for data management procedures, such as data harmonization and interoperability.
Is there evidence that digital health influences population outcomes along the AKI continuum?
Consensus statements
-
1.
The digital health influence on the AKI continuum at a population level is insufficiently addressed in the current literature.
-
2.
Health system-wide and/or nationwide population-based studies should be considered for DHAKI to assess its possible benefits, implementation barriers, costs, ease of use and portability, establish benchmarking for quality of care, and examine possible disadvantages in clinical practice.
Fewer CDSS alert studies have focused on population-based assessments compared with those using patient-level evaluations57,58,59,60,61,62,63. Nonetheless, current data suggest that AKI recognition through passive, non-interruptive alerts improves AKI documentation and remuneration28. However, population-based evaluations lack granularity with regard to the intervention details, leaving clinicians uncertain about optimal implementation strategies.
Is there evidence of the utility of digital health for AKI management across different clinical settings?
Consensus statements
-
1.
The evidence of digital health use for AKI recognition, risk classification, phenotyping and management in clinical settings has mainly originated from large academic tertiary care centres in resource-rich areas.
-
2.
DHAKI studies would benefit from differentiating AKI recognition and management in ambulatory compared with hospitalized settings, as well as in intensive care unit (ICU) compared with non-ICU settings across areas with different resource levels.
-
3.
The implementation of telehealth to support remote AKI and dialysis care in resource-limited areas will require additional investigation to assess adoption rates, utility and outcomes.
Current evidence on AKI alerts combined with ML and/or AI models used data from selected hospitalized patients in the ICU54,64,65,66, in perioperative settings67,68,69 or in the emergency department70. Of note, these have been primarily studies conducted in single health care settings in well-resourced areas. Data from community centres, particularly in resource-limited regions, are limited but the International Society of Nephrology’s 0by25 initiative, which is an ongoing feasibility study focused on resource-limited areas, shows that a digital health strategy using telemedicine, coupled with an education programme and a point-of-care kidney function test for risk assessment, can identify AKI early, and guide treatment and patient education71. These findings support the feasibility of DHAKI implementation within integrated health systems in low-to-middle-income areas.
Successful teledialysis assessment for remote KRT management in rural acute care hospitals72,73 suggests that this approach should be investigated further. Importantly, legal issues, costs and outcomes of AKI telemedicine remain unclear74.
Is there evidence that DHAKI can be used for post-AKI management?
Consensus statement
-
1.
The utility of DHAKI in post-AKI management remains unclear, and substantial knowledge gaps must be addressed to determine the potential role of DHAKI in:
-
monitoring of kidney health in AKI survivors and patients at risk of CKD development or progression in ambulatory settings.
-
patient and clinician education through mobile applications.
-
patient and caregiver empowerment through enhanced self-care.
Transitioning between the hospital and outpatient settings following AKI is challenging, and rehospitalizations are common75,76. DHAKI could empower patients to make informed decisions regarding their kidney health, especially during AKI recovery. However, although CDSS facilitates timely clinician recognition of AKI and subsequent intervention, these systems are not yet optimized to engage patients and caregivers. The role of digital mHealth applications and wearables has not been explored in AKI aftercare but, among patients with CKD or kidney transplant recipients, mHealth has had positive effects on medication adherence and safety77,78,79. Wearables were also beneficial in blood pressure monitoring, volume status assessment and oxygen saturation80,81. Future studies could focus on DHAKI-focused interventions that begin at or shortly after discharge82.
DHAKI use in AKI management
How should digital health be applied along the AKI care continuum?
Consensus statements
-
1.
Patients and health care providers could use digital health to improve AKI risk stratification and recognition, personalize care, including the use of KRT, and optimize AKI recovery and follow-up.
-
2.
Digital health could guide resource allocation, surveillance and data integration at the health care system or population level.
Digital health could guide resource allocation by deploying and activating hospital and community nephrology rapid response teams (NRRTs) to identify patients at risk of AKI83. Population data from public health sources, integrated with social determinants of health, could be used to monitor trends in the incidence of community AKI and identify novel environmental risk factors. Numerous layers of digital patient health could be integrated through digital health technology, infrastructure and applications. Digital health could also influence patient care with prompts and appropriate alerts for AKI complications among patients at a high risk after hospital discharge. Digital health tools can also interface with pharmacists, nurses, primary care physicians and nephrologists to provide continuous updates on the kidney function of a patient and facilitate timely, guided and personalized treatment recommendations. For example, a digital health tool could guide avoidance of nephrotoxic medications in patients at a high risk, personalized resuscitation or de-resuscitation based on wearable technology, and AI-guided drug dose adjustment (Fig. 2).
Digital health solutions across the acute kidney injury (AKI) continuum could apply to the community, acute and post-acute care settings. The digital profile of individual patients, which is sourced from patient-related information, health care systems and population data, could be used to risk stratify patients for AKI, identify patients with AKI, tailor the clinical response to the risk or presence of AKI, and expedite AKI recovery in different settings. Adapted from the Acute Dialysis Quality Initiative143, CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/). AI, artificial intelligence; CKD, chronic kidney disease; FAIR, findable, accessible, interoperable and reusable; HIT, health information technology; KRT, kidney replacement therapy; mHealth, mobile health.
In addition to the acute care setting, digital health tools such as point-of-care testing and wearable biosensors could be deployed in the community and in post-acute care to select patients at a high risk. For example, biosensor-enabled Bluetooth home toilet systems can provide biochemical urinalysis by integrating test strips84. Other applications of digital health solutions include monitoring kidney function in the community among patients who are at a high risk because they receive nephrotoxic medications, tracking the AKI-to-CKD transition by detecting the onset or progression of albuminuria early, or the development of cardiovascular diseases. Identifying such patients through these approaches could guide the implementation of evidence-based post-AKI long-term follow-up and prevention strategies. Approaches such as telemedicine-enabled virtual AKI clinics can prevent rehospitalization and reduce overburdening of patients or health care systems73.
Where in the AKI continuum could digital health be applied to improve care?
Consensus statements
-
1.
Digital health could be applied in community (for example, at home or in pharmacies), acute (for example, emergency department, hospital ward or ICU), and post-acute (for example, in ambulatory care or skilled nursing facilities) care settings. Digital health solutions must be adapted to the available resources, data and technology to maintain continuity across settings.
-
2.
DHAKI stakeholders include patients, care partners, multidisciplinary clinicians, administrators, public health personnel, policymakers, payors, legal experts and industry.
