Abstract
Purpose
To report trends in cataract surgery indications, visual acuity outcomes, complication rates and reoperation rates at ten Aravind Eye Hospitals in Tamil Nadu, India.
Methods
In this retrospective database study we analyzed seven years of data of cataract surgeries at Aravind during January 1, 2012 to December 31, 2018. Our main outcome measures were preoperative and 1-month postoperative uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA); and rates of intraoperative complications and reoperations. We performed Cochran–Armitage trend tests.
Results
In 1.86 million eyes that underwent cataract surgery, the percentage of eyes undergoing phacoemulsification (PE) showed an increasing trend (p < 0.0001), from 26.8% in 2012 to 33.5% in 2018. The percentage of eyes undergoing manual small incision cataract surgery (SICS) showed a decreasing trend (p < 0.0001), from 70.0% in 2012 to 65.1% in 2018. For SICS, the percentages of eyes with good postoperative UCVA and BCVA showed increasing trends (p < 0.0001 for each), and the percentages of eyes with poor postoperative UCVA and BCVA showed decreasing trends (p < 0.0001 for each). Results for PE surgeries were mixed. For both PE and SICS rates of intraoperative complications showed a declining trend (p < 0.0001 for each) and a slight increasing trend for reoperations (PE p < 0.02; SICS p < 0.0001).
Conclusions
During this seven-year period there were noticeable trends in cataract surgeries performed at Aravind in terms of the mix of surgical procedures, preoperative vision, and cataract surgical outcomes.
Similar content being viewed by others
Introduction
Cataract surgery is a relatively safe and cost-effective intervention for cataract-induced blindness. However, significant concerns remain about quality of surgical outcomes, especially in developing countries [1]. For instance, a summary [2] of eight population-based studies in sub-Saharan Africa reports that the percentage of eyes with “good” vision, defined as postoperative visual acuity (VA) ≥ 6/18 by the World Health Organization (WHO) [3], ranged from 23 to 59%. The same summary also reports that the percentage of eyes that had “poor” vision (WHO definition is postoperative VA < 6/60) after surgery ranged from 23 to 64 percent. These statistics highlight the need for careful monitoring and reporting of the quality outcomes of cataract surgery.
The Aravind Eye Care System (Aravind) is a network of fourteen specialty eye-care hospitals in Southern India. In 2017–18, Aravind hospitals served almost 4.2 million outpatient visits, and performed 300,000 cataract surgeries (Activity Report 2017–18, www.aravind.org). Since its founding in 1976, Aravind has been serving over half of its patients at deeply subsidized prices or for free, in order to achieve its mission of eliminating needless blindness [4]. Aravind’s service design is inclusive, regardless of patients’ ability to pay; through its network of 75 primary eye care centers (Vision Centers) and over 2300 outreach eye camps conducted each year, it creates access for those who are unable to reach an eye hospital. This inclusive design ensures that the patients treated at Aravind Eye Hospitals are representative of its service population of almost 100 million.
The goal of this study is to describe trends in the patient profile, cataract surgery indications, visual acuity outcomes, complication rates and reoperation rates for surgeries performed at Aravind during the seven-year period 2012-18. To our knowledge, in the Indian context there are no population-based databases available that contain details of surgical quality. Since surgeries performed at Aravind hospitals account for over 40% of all cataract surgeries performed in the state of Tamil Nadu, and about 5% of all cataract surgeries performed in India in 2017-18 [5], the trends we identify in this study are potentially relevant to a larger population.
Methods
Database
Since 2005 Aravind has been using a proprietary software tool and database developed in-house -- Cataract Surgical Quality Assurance (CatQA) -- to track quality parameters, benchmark them between hospitals and surgeons, and to identify areas of concern. The current version has been in place at all Aravind hospitals since 2012. CatQA excludes pediatric cataract surgeries (patients aged ≤ 15 years). All relevant information about each surgery, including the surgical technique, preoperative and postoperative ocular findings, and complications is transferred from the surgical record into CatQA by the ophthalmic assistants in the operating rooms or outpatient clinics where pre and post-op examinations are carried out. All entries are checked and certified by a designated person for completeness. In recent years, with the introduction of Electronic Medical Records (EMR), the required data is automatically extracted from the EMR. Independent checks are conducted periodically to compare surgeries entered in medical records with the database. In the current study we use the data stored in CatQA.
