Abstract
As global SARS-CoV-2 burden and testing frequency have decreased, wastewater surveillance has emerged as a key tool to support clinical surveillance efforts. The aims of this study were to identify and characterize SARS-CoV-2 variants in wastewater samples collected from urban centers across South Africa. Here we show that wastewater sequencing analyses are temporally concordant with clinical genomic surveillance and reveal the presence of multiple lineages not detected by clinical surveillance. We show that wastewater genomics can support SARS-CoV-2 epidemiological investigations by reliably recovering the prevalence of local circulating variants, even when clinical samples are not available. Further, we find that analysis of mutations observed in wastewater can provide a signal of upcoming lineage transitions. Our study demonstrates the utility of wastewater genomics to monitor evolution and spread of endemic viruses.
Similar content being viewed by others
Introduction
Since SARS-CoV-2 is shed into stool1,2,3 and urine1 and is detectable in wastewater4, quantification and sequencing of SARS-CoV-2 in wastewater has the potential to overcome many inherent limitations in clinically-based epidemiological approaches. Throughout the COVID-19 pandemic, clinical surveillance has relied on testing and sequencing of samples from infected individuals. However, when clinical testing forms the basis for surveillance, population health-seeking behavior, test accessibility and testing practices of attending clinicians limit the generalizability of data5. In particular, clinical testing generally only detects symptomatic cases and testing practices often vary by location and over time6, leading to an incomplete representation of virus spread and diversity. Wastewater-based testing for SARS-CoV-2 overcomes these limitations by sampling wastewater from the entire community, which adds key information to our understanding of SARS-CoV-2 transmission dynamics, and at a fraction of the cost of clinical surveillance. As such, over 70 countries now provide monitoring and public reporting of geographical and temporal trends in wastewater SARS-CoV-2 levels7,8.
Wastewater genomic surveillance enables monitoring of the specific variants circulating in a community. Whole genome sequencing9 and other methods such as real-time PCR10 enable detection and characterization of SARS-CoV-2 variants, and can be applied in wastewater samples. Recent work has shown the potential for recovery of complete virus genomes from wastewater11, demonstrated comparable lineage dynamics via wastewater and clinical surveillance, and identified novel mutations and lineages in wastewater before appearance in clinical samples6,12. To date, wastewater sequencing of SARS-CoV-2 has not been widely applied in low- or middle-income countries.
South Africa is a middle-income country with a population of over 55 million persons, most of whom live in urban centers located in five of the country’s nine provinces. South Africa has over 1,000 wastewater treatment plants13 and the majority of South Africans (84%) have access to piped sanitation (flush toilets connected to a public sewerage system or a septic tank)14. After wastewater testing for SARS-CoV-2 was first described in South Africa in June 202015, the South African Collaborative COVID-19 Environmental Surveillance System (SACCESS) arose to monitor trends in SARS-CoV-2 levels in wastewater across the country16.
Most clinical SARS-CoV-2 testing is provided to the public through an extensive network of laboratories including the National Health Laboratory Service (NHLS) that covers over 80% of the population. South Africa identified its first case of COVID-19 on the 5th of March 202017, and four waves of COVID-19 occurred within the first 24 months of virus introduction into the country. Following the initial SARS-CoV-2 wave, the Beta variant18 was discovered and was dominant from November 2020 to February 2021 (second wave). The third wave (May to September 2021) was dominated by the Delta variant19,20 and the fourth wave (November 2021 to January 2022) was driven by the Omicron BA.1 variant21. The National Institute for Communicable Diseases (NICD), a division of the NHLS, provides SARS-CoV-2 epidemiological surveillance data through collation of SARS-CoV-2 PCR results from public and private laboratories. The Network for Genomic Surveillance of South Africa22 (NGS-SA) is a collaborating group of seven sequencing hubs located at tertiary or academic laboratories across the country. The NGS-SA monitors the epidemiology of SARS-CoV-2 variants in PCR-confirmed cases in South Africa and reports weekly on findings23. The NGS-SA provided the first global reports of the emergence of Beta and Omicron variants of concern (VOC)18,21.
Here, we show that wastewater can be used to effectively characterize the dynamics of SARS-CoV-2 virus lineage spread and evolution in the population. Using surveillance from sentinel wastewater treatment plants in urban metros collected from April 2021 to the end of the Omicron BA.1 wave in January 2022, we demonstrate the utility of wastewater genomic surveillance to complement clinical surveillance efforts in a middle-income setting. We identify the potential strengths and limitations of wastewater genomic surveillance for SARS-CoV-2 in the South African context.