Digital health solutions need to be validated in diverse cohorts across various AKI care continuums (Supplementary Table 2). These solutions must be acceptable and accessible to patients, providers and payors across different health care settings. Digital health could increase connectedness to transform AKI care, particularly if these solutions seamlessly cross the continuum of care to limit disruptions. For example, patients can receive virtual health coaching85 before admission for a procedure associated with a high risk of AKI, followed by EHR-embedded risk prediction throughout the hospitalization period to deliver context-appropriate CDSS alerts or prompts to the care team86, followed by the use of wearables and remote monitoring to facilitate safe post-dismissal care and early detection of deterioration or complications87 (Fig. 2).
Digital health applications must also be tailored to the available data, technology and resources. For example, using mobile phones and point-of-care tests in community and resource-limited settings could improve AKI detection and management71. In resource-intensive settings such as ICUs, digital health could be used to phenotype AKI and predict individual risks and responses to interventions49. (Supplementary Table 2).
How could digital health advance care quality, safety and education in AKI for patients, care providers and health systems?
Consensus statements
-
1.
Digital health solutions for the AKI care continuum can improve access, timeliness, care coordination, self-management support, education, safety monitoring, quality, outcomes and the delivery of personalized care.
-
2.
Digital health could improve clinical decision-making and care quality through the development, standardization and monitoring of adherence to best practices, context-appropriate CDSS, resource allocation and suitability of care.
Digital systems have been used to improve the quality and safety of AKI care. EHRs have enabled the real-time or near real-time activation of NRRTs86. For example, the UK National Health Service (NHS) introduced a standardized electronic detection system for creatinine to decrease time-to-management88. For EHRs that support CDSS, computerized provider order entry and electronic prescribing, alerts related to rising creatinine can notify the clinical team or the patient via the EHR system or messaging, thereby providing real-time advice on the appropriate course of action and treatment choices89, sending an alert to a pharmacist or to an NRRT to prompt action90,91, and promote AKI prediction and earlier diagnosis92. The effects of employing similar systems to improve the quality of care throughout the AKI care continuum should be evaluated.
How could digital health advance AKI research?
Consensus statements
-
1.
Digital health supports discovery science and applied precision medicine by identifying causal pathways, social determinants and mechanisms of AKI, as well as enabling diagnostic and therapeutic discoveries, phenotyping and personalization.
-
2.
Digital health facilitates research across the AKI continuum through enhanced patient engagement, enrolment, intervention allocation in clinical trials, data collection, analysis and dissemination.
-
3.
Digital health interventions warrant independent evaluation for their use along the AKI continuum and within various cohorts (for example, paediatric and adult patients).
Potential applications of digital health technologies extend across the research spectrum from discovery to translational science. AI and/or ML now have an integral role in phenotyping, endotyping and genotyping kidney injury for individualized treatments, as well as in biomarker and drug discovery. Digital health solutions can target specific populations (for example, through enrichment of study populations according to risk profiles), to change the design, conduct and outcomes of AKI-related clinical trials. Other solutions, for example, virtual trial enrolment or the use of patient-collected data (obtained through wearables), can also facilitate patient participation in research and increase community engagement, thereby accelerating the collaborative development of patient-centred research. At a population level, digital health can improve the understanding of AKI by tracking disease epidemiology and augmenting the generation of real-world evidence. Importantly, digital health needs to be evaluated as an intervention itself. The effect of digital health applications on patient outcomes remains promising but is lacking thorough assessment (Supplementary Table 3).
DHAKI implementation
Which principles should guide the implementation of DHAKI solutions?
Consensus statements
-
1.
Implementation of digital health solutions should encompass four phases: exploration, deployment, implementation, and knowledge transfer or broad implementation.
-
2.
Exploration and preparation during the pre-implementation phase should focus on needs assessment, identifying the solution and engaging stakeholders.
Implementation science has delineated approaches and methods to measure the effectiveness of digital health solutions in clinical settings93,94 (Fig. 3). Needs assessment95 is a crucial component of implementation and comprises identifying important clinical problems within the AKI continuum, defining the target population and anticipated outcomes, value proposition, identifying and engaging relevant stakeholders, considering the availability of resources and expertise, assessing the local context and, finally, identifying the most appropriate digital health solution to address the defined needs96. Of note, technology readiness assessment is also important and involves engaging multiple disciplines with thorough knowledge of the available infrastructure, as well as personnel with the requisite expertise, to facilitate the uptake and validation of a digital health solution. Importantly, currently available tools for readiness assessment and implementation can facilitate behaviour change and technology acceptance97.
The four phases of digital health solution implementation include exploring the need and resources, deploying the resources required for successful project conduct, implementing the digital health solution within the workflow, and finally, knowledge transfer and broader implementation of the digital health in acute kidney injury (DHAKI) solution across institutions, regions, countries and globally. Adapted from the Acute Dialysis Quality Initiative143, CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/).
What are the key factors for a successful deployment and implementation of a DHAKI solution?
Consensus statements
Successful implementation of digital health tools requires strategic alignment with institutional priorities to enhance and sustain stakeholder engagement and secure adequate technological, personnel, educational, financial, and administrative resources for deployment, launch, quality assurance and performance improvement.
During the implementation phase, the digital health solution must be integrated within current workflows to support clinical needs, and ensure sustainability and applicability across various settings (Fig. 3). Given the heterogeneity in patients, processes of care and AKI settings, implementation techniques and methods might vary based on the DHAKI solution aims or users in an iterative process. Over time, the missteps and successes of the initial implementation should be leveraged to inform the sustainable and broader deployment of the tool, whether to other clinical service lines in the same location or other institutions.
RCTs can provide a high level of evidence regarding the efficacy and effectiveness of a digital health solution, but they also have some limitations, including the lack of external validity (that is, validation outside of the setting in which they were conducted), their high cost and complex logistics, the ethical challenges of exposing some patients to interventions of uncertain benefit or harm, potential cross-contamination between the intervention and control groups, (often) the inability to mitigate or resolve the constraints and barriers during or after completion of the trial, and the time required to perform the study. Therefore, other study designs, such as effectiveness-oriented research, might allow a better understanding of the optimal processes for successful implementation and dissemination of the intervention. In addition, these alternative study designs might prevent large-scale implementation delays and help care for all patients, including those traditionally at the highest risk of health care disparities.
The target population for DHAKI implementation should be based on comorbidity, health, digital literacy, social and cultural factors. The digital health solutions should be assessed for feasibility and efficacy in distinct clinical settings and patient populations, as well as its technical characteristics (such as maturity, performance, dependability, supply chain reliability, useability, acceptability and technical interdependency with upgrade capability), and human workflow integration abilities98. Interactions with pre-existing digital health solutions should be considered for synergies, contradictions and technical interdependencies. Last, institutional readiness, support and resources such as technical expertise also affect the ability to implement new tools successfully.