Study participants
We use data on all cataract surgeries performed at ten Aravind hospitals from January 1, 2012 to December 31, 2018. These hospitals were operational for the full period; we excluded Aravind’s four newest hospitals because these became operational after 2014.
Ethical approval
The study protocol was approved by Aravind Eye Hospital’s Institutional Review Board, and adhered to the tenets of the Declaration of Helsinki. Patient confidentiality was maintained by adherence to privacy protocols.
Visual acuity outcomes
At Aravind, eyes of patients undergoing cataract surgery are examined preoperatively, and postoperatively 1 day and ~1 month after surgery. The preoperative examination includes baseline Snellen VA assessment, slit lamp examination, duct patency, intraocular pressure measurement, biometry, and systemic comorbidity evaluation. On the day following surgery, VA is assessed with pinhole using Snellen chart and the eye is examined by slit lamp. At the 1-month follow-up visit, all patients undergo VA testing and subjective refraction. In addition, all patients except those seen in the field in outreach sites undergo slit lamp and dilated fundus examination. We consider uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) in the operated eye measured approximately 1-month after surgery as the primary measures of visual outcomes. Since there could be large changes in refractive power in the weeks immediately following surgery due to wound healing and resolution of corneal edema [6, 7], visual acuity at follow-up instead of 1 day after surgery was considered a better measure of surgical outcomes. In this study we treat visual acuity as a dichotomous variable, based on the World Health Organization’s classification of good postoperative acuity as ≥ 6/18 and poor postoperative acuity as <6/60 [3].
Adverse surgical events
We considered intraoperative complications and reoperations as the measures of adverse surgical events. Complications are graded on a 0–3 scale using the Oxford Cataract Treatment and Evaluation Team (OCTET) scoring system in CatQA [8]. Only complications of OCTET grades 2 & 3 (i.e., greater severity) were included in the analysis. Where multiple complications were present, the most serious complication was considered; if all complications had the same complication score, then the first occurring complication was considered. A patient who returned to the operating room for a corrective procedure within 49 days of the primary procedure was considered a reoperation and is included in CatQA.
Statistical analyses
We performed analyses of patient-level data with the goal of describing trends in relevant variables. To test for trend in the binomial proportions of a categorical variable over the seven years, we applied the Cochran–Armitage trend test [9] to the annual data. For categorical variables with more than two levels (e.g., surgeons are of four types: Medical Officers, Fellows, Residents, and Visiting Trainees), the trend in each level was tested relative to the other levels combined. For continuous dependent variables, trend was determined based on a simple regression on the calendar year (coded as 1, 2, …, 7) as the predictor. All reported p-values are 2-sided. Analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). We caution readers that the very large sample sizes in our data (over 1.86 million eyes) imply that even small differences are likely to lead to small p-values in tests of statistical significance.
Results
Sample description
Descriptive statistics of the sample of 1,863,145 operated eyes for each of the seven years are shown in Table 1. The number of cataract surgeries performed increased over the seven-year period (p < 0.0001), from about 240,000 to about 300,000 each year. There was no trend in terms of patient sex, and the average age increased very slightly (p = 0.01).
Patients getting surgery at Aravind come through three streams: (1) “walk-in paying” patients who pay local market rates, which are the rates charged by ophthalmologists in private practice; (2) “walk-in free” patients who pay a steeply subsidized rate (US$13) for all preoperative work-up, SICS including intraoperative lens (IOL), postoperative medications and care; and (3) “free eye camp” patients admitted through outreach screening, for whom all services including return transportation, food and stay are free. The percentages of walk-in paying and walk-in free patients increased (p < 0.0001), while the percentage of free eye camp patients decreased (p < 0.0001) during this period.
In terms of surgeons who performed the surgeries, medical officers and fellows accounted for an increasing share (p < 0.0001), while residents accounted for a decreasing share (p < 0.0001). To understand these trends better, we also looked at trends in the numbers of each type of surgeon (Fig. 1). The numbers of each of the four types of surgeons who were at Aravind for part or whole of the year increased between 2012 and 2018 but at different rates, with the total number of surgeons increasing from 576 to 793, a compound annual growth rate of 5.5%. As a consequence of this rapid growth in number of surgeons, as well as sharp increase in the volume of sub-specialty work performed by surgeons, the number of cataract surgeries per surgeon per year declined from 417 to 376, a compound annual rate of decline of 1.7%.