Results
A total of 325 wastewater samples from sites listed in Table S1 were amplified and sequenced. Of those, 229 (70.5%) samples had > 1 million reads and were included in the mutational analysis and the heatmap visualization. Out of the 325, 183 (56.3%) samples had >50% sequence coverage of the whole genome (10x depth) and these were used for Freyja analysis.
Detection of SARS-CoV-2 variants from wastewater samples
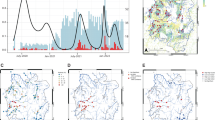
Across all wastewater collection sites, we observed clear wave-like dynamics that closely paralleled trends observed in clinical genomic surveillance (Fig. 1A–C). The Beta variant dominated early samples in April 2021 until it was displaced by the Delta variant in June 2021. Although the Alpha variant was briefly detectable in June, Delta continued to be the prevailing variant until November, at which point the Omicron variant was detected and almost immediately dominated the pathogen landscape. Freyja analyses also enabled more fine-grained analysis of individual lineages (Fig. 1B). As in clinical surveillance (Fig. 1C), AY.45 was identified as the dominant lineage during the Delta wave across South Africa, and we regularly detected low levels of C.1.2 and other B.1.1.X lineages leading up to and during the Omicron wave. We also identified cryptic circulation of A lineage viruses including A.25 as well as the Alpha-Delta recombinant lineage XC in June, neither of which had been previously reported in South Africa. During the Omicron wave, we observed the rapid rise of the Omicron BA.1 lineage, which was eventually displaced by its sister-lineage BA.2 by the end of January 2022. We also identified substantial prevalence of BA.3 and other Omicron BA.1-BA.2 recombinant lineages, including XE, XAD, and XAP, that were rarely observed in clinical surveillance during the study period.
Comparison of wastewater and clinical genomic surveillance in Gauteng, KwaZulu-Natal, and Free State provinces
In Gauteng, Freyja analysis of wastewater identified the Beta variant as the dominant variant in April and May 2021, and in low frequency in June 2021 (Fig. 2A), closely matching clinical surveillance during the same period (Fig. 2B). The Alpha variant was detected in a small proportion of clinical samples from April to July 2021, while Freyja reported the Alpha variant in June and August 2021. In May 2021, the Delta variant was first detected both in wastewater and clinical samples, and remained dominant until October 2021 in both wastewater and clinical samples. We detected a small population of the XC recombinant in June 2021, but this was not detected in wastewater or clinical surveillance from any other provinces. Freyja reported the presence of the C.1.2 virus lineage from June 2021 until August 2021, although no wastewater samples met the sequencing quality threshold in September 2021, whereas clinical surveillance detected C.1.2 through October. In October 2021, Omicron (BA.1) was first detected in clinical specimens and rapidly became the dominant lineage. BA.2 was first detected in late November and supplanted BA.1 by January 2022. However, Omicron was dominant in wastewater from November 2021 on, with BA.1, and BA.3 lineages being detected. However, the BA.2 variant was only detected in wastewater in January 2022. BA.3 variants were reported in wastewater in November 2021 and again in January 2022 by Freyja, but in clinical isolates, BA.3 was only detected in three samples, all collected in December 2021. We also detected the BA.1-BA.2 Omicron recombinant lineages XE, XAD, and XAP.
In wastewater samples from KZN Province (Fig. 2C), the Beta variant was detected in June at low read frequencies. However, wastewater samples failed to amplify in April 2021. The Beta variant was not detected in wastewater samples in May. Amongst clinical specimens collected in KZN Province (Fig. 2C), the Beta variant was detected from April to June 2021, and was dominant until May 2021. In wastewater samples, the Delta variant dominated from May 2021 until August 2021. C.1.2 appeared in wastewater samples in June and in August. By comparison, C.1.2 appeared for the first time in clinical samples from KZN in July 2021 until November 2021 at small proportions ( < 10%). In May 2021, the Delta variant appeared in clinical specimens at low read frequencies in April and May 2021, and was the dominant variant from June until October 2021. The Omicron variant appeared and quickly dominated clinical samples in November 2021, although Delta variant was still detectable along with C.1.2. In December 2021 and January 2022, Omicron completely replaced all circulating lineages. In December, BA.2 was first detected in low proportions and became co-dominant with Omicron BA.1 in January 2022 in both wastewater and clinical samples. Amongst wastewater samples, Omicron was present from November 2021, although wastewater samples failed to amplify in September and October 2021. Omicron BA.2 was detected in wastewater samples in January 2022 for the first time, along with Omicron recombinants XE and XAP, which were also observed in Gauteng wastewater.
