Abstract
Background/aim
Post-operative uveitis is the most common complication after cataract surgery in the UK. The study aims to evaluate the risk of post-operative uveitis in cataract surgery patients of different ethnicity in the presence and absence of co-morbidities as well as operative complications using multivariate analysis.
Methods
A retrospective case-control study of patients undergoing phacoemulsification cataract surgery between January 2018 to December 2019 at two hospital sites. Differences in demographic and clinical characteristics were compared between two groups defined by the development of post-operative uveitis. Statistically significant factors in univariate analysis were further analysed using multivariate analysis to account for confounders.
Results
One thousand and five hundred eighty seven eyes had undergone phacoemulsification cataract operations with 104 (6.6%) developing post-operative uveitis. Compared to eyes of White/Mixed/Other ethnicity, Asian and Afro-Caribbean eyes were associated with a twofold (OR 2.02, 95% CI 1.16–3.52, P = 0.013) and fivefold (OR 5.15, 95% CI 2.85–9.29, P < 0.001) risk of post-operative uveitis, respectively. Complicated surgery involving eyes with small pupil/iris hooks/Malyugin ring (OR 2.70, 95% CI 1.16–6.30, P = 0.022) and posterior capsular rupture (OR 6.00, 95% CI 2.55–14.12, P < 0.001) were associated with an increased risk of post-operative uveitis.
Conclusions
The factors significantly associated with a post-operative uveitis outcome were patients of Asian and Afro-Caribbean ethnicity, small intra-operative pupil size, use of iris hooks or Malyugin ring and PCR. The post-operative management plan should be tailored in these group of patients with a view of early assessment and prompt management of symptoms.
Similar content being viewed by others
Introduction
Cataract surgery is the most commonly performed ophthalmic surgery in the United Kingdom (UK). According to the Royal College of Ophthalmologists (RCOphth) National Ophthalmology Database (NOD) audit, over 400,000 cataract surgery procedures are performed in England and Wales yearly. Most of these operations are complication free and further improvements have been made to ensure patients continue to receive high quality cataract surgery care. The rate of posterior capsular rupture (PCR) has decreased 38% between 2010 and 2018 to 1.2%. However, post-operative complications still remained above 5% of cataract operations, with the most common being post-operative uveitis at a rate of 1.6% [1].
In the majority of cases, the aetiology of post-operative uveitis is unclear. There is a paucity of evidence surrounding the risk factors for post-operative uveitis in cataract surgery patients. Differences in prevalence of co-morbidities between ethnic groups can increase the risk of operative complications [2]. However, it is still unclear how patient characteristics such as ethnicity and co-morbidities interact with intra-operative complications to inform the risk of post-operative uveitis. Previous studies have only explored risk factors for chronic post-operative uveitis using univariate analysis [3,4,5], which does not account for the interaction between patient characteristics and operative parameters. The aim of our study was to investigate the association of post-operative uveitis with ethnicity, co-morbidities and operative complications together in a multivariate analysis, as this has not been done previously.
Materials and methods
Study design and population
A retrospective case-control study was undertaken in an inner London ophthalmology department at two hospital sites. The sites were chosen on the basis that the catchment area served comprises a diverse ethnic population. According to the Office for National Statistics, the two major boroughs served by the hospital Trust ranked 1st and 5th by ethnic diversity in England and Wales, comprising Asian, Afro-Caribbean and White-Caucasian ethnicities, with a predominantly Bangladeshi population within the Asian ethnicity [6]. Electronic medical records (Medisoft Ophthalmology, Medisoft Limited, Leeds, UK) used by both hospital sites were reviewed to identify eligible cases. The electronic system contained patient charts and peri-operative reports with nationally standardised data categories used by the RCOphth NOD audit [1].
A consecutive series of patients undergoing phacoemulsification cataract surgery between 1 January 2018 to 31 December 2019 were included. Cases with missing data or duplicate entries were excluded. Patients who had surgery on both eyes had one eye randomly excluded from the case set as each eye was statistically correlated to the other and statistical independence had to be assumed for data analysis. Demographic and clinical data were extracted and anonymised in March 2020, allowing a minimum of 2 months for post-operative follow-up and care. The Declaration of Helsinki, Health Research Authority and local Research Ethics Committee guidance on ethical approval was adhered to.
