Abstract
Individuals with severe combined immunodeficiency (SCID), a group of rare, genetic conditions, are at risk for life-threatening illnesses unless diagnosed and treated early. Even after early identification through newborn screening, parents of children with SCID embark on a complex journey marked by a variety of informational and emotional support needs. This paper explored the types of uncertainties experienced by parents of a child with SCID diagnosed through newborn screening. We conducted semi-structured interviews with 26 parents to discuss the types of uncertainty experienced, including scientific, practical, personal, and existential. Each interview was recorded, transcribed, and coded. Using deductive and inductive content analysis, we describe the type of uncertainty experienced across each stage of the SCID journey. We found that uncertainties in the SCID journey were chronic and multifaceted. Some uncertainties were more prominent at certain points of the journey whereas others spanned multiple stages. Parents expressed a variety of negative emotional reactions to uncertainty, from anxiety, worry, and fear, to doubt, guilt, or grief, and even anger, frustration, and depression. The results speak to the need for healthcare providers to prepare parents for the SCID journey by providing resources to help manage and cope with uncertainty.
Similar content being viewed by others
Introduction
Severe combined immunodeficiency (SCID) is a group of rare, genetic conditions characterized by a decreased amount or absence of T-cells, which results in a lack of a functioning immune system [1, 2]. Individuals with SCID are at risk for life-threating illness unless diagnosed and treated early, typically with a hematopoietic stem cell transplant or, with some variants, gene therapy [3, 4]. Given that SCID is considered a medical emergency and treatments have been shown to significantly reduce morbidity and mortality, all states now screen newborns at birth for the condition. Newborn screening has improved the clinical prognosis for children with SCID, with 92% of infants surviving after treatment [5].
Parents of children with a rare disorder often experience a diagnostic odyssey which is marked by high levels of stress and uncertainty [6, 7]. Although newborn screening alleviates the search for a diagnosis, it is not unusual for parents to experience increased anxiety and uncertainty as they wait on confirmatory testing results [8]. Even after a diagnosis is received, parents of children with rare disorders live with other uncertainties related to the long-term outcomes for their child and the impact on their family [9,10,11]. Similarly, parents of children with SCID embark on a complex journey marked by a variety of informational and emotional support needs [12]. This journey begins with a positive newborn screen for SCID and a confirmed diagnosis, and continues through the pre-treatment stage, which includes deciding on the most appropriate treatment option and possibly undergoing pretreatment conditioning (i.e., chemotherapy and/or immunosuppressants). Next is a waiting period to determine treatment response in the post-treatment stage, and finally returning home in the new normal stage where families adjust to living with SCID.
Uncertainty in healthcare and the management of diseases has been well described [13,14,15,16]. One framework, developed by Han and colleagues, categorizes uncertainty along three main dimensions: source, issue, and locus [17]. Source refers to the root causes of uncertainty, which consist of three main features of available information about a phenomenon: probability, ambiguity, and complexity. Issue refers to the substantive topic of uncertainty, which can be scientific (pertaining to the diagnosis, prognosis, causes, or treatment of health problems), practical (pertaining to the structures and processes of healthcare and the actions needed to manage health problems), and personal (pertaining to psychosocial, moral, and existential aspects of health problems). Locus refers to the person(s) in whose mind uncertainty resides. This conceptual framework previously has been applied to categorize the range of uncertainties experienced by patients dealing with various health conditions [18, 19]. We selected this framework as it encompassed the broad range of uncertainties experienced by parents of young children with a rare disease, whereas other frameworks focused specifically on the patient’s uncertainties.
The purpose of this qualitative study was to apply Han’s uncertainty framework to understand the different types of uncertainty experienced by parents of children with SCID diagnosed through newborn screening– from the time of initial diagnosis, through treatment, and into the new normal. We describe the various issues—scientific, practical, and personal—that represented the focus of parents’ uncertainties. We also include parents’ responses to these uncertainties. Elsewhere, we describe how parents coped with these uncertainties [20]. Understanding the range of uncertainties that arise at different points of this journey is a critical task in meeting the needs of parents of children with this rare genetic disorder.