In Free State, wastewater, and clinical samples, the Beta variant was present from April 2021 until June 2021 but was only dominant in April and May 2021 (Fig. 2E, F). In July 2021, a small proportion of clinical samples (<5%) yielded Beta variant but wastewater samples did not show evidence of the Beta variant. The Alpha variant was present in a small proportion of clinical specimens in April, May, and June 2021, but was not detectable by Freyja. In June 2021, the Delta variant appeared in both wastewater and clinical samples and appeared co-dominant with Beta variant by both Freyja and clinical genomic analysis. C.1.2 was detected in clinical specimens from July until October 2021, but was not detected by Freyja during the same period. The Omicron variant appeared for the first time in November 2021 in clinical samples and dominated until the end of the study period. BA.2 was detected in December 2021 and January 2022. Amongst wastewater samples, Omicron appeared in November 2021, but BA.2 was not detected in wastewater samples.
Across the provinces included in study, we observed some key differences among circulating lineages observed via wastewater. The Alpha variant was detected in Gauteng and Free State in June, but not in KZN. We also observed a small amount of Alpha (about 1% prevalence) in Gauteng in August, but not in KZN or Free State. Delta appeared dominant in the earliest samples taken from KZN, whereas Beta was clearly dominant in Gauteng and Free State. BA.1.1 appeared to play a larger role in Omicron BA.1 spread in Free State than in other provinces, and no BA.2 was observed in Free State during the study. Omicron BA.3 was only detected in Gauteng province, although other BA.1-BA.2 Omicron recombinants were detected both in Gauteng and KZN. We did not detect any BA.2 in Free State, and observed relatively little in KZN, indicative of the BA.2 wave starting earlier in Gauteng. Finally, A.25 and other A lineage circulation was not observed in Gauteng, Free State, or KZN, or in nationwide clinical surveillance, but it was observed in Eastern Cape in June, despite limited wastewater sampling from the province.
Detection of SARS-CoV-2 variants from wastewater samples using signature mutation analysis
In addition to performing lineage assignment with Freyja, we also analyzed the frequency of variant-specific “signature” mutations, which are lineage-defining, nonsynonymous mutations in the Spike region of the SARS-CoV-2 genome (Table S3). We identified signature mutations in 170 samples (52.3%), 79 samples from Gauteng, 32 from KwaZulu-Natal, 32 from Free State, 12 from Western Cape, and 15 from the Eastern Cape provinces respectively. The remaining 155 (47.7%) had no signature mutations, and thus could not be independently used to identify lineages in each catchment. We included 143 (44%) samples in our analysis from Gauteng, KwaZulu-Natal, and Free State provinces, and excluded samples from Western Cape, and Eastern Cape due to the small number of samples with signature mutations. Since no minimum genome coverage threshold was used, this approach enabled analysis of lower coverage samples not used in Freyja analyses. Using these signature mutations, we were able to identify variant waves in samples across our sites (Fig. 3A–C, supplementary figure S2). Similar to the Freyja and clinical results, the Beta variant was dominant in samples from April 2021 to June 2021 in all three provinces (Gauteng, KwaZulu-Natal, and Free State). This was followed by the domination of Delta variant and then replaced completely by Omicron BA.1 and thereafter BA.2. In Gauteng Province, Alpha was detected in May, June, and July 2021, while C.1.2 was detected from June to August 2021 (Fig. 3A). In KwaZulu–Natal province, Alpha variant mutations were detected in May, and C.1.2 was detected in August 2021 (Fig. 3B). In Free State province, we detected one mutation related to Alpha variant in June 2021. Lineage C.1.2 mutations were detected in July, and August 2021 (Fig. 3C).
Frequency of signature mutations associated with each variant per epidemiological week, for Gauteng (A), KwaZulu-Natal (B), and Free State (C) provinces. Signature mutations corresponding to each variant are described in Table S3.
Characterization of amino acid mutations in the spike region
A total of 411 amino acid mutations were observed in the spike protein amongst all sequenced samples. Analysis of mutation frequencies per amino acid position (Fig. 4A) demonstrated a characteristic pattern of mutations in each epidemiological wave of COVID-19. The transition from Delta variant to Omicron was characterized by a disappearance of viruses with mutations in the N-terminal domain (NTD) region (E156del, F157del, and R158G), and an appearance of viruses with mutations in the receptor binding (RBD) domain (G339D, S371L, 373, N440K, S477N, E484A, Q493R, G496S, Q498R), fusion peptide (FP) region (N764K, D796Y), and the heptad repeat 1 (HR1) region (Q954H, N969K, L9811F). Between the third and fourth wave of infection low sequence coverage of spike was observed, likely due to low caseload, and few mutations were detected. Of the 411 substitutions/ deletions detected during the study period, 68 were present at >1% prevalence. We used the outbreak.info database to compare those mutations to known published mutations at GISAID24 of South African sequences during the study period. Out of the 68 mutations, 58 were commonly reported (Table S4). The remaining 10 mutations (S50L, H66Y, T250S, A288T, K444T, Q498H, D627H, L828F, T859N, AND Q1201K), were detected in wastewater despite being present in <1.0% in the sequences of clinical specimens worldwide from GISAID. Further, 7 of the 10 mutations were detected in <1.0% of sequences in GISAID of South African origin (Fig. 4B), and three mutations (H66Y, T250S, and T859N) were present in a prevalence ranged between 1 and 5.5% in clinical sequences from South Africa (Table 1).