Data fields
Demographic data fields comprised: age at surgery, sex, left or right operated eye and ethnicity. Data on ethnic status were collected according to 15 categories based on electronic medical records. Due to small numbers in several categories, patients were grouped as White, Afro-Caribbean, Asian (with Bangladeshi as a subgroup) and Mixed/Other ethnicity for statistical purposes.
Pre-operative data fields comprised: pre-operative visual acuity (VA), brunescent/white cataract with no fundal view as indicators of hard cataract, diabetes status and ocular co-pathologies.
Operative data fields comprised: presence of intra-operative complications including PCR, markedly small pupils or the use of iris hooks or Malyugin ring derived from operative comments and surgeon grade.
Pre-operative VA refers to the value recorded nearest to the date of surgery. Best-corrected VA was used primarily but where this was not available, unaided VA was used, followed by pin-hole corrected VA. All values were converted to logarithm of the Minimal Angle of Resolution (logMAR) units. Values corresponding to count fingers, hand movements, perception of light (PL) and no PL were substituted with 2.10, 2.40, 2.70 and 3.00 logMAR units, respectively, in keeping with the NOD audit and previous studies [1, 7, 8]. Ocular co-pathologies were not mutually exclusive and were coded individually as being either present or absent.
Following surgery, a standard post-operative care protocol for uncomplicated phacoemulsification was used, consisting of dexamethasone 0.1% eyedrops four times daily to be tapered over 3 weeks after first follow-up within 4 weeks post-operatively. If a complication or iris manipulation has occurred, then the steroid eyedrops are increased to six times daily initially with an early review within 2 weeks post-operatively according to the surgeon’s discretion. All diabetic patients additionally receive ketorolac trometamol 0.5% eyedrops used four times daily for a period of 2 months. If persistent inflammation is observed at first follow-up, then a slower taper of steroid eyedrops was instigated with frequency reductions every fortnight. Topical ketorolac trometamol 0.5% was used as an adjunct in patients with significant uveitis on an individualised basis. All patients with significant uveitis at first post-operative visit would be reviewed in clinic on cessation of drops.
Study outcomes
The primary outcome was the diagnosis of post-operative uveitis after cataract surgery at first follow-up, which was defined as ≥0.5+ for anterior chamber cells with no other cause found apart from the post-operative state, in line with the Standardisation of Uveitis Nomenclature working group report [9]. The decision was made by consultant ophthalmologists or other consultant-supervised staff, such as trainee ophthalmologists and optometrists. This was made on consultant-led clinics and entered on Medisoft. Guidance has been given by the consultant leading the clinic. Based on the outcome, cases were categorised into two groups: post-operative uveitis and no post-operative uveitis.
Statistical analysis
A spreadsheet of anonymised coded data was created on Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and this was imported into SPSS Statistics Version 26 (IBM Corporation, Endicott, NY, USA). Differences in demographic and clinical characteristics were compared between two clinical groups defined by the development of post-operative uveitis. Univariate analysis on categorical data was performed using X2 and Fisher’s exact tests. Continuous data were first examined for normality using the Shapiro–Wilk test and Normal Q–Q plots. As all such data were shown to be non-normally distributed, the Mann–Whitney U and Kruskal–Wallis test was used to compare the variables non parametrically. A multinomial logistic regression model was initially generated to include all factors and covariates found to be significant in univariate analysis and was further refined to include only those significant in this model. Odds ratios (OR) and 95% confidence intervals (CI) were then calculated based off this final model. A P value of <0.05 was considered statistically significant for all statistical tests.
Results
Demographics
Between 1 January 2018 and 31 December 2019, a consecutive series of 2160 eligible operations were identified. 573 patients had surgery on both eyes, of these, one eye was randomly chosen so that each patient contribute only one eye to the data set. The final case set comprised 1587 eyes in total who had undergone phacoemulsification cataract operations with 104 (6.6%) developing post-operative uveitis. 744 patients (46.9%) were male and 843 patients (53.1%) were female. Median age was 69 years (range 16–94 years). 720 patients (45.4%) were Asian consisting of 403 Bangladeshi patients (25.4%) and 317 non-Bangladeshi patients (20.0%), 561 patients (35.3%) were White, 253 patients (15.9%) were Afro-Caribbean and 53 patients were Mixed/Other (3.3%) (Table 1).