There was an increasing trend in the share of PE surgeries, relative to SICS, extracapsular extraction (ECCE), and others (p < 0.0001). Nevertheless, SICS continued to account for over two-thirds of all surgeries on average.
The percentage of eyes with better preoperative vision (UCVA ≥ 6/18) was on average 25.7% for PE and only 9.8% for SICS. However, these percentages showed an increasing trend over the seven years for SICS (p < 0.0001) and a declining trend for PE (p < 0.0001). Conversely, the percentage of eyes with poorer preoperative vision (UCVA < 6/60) was 59.9% for SICS and only 32.9% for PE. These percentages showed a declining trend for SICS (p < 0.0001) and an increasing trend for PE (p < 0.0001). Finally, the percentage of surgeries that were followed up by the patient at about four weeks remained high at 87%, and increased slightly over this period (p < 0.0001).
Visual acuity outcomes
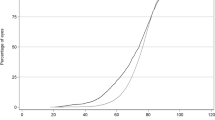
In Fig. 2 we show the percentage of eyes that achieved good vision (≥6/18) 1-month postoperatively in each of the seven years, separately for PE and SICS. Consistent with past findings [10], we see that the outcomes of PE were better than the outcomes of SICS on UCVA, but the differences between PE and SICS on BCVA were small. For SICS we find that the percentage of eyes with good UCVA outcomes increased sharply from 65.8% in 2012 to 84.9% in 2018 (p < 0.0001 for trend), and the percentage with good BCVA outcomes increased from 94.4% to 95.9% (p < 0.0001 for trend). For PE we find a slightly increasing trend for good UCVA outcomes (p < 0.0001) but a slightly decreasing trend for good BCVA outcomes (p < 0.0001).
In Fig. 3 we show the percentage of eyes that had poor vision (<6/60) 1-month postoperatively in each year. For SICS we find a decreasing trend in terms of both UCVA and BCVA (p < 0.0001 for both). By contrast, for PE we find a statistically significant increasing trend in both (p < 0.0001 for both), although there is no obvious trend in these metrics in Fig. 3. We find that the percentages of eyes with poor outcomes are very similar for SICS and PE in the most recent years, based on both UCVA and BCVA.
Complications and reoperations
In Fig. 4 we show the rates of intraoperative complications and reoperations for PE and for SICS for each year. For PE we find that the rate of intraoperative complications fell from 1.3% in 2012 to 0.7% in 2018, a decreasing trend (p < 0.0001). However, the annual rate of reoperations at around 0.5% (about 400 eyes) showed an increasing trend (p < 0.0001) although there is no discernible trend in the graph. The rate of intraoperative complications for SICS decreased from 1.6% in 2012 to 1.3% in 2018 (p < 0.0001 for trend). However, the annual rate of reoperations which was around 0.8% (about 1400 eyes), statistically showed an increasing trend (p < 0.0001) but such a trend is very slight and thus not apparent by visual inspection of the graph.
Discussion
Our analysis of over 1.86 million cataract surgeries performed at Aravind reveals important trends in patient composition and the quality of surgical outcomes. The number of cataract surgeries at Aravind grew at a compound annual growth rate of 3.7% during the period 2012–18. This is in part due to the opening of four new hospitals between 2010 and 2012. The two primary forms of surgery grew at very different rates; PE, which accounts for about a third of all surgeries, displayed a compound annual growth rate of 7.7%, while SICS, which accounts for almost two-thirds of all surgeries, grew at only 2.4% per annum. This is in the context wherein most people pay out of pocket for healthcare. Considering the higher cost of PE relative to SICS [11], this large difference in growth rates may reflect in part increasing affluence and healthcare expenditures in the Indian economy.
At Aravind, PE surgeries are offered as an option essentially to patients who come to the “paying” section. 20% of the paying patients were operated using SICS mostly due to the advanced nature of the cataract, and a smaller number of paying patients preferred SICS as it is much cheaper than a PE surgery with a foldable IOL. Paying patients who undergo SICS are only 8% of all cataract surgeries. Patients who are admitted through the “walk-in free” section or “free eye camps” get only SICS by design. The increasing proportion of PE surgeries from 26.8% in 2012 to 33.5% in 2018 (Table 1) is essentially attributable to increasing paying capacity and insurance coverage. This change in willingness and ability to pay is supported by the evidence of the proportion of overall paying cataract surgeries increasing from 34.6% in 2012 to 39.6% in 2018 (Table 1).