A Heatmap of amino acid mutations distributed across the SARS-CoV-2 spike protein in comparison with the Wuhan reference strain, arranged vertically in chronological order. Each row represents a sample, organized by the date of sample collection from earliest (top) to most recent (bottom). Each column represents an amino acid position of the spike protein annotated by region. The blue rectangle represent mutations were dominate during the third wave at the NTD and HR1, which disappeared during the fourth wave, and the purple rectangle represent new mutations introduced during the fourth wave at the SP, NTD, RBD, subdomains (SD1/SD2), FP, and HR1. B Dot plot showing the uncommon mutations of SARS-CoV-2 detected in wastewater during the period April 2021 – January 2022 and their prevalence. Each row represents specific uncommon mutations, located in the named portion of the spike protein. The x-axis represents the periods (months) and the lines bounded by shaded circles indicate the times at which the mutations were first and last observed (as represented by a continuous line between the dates). The size of the shaded circles in each row represents the number of times the mutation was observed in the collected samples.
Discussion
In this study, we demonstrated that our sequencing methodology and bioinformatics pipeline facilitated detection and genomic characterization of SARS-CoV-2 lineages present in South African wastewater treatment plants during the period April 2021 to January 2022. Our results showed similar VOC spreading dynamics to those observed amongst clinical samples, and identified lineages specific to South African outbreaks, such as the AY.45 lineage that circulated widely during the Delta wave. By analyzing the frequency of signature mutations that uniquely correspond to key variants we were able to recover lineage prevalence measurements, even from low coverage samples. We also performed unbiased analysis of amino acid mutations in the spike gene, which showed both the appearance of mutations associated with well-described lineage transitions as well as a host of amino acid mutations that were uncommon or rarely reported in clinical samples. Collectively, these findings illustrate how sequence analysis of SARS-CoV-2 in wastewater complements epidemiological findings based on clinical sequencing.
Wastewater is a complex matrix containing highly fragmented virus genomic material. Our methodology generated a high number of reads with good quality and depth when compared to other studies that have sequenced SARS-CoV-2 from wastewater25. Because wastewater contains a mix of RNA fragments from viral particles originating from many infected individuals, the generation of consensus sequences is generally not appropriate because the consensus sequences cannot be interpreted as representing a single viral haplotype present in individuals in population, in contrast with standard protocols for clinical sequence data. Our approach allowed for identification of previously described variants in wastewater samples and for detection of new patterns of mutations suggesting previously undescribed variants. We leveraged information on mutation frequency in wastewater samples (using Freyja and our signature mutation analysis) that successfully identified lineages in wastewater that corresponded to lineages identified in clinical specimens23. Results from Freyja were comparable to the prevalence of VOCs of SARS-CoV-2 reported from clinical specimens and additionally indicated the presence of lineages in our wastewater samples that were absent amongst sequences from clinical cases. This may be due in part to sampling biases inherent in clinical surveillance, in which only symptomatic patients are tested and of whom only a fraction was sequenced.
The Beta variant (first described in clinical specimens in South Africa in December 202018) was consistently observed from the start of wastewater surveillance until the end of the third wave in epidemiological week 19 (May 2021). Similarly, the Delta variant was first seen in clinical specimens during epidemiological week 21 of 202120, and was first detected in wastewater samples the same week. Lineage C.1.2, described first in South Africa26 was successfully detected in sequences from wastewater samples during week 22 to 45 in 2021 whilst clinical detections of this lineage appeared from weeks 16 to 46. In epidemiological week 46 in 2021, the Omicron variant was identified in clinical samples whilst sequences from wastewater samples also identified mutations specific to Omicron in the same week.