Age
Age was found to be non-normally distributed (Shapiro–Wilk P = 0.010). Median age of patients with post-operative uveitis was significantly lower at 66 years than patients with no post-operative uveitis at 69 years (P = 0.024).
Ethnicity
In patients of White ethnicity, 18 eyes (3.2%) had post-operative uveitis, while 2 eyes (3.8%) of Mixed/Other ethnicity had post-operative uveitis. The rate of uveitis between the White and Mixed/Other ethnic groups showed no statistically significant difference, hence the two groups were combined for further analysis. 27 eyes (6.7%) in the Bangladeshi Asian subgroup had post-operative uveitis, while 20 eyes (6.3%) in the non-Bangladeshi Asian subgroup had post-operative uveitis. Similarly, there was no statistically significant difference in post-operative uveitis rate between the Bangladeshi and non-Bangladeshi subgroups, therefore they were combined to form one group ‘Asian’. 37 eyes (14.6%) of Afro-Caribbean ethnicity had post-operative uveitis. The rate of post-operative uveitis differed significantly between the ethnic groups and is highest in Afro-Caribbean patients (P < 0.001).
Pre-operative visual acuity
Pre-operative VA was found to be non-normally distributed (Shapiro–Wilk P < 0.001). Median pre-operative VA was significantly worse in those with post-operative uveitis in (P = 0.040). Unsurprisingly, pre-operative VA was worse in patients with hard cataract (P < 0.001). The median pre-operative VA for patients with hard cataract was 2.10 logMAR compared to 0.48 logMAR in patients without hard cataract. Asian patients had statistically significant worse pre-operative VA than Afro-Caribbean and White/Mixed/Other patients (P = 0.001).
No fundal view
Fifty-five patients (3.5%) were reported to have no fundal view in the operated eye and this factor was significantly associated with post-operative uveitis (P = 0.024) and 8 (14.5%) of those in this category went on to develop post-operative uveitis compared to 96 (6.3%) of 1532 patients not reported in this category. No fundal view was also significantly associated with PCR during the operation (P = 0.003).
Co-morbidities
Four hundred thirty seven (60.7%) Asian, 115 (45.5%) Afro-Caribbean and 150 (24.4%) White/Mixed/Other patients were diabetic. The rate of diabetes differed significantly between ethnic groups (P < 0.001) but was not significantly associated with post-operative uveitis (P = 0.475). None of the recorded ocular co-morbidities were significantly associated with post-operative uveitis (Table 2).
Small pupil/iris hooks/Malyugin ring
Forty nine (3.1%) of the eyes operated on had a markedly small pupil or required the use of iris hooks or Malyugin ring and 8 (16.3%) of those within this category went onto develop post-operative uveitis compared to 96 (6.2%) of 1538 cases not in this category. This factor was significantly associated with post-operative uveitis (P = 0.012).
Operative complications
Sixty eight (4.3%) of the eyes operated on had an intra-operative complication, of which 30 eyes (1.9%) had PCR. 9 (30%) of those with PCR developed post-operative uveitis compared to 95 (6.1%) of 1557 cases without. PCR was significantly associated with post-operative uveitis (P < 0.001). Post-operative uveitis was also significantly associated with all intra-operative complications (P = 0.011), however this significance was lost when PCR was excluded, suggesting that this was due to the high significance of PCR alone. The surgeon’s grade was not significantly associated with post-operative uveitis (Table 3).
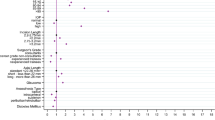
Multivariate analysis
A multiple logistic regression model was calculated with post-operative uveitis as the dependent variable and factors (ethnicity, no fundal view, small pupil/iris hooks/Malyugin ring and PCR) and covariates (age and pre-operative VA) which had been found to be significant in the univariate analysis. On running the model, no fundal view, age and pre-operative VA were shown to be insignificant with P values of 0.566, 0.209 and 0.129, respectively. The model was run again without these insignificant variables (Table 4).
