Abstract
Purpose
To examine the incidence, characteristics and outcomes of posterior capsular rupture (PCR) cases amongst the ophthalmology trainees and to evaluate the trainees’ confidence in managing PCR.
Methods
A two-staged cross-sectional study was carried out between September 2017 and April 2018 in the North East of England, UK. All ophthalmology trainees were surveyed on their confidence level in managing PCR and the characteristics and outcomes of their PCR cases.
Results
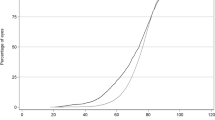
Fifteen (71.4%) out of 21 trainees completed the study. The mean number of phacoemulsification was 268.9 ± 250.9 cases (range, 0–705) per trainee. There were 82 (1.9%) cases of PCR reported among 4303 phacoemulsification. PCR occurred most commonly during quadrant removal (44.0%) and cortex removal (21.3%). The best-corrected visual acuity (in logMAR) improved significantly from 0.47 ± 0.32 preoperatively to 0.20 ± 0.19 postoperatively (p < 0.001). The supervising consultant took over 80.5% of the PCR cases. The PCR rate decreased significantly from 3.1% at 0–100 cases to 0.6% at 301–400 cases (p = 0.004) and to 0.4% at >500 cases (p = 0.005). Confidence in managing PCR (without supervision) improved from 0% (9/9) at junior level to 50% (3/6) at senior level, and the average number of anterior vitrectomies performed was 0.6 ± 0.9 (range: 0.0–2.0).
Conclusions
We observed a low PCR rate among the trainees in our region, with the majority of cases achieving good visual outcome. A significant reduction in PCR rate was observed at the threshold of >500 cases. There is however a lack of confidence among trainees in managing PCR, highlighting the need for devising new training strategies in this area.
Similar content being viewed by others
Introduction
Cataract surgery is the most commonly performed surgery in the world [1]. With the growing population and increasing life expectancy, the demand for cataract surgery is expected to continue to rise in the future [2]. Despite the rising pressure on ophthalmology services, the safety of cataract surgery remains high with good visual outcome and low complication rate [3]. Whilst safety of cataract surgery can be defined in many ways, posterior capsule rupture (PCR) rate often serves as one of the most important indicators. This is primarily attributed to the fact that PCR can negatively impact on the visual outcome and result in significant complications such as retinal detachment and endophthalmitis [3,4,5].
Cataract surgery is one of the core competencies embedded within the ophthalmology training curriculums in many countries, including the UK. Studies have shown that ~10–35% of cataract surgeries were performed by trainees [6, 7], highlighting the substantial impact of trainee-performed surgeries on patients and healthcare services. In the UK, trainees are required to perform a minimum number of 350 cataract surgeries independently—a level set by the Royal College of Ophthalmologists—prior to being certified as an ophthalmology specialist. As trainees progress through their 7-year training programme, they are expected to deal with more complex cases and manage potential intraoperative complications such as PCR. However, with the increasing safety of cataract surgery [6, 8], there is concern over the lack of experience and confidence among ophthalmic trainee surgeons in managing complications such as PCR [9, 10].
To date, there are only limited studies that have specifically examined the characteristics and outcomes of PCR among ophthalmology trainees [11, 12]. Day et al. [6] reported that the visual outcome following cataract surgery was similar between trainees and consultant ophthalmologists in the UK; however, there was no specific evaluation on the characteristics or outcomes of PCR cases related to trainee surgeons. In view of the paucity of literature, this study aimed to examine the incidence, characteristics, and outcomes of PCR among the ophthalmology trainees in the North East of England, UK, as well as to evaluate their confidence level in managing PCRs.
Materials and methods
This was a two-staged cross-sectional study carried out between September 2017 and April 2018 and involved all members of the North East Trainee Research in Ophthalmology Network (NETRiON) working in five tertiary hospitals in the North East of England, UK [13, 14]. Ethical approval was not required as this retrospective study was classified as a service evaluation study. The study was conducted in accordance with the tenets of Declaration of Helsinki.