Our spike gene-wide mutation analysis illustrated how each variant had a distinct mutational profile of RNA sequences of the spike gene, and that this changed in each wave. Through observation of the spike protein heatmap, samples with changing profiles could often be identified before the new variant was sequenced from clinical isolates. This was clear in the transition from the Delta to the Omicron variant, where a constellation of mutations in the NTD decreased in frequency and new mutations appeared in the RBD, FP, and HR1 regions (Fig. 4A). The shifting mutational profile correlated with the increased transmissibility of the Omicron variant that led to the fourth wave of infection in South Arfrica21.
Our mutational analysis identified multiple instances of rare mutations in the population (Fig. 4B). These mutations were found at a prevalence of >1.0% in wastewater samples but were detected at <0.001% in clinical cases based on the data from GISAID. Although they were uncommon, some mutations were reported previously. Mutation S50L was found to be associated with reduced protein stability27. Mutation Q498H has reportedly caused increased binding affinity of RBD to ACE228. The presence of uncommon mutations could be explained as “cryptic lineages” as described by Smyth and colleagues29, which are thought to be attributed the cryptic lineages to either un-sampled, possibly chronic, infections or spillover of SARS-CoV-2 from an unidentified animal reservoir.
Sequencing of SARS-Cov-2 in wastewater currently has a number of limitations. Refining methodological approaches is essential to prevent inhibition from substances within the wastewater matrix. Where the incidence of SARS-CoV-2 is very low, virus concentration in wastewater may proceed below the level of detection, which makes it difficult to amplify and sequence the viral genome. Improvements to virus sampling and enrichment methods may offer better sequencing results, but best practices are yet to be defined, especially for low and middle-income countries. Further, emergence of new variants, such as Omicron sub-variants BA.1 and BA.2, can lead to poor primer binding and lower coverage rates, particularly in the spike protein30, however, this itself may be considered an early warning flag of concerning viral evolution. Both scenarios render sequencing of SARS-CoV-2 from wastewater challenging. In addition, bioinformatics methods for wastewater, including mutational analysis and the Freyja tool, are currently limited by their reliance on lineage assignment based on prior clinical sequencing and publicly available sequences. On the contrary, our unbiased mutational analysis approach provides a potential tool to identify new mutations, which can used as an early warning system for the emergence of new variants.
Sequencing of SARS-CoV-2 from wastewater largely corresponded with sequencing from clinical specimens. The prevalence of VOCs and lineages in clinical specimens was shown to be detectable in wastewater during the same times, which enabled us to provide comprehensive details on VOCs and lineages in the population. Despite inherent limitations of SARS-CoV-2 sampling in wastewater, we have generated a database spanning three SARS-CoV-2 waves, that document variant and lineage changes with time and geographical location and which correspond to clinically identified variants. We have illustrated how sequences not found in clinical specimens may be identified in populations through wastewater. Our mutation-level analyses have the potential to detect new variants prior to detection in clinical samples, which may be particularly useful during times of low disease incidence between waves, when few numbers of positive clinical samples are collected and submitted for testing.
Methods
Wastewater sites
A total of 325 samples were collected from 15 wastewater treatment plants (WWTP) in metropolitan areas also being used for ongoing SARS-CoV-2 quantification by the NICD31. Sites were situated in Gauteng, Eastern Cape, Western Cape, Free State, and KwaZulu- Natal provinces (Figure S1). Supplementary Table S1 shows population sizes in the catchment area for each WWTP, and number of samples collected and sequenced. The samples were collected between April 2021 to January 2022 during the third and fourth waves of SARS-CoV-2 infections in South Africa.
Sample collection, RNA extraction, amplification, and sequencing
One liter of grab sewage samples were collected and transported to NICD at 4 °C. Viruses were concentrated from the sample by taking 200 ml and spin on a centrifuge, then 70 ml was put through a Centricon (Merck, Germany) filter for ultrafiltration32, and RNA was extracted using the QIAamp Viral RNA kit (Qiagen, GmbH, Germany). SARS-CoV-2 was detected by RT-PCR using the AllplexTM 2019- nCoV Assay from Seegene (Seoul, Korea). RNA was re-extracted from SARS-CoV-2 positive concentrates and subjected to amplicon-based whole genome sequencing using the Sinai protocol with some modifications as described previously33. Paired-end libraries were prepared using Illumina COVIDSeq Kit as previously described34 followed by sequencing (2 × 150 bp) on NextSeq 1000/2000 platform (Illumina Inc, USA).
Sequence analysis
Quality control checks
FASTQ files were trimmed, filtered based on sequence quality, assembled, and mapped to the reference genome (NC_045512.2) according to published criteria35 using Exatype web-based bioinformatics tool (https://sars-cov-2.exatype.com/). Samples with a minimum of 1,000,000 reads, a quality Phred score of 30 or more, a sliding window of 4 and a length of 100 bp were processed for mutational analysis using ARTIC protocol (https://artic.network/ncov-2019/ncov2019-bioinformatics-sop.html) in Galaxy (https://usegalaxy.eu/)36. At least 10 reads were required at each nucleotide position for downstream analysis. Amino acid mutations present at 5% of reads or less were removed from the analysis. Table S2 illustrates an example of amino acid variation analysis output.