Compared to eyes of White/Mixed/Other ethnicity, eyes of Asian and Afro-Caribbean ethnicity were twice as likely (OR 2.02, 95% CI 1.16–3.52, P = 0.013) and five times as likely (OR 5.15, 95% CI 2.85–9.29, P < 0.001) to develop post-operative uveitis, respectively. Eyes with small pupil/iris hooks/Malyugin ring were 2.7 times more likely to develop post-operative uveitis than eyes without (OR 2.70, 95% CI 1.16–6.30, P = 0.022). Eyes with PCR were six times more likely to develop post-operative uveitis than eyes without (OR 6.00, 95% CI 2.55–14.12, P < 0.001).
Age was found to be statistically insignificant in multivariate analysis and its apparent significance in the univariate analysis could be due to Afro-Caribbean patients being younger and patients of White/Mixed/Other ethnicity being older. The median age of Afro-Caribbean patients was 68 years compared to patients of White/Mixed/Other ethnicity which was 73 years and a comparison of age distribution across these two groups showed a statistically significant difference (P < 0.001). This suggests that the apparent significance of age in the univariate analysis is related to the difference in ethnicity instead of post-operative uveitis. Similarly, no fundal view and pre-operative VA were both found to be insignificant in multivariate analysis. Their apparent significance in univariate analysis is probably because they are strong predictors of PCR, which was found to be a significant factor in the multivariate analysis.
Confounding associations between the significant risk factors were accounted for through the multivariate analysis. The factors significantly associated with a post-operative uveitis outcome were patients of Asian and Afro-Caribbean ethnicity, a complicated surgery with markedly small pupils, iris hooks or Malyugin ring use and PCR. Chi-squared analysis also showed that there is no significant association between ethnicity, use of pupil expansion devices and PCR, indicating that each of these factors are independent risk factors and not confounding.
Discussion
This study reported on the risk factors for post-operative uveitis using ethnicity, ocular co-pathologies and operative complications together using a robust multivariate analysis. Post-operative uveitis remains the most common complication after an ophthalmic surgery within the UK. This can cause pain, decreased vision and patient distress in the acute phase [10]. As the number of cataract operations performed yearly continues to rise, post-operative uveitis increasingly represents a significant burden amongst uveitis cases. Identifying risk factors associated with post-operative uveitis will allow a better understanding of the possible underlying aetiologies or predisposing factors of post-operative inflammation, which can help guide management in this group of patients.
The results of this study suggest that patient ethnicity remains a significant factor in the development of post-operative uveitis. Afro-Caribbean patients are at the highest risk of developing post-operative uveitis followed by a smaller but significantly higher risk in Asian patients compared to patients of White/Mixed/Other ethnicity. There have been reports of similar associations in American studies. A recent study by Edmiston et al. found that African American patients were significantly more likely to develop post-operative inflammation after combined phacoemulsification and endoscopic cyclophotocoagulation compared to patients of White ethnicity [11]. Similarly, two other studies found a significantly higher risk of persistent anterior uveitis in African American patients who had undergone cataract surgery [3, 4].
There are several theories behind the higher incidence of post-operative inflammation in Afro-Caribbean and Asian patients. The first being a higher amount of melanin in Afro-Caribbean and Asian eyes. Melanin is thought to augment intraocular inflammation and melanin-induced uveitis in animal models resemble acute anterior uveitis in humans [12, 13]. The second being differences in inflammatory response between ethnic groups. Studies have shown a higher risk of inflammation and oxidative stress in patients of African ethnicity in the USA [14, 15]. It is possible that a stronger inflammatory response after cataract surgery combined with a higher ocular melanin content have led to a significantly higher risk of post-operative uveitis in Afro-Caribbean patients and in Asian patients to a smaller extent.