Stage 1: questionnaire-based survey
In order to assess the experience and confidence in dealing with PCR, an electronic questionnaire-based survey (see Supplementary Table 1) was sent to all NETRiON trainees via email in September 2017, followed up by another reminder email in November 2017. Relevant data, including the trainee’s grade, total number of cataract surgeries, PCR and anterior vitrectomies performed, confidence in managing PCR and potential strategies to improve confidence, were collected from trainees’ e-logbook and analysed.
Stage 2: retrospective examination of PCR cases
At the second stage, all the respondents were asked to retrospectively review all of their PCR cases via e-medical records and case notes for further data collection. Eligible cases were those performed on patients aged ≥18 years using phacoemulsification. PCR, with or without vitreous loss, was defined as an unintentional communication with the posterior segment as result of a breach in the posterior capsule. The following data were included for the study: trainee’s grade at time of PCR, number of cataract cases they had completed prior to the PCR, preoperative best-corrected visual acuity (BCVA), ocular co-morbidities (that could affect the visual prognosis), potential surgical complicating factors (based on Muhtaseb et al. risk-scoring system) [15], type of anaesthesia used, stage of surgery when PCR occurred, any primary insertion of intraocular lens (IOL), degree of senior supervision, take-over by supervisor, involvement of the vitreoretinal team, complications and post-operative BCVA (defined by the best-measured visual acuity within 1 year of post cataract surgery). The second stage of study was completed in April 2018.
Statistical analysis
Statistical analysis was performed using SPSS version 26.0 (IBM SPSS Statistics for Windows, Armonk, NY, USA). Snellen vision was converted to logMAR vision for analytic purpose and counting fingers were quantified as 1.9 logMAR [16]. Significant visual loss was defined as a reduction of BCVA by ≥0.30 logMAR between preoperative and post-operative visits [6]. Comparison between groups was conducted using Pearson’s Chi-square or Fisher’s Exact test where appropriate for categorical variables, and T-test or Mann–Whitney U test for continuous variables. Normality of data distribution was assumed if the skewness and kurtosis z values were between −1.96 and +1.96 and the Shapiro–Wilk test p value was >0.05. All continuous data were presented as mean ± standard deviation.
For descriptive and analytic purposes, trainees were divided into two groups, namely the junior trainees who were in ophthalmic specialist training (OST) year 1–4 and senior trainees who were in OST5–7. In addition, influence of trainees’ experience on the PCR rate was analysed in 5 groups of 100 cases in succession, from 0–100 cases to >500 cases. p value of <0.05 was considered statistically significant and crude Bonferroni-type adjustment was used for subgroup analysis to keep the overall false positive rate at 0.05 [e.g., p value of <0.01 (based on 0.05/5) was considered significant if five subgroups were compared] [17].
Results
Of all 21 members of NETRiON, 15 (71.4%) trainees completed both parts of the study; 9 (60.0%) and 6 (40.0%) were junior (OST1–4) and senior trainees (OST5–7), respectively. All senior trainees were either in OST6 or OST7. A total of 4303 phacoemulsification operations were performed with 82 (1.9%) PCR episodes being reported. The mean number of phacoemulsification was 268.9 ± 250.9 cases (range, 0–705) per trainee.
Preoperative and intraoperative characteristics
Based on 59 (72.0%) cases with available information (missing data were due to case note unavailability), the mean preoperative BCVA (in logMAR) was 0.47 ± 0.32 (range, 0.0–1.9). Ocular co-morbidities were present in 15 (18.3%) cases, with age-related macular degeneration (11, 73.3%) being the most common condition. Surgical complicating factors were reported in 13 (15.9%) cases, with 7 (8.5%) cases having one factor and 6 (7.3%) cases having two factors (Table 1). Of all 19 reported factors, small pupil (5, 26.3%), uncooperative patient (5, 26.3%), shallow anterior chamber (4, 21.1%) and use of alpha-blocker medication/intraoperative floppy iris syndrome (3,15.8%) were the common factors. No difference was noted in the proportion of ocular co-morbidities (p = 1.0) and surgical complicating factors (p = 0.72) between the junior and senior trainees’ groups (Table 1). Of the 77 cases with recorded anaesthetic method, topical ± intracameral anaesthesia (41, 53.2%) was the most commonly used method, followed by sub-Tenon’s (33, 42.9%), retrobulbar (2, 2.6%) and general anaesthesia (1, 1.3%).