Analysis using the Freyja tool
To capture the dynamics of virus evolution and spread, we used Freyja37, a tool to estimate the relative abundance of virus lineages present in wastewater. Freyja uses a “barcode” library of lineage-defining mutations to uniquely define all known SARS-CoV-2 lineages and solves for lineage abundance using a depth-weighted, least absolute deviation regression approach. Freyja is free to use and available at https://github.com/andersen-lab/Freyja. Samples with at least 50% genome coverage were included in Freyja analysis.
Clinical samples and sequencing of SARS-CoV-2
The NGS-SA receives randomly selected clinical samples for sequencing every week including remnant nucleic acid extracts or remnant nasopharyngeal and oropharyngeal swab samples from routine diagnostic SARS-CoV-2 PCR testing from public and private laboratories in South Africa. The NGS-SA sequencing hubs used either the Oxford Nanopore Midnight protocol or the Illumina COVIDseq Assay as described in Tegally et al38. All sequences are uploaded into GISAID38 weekly. We downloaded all sequences from GISAID of South Africa origin for that were collected during the period from April 1st, 2021-January 31st 2022 excluding low coverage samples ( > 5% ambiguous bases), and used pangolin lineage assignments. We generated graphs of reported lineage by month of sample collection date using custom Python scripts.
Sequence analysis using amino acid mutations
Amino acid variation analysis
Since SARS-CoV-2 RNA in wastewater is fragmented, and fragments originate from multiple individuals (generally infected with genetically distinct viruses), the generation of consensus sequences from wastewater samples is generally not appropriate because the consensus sequences cannot be interpreted as representing a viral haplotype present in individuals in population. Rather, we inferred the presence of variants by using signature amino acid mutations. The signature mutations were defined as mutations only found in a specific variant at a prevalence of more than 1% of the total sequences deposited in GISAID. We used the amino acid variation data file generated by the ARTIC bioinformatics pipeline and R (version 4.2.0) software to collate spike-gene mutations in a matrix such that the columns represented the amino acid positions of the spike protein and each row recorded and recorded the frequency of mutations (the proportion of all reads at that site with that mutation) for each wastewater sample. Using this list of unique mutations for each VOC and VOI in the spike protein region (Table S3) we interrogated our matrix for the presence or absence of known signature mutations in each sample using R (version 4.2.0) software. As new variants/lineages were detected and identified in the PANGO public database (https://cov-lineages.org/), we added signature mutations to the R (version 4.2.0) code, allowing us to identify the presence of new variants both retrospectively and prospectively.
Visualization of amino acid changes using heatmap and dot blot
Using the amino acid variations data output file from the ARTIC bioinformatics pipeline and the generated excel file that contains all amino acid variations and their respective read frequency, a heatmap was generated and interpreted to visually identify patterns of novel mutations abundance in the spike gene.
Identification of uncommon mutations in the spike gene
To identify the events and times at which uncommon mutations were identified in our samples, an in-house R script (R v.4.2.0) was used to generate a mutational dot plot. We defined uncommon mutations in wastewater samples as mutations that present in the Outbreak.info (https://outbreak.info/) database at less than 1% prevalence during the study period.
Ethics approval and consent to participant
The study did not involve any human participants. An application for ethics waiver was made to the Human Research Ethics Committee of the University of the Witwatersrand and was approved (number R14/49).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data (raw sequence reads) have been deposited to NCBI with accession number (PRJNA941107), and can be found in the link: https://www.ncbi.nlm.nih.gov/bioproject/?term=PRJNA941107. The findings of this study are based on metadata associated with 20,949 sequences available on GISAID up to July 13, 2023, and accessible at https://doi.org/10.55876/gis8.230825ag”. The following database have been used in the study: 1. The Global Initiative on Sharing All Influenza Data (GISAID), available at: https://gisaid.org. 2. Pango lineages: latest epidemiological lineages of SARS-CoV-2, available at: https://cov-lineages.org. 3. National Library of Medicine, National Center for Biotechnology Information (NCBI), accession number: NC_045512.2. 4. Outbreak.info: a tool to explore the COVID-19 and SARS-CoV-2 data with variant surveillance reports, data on cases and deaths, and a standardized, searchable research library, available at: https://outbreak.info/.