A nephrotoxic medication-associated AKI prevention programme that identified children at a higher risk of AKI based on available epidemiological data99,100 transitioned from manual to automated processes90,101 and evolved from a single-centre experience to successful multicentre dissemination and implementation, while imparting knowledge at each stage to accelerate wider dissemination34. The multicentre project secured a series of commitments from each centre before admission to the collaborative34 (Supplementary Box 1).
What resources and steps are necessary to maintain and accelerate DHAKI dissemination after successful implementation?
Consensus statements
-
1.
Sustaining an implemented digital health solution is a dynamic process to accommodate changes over time.
-
2.
Defining the scope of digital health solution dissemination is crucial as broader implementation could be achieved across service lines in a single hospital, health system, or a broader entity, including several health systems or countries.
To ensure that digital health solutions are sustainable, they should be systematically redirected to comply with changing policies and maintain stakeholder engagement at the community level94. Moreover, in most cases, DHAKI solutions such as AKI alerts have not been widely adopted102,103,104,105, despite their reported benefits28,106,107. The inability to successfully implement digital health solutions is primarily due to scarcity, conflict, or distrust in existing evidence. Digital health dissemination is challenging when standardization in EHRs, procedures, protocols and institutional culture and leadership is limited, because it increases the required effort, time, resources, and consensus across stakeholders. Digital health dissemination across health systems with different institutional and contextual structures requires a deep understanding of resources, institutional culture and the capabilities of stakeholders.
Challenges of DHAKI utilization in clinical practice
What are the barriers to implementing and sustaining DHAKI tools in routine clinical practice?
Consensus statements
-
1.
Implementing digital health across the AKI continuum is complex and influenced by administrative issues, team capabilities, hardware and software limitations, and the cultural milieu.
-
2.
Following validation of DHAKI solutions in controlled research settings, translational studies are necessary to establish clinical benefits.
Several barriers and constraints can affect DHAKI implementation (Figs. 4 and 5). Varying access to health care and digital literacy is a fundamental problem108,109. Moreover, the datasets used to create AI and/or ML approaches to AKI risk management often lack diversity, which limits their generalizability54. Digital health resources and expertise in clinical environments can be very limited110. The heterogeneity in software and hardware environments across health care systems leads to competing devices with varying cost-effectiveness, which is a major barrier to digital health solution dissemination111,112. Equally important is the human–technology interaction, which encompasses technology preparedness among health care providers, end-user acceptance113,114 and the need to localize scientific units and language interfaces across the global market115. Digital health solution integration into clinical workflows is challenging. Changes in clinical workflows in tandem with the introduction of a new digital health solution are often necessary to maximize efficiency and effectiveness. Moreover, although AI advancements such as large language models, promise huge potential for applications such as medical documentation, decision support systems and patient education, they also raise many ethical and societal issues, especially regarding the misalignment of human-intended objectives and AI actions116.
Digital health in acute kidney injury care (DHAKI) implementation is conditioned by barriers, enablers and constraints that can inhibit or promote the identification of health care needs and of the appropriate choice of digital health solutions to improve the prevention, detection or treatment of AKI. These factors are also affected by health determinants and the geographical scale of implementation. Adapted from the Acute Dialysis Quality Initiative143, CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/). CKD, chronic kidney disease; Cr, creatinine; DH, digital health; ELSI, ethical, legal and social implications.
The development and implementation of digital health in acute kidney injury care (DHAKI) solutions must consider the needs that the solution must address, existing constraints, as well as the available technology choices and design approaches. A successful DHAKI solution implementation requires alignment among all of these major components. Adapted from the Acute Dialysis Quality Initiative143, CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/). Cr, creatinine; DH, digital health; ELSI, ethical, legal and social implications; IT, information technology.
Digital health tools might meet the regulatory definition of a medical device and be subject to regulatory and approval processes, some of which might not be well adapted to specific aspects of digital health. Obtaining the necessary regulatory authorizations to introduce these tools into clinical use can therefore lead to delays and raise costs. Many digital health tools rely on shared data, which can raise complex ELSI concerns117. Therefore, improved transparency in the use of private health information might promote successful implementation of new digital health solutions118.
AKI-specific challenges include AKI heterogeneity, with differences across subpopulations119,120. The broad AKI spectrum in diverse practice settings mandates wide distribution121,122,123. Perceived therapeutic nihilism around current AKI management might also reduce end-user acceptance, particularly with competing priorities from other acute and chronic medical conditions such as heart or liver failure. Evaluation of predictive or diagnostic digital health solutions should also include reporting of sensitivity and specificity because too many false negatives (that is, missed cases) or false positives (that is, incorrect diagnoses) would likely reduce trust and acceptance.
What ethical, legal and social implications create DHAKI access and usage barriers?
Consensus statement
Existing inequities in communities, health care systems and data can potentially propagate biases during the development and implementation of digital health tools, leading to further discriminatory practices that disadvantage historically excluded groups.
ELSI concerns might arise from issues related to patient safety (owing to a lack of supportive evidence), equity (related, for example, to affordability, ease of use, health literacy or algorithm biases), lack of transparency, regulation (data protection, security, consent, conflicts of interest with industry), liability, accountability and unintentional impacts on the patient–clinician relationship124,125,126. Unequal access to care and technology, driven by historical biases and the digital divide, can compromise the ability of digital health solutions to serve a diverse, global population127. For example, the use of telemedicine increased rapidly during the COVID-19 pandemic. However, this increase also exposed the large divide between resource-rich and resource-constrained settings, where the lack of stable internet connectivity was a large barrier to access to care128. This multi-faceted problem should be tackled on different fronts, including through policies aimed at bringing equitable access to the internet, through novel technologies that can work in areas of poor connectivity or intermittent connections129, and by educating the end users in using the relevant technology. Hence, systems need to be carefully validated to ensure equitable performance across all affected population subgroups130,131. Patient-facing tools can also be inaccessible because of language barriers. Moreover, existing datasets and digital health design decisions might reflect the needs of a limited subset of patients with AKI, which could lead to biased predictions and recommendations54. For example, digital health solutions developed for resource-rich settings might not be relevant in resource-limited settings132, and the complexity of digital health solutions might negate the potential benefits to patients. Digital health tools using black-box AI and/or ML models (that is, models with undisclosed processes or features) might also introduce bias and, occasionally, be counterproductive when health care professionals, patients and the public misinterpret their reasoning133. Finally, transparency issues can lead to downstream safety and security issues in the case of complex models and tools.