Characteristics and management of PCR
Of the 82 (1.9%) with PCR, vitreous loss was reported in 62 (75.6%) cases. Of 75 cases with available information, PCR occurred most commonly during the stage of quadrant removal (33, 44.0%), followed by cortex removal (16, 21.3%), and insertion of IOL (10, 13.3%; Fig. 1). There was a borderline significant difference in the stages of PCR between junior and senior trainee groups (p = 0.06), particularly during hydrodissection (3.4% vs. 17.6%), cortex removal (17.2% vs. 35.3%) and IOL insertion (15.5% vs. 5.9%; Table 1). One case occurred during the stage of wound hydration, which was secondary to an inadvertent cannula injury. Of 78 cases with available information, a primary IOL was inserted in 58 (74.4%) cases at the time of complication, with 40 (69.0%), 17 (29.3%) and 1 (1.7%) cases of IOL implanted in the sulcus, in the bag, and in the anterior chamber, respectively.
In the majority of cases (66, 80.5%), the supervising consultant took over the case and managed the PCR. The take-over rate reduced significantly as the trainees progressed from junior to senior level (p < 0.001; Table 1 and Fig. 2). Of the 16 (19.5%) PCR cases managed by trainees, 4 (25.0%) and 12 (75.0%) were performed by the junior and senior trainees, respectively. When the PCR occurred, the supervising consultant was scrubbed with the trainee in 43 (52.4%) cases, and this was significantly higher in cases performed by the junior trainees (p = 0.002; Table 1). Referral to vitreoretinal team was warranted in 21 (25.6%) cases.
Post-operative visual outcome and complications
Of 59 (72.0%) recorded cases, the mean BCVA (in logMAR) improved significantly from 0.47 ± 0.32 to 0.20 ± 0.19 (p < 0.001). The proportion of patients with BCVA ≤ 0.3 logMAR (equal or better than 6/12) improved significantly from 26 (44.1%) patients to 46 (78.0%) patients (p < 0.001; Fig. 3). In 47 patients with no ocular co-morbidity (and with available information), 41 (87.2%) patients achieved BCVA of ≤0.3 logMAR. Two (3.4%) patients experienced significant visual loss (>0.3 logMAR) due to persistent cystoid macular oedema (CMO).
Influence of trainees’ experience on PCR rate
Overall, the PCR rate was 2.5% (63 of 2473 cases) and 1.0% (19 of 1830 cases) during junior and senior training years, respectively. Compared to the first 100 cases of cataract surgery, there was a significant decrease in the risk of PCR by 81% at 301–400 cases (p = 0.006) and by 87% after 500 cases (p = 0.005; Table 2).
Confidence in managing PCR
There was a significant difference in the confidence level of managing PCR between junior and senior trainees (Table 1). Overall, eight (53.3%) trainees were not confident in managing PCR even with supervision and only three (50%) of six senior trainees were confident in managing PCR without supervision. In 24 (37.5%) of the 64 PCR cases which were taken over by the supervising consultant, trainees stated that they would like to have continued with the case themselves and developed skills in managing PCR. In the other 40 (62.5%) cases, lack of experience and/or confidence was reported as the main reason why the trainees did not want to manage the PCR. In 2 (3.1%) cases, time constraint was reported to be the main factor why PCR was not managed by the trainee.
The mean number of anterior vitrectomies performed by trainees was 0.6 ± 0.9 (range: 0.0–2.0) with senior trainees having performed a mean of 1.2 ± 1.0 (range 0.0–2.0). Two (33%) senior trainees had never performed an anterior vitrectomy. The trainees felt that they needed to manage at least an average of 6.4 ± 5.0 PCR cases (range, 2–20) in order to handle the complication confidently as a consultant.
Discussion
To the best of our knowledge, this represents the first study examining the incidence, characteristics, outcomes and confidence in managing PCR during cataract surgery amongst the ophthalmology trainees in the North East of England, UK. Based on 4303 cases of phacoemulsification, we demonstrated a 1.9% PCR rate among the ophthalmology trainees in our region. This was considerably lower than the rate reported in the literature, which was estimated at 5.7% based on 44 studies [18]. The heterogeneity of PCR rate could be attributed to the variations in the length and intensiveness of the training programmes, the case-mix, and the surgical experience of trainees.