Notably, the cost of cataract surgery to the patient at Aravind remained roughly the same during this period. For patients admitted through free eye camps, cataract surgery continued to be totally free. For walk-in free patients, the fee earlier was Rs. 750 (US$ 11.50) but patients had to purchase postoperative drugs. To improve compliance to postoperative medications, the fee was raised to Rs. 850 (US$ 13) with the cost of medicines bundled into the fee. For paying patients the fees for SICS and entry-level PE surgery essentially remained unchanged. However, as more premium IOLs were introduced, they were priced to reflect the market.
Table 1 shows that females constituted about 55% of patients who underwent cataract surgery at Aravind, versus 45% male, and that these percentages remained largely unchanged during this seven-year period. Previous studies have found that the prevalence of unoperated cataract was higher in women than in men in South India [12], and that females had a 56% higher risk of blindness (presenting vision < 6/60 in the better eye) than men [13]. The larger percentage of women being operated on at Aravind we now report suggests that the higher prevalence of female blindness reported in previous studies may not be entirely due to lower access to treatment, but may also be due to greater exposure to risk factors such as biomass cooking fuels [14].
The mean age of operated patients showed an imperceptibly small increasing trend (p = 0.01). Interestingly, the mean age in our data at 60.4 years is considerably lower than the mean ages reported in Lundstrom et al. [15] for Malaysia (64.6 years) and Sweden (74.6 years) for the period 2008 to 2012. Reasons for inter-country differences could include differences in the mean age of the population, age-related cataract onset, or the cataract surgical rates (CSR). For instance, the prevalence of unoperated cataract in people aged ≥60 years in India has been reported [12] to be higher than similar populations in the US [16].
We found that the mix of operated patients shifted over time in favor of “walk-in paying” and “walk-in free” patients, relative to “free eye camp” patients. We believe this trend is due to a number of factors. First, increasing awareness about available treatments for cataract leads to “free eye camp” patients coming to Aravind hospitals for second-eye surgery on their own. Another factor is rising incomes and standards of living in India. A third factor is the opening of Aravind eye hospitals in four new locations between 2010 and 2012, and referrals from Aravind’s growing networks of primary eye care centers and other providers [17].
An important trend that is evident in these data is better preoperative vision before surgery (Table 1) in the case of SICS. A similar temporal pattern for all cataract surgeries has been reported in multiple studies in countries such as the Netherlands, Sweden and Malaysia [15], England [18], Australia [19], Sweden [20], and the United States [21]. Lower visual thresholds for surgery are often accompanied with increased cataract surgery rates [22]. Relatedly, we found that the proportion of patients with preoperative vision <6/60 who underwent SICS declined in our data (Table 1). A higher proportion of VA < 6/60 before cataract surgery has been reported to be strongly associated with low development at the country level, and inversely associated with the national CSR [23]. This trend in preoperative vision we have identified bears closer examination in the Indian context since it has critical implications for the demand and supply of cataract surgery. In the case of PE patients, the opposite trend was found: the percentage of PE patients with good preoperative vision decreased, and the percentage of patients with poor preoperative vision increased. Although statistically significant, these trends are relatively weak; nevertheless, they are noteworthy and should be monitored.
The rate of patient follow-up at four weeks at Aravind after surgery is high (87%) and increasing over time (Table 1). This should be viewed in the context of recent evidence which shows that there are large changes in visual acuity between discharge and follow-up, and that a substantial fraction of eyes can benefit from refraction at follow-up, especially for SICS [6, 24]. Such a high follow-up rate allows us to use visual acuity at follow-up as a measure of surgical quality with greater confidence, without fear of biased measurement.