Code availability
All data analysis and visualization of wastewater genomic sequencing data was performed using the following: 1. Exatype v4.2.0-dev20230731 available at (https://sars-cov-2.exatype.com). 2. Bioinformatics pipeline on Galaxy, version 0.7.17.1. The pipeline uses BWA mem (Galaxy Version 0.7.17.1), samtools (Galaxy Version 1.9), iVar (Galaxy Version 1.2.2) and LoFreq (Galaxy Version 2.1.5). 3. Freyja (v1.3.10) hosted publicly on github (https://github.com/andersen-lab/Freyja) and is available under a BSD-2-Clause License (doi:10.5281/zenodo.6954863, version 1.3.10). Freyja is accessible as a package via bioconda (https://bioconda.github.io/recipes/freyja/README.html). 4. Custom R (version 4.2.0) and Python scripts available in the project github repository (https://github.com/setshabaTaukobong/Heatmap-Matrix) (https://doi.org/10.5281/zenodo.8252094) and (https://github.com/setshabaTaukobong/Mutational-Dotplot) (https://doi.org/10.5281/zenodo.8252080).
References
Jones, D. L. et al. Shedding of SARS-CoV-2 in feces and urine and its potential role in person-to-person transmission and the environment-based spread of COVID-19. Sci. Total Environ. 749, 141364 (2020).
Vaselli, N. M. et al. Investigation of SARS-CoV-2 faecal shedding in the community: a prospective household cohort study (COVID-LIV) in the UK. BMC Infect. Dis. 21, 784 (2021).
Miura, F., Kitajima, M. & Omori, R. Duration of SARS-CoV-2 viral shedding in faeces as a parameter for wastewater-based epidemiology: Re-analysis of patient data using a shedding dynamics model. Sci. Total Environ. 769, 144549 (2021).
Peng, L. et al. SARS‐CoV‐2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J. Med. Virol. 92, 1676–1680 (2020).
WHO. Environmental surveillance for SARS-COV-2 to complement public health surveillance – Interim Guidance. https://www.who.int/publications/i/item/WHO-HEP-ECH-WSH-2022.1 (2022).
Fontenele, R. S. et al. High-throughput sequencing of SARS-CoV-2 in wastewater provides insights into circulating variants. Water Res. 205, 117710 (2021).
The economist. How covid-19 spurred governments to snoop on sewage. (2022).
COVID19WBEC. COVID-19 WBE Collaborative. https://www.covid19wbec.org/ (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Wang, W. et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 323, 1843–1844 (2020).
Lara, R. W. I. et al. Monitoring SARS-CoV-2 circulation and diversity through community wastewater sequencing. medRxiv (2020).
Crits-Christoph, A. et al. Genome sequencing of sewage detects regionally prevalent SARS-CoV-2 variants. MBio 12, e02703–20 (2021).
DWS. National Integrated Water Information System. https://www.dws.gov.za/niwis2?AspxAutoDetectCookieSupport=1 (2022).
STATS SA. Stats SA General Household Survey 2021. https://www.statssa.gov.za/?p=15482 (2021).
Johnson, R. et al. Qualitative and quantitative detection of SARS-CoV-2 RNA from untreated wastewater in the Western Cape, South Africa. Methodol. Detect. SARS COV 2 RNA lN WASTEWATER SURVElLLANCE 52 (2020).
NICD. Wastewater-based epidemiology for sars-cov-2 in south africa including wastewater genomics. https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/surveillance-reports/weekly-reports/wastewater-based-epidemiology-for-sars-cov-2-in-south-africa/ (2022).
NICD. First case of covid-19 coronavirus reported in SA. https://www.nicd.ac.za/first-case-of-covid-19-coronavirus-reported-in-sa/ (2020).
Tegally, H. et al. Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. MedRxiv (2020).
ECDC. Brief, Threat Assessment: Emergence of SARS-CoV-2 B. 1.617 variants in India and situation in the EU/EEA. (2021).
Tegally, H. et al. Rapid replacement of the Beta variant by the Delta variant in South Africa. MedRxiv (2021).
Karim, S. S. A. & Karim, Q. A. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet 398, 2126–2128 (2021).
Msomi, N. et al. A genomics network established to respond rapidly to public health threats in South Africa. Lancet Microbe 1, e229–e230 (2020).
NICD. Network for Genomic Surveillance in South Africa (NGS-SA). SARS-CoV-2 Sequencing Update 19 August 2022. (2022).
Elbe, S. & Buckland‐Merrett, G. Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob. Chall. 1, 33–46 (2017).