As with any type of surgery, phacoemulsification is associated with a learning curve. According to the UK National Ophthalmology Database, the overall PCR rate of consultant ophthalmologists and trainee surgeons were 1.6% and 3.2%, respectively [6]. Randleman et al. [19] reported a considerable difference in the PCR rate before and after 80 cases (6.3% vs. 3.5%). In a similar vein, we observed a significant bimodal reduction in the risk of PCR from 3.1% (at 0–100 cases) to 0.6% (after 300 cases) and to 0.4% (beyond 500 cases). An important point to consider which can significantly affect complication rates in cataract surgery is the complexity of cases which trainees are operating on [15, 20]. In our study, 16% of eyes had at least one complicating factor which made the surgery more difficult. However, there was no significant difference in the number of complicating factors between junior and senior trainees’ groups, suggesting that the higher PCR rate in the former group was related to the learning curve of surgery.
With the recent “Get It Right First Time” report [21], UK hospitals are bench marked to perform at least eight cataract operations within a 4-h session. Because of these time constraints, it is likely that more difficult cases will be allocated to consultants. With careful selection of case-mix using a risk-stratifying system, sufficient time may be allocated for the trainees to perform on high-risk cases [5, 15, 20, 22].
Characteristics of PCR
In our study, we demonstrated that PCR most commonly occurred during quadrant removal (44%) and cortex removal (21%). This pattern remained similar between junior and senior trainees’ groups. This parallels the findings of a study conducted in Singapore where phacoemulsification (60%) and irrigation/aspiration (25%) were found to be the most common stages of PCR based on 887 cases [12]. Knowledge of the most common stages in which PCR occurs can enable trainers to place more emphasis and closer supervision in these areas when teaching ophthalmology trainees. Interestingly, 13% of PCR cases occurred during the stage of IOL insertion in our study. Further post hoc “face-to-face interview” with the involved trainees revealed that a few cases were related to the use of an unfamiliar three-piece IOL and other cases were reported that the stage of PCR was uncertain but was noted during the IOL insertion. In addition, one PCR case occurred during the last stage of cataract surgery (i.e., wound hydration) secondary to an inadvertent cannula injury, which has been recognised as a rare yet potentially sight-threatening complication of cataract surgery [23, 24].
Visual outcome and complication
Studies have shown that PCR is a significant modifiable adverse risk indicator for visual prognosis and major complications following cataract surgery [3, 5, 12]. In a study of cataract surgery complicated by PCR [12], the visual outcome was significantly worse when compared to uncomplicated surgeries (94% of eyes achieving ≥6/12 in PCR cases compared to 99% in uncomplicated cases). However, there was no statistical difference in visual outcomes between cases performed by faculty and residents. In our study, we demonstrated that good outcome can be achieved following PCR among ophthalmology trainees, with a mean improvement of 0.28 logMAR vision. Visual outcomes were similar to the results of the National Ophthalmology Database Audit where 77% of eyes with PCR (performed by trainees or consultants) had a post-operative BCVA of logMAR ≤ 0.3 [3]. In addition, our results were better than a previous study of 133 eyes with complicated cataract surgery where significant improvement of BCVA (≥3 Snellen lines) was only achieved in 44% of patients at 12 months post operative [25]. Two (3.4%) of our patients experienced significant visual loss (>3 Snellen line) due to persistent CMO, for which the treatment was still ongoing.
The favourable outcomes observed in our study might be attributable to careful supervision of the trainees during surgery with high take-over rate (81%) by the supervising surgeon, and good post-operative management. However, it is important to strike a fine balance between achieving good outcome and training the trainees to manage PCR independently and safely.
Confidence in managing PCR
Increased safety of cataract surgery combined with reduced working hours for trainees have limited the amount of surgical training and reduced the opportunities for trainees to deal with cataract complications. Our study adds further evidence to this with the mean number of anterior vitrectomies carried out by trainees being 0.6, with 33% of senior trainees having never performed an anterior vitrectomy. We found that only 50% of senior trainees felt confident in managing PCR without supervision. Although this was higher than the rate (18%) reported in the Wessex Deanery [9], it was lower than the rate (74%) reported in a recent UK study [10]. In order to produce junior consultants who are confident in managing PCR themselves and teaching trainees on managing PCR, it is important for them to develop this competency before their CCT.
