Abstract
Background/Objectives
Observational studies link elevated homocysteine concentrations (Hcy) with female fertility, pregnancy loss, and low offspring birthweight. Maternal rs1801133, a functional variant in MTHFR strongly associated with lifelong elevated Hcy, is associated with recurrent pregnancy loss and offspring birthweight in Asian women. We investigated if genetically elevated Hcy is associated with fertility, pregnancy loss, and offspring birthweight in European women.
Subjects/Methods
We performed a two-sample Mendelian randomization (MR) study using publicly available data. We obtained 18 genetic variants (five involved in Hcy metabolism) explaining up to 5.9% of the variance in Hcy from a genome-wide association meta-analysis of 44,147 European individuals (82% women). We investigated fertility (including age at menopause), pregnancy loss, and offspring birthweight in the UK Biobank (N = 194,174), EGG (N = 190,406), and ReproGen (N = 69,360–252,514) consortia using summary statistics. We calculated inverse-variance weighted, and several sensitivity MR regression statistics.
Results
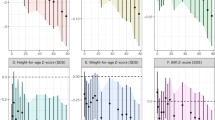
rs1801133 was associated with a 7.45 months (95% CI: 4.09, 10.80) increase in age at menopause and 29.69 (12.87, 46.51) g decrease in offspring birthweight per SD increase in Hcy in the UK biobank, and confirmed in EGG and ReproGen. MR for Hcy metabolism alone (five variants in MTHFR, MTR, CBS) showed similar results for offspring birthweight across consortia. However, using all 18 variants resulted in no association for any of the outcomes across consortia.
Conclusion
Hcy and suggestively vitamin B variants are most likely the drug targets for folate supplementation in pregnant women on the offspring birthweight, while Hcy variants related to renal function or diabetes are not involved.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Code availability
Strength of the genetic variants was calculated as F = β2exposure/SE2exposure. Two-sample MR analyses were performed by the freely available mrrobust Stata package [42].
References
Tallova J, Tomandl J, Bicikova M, Hill M. Changes of plasma total homocysteine levels during the menstrual cycle. Eur J Clin Invest. 1999;29:1041–4.
Hak AE, Polderman KH, Westendorp IC, Jakobs C, Hofman A, Witteman JC, et al. Increased plasma homocysteine after menopause. Atherosclerosis 2000;149:163–8.
Mascarenhas M, Habeebullah S, Sridhar MG. Revisiting the role of first trimester homocysteine as an index of maternal and fetal outcome. J Pregnancy. 2014;2014:123024.
Dodds L, Fell DB, Dooley KC, Armson BA, Allen AC, Nassar BA, et al. Effect of homocysteine concentration in early pregnancy on gestational hypertensive disorders and other pregnancy outcomes. Clin Chem. 2008;54:326–34.
Hogeveen M, Blom HJ, den Heijer M. Maternal homocysteine and small-for-gestational-age offspring: systematic review and meta-analysis. Am J Clin Nutr. 2012;95:130–6.
Bergen NE, Jaddoe VW, Timmermans S, Hofman A, Lindemans J, Russcher H, et al. Homocysteine and folate concentrations in early pregnancy and the risk of adverse pregnancy outcomes: the Generation R Study. BJOG 2012;119:739–51.
Kalhan SC. One carbon metabolism in pregnancy: Impact on maternal, fetal and neonatal health. Mol Cell Endocrinol. 2016;435:48–60.
Cueto HT, Riis AH, Hatch EE, Wise LA, Rothman KJ, Sorensen HT, et al. Folic acid supplement use and menstrual cycle characteristics: a cross-sectional study of Danish pregnancy planners. Ann Epidemiol. 2015;25:723–9 e1.
De-Regil LM, Pena-Rosas JP, Fernandez-Gaxiola AC, Rayco-Solon P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev. 2015:CD007950.
Lassi ZS, Salam RA, Haider BA, Bhutta ZA. Folic acid supplementation during pregnancy for maternal health and pregnancy outcomes. Cochrane Database Syst Rev. 2013:CD006896.
