Abstract
Background/objectives
Standard sub-Tenon’s block (STB) involves incision (dissection) of conjunctiva and Tenon’s capsule with the help of blunt scissors and forceps, insertion of a blunt sub-Tenon’s cannula under the Tenon’s capsule and injection of local anaesthetic agent. STB is frequently associated with minor complications such as chemosis and postoperative subconjunctival haemorrhage but rare sight and life-threatening complications. To reduce these minor complications, several variations of incisionless STB have been described however, there are no comparative data. One such incisionless STB involves the use of lacrimal dilator which is easily available in the operating theatre. We compared incisionless lacrimal dilator-facilitated with the standard STB for effectiveness, chemosis, and postoperative subconjunctival haemorrhage.
Subjects/methods
After obtaining ethical approval, patients scheduled to undergo elective phacoemulsification cataract surgery were enroled to receive incisionless lacrimal dilator-facilitated STB (Group LD) or a standard STB using Wescott scissors and blunt forceps (Group WS). All patients received 3 mL 2% lidocaine without any adjuvant. No sedation was administered. Demographics of the patients, duration of the procedure, analgesia, akinesia, duration of the procedure intraoperative chemosis, and postoperative subconjunctival haemorrhage were compared.
Results
Both groups were comparable for demographic data, duration of the procedure, analgesia, and akinesia (p > 0.05). The severity of chemosis and postoperative subconjunctival haemorrhage were significantly lower in Group LD (n = 32) in comparison to Group WS (n = 31) (p < 0.001).
Conclusions
Incisionless lacrimal dilator-facilitated STB decreases intraoperative chemosis and postoperative conjunctival haemorrhage in comparison to standard STB. Analgesia and akinesia are comparable in both techniques.
Similar content being viewed by others
Introduction
A standard sub-Tenon’s block (STB) involves dissection (incision) of conjunctival and Tenon’s capsule with the help of blunt scissors and forceps, insertion of blunt sub-Tenon’s cannula followed by injection of a local anaesthetic agent under the Tenon’s capsule [1, 2]. Although STB is a versatile technique but it is only popular in some countries despite its comparative reduced risks of sight and life-threatening complications associated with popular needle-based blocks [3]. The exact usage of STB for ophthalmic surgery is unknown and difficult to ascertain due to the lack of scientific data. According to the published national surveys of STB usage for cataract surgery, it was popular in Canada [4] (67%), Japan [5] (63%), New Zealand [6] (86%), and United Kingdom [7] (72%) and infrequently used in Singapore [8] (7%) as well as USA [9] (5%).
Unfortunately, STB is frequently associated with varying degrees of akinesia, chemosis, and postoperative conjunctival haemorrhage [10, 11]. The requirement of akinesia for popular and increasingly sophisticated phacoemulsification cataract surgery is questionable but many ophthalmic surgeons dislike chemosis and postoperative subconjunctival haemorrhage. Chemosis is the swelling of conjunctiva and its incidence is reported to vary between 5.6% [12] and 100% [13]. Chemosis is reported to interfere during surgery in 1 in 1600 cases [12,13,14]. Postoperative subconjunctival haemorrhage usually occurs due to tearing or severing of blood vessels during the dissection and injection. The incidence of postoperative subconjunctival haemorrhage varies widely ranging between 4.3% [11] and 100% [13].
Several authors have described incisionless STB to decrease the incidence of chemosis and postoperative subconjunctival haemorrhage. Allman et al. [15] introduced a special tri-port disposable cannula making the technique costlier. Kumar and Seet [16] described an incisionless STB with a reusable metal sterilisable cannula making it affordable for poorer countries. Palte and Gayer [17] described a superomedial incisionless STB in porcine eyes with the help of recently introduced plastic disposable conjunctival probe as an auxiliary tool in lieu of scissors to avoid surgical incision, minimize local trauma, and improve surgical field but at the increased cost of the technique. We are not aware of any published study of the use of conjunctival probe in humans. Chua et al. [18] described another incisionless STB with a lacrimal dilator (also known as punctal lacrimal dilator, punctum dilator) which is easily available in the operating theatre which can be resterilized. A lacrimal dilator is used instead of Wescott scissors to create a small aperture in the conjunctiva and Tenon’s capsule and a blunt sub-Tenon’s cannula is inserted just like a standard STB. Unfortunately, all the published incisionless techniques are descriptive as authors preferred methods and there is no comparative data.