We recognize that technology will not solve all existing ELSI issues. However, discourse around technology can start to provide solutions that address issues in justice, autonomy, privacy, security, trust, accountability and transparency134. Promoting responsive and sustainable solutions is also important, as emphasized by recent WHO guidelines on AI for health care135. For example, current data suggest that oxygen saturation and heart rate monitoring in wearable devices via photoplethysmography are affected by skin tone and are less accurate in individuals with darker skin tones136. This discrepancy might also apply to oxygen saturation monitoring using a pulse oximeter in inpatient settings137. Social determinants can also influence access to wearable technologies and the willingness to share health data138. Therefore, studies of wearables might fail to address the population needs appropriately, and perpetuate the under-representation of subsets of patients in collected datasets, and in the subsequent research and algorithm design. Additional ethical considerations are addressed in the US White House Blueprint for an AI Bill of Rights139, the US Department of Health and Human Services Office of the National Coordinator for Health Information Technology, the Coalition for Health AI, the Health AI Partnership, and the proposed Artificial Intelligence Act from the European Union140. In addition, playbooks and auditing tools are available to identify and reduce biases141,142.
Conclusion
Digital health tools offer a unique opportunity to enhance the care of patients with AKI worldwide by empowering both patients and providers to communicate effectively, bridging gaps in care delivery and reducing barriers of access to care. Given the rapid advancement and growth of digital health solutions, their use for AKI detection and management will continue to evolve. Importantly, implementation of DHAKI solutions will need to be monitored for unintended consequences, such as the introduction or exacerbation of inequities in care delivery.
References
Hoste, E. A. et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive care Med. 41, 1411–1423 (2015).
Lameire, N. H. et al. Acute kidney injury: an increasing global concern. Lancet 382, 170–179 (2013).
Venkataraman, R. & Kellum, J. A. Prevention of acute renal failure. Chest 131, 300–308 (2007).
Sarbadhikari, S. & Sarbadhikari, S. N. The global experience of digital health interventions in COVID-19 management. Indian J. Public Health 64, S117–S124 (2020).
Ronquillo, Y., Meyers, A. & Korvek, S. J. StatPearls (StatPearls Publishing LLC., 2022).
Chawla, L. S. et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 workgroup. Nat. Rev. Nephrol. 13, 241–257 (2017).
Kashani, K. et al. Quality improvement goals for acute kidney injury. Clin. J. Am. Soc. Nephrol. 14, 941–953 (2019).
Kellum, J. A., Bellomo, R. & Ronco, C. Acute Dialysis Quality Initiative (ADQI): methodology. Int. J. Artif. Organs 31, 90–93 (2008).
U. S. Food and Drug Administration. What is digital health? https://www.fda.gov/medical-devices/digital-health-center-excellence/what-digital-health (2020).
World Health Organization. Digital health. https://www.who.int/health-topics/digital-health#tab=tab_1 (2020).
Healthcare Information and Management Systems Society. Digital health transformation: your blueprint for digital health advancement. https://www.himss.org/what-we-do-solutions/digital-health-transformation?gclid=EAIaIQobChMIsdqA6sDX9wIV5BTUAR1evQXIEAAYASAAEgLNbPD_BwE (2005).
American Medical Association. AMA digital health care 2022 study findings. https://www.ama-assn.org/about/research/ama-digital-health-care-2022-study-findings (2022).
Hunter, J. S. Enhancing Friedman’s “fundamental theorem of biomedical informatics”. J. Am. Med. Inf. Assoc. 17, 112–113 (2010).
Jain, G., Ahmad, M. & Wallace, E. L. Technology, telehealth, and nephrology: the time is now. Kidney360 1, 834–836 (2020).
Yang, Y., Chen, H., Qazi, H. & Morita, P. P. Intervention and evaluation of mobile health technologies in management of patients undergoing chronic dialysis: scoping review. JMIR Mhealth Uhealth 8, e15549 (2020).
Loncar-Turukalo, T., Zdravevski, E., Machado da Silva, J., Chouvarda, I. & Trajkovik, V. Literature on wearable technology for connected health: scoping review of research trends, advances, and barriers. J. Med. Internet Res. 21, e14017 (2019).
Digital Therapeutics Alliance, D. T. Transforming global healthcare by advancing digital therapeutics. https://dtxalliance.org/ (2022).
Barracca, A. et al. Digital health: a new frontier. J. Transl. Crit. Care Med. 5, e00018 (2023).
Ramakrishnan, P., Yan, K., Balijepalli, C. & Druyts, E. Changing face of healthcare: digital therapeutics in the management of diabetes. Curr. Med. Res. Opin. 37, 2089–2091 (2021).
Tolan, N. V. et al. The impact of outpatient laboratory alerting mechanisms in patients with AKI. Kidney360 2, 1560–1568 (2021).
Wu, Y. et al. Value of electronic alerts for acute kidney injury in high-risk wards: a pilot randomized controlled trial. Int. Urol. Nephrol. 50, 1483–1488 (2018).
Kothari, T., Jensen, K., Mallon, D., Brogan, G. & Crawford, J. Impact of daily electronic laboratory alerting on early detection and clinical documentation of acute kidney injury in hospital settings. Acad. Pathol. 5, 2374289518816502 (2018).
West Midlands Acute Medicine Collaborative. The impact of the NHS electronic-alert system on the recognition and management of acute kidney injury in acute medicine. Clin. Med. 19, 109–113 (2019).
Thomas, M. E. et al. The acute kidney outreach to prevent deterioration and death trial: a large pilot study for a cluster-randomized trial. Nephrol. Dial. Transpl. 36, 657–665 (2021).
Tollitt, J. et al. Improved management of acute kidney injury in primary care using e-alerts and an educational outreach programme. Fam. Pract. 35, 684–689 (2018).
Colpaert, K. et al. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit. Care Med. 40, 1164–1170 (2012).
Arias Pou, P., Aquerreta Gonzalez, I., Idoate Garcia, A. & Garcia-Fernandez, N. Improvement of drug prescribing in acute kidney injury with a nephrotoxic drug alert system. Eur. J. Hosp. Pharm. 26, 33–38 (2019).
Selby, N. M. et al. An organizational-level program of intervention for AKI: a pragmatic stepped wedge cluster randomized trial. J. Am. Soc. Nephrol. 30, 505–515 (2019).
McCoy, A. B. et al. Real-time pharmacy surveillance and clinical decision support to reduce adverse drug events in acute kidney injury: a randomized, controlled trial. Appl. Clin. Inf. 3, 221–238 (2012).
Kotwal, S. et al. Electronic alerts and a care bundle for acute kidney injury — an Australian cohort study. Nephrol. Dial. Transplant. 38, 610–617 (2022).