Materials and methods
Participants
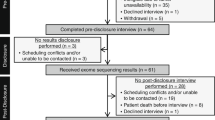
We recruited parents through two patient advocacy organizations: the Immune Deficiency Foundation and SCID, Angels for Life Foundation. A notification about the study was posted on each groups’ private Facebook page. Parents who expressed interest were emailed to determine eligibility. Parents were eligible if they were 18 years or older, spoke English, lived in the United States, and had a child with SCID or a SCID-like condition (e.g., DiGeorge syndrome) that was diagnosed through newborn screening. In total, 26 parents participated. On average, parents were 35.1 years of age, mostly mothers, and the majority had a child <6 years of age (see Table 1). Collectively, parents were in a variety of stages of the SCID journey, but most were in the New Normal stage with children one to 9 years out from treatment.
Measures and data collection
We conducted qualitative interviews using a semi-structured interview guide to explore different types of uncertainties experienced by parents. The interviews were used to further explore findings from a survey in which parents of children with SCID indicated needing support to understand what to expect over their child’s lifespan and how to manage uncertainty [12]. The guide asked broad questions about uncertainty at different stages of the SCID journey. Interviewers probed about specific uncertainty issues, if needed. For example, parents were asked if they experienced any uncertainties related to their child’s treatment if the topic had not been discussed. Interviews lasted about 60 min. The interviewer took extensive notes using a structured template which helped to organize uncertainty by journey stage. Each interview was audio recorded and then transcribed using a cloud service. As a thank you for their time, participants were offered $100.
Data analysis
We used a combination of deductive content analysis, which was informed by Han’s taxonomy, and inductive content analysis to describe parents’ responses to uncertainty. The research team, consisting of coders (OK and EM), interviewers (SA and AG), and senior researchers with expertise in newborn screening (MR) and health behavior (BBB), developed an initial list of uncertainty codes. These codes were organized into four main types of uncertainty: Scientific, Practical, Personal, and Existential. In the original taxonomy, existential uncertainty was a subcategory of personal uncertainty. Here, we created a separate category for this type of uncertainty as it was a central and a frequently cited issue to parents of children with SCID. Subcodes were assigned to each type of uncertainty based on the taxonomy (e.g., prognostic uncertainty was a subcode for Scientific uncertainty). Additional codes included emotional responses to uncertainty which emerged from the data. We used the timepoints of the SCID journey (Diagnostic, Pre-treatment, Treatment/ Post-treatment, New Normal) to describe the progression of uncertainty.
To ensure the codebook was appropriately capturing the interview data, the first six transcripts were double-coded. Any codes that were unclear were discussed and refined [21]. To establish interrater reliability, two additional transcripts were double-coded. Cohen’s kappa for the first 8 transcripts (30%) was 0.78, which indicated substantial agreement between the coders [22]. The remaining 18 transcripts were divided between the two coders. To ensure coders maintained high interrater reliability, 3 of these were double coded at intervals throughout the independent coding. Coding and analysis of all data were conducted in NVivo 12.
Results
Results are organized around the issues of uncertainty experienced by parents, with a description of how they emerged or changed throughout the SCID journey. An overview of the frequency of each uncertainty issue was mentioned at each stage of the journey is presented in Fig. 1. Parental perceptions of and responses to uncertainty are also reported. Table 2 provides illustrative quotes from participants by type of uncertainty experienced or response to uncertainty at each stage of the journey.
Scientific uncertainty
Scientific uncertainties were very commonly experienced in all stages of the SCID journey, especially early on (see Fig. 1). The dominant subtype of scientific uncertainty was diagnostic in nature. In particular, there was uncertainty regarding the validity of the newborn screening result. Several parents noted that their child’s pediatrician told them not to worry or that their internet searches indicated that SCID screening has a high false positive rate. Another manifestation of diagnostic uncertainty was a lack of understanding about SCID symptoms. Many parents reported that their child appeared to be healthy and were surprised by the news of the screening results. A common next step was for parents to search the internet, despite being advised not to, which was not as useful as they had hoped (see Table 2, Quote 1.1).