We conducted a randomized, prospective, and non-inferiority comparative study to confirm that lacrimal dilator-facilitated incisionless STB would be noninferior to that of a standard STB. We included demographic of the patients, duration of the procedure, analgesia (pain), akinesia, duration of the procedure intraoperative chemosis, and postoperative subconjunctival haemorrhage.
Materials and methods
The study was approved by the Baskent University Institutional Review Board and Ethics Committee, Ankara, Turkey (Project no: KA19/165) and supported by a small grant by Baskent University Research Fund. The study was also registered to ClinicalTrials.gov with the identifier number of NCT04345172. We obtained written informed consent from all patients scheduled to undergo routine phacoemulsification cataract surgery. Exclusion criteria included allergy to lidocaine, history of previous retinal and strabismus surgery, bleeding disorders and oral anticoagulant use, the presence of glaucoma or high IOP, thick pterygia, any pathological condition that conjunctiva, and Tenon’s capsule cannot be lifted away from the sclera. The patients who refused STB and who required general anaesthesia were also excluded from the study. The patients were randomly allocated to receive STB performed with a lacrimal dilator (Group LD) and with Wescott scissors (Group WS). The sample size was calculated according to the results of a pilot study of ten patients in each group where no chemosis were 30% and 20% in Group DL and Group WS, respectively. Based on these assumptions, the sample size was estimated to be 32 per group with a power of 80% and α = 0.05 (http://www.stat.uiowa.edu/~rlenth/Power) considering the total number of patients undergoing cataract surgery in 1 year at the setting. A total of 64 patients were included in the study after obtaining written informed consent. Randomization was ensured by sealed envelopes prepared according to a computer-generated table and the envelopes were opened by the operator just before the STB.
Study protocol
Tetracaine eye drops 1% were installed into the conjunctiva followed by povidone (iodine) 5% aqueous drops to the conjunctival sac for 3 min [19]. A wired eyelid speculum was inserted to separate eyelids.
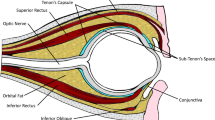
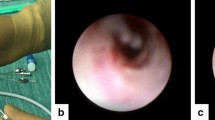
In group LD, the conjunctiva and Tenon’s capsule were lifted together tightly with a blunt forceps like a tent in the inferonasal quadrant and a lacrimal dilatator (Castroviejo Lacrimal Dilatator, Katena Products, Inc, Denville, NJ, USA) was placed tangential to the globe creating a round and small hole at 5 mm away from the limbus (Fig. 1). A disposable sub-Tenon metal cannula, 19G, 2.54-cm long, curved with a blunt flat tip (Visitec, Beaver-Visitec International Ltd, Warwickshire, UK) was used for the delivery of the local anaesthetic agent.
In Group WS, after lifting the conjunctiva and Tenon’s capsule together with a blunt forceps an incision was performed with a blunt tip Westcott scissors in the inferonasal quadrant 5 mm away from the limbus to expose sub-Tenon’s space. The local anaesthetic agent was delivered with help of a disposable sub-Tenon metal cannula, 19G, 2.54-cm long, curved with a blunt flat tip.
All patients received 3 mL of 2% lidocaine without any adjuvant. No sedative was administered. STB and surgery were performed by the same investigator but the blocks were evaluated by an investigator who was blinded to the technique used. All patients were discharged on the day of surgery and were checked on the 1st postoperative day.