In terms of postoperative visual acuity, for SICS all our metrics indicate improvements over this seven-year period: the percentage of eyes with good outcomes showed an increasing trend, and the percentage of eyes with poor outcomes showed a decreasing trend. Notably, the growth in the percentage of good outcomes in terms of UCVA in SICS was dramatic, from 65.8% to 84.9% (Fig. 2). This improvement in UCVA followed conscious and sustained efforts to strengthen refractive and visual outcomes with the SICS technique. This highlights the importance of having a system for rigorous monitoring and reviewing of the data with appropriate benchmarks and trends. Through CatQA, the surgery monitoring software, individual surgeons had access to their outcomes, including the ability to benchmark against their colleagues. More procedures were performed through temporal incisions in order to negate the pre-existing astigmatism in the horizontal meridian (against the rule astigmatism), which was most common in this age group. Moreover, care was taken to accurately perform refraction and to document vision by using standard illuminated vision charts at all follow-up outreach camps.
By contrast, the news for PE was mixed. Although the percentage of eyes with good UCVA outcomes increased, the percentage of eyes with good BCVA outcomes decreased, and the percentage of eyes with poor UCVA and BCVA outcomes increased. Possible reasons for these trends include an increase in the percentage of patients with systemic comorbidities, an increasing trend in the percentage of patients with poor preoperative vision (UCVA < 6/60, Table 1), and an increase in the percentage of patients with advanced cataracts. We should also note that in each of the seven years the percentage of good BCVA outcomes is higher than 97.1% (Fig. 2), and the percentage of poor outcomes is lower than 1.4% (Fig. 3). This implies that the measures may be subject to ceiling and floor effects respectively, making it difficult to see systematic increases and decreases.
We also show in Fig. 2 the WHO’s target thresholds for good outcomes of at least 80% in terms of “available correction” and 90% for “best correction” [3]. While both UCVA and BCVA for PE, and BCVA for SICS, easily crossed the target thresholds in all years, UCVA outcomes for SICS have crossed the target threshold of 80% only in the last three years in our data. We also show in Fig. 3 the WHO’s target threshold of no more than 5% for poor outcomes for both available correction and best correction [3], and note that outcomes at Aravind for both PE and SICS comfortably met this target in each year in our data.
In terms of adverse surgical events, the overall rates of intraoperative complications for PE and SICS were comparably low, as also found in a previous study [25]. The most commonly occurring intraoperative complications in both types of surgical techniques were posterior capsule rupture and vitreous loss (details are shown in Supplementary Table S1). Further, we found that there were declines in the rates of intraoperative complications for both SICS and PE (Fig. 4). Efforts such as regular weekly reviews with the surgical team, standardized and hands-on training schedules, and improved instrumentation and machines, probably contributed to reduction in complication rates.
For both techniques, the rates of reoperations were low (they ranged from 0.8% to 1.0% for SICS, and from 0.4% to 0.6% for PE), but showed statistically significant increasing trends (Fig. 4). A more in-depth examination of types of reoperations (details are not shown for reasons of space) revealed that the most commonly performed reoperations were residual cortex aspiration, IOL repositioning, and anterior chamber formation with suturing, and these remained the same during this 7-year period.
A key strength of this study is the use of standardized data collection and recording procedures across the ten hospitals and seven years. Further, the availability of large samples leads to more precise estimates, and our use of multiple outcome measures enables us to offer more complete picture of surgical quality and when patients seek surgery. A limitation of this study relative to population-based studies is the reliance on data from a single provider.
Summary
What was known before
-
Data on multi-year trends in cataract surgical outcomes in India have so far not been published.
What this study adds
-
Data on trends in surgical outcomes of 1.86 million cataract surgeries over the period 2012–18 in India.
-
Phacoemulsification has been growing in use relative to small incision cataract surgery (SICS).
-
Visual acuity outcomes for SICS have been improving.
-
Rates of intraoperative complications in both phacoemulsification and SICS have been decreasing.
References
Lindfield R, Vishwanath K, Ngounou F, Khanna RC. The challenges in improving outcome of cataract surgery in low and middle income countries. Indian J Ophthalmol. 2012;60:464–9.
Lewallen S, Thulasiraj RD. Eliminating cataract blindness - how do we apply lessons from Asia to sub-Saharan Africa? Glob Public Health. 2010;5:639–48.
World Health Organization. Informal consultation on analysis of blindness prevention outcomes. 1998. http://apps.who.int/iris/handle/10665/67843. Accessed 5 June, 2017.
Le H-G, Ehrlich JR, Venkatesh R, Srinivasan A, Kolli A, Haripriya A, et al. A sustainable model for delivering high-quality, efficient cataract surgery In Southern India. Health Aff Proj Hope. 2016;35:1783–90.