A second subtype of scientific uncertainty experienced by parents in the Diagnostic stage was causal uncertainty regarding the genetic pathways that led to SCID. Many parents didn’t know that SCID could be inherited and were unsure if the mother was a carrier or if the diagnosis resulted from a de novo mutation. This was especially true of parents who already had healthy children or those who didn’t have extended family members with SCID. As a result, parents reported having to wait on cascade testing. Although the genetic test result of the mother often did not affect the treatment path for the child, it raised uncertainty as parents thought about the future and possible implications for reproductive planning.
Therapeutic uncertainty was abundant in the Pre-treatment stage. Although many parents stated they felt like an active partner in making the choice, some struggled with uncertainty about treatment decisions. For parents who decided on a hematopoietic stem cell transplant for their child, therapeutic uncertainty revolved around finding a donor match. For example, parents expressed uncertainty about who could be an eligible donor, how close a match was best for their child, or whether/when a suitable non-related donor would be identified. Given that outcomes are best when a transplant occurs by 3 months of age, some parents faced a difficult choice about whether to proceed with the transplant using a less well-matched donor versus waiting for a full match. Another type of therapeutic uncertainty was whether the child should undergo pre-treatment immunosuppressants or chemotherapy and, if so, the appropriate dosage for their child (see Table 2, Quote 1.2).
Later in the SCID journey, therapeutic uncertainty was closely followed by prognostic uncertainty. In the Treatment and Post-treatment stage, most parents reported that the treatment procedure was uneventful. However, uncertainties about the success of the treatment were at the forefront of almost all these parents’ minds. Common uncertainties were about whether and when their child’s T- and B-cell counts would rise. If counts did not increase as quickly as expected, or if there was fluctuation in the counts, parents were uncertain whether that meant the treatment was unsuccessful (see Table 2, Quote 1.3). In a few cases when it was clear that the transplant did not work, parents were uncertain about next steps. Another example of prognostic uncertainty was whether the child would experience any complications from the treatment, such as graft versus host disease, or have secondary problems because of the treatment (e.g., anemia). In the New Normal stage, many wondered, “Will the transplant last?” Parents stated they felt like they “couldn’t let their guard down.” This uncertainty included unknowns related to whether the child would need immunoglobulin therapy to boost their B cell counts or the possibility of another transplant or other treatment plan if the child’s T cell counts began to trend downwards.
Practical uncertainty
Practical uncertainties occurred throughout the SCID journey but were mentioned most frequently in the Pre-treatment and New Normal stages (see Fig. 1). One of the main practical uncertainties was financial. In the Diagnostic stage, parents expressed uncertainty about the short- and long-term impact on jobs and careers, including the ability to take extended time off or whether the diagnosis would affect career advancement. Some also mentioned the immediate financial costs experienced during this stage (e.g., extra medical bills). For example, one parent was offered fast turnaround genetic testing for their child to help determine appropriate next steps, but they expressed uncertainty about whether they could afford it. Financial uncertainty continued into the Pre-Treatment stage, with several parents indicating concern about whether their insurance policy would cover the cost of transplants, infusions, or other costly procedures. In addition, many talked about the expenses related to receiving treatment away from home (e.g., housing, food, parking) and extended time off work. As a result, parents described uncertainty around finding support from government or non-profit organizations and whether they would qualify for it. Financial uncertainties were reiterated during the New Normal stage as parents expressed uncertainty about whether the child will reach lifetime caps on their insurance coverage.
Other types of practical uncertainty were logistic. During the Diagnostic stage, parents were unsure where to go for a confirmatory test. In the Pre-treatment stage, logistical uncertainties centered on household management and the caring of other children. Parents who were isolating at home prior to treatment began to worry about the cleanliness of the house and the uncertainty it caused (see Table 2, Quote 2.1). Some had to get rid of family pets or remove their houseplants. Other parents talked about the challenge of taking care of older siblings while trying to keep their child healthy, especially if older children were enrolled in childcare or school. This subtype of practical uncertainty persisted into the Post-treatment stage. When a child was released soon after a transplant, families experienced logistical uncertainty about maintaining the same safety protocols in their own homes, especially if they had other children. In the New Normal stage, some parents were uncertain about where they would access care if the treatment was done out of state or if the family or their child’s provider moved.