Surgical simulation (e.g., Eyesi surgical simulator, VRMagic Holding AG, Mannheim, Germany) and vitrectomy training during vitreoretinal rotations have been suggested to enhance trainees’ confidence in cataract surgery and reduce complication rate [9, 10, 26]. In addition, as all OSTs are expected to attend the RCOphth microsurgical skill course at the start of training, a potential solution is to perhaps roll out a mandatory RCOphth-based course on the management of PCR during OST4–5 level to improve the trainees’ competency and confidence. Although not evaluated in this study, other potential issues that could also affect the training of cataract surgery include high volume private providers cherry picking the easy cataract surgery cases locally, increased pressure on service demand where high volume cataract lists are required, and the lack of wet lab or cataract/VR surgery simulation platforms in some regions.
Limitations
One of the limitations of this study is that the results were restrained to only one of the 15 deaneries in England. However, all trainees in the UK are required to undergo the same robust national training programme that is approved and accredited by the Royal College of Ophthalmologists and the General Medical Council. We therefore believe that our results are likely to be representative of the training throughout the country. Future similar studies conducted at the national level would help further validate our findings and ascertain the underlying factors that could affect the training of cataract surgery and management of PCR. Another limitation of the study is that the results are based on the accuracy of the documentation and therefore the trainee’s subjective assessment of the operation, including stages of PCR occurred and surgical complicating factors. Video recording—an invaluable teaching and training tool—would also help provide more accurate and objective assessment of these PCR cases. Long-term follow-up of these cases would also provide invaluable information on the long-term outcome and complications such as retinal detachment, which may not manifest during the first post-operative year.
In conclusion, this study provides detailed information on the incidence, characteristics and outcomes of PCR among ophthalmology trainees and evaluates their perspective and confidence in managing PCRs. We observed that good visual prognosis can be achieved in these patients when PCR was appropriately managed. However, we observed a lack of confidence among trainees in managing PCR, highlighting the need for devising new training strategies in this area.
Summary
What was known before
-
Cataract surgery is associated with a learning curve.
-
The rate of posterior capsular rupture (PCR) among ophthalmology trainees was estimated at 5–6% in the recent literature.
-
Few studies have highlighted the lack of experience and confidence in managing cataract surgery complications.
What this study adds
-
This represents the first study in the North East of England that examined the incidence, characteristics and outcomes of PCR among the ophthalmology trainees.
-
We observed a low (1.9%) PCR rate among the ophthalmology trainees, with good visual outcome being achieved in the majority of cases.
-
The risk of PCR significantly decreased after the threshold of 500 cases.
-
PCR most commonly occurred during quadrant removal and cortex removal.
-
There is a lack of experience and confidence in managing PCR among the trainees, with a high consultant take-over rate (81%).
References
https://ec.europa.eu/eurostat/statisticsexplained/index.php/Surgical_operations_and_procedures_statistics#Number_of_surgical_operations_and_procedures. Accessed 2 May 2020.
Minassian D, Reidy A. Future Sight Loss UK: an epidemiologic and economic model for sight loss in the decade 2010-20. A RNIB report; 2009.
The Royal College of Ophthalmologists. National Ophthalmology Database Audit, year 4 annual report—the third prospective report of the National Ophthalmology Database Audit; 2019.
Ionides A, Minassian D, Tuft S. Visual outcome following posterior capsule rupture during cataract surgery. Br J Ophthalmol. 2001;85:222–4.
Sparrow JM, Taylor H, Qureshi K, UK EPR user group. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: risk indicators for monocular visual acuity outcomes. Eye. 2012;26:821–6.
Day AC, Donachie PH, Sparrow JM, Johnston RL. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye. 2015;29:552–60.
Low SA, Braga-Mele R, Yan DB, El-Defrawy S. Intraoperative complication rates in cataract surgery performed by ophthalmology resident trainees compared to staff surgeons in a Canadian academic center. J Cataract Refract Surg. 2018;44:1344–49.
Ting DS, Rees J, Ng JY, Allen D, Steel DH. Effect of high-vacuum setting on phacoemulsification efficiency. J Cataract Refract Surg. 2017;43:1135–9.