Goldstein, S. L. et al. A sustained quality improvement program reduces nephrotoxic medication-associated acute kidney injury. Kidney Int. 90, 212–221 (2016).
Kellum, J. A., Kane-Gill, S. L. & Handler, S. M. Can decision support systems work for acute kidney injury? Nephrol. Dial. Transpl. 30, 1786–1789 (2015).
Wilson, F. P. et al. Electronic health record alerts for acute kidney injury: multicenter, randomized clinical trial. BMJ 372, m4786 (2021).
Goldstein, S. L. et al. A prospective multi-center quality improvement initiative (NINJA) indicates a reduction in nephrotoxic acute kidney injury in hospitalized children. Kidney Int. 97, 580–588 (2020).
Wilson, F. P. et al. Automated, electronic alerts for acute kidney injury: a single-blind, parallel-group, randomised controlled trial. Lancet 385, 1966–1974 (2015).
Pattharanitima, P. et al. Comparison of approaches for prediction of renal replacement therapy-free survival in patients with acute kidney injury. Blood Purif. 50, 621–627 (2021).
Akl, A. I., Sobh, M. A., Enab, Y. M. & Tattersall, J. Artificial intelligence: a new approach for prescription and monitoring of hemodialysis therapy. Am. J. Kidney Dis. 38, 1277–1283 (2001).
Neyra, J. A. & Nadkarni, G. N. Continuous kidney replacement therapy of the future: innovations in information technology, data analytics, and quality assurance systems. Adv. Chronic Kidney Dis. 28, 13–19 (2021).
Kang, M. W. et al. Machine learning model to predict hypotension after starting continuous renal replacement therapy. Sci. Rep. 11, 17169 (2021).
Park, S. et al. Impact of electronic Acute Kidney Injury (AKI) alerts with automated nephrologist consultation on detection and severity of AKI: a quality improvement study. Am. J. Kidney Dis. 71, 9–19 (2018).
Kolhe, N. V. et al. Impact of compliance with a care bundle on acute kidney injury outcomes: a prospective observational study. PLoS One 10, e0132279 (2015).
Hodgson, L. E. et al. The ICE-AKI study: impact analysis of a clinical prediction rule and electronic AKI alert in general medical patients. PLoS One 13, e0200584 (2018).
Newton, E. S., Kurzen, E. A., Linnemann, R. W. & Shin, H. S. Use of the NINJA (Nephrotoxic Injury Negated by Just-in-Time Action) program to identify nephrotoxicity in pediatric patients with cystic fibrosis. J. Pediatr. Pharmacol. Ther. 26, 379–383 (2021).
Kane-Gill, S. L., Barreto, E. F., Bihorac, A. & Kellum, J. A. Development of a theory-informed behavior change intervention to reduce inappropriate prescribing of nephrotoxins and renally eliminated drugs. Ann. Pharmacother. 55, 1474–1485 (2021).
Lamming, L. et al. Barriers and enablers to the implementation of a complex quality improvement intervention for acute kidney injury: a qualitative evaluation of stakeholder perceptions of the Tackling AKI study. PLoS One 14, e0222444 (2019).
Koyner, J. L., Carey, K. A., Edelson, D. P. & Churpek, M. M. The development of a machine learning inpatient acute kidney injury prediction model. Crit. Care Med. 46, 1070–1077 (2018).
Zimmerman, L. P. et al. Early prediction of acute kidney injury following ICU admission using a multivariate panel of physiological measurements. BMC Med. Inf. Decis. Mak. 19, 16 (2019).
Koyner, J. L., Adhikari, R., Edelson, D. P. & Churpek, M. M. Development of a multicenter ward-based AKI prediction model. Clin. J. Am. Soc. Nephrol. 11, 1935–1943 (2016).
Chiofolo, C., Chbat, N., Ghosh, E., Eshelman, L. & Kashani, K. Automated continuous acute kidney injury prediction and surveillance: a random forest model. Mayo Clin. Proc. 94, 783–792 (2019).
Schwager, E. et al. Accurate and interpretable prediction of ICU-acquired AKI. J. Crit. Care 75, 154278 (2023).
Rank, N. et al. Deep-learning-based real-time prediction of acute kidney injury outperforms human predictive performance. NPJ Digit. Med. 3, 139 (2020).
Xu, Z. et al. Predictive modeling of the risk of acute kidney injury in critical care: a systematic investigation of the class imbalance problem. AMIA Jt. Summits Transl. Sci. Proc. 2019, 809–818 (2019).
Xu, Z. et al. Identifying sub-phenotypes of acute kidney injury using structured and unstructured electronic health record data with memory networks. J. Biomed. Inf. 102, 103361 (2020).
Tomašev, N. et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572, 116–119 (2019).
Churpek, M. M. et al. Internal and external validation of a machine learning risk score for acute kidney injury. JAMA Netw. Open. 3, e2012892 (2020).
Song, X. et al. Cross-site transportability of an explainable artificial intelligence model for acute kidney injury prediction. Nat. Commun. 11, 5668 (2020).
Al-Jaghbeer, M., Dealmeida, D., Bilderback, A., Ambrosino, R. & Kellum, J. A. Clinical decision support for in-hospital AKI. J. Am. Soc. Nephrol. 29, 654–660 (2018).
Bataineh, A. et al. Sustained effects of a clinical decision support system for acute kidney injury. Nephrol. Dial. Transpl. 35, 1819–1821 (2020).
Barker, J. et al. Electronic alerts for acute kidney injury across primary and secondary care. BMJ Open. Qual. 10, e000956 (2021).
Holmes, J. et al. Acute kidney injury electronic alerts in primary care — findings from a large population cohort. QJM 110, 577–582 (2017).
Holmes, J. et al. Utility of electronic AKI alerts in intensive care: a national multicentre cohort study. J. Crit. Care 44, 185–190 (2018).
Holmes, J., Donovan, K., Geen, J., Williams, J. & Phillips, A. O. Acute kidney injury demographics and outcomes: changes following introduction of electronic acute kidney injury alerts — an analysis of a national dataset. Nephrol. Dial. Transpl. 36, 1433–1439 (2021).
Holmes, J. et al. Community acquired acute kidney injury: findings from a large population cohort. QJM 110, 741–746 (2017).
Dong, J. et al. Machine learning model for early prediction of acute kidney injury (AKI) in pediatric critical care. Crit. Care 25, 288 (2021).
Flechet, M. et al. Machine learning versus physicians’ prediction of acute kidney injury in critically ill adults: a prospective evaluation of the AKI predictor. Crit. Care 23, 282 (2019).