Personal uncertainty
Across all the stages, personal uncertainties were most frequent in the Pre-treatment and New Normal stages (see Fig. 1). Relational uncertainty was the most common subtype. Some parents experienced uncertainty about the impact of the SCID diagnosis on their relationships with friends and family. This was often expressed in the Diagnostic stage because of the child’s need for isolation prior to confirmatory testing, which meant that those outside the immediate family could not meet the baby or offer any sort of in-person support. Challenges were also experienced between parents. Often, one parent became the primary caregiver for the child with SCID, including taking the child to appointments, entering isolation in the hospital, or even making decisions about treatment. These challenges caused uncertainty within marital relationships about who would take on the role of the primary caregiver (see Table 2, Quote 3.1). Additionally, several mothers noted that they were told to stop breastfeeding until they were tested for CMV, which caused personal uncertainty about the ability to form strong interpersonal bonds with their newborn.
Parents expressed relational uncertainty about whether time away from their other children during the Treatment and Post-treatment stages would cause problems between the siblings later, such as feelings of resentment, or affect the bond between the parent and other children. For some, the inability to see extended family while in the hospital caused additional relational uncertainty. Further, many parents reported being physically separated from their spouse, with one parent in the hospital with child with SCID and the other at home and going to work, which caused added strain and relational uncertainty. Others talked about differences in how they and their spouses handled Treatment and Post-treatment uncertainties (See Table 2, Quote 3.2).
In the New Normal stage, as parents returned home and tried to adapt to living with SCID, many stated that their relationships with friends had changed. Parents said they were not able to spend as much time with friends as they used to because they were worried about getting their child sick or that they didn’t connect with friends in the same way (see Table 2, Quote 3.3). Some parents experienced uncertainty about having their extended family visit due to possible exposure to germs. Within the immediate family, relational uncertainty centered on the parent’s relationship with their child with SCID, other children in the household, and their spouse. Parents talked about the challenge of getting their other children to understand the seriousness of needing to maintain a clean house or strict hygiene procedures. They also spoke about how being in isolation had a negative impact on their other children. Finally, parents discussed the toll uncertainties took on their relationship with their spouse. Although it was rare, there were examples of parents divorcing during this stage due to ongoing relational strain.
Existential uncertainty
Existential uncertainties were mentioned early in the SCID journey, but most frequently in the New Normal stage. During the Diagnostic stage, several parents wondered how much SCID would come to define their child’s or family’s life. Many expressed uncertainty about their child’s survival and how SCID would affect the child and family (see Table 2, Quote 4.1). In the Pre-treatment stage, parents continued to focus on the uncertainty surrounding their child’s survival. Some also talked about whether their child would have a normal life and how SCID would affect them into adulthood. Existential uncertainty lingered into the Treatment and Post-treatment stages, although it was mentioned less frequently. Some parents expressed uncertainty about whether they made the right treatment choices for their child and the uncertainty of how their child would react years later to the decisions they were making now. In the New Normal stage, parents expressed uncertainty about whether their child’s development would be similar to children who do not have SCID. There was enduring uncertainty about the long-term survival or the possibility of developing subsequent complications or conditions (see Table 2, Quote 4.2). Examples of these uncertainties included whether the child would develop cancer or experience infertility as a result of pre-treatment conditioning. Finally, many parents talked about the existential uncertainty of their child’s health and well-being because of the COVID-19 global pandemic, which forced them back into isolation. Parents said it brought up old uncertainties or exacerbated existing uncertainties about their child’s survival.
Reactions to uncertainty
Parents reported a variety of emotional reactions to uncertainty during the Diagnostic stage. Almost all parents expressed anxiety, worry, and fear about the severity of SCID. Some reported feelings of doubt related to the truth of the screening results. Others expressed confusion about the implications of a SCID diagnosis. Some mentioned feeling guilty about the possibility that they passed the gene variant on to their child. A common theme among parents was feeling overwhelmed by the possible diagnosis and what was to come (see Table 2, Quote 5.1).
In the Pre-Treatment stage, parents still felt overwhelmed about having to make treatment decisions, balance the needs of their family, friends, or jobs with how to care for their child with SCID. Others expressed anger and frustration about the demands of their jobs or the complexities of applying for insurance or other forms of financial support. Anxiety, fear, and worry was also prevalent during this stage as parents thought about the road ahead for their child and family. A few parents also talked about how they experienced sadness or even depressive symptoms at this stage of the journey.