Turnbull AM, Lash SC. Confidence of ophthalmology specialist trainees in the management of posterior capsule rupture and vitreous loss. Eye. 2016;30:943–8.
Dean WH, Grant S, McHugh J, Bowes O, Spencer F. Ophthalmology specialist trainee survey in the United Kingdom. Eye. 2018;33:917–24.
Bai H, Yao L, Wang H. Clinical investigation into posterior capsule rupture in phacoemulsification operations performed by surgery trainees. J Ophthalmol. 2020:1317249.
Ti SE, Yang YN, Lang SS, Chee SP. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity. Am J Ophthalmol. 2014;157:180–5.
Ting DS, Vrahimi M, Varma D, Steel DH, NETRiON. Trainee-led research networks in ophthalmology: is this the way forward? Eye. 2018;32:476–7.
Ting DS, Vrahimi M, Varma D, Steel DH, NETRiON. Research attitudes and perceived barriers to conducting research among ophthalmology trainees. Eye. 2018;32:653–5.
Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol. 2004;88:1242–6.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “Hand Motion” and “Counting Fingers” can be quantified with the freiburg visual acuity test. Investig Ophthalmol Vis Sci. 2006;47:1236–40.
Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34:502–8.
Kaplowitz K, Yazdanie M, Abazari A. A review of teaching methods and outcomes of resident phacoemulsification. Surv Ophthalmol. 2018;63:257–67.
Randleman JB, Wolfe JD, Woodward M, Lynn MJ, Cherwek DH, Srivastava SK. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125:1215–9.
Kim BZ, Patel DV, Sherwin T, McGhee CN. The Auckland Cataract Study: assessing preoperative risk stratification systems for phacoemulsification surgery in a teaching hospital. Am J Ophthalmol. 2016;171:145–50.
MacEwen C, Davis A, Chang L. Ophthalmology GIRFT programme national specialty report. 2019.
Nderitu P, Ursell P. Updated cataract surgery complexity stratification score for trainee ophthalmic surgeons. J Cataract Refract Surg. 2018;44:709–17.
Ting DS, Vaideanu-Collins D, Ellerton C. Cannula-associated ocular injuries during cataract surgery: the North East England Study. Eye. 2016;30:764–5.
Ting DS, Dees C, Ellerton C. Cannula-associated ocular injuries during cataract surgery: a preventable intraoperative complication? Middle East Afr J Ophthalmol. 2017;24:54–56.
Gregori NZ, Rodriguez M, Staropoli PC, Junk AK. Visual and anatomic outcomes of cataract surgery with intraoperative or postoperative complications in a teaching institution. Can J Ophthalmol. 2019;54:382–7.
Staropoli P, Gregori N, Junk A, Feuer W. Surgical simulation training reduces intraoperative cataract surgery complications among resident. Simul Healthc. 2018;13:11–15.
North East Trainee Research in Ophthalmology Network (NETRiON)
Tejaswi Bommireddy1,4,8, Mohammed Cheema1,4,8, Yanmei Chen1,4,8, Yunzi Chen1,4,8, Alan Cunningham1,4,8, Karim El-Assal1,4,8, Elizabeth Hill1,4,8, Rehab Ismail1,4,8, Jeffrey Hogg1,4,8, Lyudmila Kishikova1,4,8, David L. Lunt1,4,8, Haifa Madi1,4,8, Mark Markham1,4,8, Ibrahim Masri1,4,8, Esther Ting1,4,8, Maria Vrahimi1,4,8, Clara Wu1,4,8.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the North East Trainee Research in Ophthalmology Network (NETRiON) that have contributed to this study are listed below Summary.
Supplementary information
Rights and permissions
About this article
Cite this article
Grinton, M., Sandhu, J., Shwe-Tin, A. et al. Incidence, characteristics, outcomes and confidence in managing posterior capsular rupture during cataract surgery in the UK: an ophthalmology trainees’ perspective. Eye 35, 1213–1220 (2021). https://doi.org/10.1038/s41433-020-1057-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1057-z
This article is cited by
-
Experience and perception of cataract training within the national health service and independent sector in the UK: a regional trainee survey
Eye (2023)
-
Returning to cataract surgery after a hiatus: a UK survey report
Eye (2022)
-
Trainee research network (TRN): a potential global model for promoting research training and outputs among trainees
Eye (2022)