Lou, E. G. et al. Direct comparison of RT-ddPCR and targeted amplicon sequencing for SARS-CoV-2 mutation monitoring in wastewater. Sci. Total Environ. 833, 155059 (2022).
Scheepers, C. et al. Emergence and phenotypic characterization of C. 1.2, a globally detected lineage that rapidly accumulated mutations of concern. (2021).
Laha, S. et al. Characterizations of SARS-CoV-2 mutational profile, spike protein stability and viral transmission. Infect. Genet. Evol. 85, 104445 (2020).
Bate, N. et al. In vitro evolution predicts emerging SARS-CoV-2 mutations with high affinity for ACE2 and cross-species binding. PLoS Pathog. 18, e1010733 (2022).
Smyth, D. S. et al. Tracking cryptic SARS-CoV-2 lineages detected in NYC wastewater. Nat. Commun. 13, 1–9 (2022).
WHO. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (2021).
Iwu-Jaja, C. et al. The role of wastewater-based epidemiology for SARS-CoV-2 in developing countries: cumulative evidence from South Africa supports sentinel site surveillance to guide public health decision-making. Sci. Total Environ. 903, 165817 (2023).
Ikner, L. A., Soto-Beltran, M. & Bright, K. R. New method using a positively charged microporous filter and ultrafiltration for concentration of viruses from tap water. Appl. Environ. Microbiol. 77, 3500–3506 (2011).
Gonzalez-Reiche, A. S. et al. Introductions and early spread of SARS-CoV-2 in the New York City area. Sci. (80-.) 369, 297–301 (2020).
Bhoyar, R. C. et al. High throughput detection and genetic epidemiology of SARS-CoV-2 using COVIDSeq next-generation sequencing. PLoS One 16, e0247115 (2021).
Khailany, R. A., Safdar, M. & Ozaslan, M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 19, 100682 (2020).
Afgan, E. et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2016 update. Nucleic Acids Res. 44, W3–W10 (2016).
Karthikeyan, S. et al. Wastewater sequencing reveals early cryptic SARS-CoV-2 variant transmission. Nature 609, 101–108 (2022).
Tegally, H. et al. Emergence of SARS-CoV-2 omicron lineages BA. 4 and BA. 5 in South Africa. Nat. Med. 28, 1785–1790 (2022).
Acknowledgements
We gratefully acknowledge all data contributors, i.e., the Authors and their Originating laboratories responsible for obtaining the specimens, and their Submitting laboratories for generating the genetic sequence and metadata and sharing via the GISAID Initiative, on which this research is based. We would like to thank the local government and wastewater treatment staff for sample collection and transport. We also thank the staff of the NICD Centre for Vaccines and Immunology and the Centre for Respiratory Disease and Meningitis. special thanks to: Josie Everatt, Boitshoko Mahlangu, Anele Mnguni, Noxolo Ntuli, Gerald Motsatsi for their assistance in setting up and troubleshooting PCR testing, and ongoing supportive collaboration. We thank the team at Hyrax Biosciences for the use of their tool exatype. We would like to acknowledge the contribution from the SACCESS network. We acknowledge the financial support from the National Institute for Communicable Diseases (NICD) of South Africa, Bill, and Melinda Gates foundation (BMGF) the Water Research Commission (WRC) of South Africa (2020/2021-00669//3), the German Society for International Cooperation (GIZ), and the donation of reagents we received from Africa CDC. MY is recipient of a grant by BMGF (INV- 036531). K.G.A. is supported by National Institutes of Health (NIH) National Institute of Allergy and Infectious Diseases U01AI151812 (WARN-ID) and National Center for Advancing Translational Sciences UL1TR002550 (CTSA). J.I.L. is funded by NIH 5T32AI007244-38.
Author information
Authors and Affiliations
Contributions
MY: co-conceptualized study, co-performed analysis, wrote, edited, and reviewed manuscript. SR: co-conceptualized study, edited, and reviewed manuscript. ST: co-performed analysis, edited, and reviewed manuscript. NN: co-performed analysis, edited, and reviewed manuscript. JIL: co-performed analysis, edited, and reviewed manuscript. MS: co-conceptualized, edited, and reviewed manuscript. KM: co conceptualized, edited, and reviewed manuscript. CI, WH, SM, NM, SG, KGA, CS, AvG, NW, JNB, DGA, AI: edited, and reviewed manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yousif, M., Rachida, S., Taukobong, S. et al. SARS-CoV-2 genomic surveillance in wastewater as a model for monitoring evolution of endemic viruses. Nat Commun 14, 6325 (2023). https://doi.org/10.1038/s41467-023-41369-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-41369-5
This article is cited by
-
Monitoring pathogens in wastewater
Nature Reviews Microbiology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.