In the Treatment and Post-treatment stages, the predominant reaction to uncertainty was anxiety and worry as parents waited to see if their child’s cell counts would increase after treatment. They also expressed worry about the possible complications, and some parents expressed guilt about being in the hospital and not home with their other children. Many parents were mentally and physically drained from constant stress. One parent expressed that the long waiting period in the hospital led to feelings of detachment (see Table 2, Quote 5.2).
In the New Normal stage, parents expressed lingering fear and worry about their child’s health and well-being. Despite the success of treatments, parents reported feeling nervous about setbacks. Many acknowledged that they expected to have to live with constant apprehension for the rest of their lives (see Table 2, Quote 5.3). Notably, some parents said that during this stage, they were finally able to focus on themselves and reflect on their own anxiety, depression, and mental health.
Discussion
Summary of findings
This paper aids in the understanding of the uncertainties experienced by parents who have a child with a condition identified through newborn screening. Despite receiving a diagnosis early in their child’s life, parents of a child with SCID had many uncertainties about the journey ahead. Our findings echo those of others who have examined uncertainty for conditions identified prenatally or through newborn screening. Parents of children with a prenatal diagnosis of congenital heart disease expressed short-term uncertainty related to immediate next steps after the diagnosis as well as longer term uncertainty related to prognosis for their child [23]. Uncertainty also was experienced by parents of children who screen positive for cystic fibrosis, but have an inconclusive diagnosis [24]. Parents of children with the later-onset form of Pompe disease who were identified through newborn screening had a diagnosis but their children became “patients in waiting” as they experienced uncertainty related to when symptoms would emerge and treatment would be needed [25]. For those with children who had the infantile-onset form, uncertainties typically focused on their child’s current health as well as those related to caring for other children, the logistics of medical appointments, and balancing job responsibilities. These findings suggest that making a presymptomatic diagnosis through newborn screening does not alleviate uncertainty for parents as might be expected based on the diagnostic odyssey literature. Rather, parents with these oftentimes rare disorders continue to have uncertainty related to treatment choices and outcomes as well as what to expect over the course of a child’s life.
A key finding of our study was that parents of children with SCID experienced changing yet chronic uncertainties across the journey. Some uncertainties were more prominent at certain points of the journey whereas others spanned multiple stages. In particular, we found that scientific uncertainty, especially diagnostic and therapeutic, was most prevalent early in the SCID journey, with prognostic uncertainty emerging in the Post-treatment phase. Personal and practical uncertainties centered on logistical, financial, and relational issues in the Pre-treatment and New Normal stages. Existential uncertainty was frequently reported early on but resurfaced in the New Normal stage and may persist throughout the child’s life. Patterns of uncertainty over time have also been found in other studies. In patients who were waiting for sequencing results for cancer, experiences of uncertainty changed over time [26]. Similarly, parents of children with other chronic conditions described uncertainty as evolving as they adapted to the diagnosis, its impact on daily life, and, for some, the cyclical nature of the condition [10, 27, 28]. These results highlight the importance of supporting parents of children with SCID throughout their journey in order to help them cope with the uncertainties they experience [20].
Parents in this study expressed a variety of negative emotional reactions to uncertainty, from anxiety, worry, and fear, to doubt, guilt, or grief, and even anger, frustration, and depression. These results highlight the need for healthcare providers to communicate with parents about the possible uncertainties ahead and help them to cope with uncertainty. The management of uncertainty and reactions to it for parents of children with rare genetic conditions such as SCID is complex process that ends in adaptation and acceptance [29]. Studies have found there are different factors that can help with managing uncertainty. In particular, hope, optimism, and psychosocial support are related to coping efficacy and overall adaptation [9, 30,31,32]. In addition, the provision of information by healthcare providers can help with managing uncertainty [7, 33, 34].