Neyra, J. A. et al. Prediction of mortality and major adverse kidney events in critically ill patients with acute kidney injury. Am. J. Kidney Dis. 81, 36–47 (2023).
Lei, V. J. et al. Risk stratification for postoperative acute kidney injury in major noncardiac surgery using preoperative and intraoperative data. JAMA Netw. Open. 2, e1916921 (2019).
Demirjian, S. et al. Predictive accuracy of a perioperative laboratory test-based prediction model for moderate to severe acute kidney injury after cardiac surgery. JAMA 327, 956–964 (2022).
Rashidi, H. H. et al. Early recognition of burn- and trauma-related acute kidney injury: a pilot comparison of machine learning techniques. Sci. Rep. 10, 205 (2020).
Martinez, D. A. et al. Early prediction of acute kidney injury in the emergency department with machine-learning methods applied to electronic health record data. Ann. Emerg. Med. 76, 501–514 (2020).
Macedo, E. et al. Recognition and management of community-acquired acute kidney injury in low-resource settings in the ISN 0by25 trial: a multi-country feasibility study. PLoS Med. 18, e1003408 (2021).
Montanari, A. et al. Can teledialysis help in the clinical management of patients on remote hemodialysis? Int. J. Artif. organs 15, 397–400 (1992).
Androga, L. A. et al. Provider perspectives and clinical outcomes with inpatient telenephrology. Clin. J. Am. Soc. Nephrol. 17, 655–662 (2022).
Kane-Gill, S. L. & Rincon, F. Expansion of telemedicine services: telepharmacy, telestroke, teledialysis, tele-emergency medicine. Crit. care Clin. 35, 519–533 (2019).
Mayer, K. P. et al. Acute kidney injury contributes to worse physical and quality of life outcomes in survivors of critical illness. BMC Nephrol. 23, 137 (2022).
Silver, S. A. et al. What insights do patients and caregivers have on acute kidney injury and posthospitalisation care? A single-centre qualitative study from Toronto, Canada. BMJ Open. 8, e021418 (2018).
Fleming, J. N. et al. Impact of a pharmacist-led, mHealth-based intervention on tacrolimus trough variability in kidney transplant recipients: a report from the TRANSAFE Rx randomized controlled trial. Am. J. Health Syst. Pharm. 78, 1287–1293 (2021).
McGillicuddy, J. W., Chandler, J. L., Sox, L. R. & Taber, D. J. Exploratory analysis of the impact of an mhealth medication adherence intervention on tacrolimus trough concentration variability: post hoc results of a randomized controlled trial. Ann. Pharmacother. 54, 1185–1193 (2020).
Gonzales, H. M. et al. Pharmacist-led mobile health intervention and transplant medication safety: a randomized controlled clinical trial. Clin. J. Am. Soc. Nephrol. 16, 776–784 (2021).
Castro, A. C. et al. Wearable artificial kidney and wearable ultrafiltration device vascular access — future directions. Clin. Kidney J. 12, 300–307 (2019).
Wieringa, F. P., Broers, N. J. H., Kooman, J. P., Van Der Sande, F. M. & Van Hoof, C. Wearable sensors: can they benefit patients with chronic kidney disease? Expert. Rev. Med. Devices 14, 505–519 (2017).
Siew, E. D. et al. Improving care for patients after hospitalization with AKI. J. Am. Soc. Nephrol. 31, 2237–2241 (2020).
Ronco, C., Rizo-Topete, L., Serrano-Soto, M. & Kashani, K. Pro: prevention of acute kidney injury: time for teamwork and new biomarkers. Nephrol. Dial. Transpl. 32, 408–413 (2017).
Park, S. M. et al. A mountable toilet system for personalized health monitoring via the analysis of excreta. Nat. Biomed. Eng. 4, 624–635 (2020).
Boehmer, K. R. et al. Capacity coaching: a new strategy for coaching patients living with multimorbidity and organizing their care. Mayo Clin. Proc. 94, 278–286 (2019).
Rizo-Topete, L. M., Rosner, M. H. & Ronco, C. Acute kidney injury risk assessment and the nephrology rapid response team. Blood Purif. 43, 82–88 (2017).
Coffey, J. D. et al. Implementation of a multisite, interdisciplinary remote patient monitoring program for ambulatory management of patients with COVID-19. NPJ Digit. Med. 4, 123 (2021).
Connell, A. & Laing, C. Acute kidney injury. Clin. Med. 15, 581–584 (2015).
Chang, J., Ronco, C. & Rosner, M. H. Computerized decision support systems: improving patient safety in nephrology. Nat. Rev. Nephrol. 7, 348–355 (2011).
Goldstein, S. L. et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics 132, e756–e767 (2013).
Connell, A. et al. Evaluation of a digitally-enabled care pathway for acute kidney injury management in hospital emergency admissions. NPJ Digit. Med. 2, 67 (2019).
Van Driest, S. L. et al. Acute kidney injury risk-based screening in pediatric inpatients: a pragmatic randomized trial. Pediatr. Res. 87, 118–124 (2020).
Bauer, M. S., Damschroder, L., Hagedorn, H., Smith, J. & Kilbourne, A. M. An introduction to implementation science for the non-specialist. BMC Psychol. 3, 32 (2015).
Aarons, G. A., Hurlburt, M. & Horwitz, S. M. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm. Policy Ment. Health 38, 4–23 (2011).
NHS. Design principles. NHS Digital Service Manual https://service-manual.nhs.uk/design-system/design-principles (2022).
Kayser, L., Kushniruk, A., Osborne, R. H., Norgaard, O. & Turner, P. Enhancing the effectiveness of consumer-focused health information technology systems through ehealth literacy: a framework for understanding users’ needs. JMIR Hum. Factors 2, e9 (2015).
Camacho, J., Zanoletti-Mannello, M., Landis-Lewis, Z., Kane-Gill, S. L. & Boyce, R. D. A conceptual framework to study the implementation of clinical decision support systems (BEAR): literature review and concept mapping. J. Med. Internet Res. 22, e18388 (2020).
Greenhalgh, T. et al. The NASSS-CAT tools for understanding, guiding, monitoring, and researching technology implementation projects in health and social care: protocol for an evaluation study in real-world settings. JMIR Res. Protoc. 9, e16861 (2020).
Moffett, B. S. & Goldstein, S. L. Acute kidney injury and increasing nephrotoxic-medication exposure in noncritically-ill children. Clin. J. Am. Soc. Nephrol. 6, 856–863 (2011).
Zappitelli, M. et al. Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin. J. Am. Soc. Nephrol. 3, 948–954 (2008).
Kirkendall, E. S. et al. Development and performance of electronic acute kidney injury triggers to identify pediatric patients at risk for nephrotoxic medication-associated harm. Appl. Clin. Inf. 5, 313–333 (2014).