Anon. National Programme for Control of Blindness, Ministry of Health & Family Welfare, Government of India. http://npcb.nic.in/index1.asp?linkid=93&langid=1. Accessed 11 March, 2019.
Gupta S, Ravindran RD, Subburaman G-BB, Vardhan A, Ravilla T. Evidence on importance of follow-up visits after cataract surgery. Ophthalmology. 2018;26:910–2.
Limburg H, Foster A, Gilbert C, Johnson GJ, Kyndt M, Myatt M. Routine monitoring of visual outcome of cataract surgery. Part 2: Results from eight study centres. Br J Ophthalmol. 2005;89:50–52.
OCTET Team. Use of a grading system in the evaluation of complications in a randomised controlled trial on cataract surgery. Oxford Cataract Treatment and Evaluation Team (OCTET). Br J Ophthalmol. 1986;70:411–4.
Agresti A. Categorical data analysis. 2nd ed. New York: Wiley-Interscience; 2002. https://doi.org/10.1002/0471249688.
Rengaraj V, Ma SS, Chang DF. Manual small-incision cataract surgery. In: Henderson BA, ed. Manual small incision cataract surgery. Cham: Springer International Publishing; 2016. p. 1–15. http://link.springer.com/10.1007/978-3-319-24666-6_1. Accessed 20 Dec, 2018.
Gogate P, Deshpande M, Nirmalan PK. Why do phacoemulsification? Manual small-incision cataract surgery is almost as effective, but less expensive. Ophthalmology. 2007;114:965–8.
Vashist P, Talwar B, Gogoi M, Maraini G, Camparini M, Ravindran RD, et al. Prevalence of cataract in an older population in India. Ophthalmology. 2011;118:e2.
John N, Rachel J, Praveen V, Murthy GVS. Rapid Assessment of Avoidable Blindness in India. PLoS ONE 2008;3. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2478719/. Accessed April 11, 2019.
Ravilla TD, Gupta S, Ravindran RD, Vashist P, Krishnan T, Maraini G, et al. Use of cooking fuels and cataract in a population-based study: the India eye disease study. Environ Health Perspect. 2016;124:1857–62.
Lundström M, Goh P-P, Henry Y, Salowi MA, Barry P, Manning S, et al. The changing pattern of cataract surgery indications: a 5-year study of 2 cataract surgery databases. Ophthalmology. 2015;122:31–38.
Eye Diseases Prevalence Research Group. Prevalence of cataract and pseudophakia/aphakia among adults in theUnited States. Arch Ophthalmol. 2004;122:487–94.
Misra V, Vashist P, Malhotra S, Gupta SK. Models for primary eye care services in India. Indian J Community Med Publ Indian Assoc Prev Soc Med. 2015;40:79–84.
Keenan T, Rosen P, Yeates D, Goldacre M. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol. 2007;91:901–4.
Taylor HR, Vu HTV, Keeffe JE. Visual acuity thresholds for cataract surgery and the changing Australian population. Arch Ophthalmol Chic Ill 1960 2006;124:1750–3.
Behndig A, Montan P, Stenevi U, Kugelberg M, Lundstrom M. One million cataract surgeries: Swedish National Cataract Register 1992-2009. J Cataract Refract Surg. 2011;37:1539–45.
Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39:1383–9.
Erie JC. Rising cataract surgery rates: demand and supply. Ophthalmology. 2014;121:2–4.
Shah SP, Gilbert CE, Razavi H, Turner EL, Lindfield RJ. Preoperative visual acuity among cataract surgery patients and countries’ state of development: a global study. World Health Organ Bull World Health Organ Geneva. 2011;89:749–56.
Gupta S, Ravindran RD, Subburaman G-BB, Vardhan A, Ravilla T. Predictors of patient compliance with follow-up visits after cataract surgery. J Cataract Refract Surg. 2019;45:1105–12.
Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phacoemulsification and manual small-incision cataract surgery at Aravind Eye Hospital. J Cataract Refract Surg. 2012;38:1360–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ravindran, R.D., Gupta, S., Haripriya, A. et al. Seven-year trends in cataract surgery indications and quality of outcomes at Aravind Eye Hospitals, India. Eye 35, 1895–1903 (2021). https://doi.org/10.1038/s41433-020-0954-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0954-5