Limitations
We acknowledge there are some limitations to our study that should be taken into consideration when interpreting the results. First, we used a convenience sample of English-speaking parents, predominantly mothers, who had a child with SCID diagnosed through newborn screening who were recruited through patient advocacy groups. Although efforts were made to include a diverse array of participants, the findings from our interviews may not generalize to all parents of a child with SCID. Similarly, parents were from a variety of locations and may have had different treatment options which may have affected their experiences with uncertainties. Finally, we used a semi-structured interview that asked parents about overall types of uncertainties experienced (e.g., personal) but did not ask parents to describe different subtypes of uncertainties (e.g., relational). Thus, there may have been uncertainties that parents experienced but did not discuss.
Conclusion
The goal of this paper was to understand the types of uncertainties experience by parents of a child with SCID diagnosed through newborn screening. We found that uncertainties in the SCID journey were chronic and multifaceted. The results speak to the importance of preparing parents for the SCID journey by communicating about and helping parents to cope with uncertainty. Healthcare providers, including genetic counselors, immunologists, and transplanters, play a critical role in working with parents and providing informational and emotional support. External resources as well as intrinsic coping skills will aid parents on the road ahead and promote positive adaptation.
Data availability
Deidentified data from this study are available through a data use agreement from the corresponding author on request.
References
Buckley RH. Molecular defects in human severe combined immunodeficiency and approaches to immune reconstitution. Annu Rev Immunol. 2004;22:625–55.
Cirillo E, Giardino G, Gallo V, D’Assante R, Grasso F, Romano R, et al. Severe combined immunodeficiency—an update. Ann N Y Acad Sci. 2015;1356:90–106.
Buckley RH, Schiff SE, Schiff RI, Markert ML, Williams LW, Roberts JL, et al. Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. N. Engl J Med. 1999;340:508–16.
Cavazzana-Calvo M, Lagresle C, Hacein-Bey-Abina S, Fischer A. Gene therapy for severe combined immunodeficiency. Annu Rev Med. 2005;56:585–602.
Kwan A, Abraham RS, Currier R, Brower A, Andruszewski K, Abbott JK, et al. Newborn screening for severe combined immunodeficiency in 11 screening programs in the United States. JAMA. 2014;312:729–38.
Carmichael N, Tsipis J, Windmueller G, Mandel L, Estrella E. “Is it going to hurt?”: The impact of the diagnostic odyssey on children and their families. J Genet Couns. 2015;24:325–35.
Grier J, Hirano M, Karaa A, Shepard E, Thompson JL. Diagnostic odyssey of patients with mitochondrial disease: results of a survey. Neurol Genet. 2018;4:e230.
Dillard JA, Carson CL. Uncertainty management following a positive newborn screening for cystic fibrosis. J Health Commun. 2005;10:57–76.
Bell M, Biesecker BB, Bodurtha J, Peay HL. Uncertainty, hope, and coping efficacy among mothers of children with Duchenne/Becker muscular dystrophy. Clin Genet. 2019;95:677–83.
Hinton D, Kirk S. Living with uncertainty and hope: a qualitative study exploring parents’ experiences of living with childhood multiple sclerosis. Chronic Illn. 2017;13:88–99.
Kerr AM, Haas SM. Parental uncertainty in illness: managing uncertainty surrounding an” orphan” illness. J Pediatr Nurs. 2014;29:393–400.
Raspa M, Lynch M, Squiers L, Gwaltney A, Porter K, Peay H, et al. Information and emotional support needs of families whose infant was diagnosed with SCID through newborn screening. Front Immunol. 2020;11:885.
Babrow AS. Uncertainty, value, communication, and problematic integration. J Commun. 2001;51:553–73.
Brashers DE. Communication and uncertainty management. J Commun. 2001;51:477–97.
Mishel MH. The measurement of uncertainty in illness. Nurs Res. 1981;30:258–63.
Mishel MH. Uncertainty in illness. Image: J Nurs Scholarsh. 1988;20:225–32.
Han PK, Umstead KL, Bernhardt BA, Green RC, Joffe S, Koenig B, et al. A taxonomy of medical uncertainties in clinical genome sequencing. Genet Med. 2017;19:918–25.
Biesecker BB, Klein W, Lewis KL, Fisher TC, Wright MF, Biesecker LG, et al. How do research participants perceive “uncertainty” in genome sequencing? Genet Med. 2014;16:977–80.