Surprisingly, diabetes was not a statistically significant risk factor for post-operative uveitis in our study, despite type 2 diabetes being three and five times more common in people of Afro-Caribbean and South Asian descent, respectively, and a study from the USA reported diabetes as a risk factor for persistent post-operative iritis [3, 16]. This may be due to the protective effect of additional anti-inflammatory therapy received by diabetic patients, as they were routinely given ketorolac trometamol eyedrops in addition to steroids post-operatively.
Complicated surgery involving markedly small pupils, the use of iris hooks or Malyugin ring or the occurrence of a PCR was associated with an increased risk of post-operative uveitis. The use of intra-operative pupil expansion devices together with small pupils can lead to greater iris trauma during device placement or manipulation during surgery, which leads to the disruption of the blood–aqueous barrier. This is consistent with findings from the study by Neatrour et al. which found an increased risk of persistent iritis after cataract operations that involved the use of pupil expansion devices [3].
PCR is a very strong risk factor for post-operative uveitis, as it results in prolonged surgery, with greater likelihood of iris manipulation, and the need for vitrectomy. There is also the potential for retained lens fragments. All of these factors have the potential for causing ocular inflammation. Even with uncomplicated phacoemulsification, there is evidence of prolonged disruption of the blood–aqueous barrier post-operatively as measured by anterior chamber flare metre, therefore PCR would be expected to cause greater barrier disruption [17]. However, it is important to consider that the individual examining patients with PCR might be more vigilant in looking for presence of anterior chamber cells, which could overestimate the relationship strength between PCR and post-operative uveitis.
Based on the findings of the study, we recommend an earlier post-operative review and a more gradual taper of topical anti-inflammatory drops with greater reliance on topical non-steroidal anti-inflammatory drugs (NSAIDs) for all patients with risk factors of post-operative uveitis. We also recommend the addition of topical NSAIDs as routine for all Afro-Caribbean patients. A randomised study has suggested that the addition of a topical NSAID to topical steroid therapy significantly reduces intraocular inflammation in the early post-operative period [18]. A systematic review of 48 randomised clinical trials have shown that topical NSAIDs and steroids are equally effective [19]. Both drops can be used synergistically to manage patients with post-operative uveitis at the early post-operative stage.
The main limitation of the study is that it is a retrospective study, therefore the true incidence cannot be determined and there are disproportionate numbers within each patient group. However, confounders have been accounted through the use of multivariate analysis. A retrospective study also meant that the follow-up period is not identical between patients although they were seen within 4 weeks post-operatively. Another limitation is that patient characteristics and outcomes were confined to information available on the electronic medical records. Characteristics such as patient symptomatology and treatment compliance could not be assessed unless they were specifically reported in the records.
In conclusion, the strongest predictive factors for post-operative uveitis after cataract surgery were PCR and Afro-Caribbean ethnicity, followed by markedly small pupils or the use of iris hooks or Malyugin ring and Asian ethnicity. Prompt management of post-operative inflammation in these groups of patients is key as it can cause significant pain, decreased vision and anxiety in the acute phase. The post-operative treatment plan should be tailored in these group of patients with a view to alleviate symptoms and improve recovery. Future work can involve evaluating the efficacy of early treatment in patients that fall under these risk groups.
Summary
What was known before
-
Post-operative inflammation can cause pain, decreased vision and patient distress in the acute phase.
-
Differences in prevalence of co-morbidities between ethnic groups can increase the risk of operative complications.
-
USA studies have shown that diabetes, African American ethnicity, use of pupil expansion devices and intra-operative complications were associated with increased risk of chronic post-operative uveitis.
What this study adds
-
Accounts for the interactions and confounders between ethnicity, co-morbidities and operative complications through multivariate analysis.
-
Perspective from an ethnically diverse inner London population.
-
Risk factors are Asian and Afro-Caribbean ethnicity, small intra-operative pupil size, use of pupil expansion devices and PCR.
References
Henry P, Donachie J, Sparrow JM. Year 4 annual report—the third prospective report of the National Ophthalmology Database Audit Improvement Partnership 2 NOD audit fourth annual report—third prospective audit year report. 2019. www.hqip.org.uk/national-programmes.