Wu X, Zhao L, Zhu H, He D, Tang W, Luo Y. Association between the MTHFR C677T polymorphism and recurrent pregnancy loss: a meta-analysis. Genet Test Mol Biomark. 2012;16:806–11.
Kamali M, Hantoushzadeh S, Borna S, Neamatzadeh H, Mazaheri M, Noori-Shadkam M, et al. Association between Thrombophilic Genes Polymorphisms and Recurrent Pregnancy Loss Susceptibility in the Iranian Population: a systematic review and meta-analysis. Iran Biomed J 2018;22:78–89.
Cao Y, Xu J, Zhang Z, Huang X, Zhang A, Wang J, et al. Association study between methylenetetrahydrofolate reductase polymorphisms and unexplained recurrent pregnancy loss: a meta-analysis. Gene 2013;514:105–11.
Yajnik CS, Chandak GR, Joglekar C, Katre P, Bhat DS, Singh SN, et al. Maternal homocysteine in pregnancy and offspring birthweight: epidemiological associations and Mendelian randomization analysis. Int J Epidemiol. 2014;43:1487–97.
Lee HA, Park EA, Cho SJ, Kim HS, Kim YJ, Lee H, et al. Mendelian randomization analysis of the effect of maternal homocysteine during pregnancy, as represented by maternal MTHFR C677T genotype, on birth weight. J Epidemiol. 2013;23:371–5.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–98.
Davey Smith G, Paternoster L, Relton C. When will Mendelian randomization become relevant for clinical practice and public health? Jama 2017;317:589–91.
Haycock PC, Burgess S, Wade KH, Bowden J, Relton C, Davey Smith G. Best (but oft-forgotten) practices: the design, analysis, and interpretation of Mendelian randomization studies. Am J Clin Nutr. 2016;103:965–78.
Holmes MV, Ala-Korpela M, Smith GD. Mendelian randomization in cardiometabolic disease: challenges in evaluating causality. Nat Rev Cardiol. 2017;14:577–90.
Benn M, Nordestgaard BG. From genome-wide association studies to Mendelian randomization: novel opportunities for understanding cardiovascular disease causality, pathogenesis, prevention, and treatment. Cardiovasc Res. 2018;114:1192–208.
Hartwig FP, Davies NM, Hemani G, Davey Smith G. Two-sample Mendelian randomization: avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int J Epidemiol. 2016;45:1717–26.
van Meurs JB, Pare G, Schwartz SM, Hazra A, Tanaka T, Vermeulen SH, et al. Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease. Am J Clin Nutr. 2013;98:668–76.
Borges MC, Hartwig FP, Oliveira IO, Horta BL. Is there a causal role for homocysteine concentration in blood pressure? A Mendelian randomization study. Am J Clin Nutr. 2016;103:39–49.
Larsson SC, Traylor M, Markus HS. Homocysteine and small vessel stroke: a mendelian randomization analysis. Ann Neurol. 2019;85:495–501.
Warrington NM, Beaumont RN, Horikoshi M, Day FR, Helgeland O, Laurin C, et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat Genet. 2019;51:804–14.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey, Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–63.
Greco MF, Minelli C, Sheehan NA, Thompson JR. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015;34:2926–40.
Bowden J, Davey, Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan NA, Thompson JR. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int J Epidemiol. 2016;45:1961–74.
Cerne JZ, Pohar-Perme M, Cerkovnik P, Gersak K, Novakovic S. Age at menarche and menopause is not associated with two common genetic variants in the methylenetetrahydrofolate reductase (MTHFR) gene. Eur J Contracept Reprod Health Care. 2011;16:241–7.
Liu P, Lu Y, Recker RR, Deng HW, Dvornyk V. Association analyses suggest multiple interaction effects of the methylenetetrahydrofolate reductase polymorphisms on timing of menarche and natural menopause in white women. Menopause 2010;17:185–90.