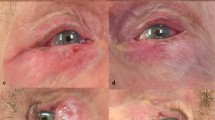
The parameters recorded included demographic of the patients, duration of the procedure, analgesia, akinesia, duration of the procedure intraoperative chemosis, and postoperative subconjunctival haemorrhage. Analgesia was evaluated using a numeric rating scale for pain (0–10; 0—no pain, 10—the worst imaginable pain) immediately after the operation. Akinesia (ocular movements) was checked in all 4-primary gazes, 10 min after STB. Intraoperative chemosis and postoperative conjunctival haemorrhage (1st postoperative day) were assessed in the quadrant or quadrants affected (superior nasal, superior temporal, inferior nasal, inferior temporal) using a 5-point scale (0–4; 0—no for chemosis and haemorrhage, 4 for chemosis or haemorrhage in all 4 quadrants).
Statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA). The primary outcome parameter of this study included chemosis in patients undergoing cataract surgery with STB. Categorical data were analyzed by χ2 test and expressed in numbers and percentages. Numerical variables were expressed as a mean and standard deviation and as a median and minimum–maximum, when necessary. Statistical tests included independent samples t-test for between-group comparisons and Mann–Whitney U test where the number and distribution of data required non-parametric tests. A p value of <0.05 was considered significant.
Results
Sixty-four patients were enroled in the study. One patient in Group WS was excluded from the final analysis due to breach of the study protocol (Group LD; n = 32, Group WS; n = 31).
The patients in both groups were comparable with regards to demographic data and the duration of the procedure (p > 0.05) (Table 1). Analgesia scores were comparable between groups (Group LD vs. Group WS; 0.7 ± 0.9 vs. 1.0 ± 1.0 respectively, >0.05). Akinesia scores were also comparable between groups (Fig. 2).
The severity of chemosis and postoperative conjunctival haemorrhage were significantly lower in Group LD in comparison to Group WS (p < 0.001) (Figs. 3 and 4, respectively).
There was no anaesthetic and surgical complication or cancellation occurred due to the techniques used.
Discussion
This study reports that lacrimal dilator-facilitated incisionless STB is associated with less chemosis and postoperative subconjunctival haemorrhage in comparison to standard STB while ensuring comparable analgesia and akinesia.
STB is considered a safer and effective regional ophthalmic technique for routine ophthalmic procedures compared to needle-based blocks [20, 21]. The incidence of life and sight-threatening complications is very rare [22]. It is also been reported to provide better intraoperative analgesia (anaesthesia) in comparison to both topical anaesthesia as well as needle-based blocks for cataract surgery [23].
A national guideline on “Cataract in Adults: Management” published by the UK National Institute for Health and Care Excellence in 2017 states that STB should be offered to patients having cataract surgery [24]. That may be the reason why STB is the most frequently used block for cataract surgery in UK [25]. However, the practice varies in the world. For example, STB has been less frequently performed in US, potentially due to reluctance for scissors use and long-established needle block tradition among anaesthesiologists and non-anaesthesiologist practitioners [17]. We believe that lacrimal dilatator-facilitated STB may encourage anaesthesiologists who hesitate to surgically incise conjunctiva and thus increase the use of STB.
A standard STB involves injection of a local anaesthetic agent through a blunt cannula after dissection and opening “a small buttonhole” into the conjunctiva and Tenon’s capsule with blunt Wescott scissors, while grasping the conjunctiva with a small forceps [23]. This small buttonhole like aperture is sometimes uneven leading to spread and/or leakage of local anaesthetic in or out of the intended space even in the experienced hands affecting onset and development of akinesia. More importantly, inadequate dissection and unintentional tissue injury during the dissection result in chemosis and subconjunctival haemorrhage. Both complications, although presumed as minor may appear unsightly at the surgical site thus making some surgeons dislike for STB and postoperative patients’ satisfaction may also be compromised.