Reyes KG, Clark C, Gerhart M, Newson AJ, Ormond KE. “I wish that there was more info”: characterizing the uncertainty experienced by carriers of pathogenic ATM and/or CHEK2 variants. Fam Cancer. 2022;21:143–55.
Kutsa O, Andrews SM, Mallonee E, Gwaltney A, Creamer A, Han PK, et al. Parental coping with uncertainties along the severe combined immunodeficiency journey. Orphanet J Rare Dis. 2022;17:390.
Hill CE, Knox S, Thompson BJ, Williams EN, Hess SA, Ladany N. Consensual qualitative research: an update. J Couns Psychol. 2005;52:196.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3.
Harris KW, Brelsford KM, Kavanaugh-McHugh A, Clayton EW. Uncertainty of prenatally diagnosed congenital heart disease: a qualitative study. JAMA Netw Open. 2020;3:e204082.
Barben J, Southern KW. Cystic fibrosis screen positive, inconclusive diagnosis. Curr Opin Pulm Med. 2016;22:617–22.
Pruniski B, Lisi E, Ali N. Newborn screening for Pompe disease: Impact on families. J Inherit Metab Dis. 2018;41:1189–203.
Bartley N, Napier CE, Butt Z, Schlub TE, Best MC, Biesecker BB, et al. Cancer patient experience of uncertainty while waiting for genome sequencing results. Front Psychol. 2021;12(Apr):647502.
Sparud-Lundin C, Berg S, Fasth A, Karlsson A, Wekell P. From uncertainty to gradually managing and awaiting recovery of a periodic condition-a qualitative study of parents experiences of PFAPA syndrome. BMC Pediatr. 2019;19:1–9.
Webster M. The cycle of uncertainty: parents’ experiences of childhood epilepsy. Sociol Health Illn. 2019;41:205–18.
Biesecker BB, Erby L. Adaptation to living with a genetic condition or risk: a mini‐review. Clin Genet. 2008;74:401–7.
Madeo AC, O’Brien KE, Bernhardt BA, Biesecker BB. Factors associated with perceived uncertainty among parents of children with undiagnosed medical conditions. Am J Med Genet Part A. 2012;158:1877–84.
Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Educ Couns. 2012;87:233–8.
Yanes T, Humphreys L, McInerney-Leo A, Biesecker B. Factors associated with parental adaptation to children with an undiagnosed medical condition. J Genet Couns. 2017;26:829–40.
Lipinski SE, Lipinski MJ, Biesecker LG, Biesecker BB. Uncertainty and perceived personal control among parents of children with rare chromosome conditions: the role of genetic counseling. Am J Med Genet Part C Semin Med Genet. 2006;142:232–40.
Zhong L, Woo J, Steinhardt MA, Vangelisti AL. “Our job is that whole gray zone in between there”: investigating genetic counselors’ strategies for managing and communicating uncertainty. Health Commun. 2020;35:1583–92.
Acknowledgements
We would like to extend our heartfelt thanks to the families who participated in this study. We are grateful for their time and input.
Funding
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $2.97 million with 0% financed with nongovernmental sources. The contents are those of the author(s)and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.
Author information
Authors and Affiliations
Contributions
MR, SMA, AYG, AC, and BBB were involved in study design and conceptualization. SMA and AYG collected the data. MR, OK, SMA, AYG, EM, and BBB analyzed and interpreted the data. MR, OK, SMA, AYG, EM, PKJH, and BBB were involved in writing and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was reviewed and approved by the RTI International Institutional Review Board. Participants provided informed consent prior to data collection.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Raspa, M., Kutsa, O., Andrews, S.M. et al. Uncertainties experienced by parents of children diagnosed with severe combined immunodeficiency through newborn screening. Eur J Hum Genet 32, 392–398 (2024). https://doi.org/10.1038/s41431-023-01345-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01345-5
This article is cited by
-
Artificial intelligence â the next generation of sequencing?
European Journal of Human Genetics (2024)
-
What is health and what do we mean when we say an intervention improves health?
European Journal of Human Genetics (2024)
-
Parental Engagement in Identifying Information Needs After Newborn Screening for Families of Infants with Suspected Athymia
Journal of Clinical Immunology (2024)