Walsh, K. E., Bundy, D. G. & Landrigan, C. P. Preventing health care-associated harm in children. JAMA 311, 1731–1732 (2014).
Leape, L. L. & Berwick, D. M. Five years after to err is human: what have we learned. JAMA 293, 2384–2390 (2005).
Landrigan, C. P. et al. Temporal trends in rates of patient harm resulting from medical care. N. Engl. J. Med. 363, 2124–2134 (2010).
Shekelle, P. G. et al. Assessing the Evidence for Context-Sensitive Effectiveness and Safety of Patient Safety Practices: Developing Criteria (Agency for Healthcare Research and Quality, 2010).
Wilson, F. P. et al. A randomized clinical trial assessing the effect of automated medication-targeted alerts on acute kidney injury outcomes. Nat. Commun. 14, 2826 (2023).
Bourdeaux, C. et al. Impact of a computerized decision support tool deployed in two intensive care units on acute kidney injury progression and guideline compliance: a prospective observational study. Crit. Care 24, 656 (2020).
Price-Haywood, E. G., Harden-Barrios, J., Ulep, R. & Luo, Q. eHealth literacy: patient engagement in identifying strategies to encourage use of patient portals among older adults. Popul. Health Manag. 20, 486–494 (2017).
Triana, A. J., Gusdorf, R. E., Shah, K. P. & Horst, S. N. Technology literacy as a barrier to telehealth during COVID-19. Telemed. J. E Health 26, 1118–1119 (2020).
UK Government. The Future of Healthcare: Our Vision for Digital, Data and Technology in Health and Care https://www.gov.uk/government/publications/the-future-of-healthcare-our-vision-for-digital-data-and-technology-in-health-and-care/the-future-of-healthcare-our-vision-for-digital-data-and-technology-in-health-and-care (2018).
Goldstein, B. A., Navar, A. M., Pencina, M. J. & Ioannidis, J. P. Opportunities and challenges in developing risk prediction models with electronic health records data: a systematic review. J. Am. Med. Inf. Assoc. 24, 198–208 (2017).
Selby, N. M. et al. Standardizing the early identification of acute kidney injury: the NHS England national patient safety alert. Nephron 131, 113–117 (2015).
Singh, K. et al. Patients’ and nephrologists’ evaluation of patient-facing smartphone apps for CKD. Clin. J. Am. Soc. Nephrol. 14, 523–529 (2019).
Singh, K. et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Aff. 35, 2310–2318 (2016).
Rodriguez, J. A. & Singh, K. The Spanish availability and readability of diabetes apps. J. Diabetes Sci. Technol. 12, 719–724 (2018).
Walter, Y. The rapid competitive economy of machine learning development: a discussion on the social risks and benefits. AI Ethics https://doi.org/10.1007/s43681-023-00276-7 (2023).
Denham, E. RFA0627721 — Provision of Patient Data to DeepMind https://ico.org.uk/media/action-weve-taken/undertakings/2014353/undertaking-cover-letter-revised-04072017-to-first-person.pdf (2017).
Royal Free London NHS Foundation Trust. Information Commissioner’s Office (ICO) Investigation https://www.royalfree.nhs.uk/patients-visitors/how-we-use-patient-information/information-commissioners-office-ico-investigation-into-our-work-with-deepmind/ (2019).
Barasch, J., Zager, R. & Bonventre, J. V. Acute kidney injury: a problem of definition. Lancet 389, 779–781 (2017).
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2 (Suppl.), 1–138 (2012).
Selby, N. M. et al. Use of electronic results reporting to diagnose and monitor AKI in hospitalized patients. Clin. J. Am. Soc. Nephrol. 7, 533–540 (2012).
UK Renal Registry. Acute Kidney Injury (AKI) in England — A Report on the Nationwide Collection of AKI Warning Test Scores from 2018 https://ukkidney.org/sites/renal.org/files/AKI_report_FINAL_13072020.pdf (2020).
Hoste, E. A. J. et al. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol. 14, 607–625 (2018).
Cummins, N. & Schuller, B. W. Five crucial challenges in digital health. Front. Digit. Health 2, 536203 (2020).
Cordeiro, J. V. Digital technologies and data science as health enablers: an outline of appealing promises and compelling ethical, legal, and social challenges. Front. Med. 8, 647897 (2021).
Čartolovni, A., Tomičić, A. & Lazić Mosler, E. Ethical, legal, and social considerations of AI-based medical decision-support tools: a scoping review. Int. J. Med. Inform. 161, 104738 (2022).
Suresh, H. & Guttag, J. Equity and Access in Algorithms, Mechanisms, and Optimization (EAAMO ‘21) (ACM, 2021).
Julien, H. M., Eberly, L. A. & Adusumalli, S. Telemedicine and the forgotten America. Circulation 142, 312–314 (2020).
Huang, G. K. L. et al. Telemedicine in resource-limited settings to optimize care for multidrug-resistant tuberculosis. Front. Public. Health 7, 222 (2019).
Yala, A. et al. Multi-institutional validation of a mammography-based breast cancer risk model. J. Clin. Oncol. 40, 1732–1740 (2022).
Yala, A. et al. Toward robust mammography-based models for breast cancer risk. Sci. Transl. Med. 13, eaba4373 (2021).
Price, W. N. II. Medical AI and Contextual Bias. 33 Harv. J.L. & Tech. 66 (2019), U of Michigan Public Law Research Paper No. 632 https://ssrn.com/abstract=3347890 (2019).
Gerke, S., Minssen, T. & Cohen, G. Ethical and legal challenges of artificial intelligence-driven healthcare. In Artificial Intelligence in Healthcare (eds. Bohr, A. & Memarzadeh, K.) Ch. 12, 295–336 (Elsevier, 2020).
Brall, C., Schroder-Back, P. & Maeckelberghe, E. Ethical aspects of digital health from a justice point of view. Eur. J. Public. Health 29, 18–22 (2019).
World Health Organization. Ethics and Governance of Artificial Intelligence for Health: WHO Guidance https://www.who.int/publications-detail-redirect/9789240029200 (2021).
Shcherbina, A. et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J. Pers. Med. 7, 3 (2017).
Valbuena, V. S. M. et al. Racial bias and reproducibility in pulse oximetry among medical and surgical inpatients in general care in the Veterans Health Administration 2013–19: multicenter, retrospective cohort study. BMJ 378, e069775 (2022).
Vogels, E. A. Digital divide persists even as Americans with lower incomes make gains in tech adoption. https://www.pewresearch.org/short-reads/2021/06/22/digital-divide-persists-even-as-americans-with-lower-incomes-make-gains-in-tech-adoption/ (2021).