Chemosis is due to local anaesthetic flow anteriorly along the rectus muscles between the sheaths and the conjunctiva/sclera as well as posteriorly in the episcleral space near the optic nerve from behind the globe [26]. An animal report with this technique in four ex-vivo porcine eyes showed the circumferential spread of dye solution inside Tenon’s capsule with extension to the posterior of the globe with this technique as well as the creation of a smaller aperture and less local anaesthetic reflux [27]. In our study, chemosis was less frequently observed with lacrimal dilator-facilitated STB. This may be due to the more standardized introduction to the sub-Tenon’s space with the dilator and a smaller and even hole formation in comparison to the one created by a Wescott scissors. This resulted in less reflux of local anaesthetic enabling satisfactory anaesthesia, less chemosis and less subconjunctival haemorrhage which all contribute to optimal surgical conditions.
The described novel technique is minimal invasive incisionless lacrimal dilatator-facilitated STB and there is no need to use Wescott or other scissors for dissection. This dilator enables the avoidance of scissors which, technically, has a higher potential of globe damage during STB [28]. A round hole suitable for the cannula insertion is made with the lacrimal dilator. Lacrimal dilator pierces the conjunctiva more smoothly in comparison to scissors. The dilator is available in the ophthalmic operating theatre, made of metal and can be easily sterilised and reused. Although sub-Tenon’s cannula has been used for incisionless STB without making a hole [15, 16, 29], the dilator-facilitated insertion of a cannula into the sub-Tenon’s space requires less pressure. The described incisionless technique reduces the overall cost of STB and can be affordable in poorer countries. To our knowledge, our study is the first randomized and comparative study evaluating the efficacy of an incisionless STB.
The study has a few limitations. This is a one-centre study that may be subject to reproduction misinterpretation in different clinical settings. Since the conduct of this study, the technique has been adapted and followed by the remaining ophthalmic anaesthesia providers in our institution.
In conclusion, incisionless lacrimal dilator-facilitated STB not only decreases intraoperative chemosis and postoperative conjunctival haemorrhage in comparison to a standard STB but also provides comparable analgesia and akinesia. We believe that this technique has the potential to increase adopt of STB practice in countries where this block is not popular and may even decrease sight and life-threatening complications related to needle-based blocks.
Summary
What was known before
-
Standard sub-Tenon’s block (STB) involves incision of conjunctiva and Tenon’s capsule with the help of blunt scissors.
-
STB is frequently associated with chemosis and postoperative subconjunctival haemorrhage but rare sight and life-threatening complications.
What this study adds
-
STB can be performed with a lacrimal dilator without scissors.
-
Incisionless lacrimal dilator-facilitated STB decreases chemosis and conjunctival haemorrhage while ensuring comparable analgesia and akinesia as standard technique.
References
Greenbaum S. Parabulbar anesthesia. Am J Ophthalmol. 1992;114:776.
Stevens JD. Curved, sub-Tenon cannula for local anesthesia. Ophthalmic Surg. 1993;24:121–2.
Kumar CM, Eid H, Dodds C. Sub-Tenon’s anaesthesia: complications and their prevention. Eye. 2011;25:694–703.
Ong-Tone L. Practice patterns of Canadian ophthalmological society members in cataract surgery: 2017 survey. Can J Ophthalmol. 2018;53:1.
Oshika T, Amano S, Araie M, Majima Y, Leaming DV. Current trends in cataract and refractive surgery in Japan: 1999 survey. Jpn J Ophthalmol. 2001;45:383–7.
Pick ZS, Leaming DV, Elder MJ. The fourth New Zealand cataract and refractive surgery survey: 2007. Clin Exp Ophthalmol. 2008;36:604–19.
El-Hindy N, Johnston RL, Jaycock P, Eke T, Braga AJ, Tole DM, et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: anaesthetic techniques and complications. Eye. 2009;23:50–55.
Tam YS, Kumar CM, Au Eong KG, Yip CC, Cheng J. Trends in cataract surgery technique and anaesthesia preferences in Singapore: a 2016 survey. Ann Acad Med Singap. 2018;47:390–3.