Oyewole K, Tsogkas F, Westcott M, Patra S. Benchmarking cataract surgery outcomes in an ethnically diverse and diabetic population: final post-operative visual acuity and rates of post-operative cystoid macular oedema. Eye. 2017;31:1672–7.
Neatrour K, McAlpine A, Owens TB, Trivedi RH, Poole, Perry LJ. Evaluation of the etiology of persistent iritis after cataract surgery. J Ophthalmic Inflamm Infect. 2019;9:4.
Reddy AK, Patnaik JL, Miller DC, Lynch AM, Palestine AG, Pantcheva MB. Risk factors associated with persistent anterior uveitis after cataract surgery. Am J Ophthalmol. 2019;206:82–6.
Patel C, Kim SJ, Chomsky A, Saboori M. Incidence and risk factors for chronic uveitis following cataract surgery. Ocul Immunol Inflamm. 2013;21:130–4.
Office for National Statistics. Regional ethnic diversity—GOV.UK Ethnicity facts and figures. England and Wales 2011 Census. 2018. https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/national-and-regional-populations/regional-ethnic-diversity/latest#ethnic-diversity-by-area.
Chu CJ, Dick AD, Johnston RL, Yang YC, Denniston AK. Cataract surgery in uveitis: a multicentre database study. Br J Ophthalmol. 2017;101:1132–7.
Day AC, Donachie PHJ, Sparrow JM, Johnston RL. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye. 2015;29:552–60.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Atmaca LS, Becker MD, Brezin AP, et al. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005;140:509–16.
Mohammadpour M, Jafarinasab MR, Javadi MA. Outcomes of acute postoperative inflammation after cataract surgery. Eur J Ophthalmol. 2007;17:20–8.
Edmiston AM, Soohoo JR, Seibold LK, Kahook MY, Palestine AG, Pantcheva MB. Postoperative inflammation after endoscopic cyclophotocoagulation: racial distribution and effect on outcomes. J Glaucoma. 2018;27:266–8.
Kaya M, Edward DP, Tessler H, Hendricks RL. Augmentation of intraocular inflammation by melanin. Investig Ophthalmol Vis Sci. 1992;33:522–31.
Smith JR, Rosenbaum JT, Williams KA. Experimental melanin-induced uveitis: experimental model of human acute anterior uveitis. Ophthalmic Res. 2008;40:136–40.
Carroll JF, Fulda KG, Chiapa AL, Rodriquez M, Phelps DR, Cardarelli KM, et al. Impact of race/ethnicity on the relationship between visceral fat and inflammatory biomarkers. Obesity. 2009;17:1420–7.
Feairheller DL, Park JY, Sturgeon KM, Williamson ST, Diaz KM, Veerabhadrappa P, et al. Racial differences in oxidative stress and inflammation: in vitro and in vivo. Clin Transl Sci. 2011;4:32–7.
Goff LM. Ethnicity and Type 2 diabetes in the UK. Diabet Med. 2019;36:927–38.
Siriwardena D, Kotecha A, Minassian D, Dart JKG, Khaw PT. Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol. 2000;84:1056–7.
Shilpy N, Patel DB. Comparison of nepafenac plus steroid versus steroid alone for control of ocular inflammation after phacoemulsification. Int J Contemp Med Res. 2019;6:A1–A3.
Juthani VV, Clearfield E, Chuck RS. Non-steroidal anti-inflammatory drugs versus corticosteroids for controlling inflammation after uncomplicated cataract surgery. Cochrane Database Syst Rev. 2017;7:CD010516.
Acknowledgements
The authors thank Mr. Mark Westcott, Medical Retina Department, Moorfields Eye Hospital, for his expert comments on the paper.
Author information
Authors and Affiliations
Contributions
Study conception: JH, NC and AC. Data collection: JH and NC. Statistical analysis: FW. Paper drafting: JH and FW. All authors contributed to the critical review and final approval of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Halim, J., Westcott, F., Cascone, N. et al. Risk factors associated with post-operative uveitis after cataract surgery: a retrospective case-control study. Eye 36, 198–205 (2022). https://doi.org/10.1038/s41433-021-01486-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01486-1