The White House. Blueprint for an AI Bill of Rights: Making Automated Systems Work for the American People https://www.whitehouse.gov/ostp/ai-bill-of-rights/ (2022).
European Commission. A European Approach to Artificial Intelligence https://digital-strategy.ec.europa.eu/en/policies/european-approach-artificial-intelligence (2021).
Metaxa, D. et al. Auditing algorithms: understanding algorithmic systems from the outside in. Found. Trends Hum. Comput. Interact. 14, 272–344 (2021).
Obermeyer, Z. et al. Algorithmic Bias Playbook https://www.chicagobooth.edu/-/media/project/chicago-booth/centers/caai/docs/algorithmic-bias-playbook-june-2021.pdf (2021).
Acute Dialysis Quality Initiative. AKI in digital health figures. https://pittccmblob.blob.core.windows.net/adqi/27fig.pdf (2022).
Acknowledgements
The ADQI consensus meeting received unrestricted grants from BioMérieux Inc., Baxter International Inc., BioPorto, MediBeacon Inc., ExThera, UAB/UCSD O’Brien Center for AKI Research, University of Florida, Mayo Clinic and the University of California San Diego. Corporate sponsors were allowed to attend all meeting sessions as observers but were not allowed to participate in the consensus process and therefore had no input in preparing final recommendations or this manuscript.
Author information
Authors and Affiliations
Contributions
K.B.K., R.L.M. and A.B. organized the ADQI consensus meeting. All authors actively participated in the group and plenary discussions, made substantial contributions to discussions of the content and wrote, reviewed or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
K.B.K. received research grants from Philips Research North America and Google; speaker honorarium from Nikkiso Critical Care Medical Supplies (Shanghai) Co., Ltd; Funding from National Institute of Diabetes and Digestive and Kidney Diseases grant (R01DK131586); also reports consulting fees to Mayo Clinic from Baxter Inc. L.A. holds grant funding from the UCSD-UAB O’Brien Center for AKI (NIDDK) and Sony Electronics, Inc. S.M.B. is supported by a Canada Research Chair in Critical Care Outcomes and Systems Evaluation, and received fees for scientific advisory and speaking from Baxter, fees for scientific advisory from Novartis, fees for data safety monitoring for I-SPY-COVID, and fees for scientific advisory and adjudication from BioPorto. E.F.B. received consulting fees for FAST Biomedical, Wolters-Kluwer (unrelated), and also research support from NIH, AHRQ. R.C.-D.G. received consulting fees from Medtronic for developing CRRT educational material and a speaker honorarium from Nova Biomedical. B.J.E. did not disclose any conflicting interests. L.G.F. received research funding from Baxter, Ortho Clinical Diagnostics, NIHR. E.G. is employed in Philips Research North America and owns stock in Philips. S.L.K.-G. receives royalties from Vigilanz Corporation (Minneapolis, MN, USA) for the Nephrotoxic Injury Negated by Just-in-Time (NINJA) application licensed to Vigilanz from Cincinnati Children’s Hospital Medical Center. S.L.K.-G. receives research funding from NIDDK and NCCIH and is a member of the executive committee for the Society of Critical Care Medicine. J.L.K. received research funding from NIH, Fresenius Medical, Astute/BioMérieux; consulting fees from Baxter, Astute/BioMérieux, Novartis, Guard Therapeutic, and honoraria from ASN. M.L. received research funding from NIDDK (R01DK116986), NSF (2014554) and NCATS (UL1TR002366). R.M. received research funding from the National Institute of Diabetes and Digestive and Kidney Diseases grant (R01DK131586), consulting fees from Baxter Inc unrelated to this study. G.N.N. received consulting fees from AstraZeneca, Reata, BioVie, Daiichi Sankyo, Qiming Capital and GLG, financial compensation as a scientific board member and adviser to Renalytix, and owns equity in Renalytix, Nexus iConnect, Data2Wisdom, and Pensieve Health as a cofounder. J.A.N. received consulting fees form Baxter, Outset, Vifor and Leadiant Biosciences, and research funding from NIDDK (R56 DK126930, R01 DK128208, U01 DK129989, and P30 DK079337). M.O. receives research funding from Fresenius Medical Care, Baxter, Biomérieux and LaJolla Pharma, and speaker honoraria from Fresenius Medical Care, Baxter, BioMérieux and Gilead. P.R. receives research funding from the National Institutes of Health (R21 AG073769, R01 GM110240, OT2 OD032701), NIH/National Institute of Biomedical Imaging and Bioengineering (R01 EB029699), NIH/National Institute of Neurological Disorders and Stroke (R01 NS120924), NIH/National Institute of Diabetes and Digestive and Kidney Diseases (R01 KD121730), and the National Science Foundation (CAREER 1750192). N.M.S. received research funding from the NIHR HS&DR Programme (NIHR131948, co-applicant), NIHR Health Technology Assessment (HTA) program (NIHR129617 Co-Chief Investigator) and speaker honoraria from GE, Fresenius and AstraZeneca, and has a provisional patent for measuring pressure waves in dialysis lines to derive continuous arterial blood pressure. K.S. receives grant funding from Blue Cross Blue Shield of Michigan and Teva Pharmaceuticals for unrelated work, and serves on a scientific advisory board for Flatiron Health (New York, NY, USA). R.L.M. receives consulting fees from Baxter, AM Pharma, BioMérieux, Mallinckrodt, GE Healthcare; Sanofi, Nova BioMed, Abiomed, Novartis, Fresenius, Renasym, Alexion, Renibus, SeaStar, Abbott, Guard. J.K., J.N., N.P., C.R., M.H.R., B.S., D.E.S., S.M.S. and A.B. declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks L. Celi, E. Gottlieb, P. Wilson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Coalition for Health AI: https://coalitionforhealthai.org/
Health AI partnership: https://healthaipartnership.org/
Office of the National Coordinator for Health Information Technology: https://www.healthit.gov/topic/health-equity
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kashani, K.B., Awdishu, L., Bagshaw, S.M. et al. Digital health and acute kidney injury: consensus report of the 27th Acute Disease Quality Initiative workgroup. Nat Rev Nephrol 19, 807–818 (2023). https://doi.org/10.1038/s41581-023-00744-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-023-00744-7
This article is cited by
-
Drug stewardship in chronic kidney disease to achieve effective and safe medication use
Nature Reviews Nephrology (2024)
-
Advances in pediatric acute kidney injury pathobiology: a report from the 26th Acute Disease Quality Initiative (ADQI) conference
Pediatric Nephrology (2024)