Leaming DV. Practice styles and preferences of ASCRS members—2003 Survey. J Cataract Refract Surg. 2004;30:892–900.
Kumar CM, Dowd TC. Complications of ophthalmic regional blocks: their treatment and prevention. Ophthalmologica. 2006;220:73–82.
Lerch D, Venter JA, James AM, Pelouskova M, Collins BM, Schallhorn SC. Outcomes and adverse events of sub-tenon’s anesthesia with the use of a flexible cannula in 35,850 refractive lens exchange/cataract procedures. Clin Ophthalmol. 2020;14:307–15.
Guise PA. Sub-Tenon anesthesia: a prospective study of 6000 blocks. Anesthesiology. 2003;98:964–8.
Kumar CM, Dodds C. Evaluation of the Greenbaum sub-Tenon’s block. Br J Anaesth. 2001;87:631–3.
Roman SJ, Chong Sit DA, Boureau CM, Auclin FX, Ullern MM. Sub-Tenon’s anaesthesia: an efficient and safe technique. Br J Ophthalmol. 1997;81:673–6.
Allman KG, Theron AD, Byles DB. A new technique of incisionless minimally invasive sub-Tenon’s anaesthesia. Anaesthesia. 2008;63:782–3.
Kumar CM, Seet E. Effective and cost-saving incisionless sub-Tenon’s block. Indian J Anaesth. 2017;61:84–85.
Palte HD, Gayer S. Novel technique for minimally invasive sub-Tenon’s anesthesia. Reg Anesth Pain Med. 2019;44:131–2.
Chua A, Chua MJ, Kumar CM. Punctal dilator facilitates insertion of blunt cannula during sub-Tenon’s block. Anaesth Intensive Care. 2018;46:239–40.
Kumar CM, Dodds C. Sub-Tenon’s anesthesia. Ophthalmol Clin North Am. 2006;19:209–19.
Jaichandran VV. Ophthalmic regional anaesthesia: a review and update. Indian J Anaesth. 2013;57:7–13.
Villafranca Barba A, Mouslim S, De la Gala García FA, Reyes Fierro A. Sub-tenon block for ocular globe anesthesia: a review. Rev Esp Anestesiol Reanim. 2011;58:167–73.
Gayer S, Kumar CM. Ophthalmic regional anesthesia techniques. Minerva Anestesiol. 2008;74:23–33.
Guay J, Sales K. Sub-Tenon’s anaesthesia versus topical anaesthesia for cataract surgery. Cochrane database Syst Rev. 2015;8:CD006291.
Anon. NICE Cataract Guideline Committee. Cataracts in adults: management (NG77). London, UK: National Institute for Health and Care Excellence; 2017.
Eke T, Kumar CM. Preventing adverse events in cataract surgery: sub-Tenon’s block. Anesth Analg. 2018;127:e68–e69.
Palte HD, Gayer S. Chemosis secondary to anterograde episcleral (sub-tenon) spread of local anesthetic during retrobulbar eye block. Anesthesiology. 2014;121:877.
Palte HD. Ophthalmic regional blocks: management, challenges, and solutions. Local Reg Anesth. 2015;8:57–70.
Rüschen H, Bremner FD, Carr C. Complications after sub-Tenon’s eye block. Anesth Analg. 2003;96:273–7.
Lin S, Ling RH, Allman KG. Real-time visualisation of anaesthetic fluid localisation following incisionless sub-Tenon block. Eye. 2014;28:497–8.
Funding
This study was supported and funded by Baskent University Research Fund, Turkey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Coban-Karatas, M., Cok, O.Y. & Kumar, C.M. Lacrimal dilator-facilitated incisionless vs. standard sub-Tenon’s block: a randomized, prospective and non-inferiority comparative study. Eye 35, 1961–1966 (2021). https://doi.org/10.1038/s41433-020-01207-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01207-0