Chaudhry SH, Taljaard M, MacFarlane AJ, Gaudet LM, Smith GN, Rodger M, et al. The role of maternal homocysteine concentration in placenta-mediated complications: findings from the Ottawa and Kingston birth cohort. BMC Pregnancy Childbirth. 2019;19:75.
Timmermans S, Jaddoe VW, Hofman A, Steegers-Theunissen RP, Steegers EA. Periconception folic acid supplementation, fetal growth and the risks of low birth weight and preterm birth: the Generation R Study. Br J Nutr. 2009;102:777–85.
Li N, Li Z, Ye R, Liu J, Ren A. Impact of periconceptional folic acid supplementation on low birth weight and small-for-gestational-age infants in China: a large prospective cohort study. J Pediatr. 2017;187:105–10.
Wu H, Zhu P, Geng X, Liu Z, Cui L, Gao Z, et al. Genetic polymorphism of MTHFR C677T with preterm birth and low birth weight susceptibility: a meta-analysis. Arch Gynecol Obstet. 2017;295:1105–18.
O’Connor LJ, Price AL. Distinguishing genetic correlation from causation across 52 diseases and complex traits. Nat Genet. 2018;50:1728–34.
Kumar J, Ingelsson E, Lind L, Fall T. No evidence of a causal relationship between plasma homocysteine and type 2 Diabetes: a Mendelian randomization study. Front Cardiovascular Med. 2015;2:11.
Miao L, Deng G-X, Yin R-X, Nie R-J, Yang S, Wang Y, et al. No causal effects of plasma homocysteine levels on the risk of coronary heart disease or acute myocardial infarction: a Mendelian randomization study. Eur J of Prev Cardiol. 0:2047487319894679.
Xu T, Chen S, Yang F, Wang Y, Zhang K, Fu G, et al. The impact of homocysteine on the risk of coronary artery diseases in individuals with diabetes: a Mendelian randomization study. Acta Diabetol. 2021;58:301–7.
VanderWeele TJ, Tchetgen Tchetgen EJ, Cornelis M, Kraft P. Methodological challenges in mendelian randomization. Epidemiology 2014;25:427–35.
Lawlor D, Richmond R, Warrington N, McMahon G, Davey Smith G, Bowden J, et al. Using Mendelian randomization to determine causal effects of maternal pregnancy (intrauterine) exposures on offspring outcomes: sources of bias and methods for assessing them. Wellcome Open Res. 2017;2:11.
Spiller W, Davies NM, Palmer TM. Software application profile: mrrobust—a tool for performing two-sample summary Mendelian randomization analyses. Int J Epidemiol. 2018;48:684–90.
Acknowledgements
This study was based solely on publicly available summary statistics data from published literature (GWASs), the UK Biobank (provided by the Neale lab at: http://www.nealelab.is/uk-biobank/), EGG (Early Growth Genetics) Consortium using the UK Biobank Resource (downloaded at: www.egg-consortium.org) and ReproGen consortium (provided by ReproGen consortium at: https://www.reprogen.org/data_download.html). For this, the authors are deeply grateful to this open collaboration community.
Funding
ADK received financial support from Carl and Ellen Hertz’ foundation and Ellen Pedersen’s scholarship for traveling expenses during her stay as a visiting researcher at the Department of Laboratory Medicine, Boston Children’s Hospital, Boston, USA. YW received financial support from Hesheng Zhujiang foundation for traveling and living expenses during her stay as a visiting researcher at the Department of Laboratory Medicine, Boston Children’s Hospital, Boston, USA. ZW received funding from the National Natural Science Foundation of China (81771606). CE, MNK, and WM report no funding sources.
Author information
Authors and Affiliations
Contributions
Designed research: ADK, YW, CE. Conducted research: ADK, YW, MNK, CE. Provided essential materials: ADK, YW, MNK. Analyzed data and performed statistical analyses: ADK, CE. Wrote paper: ADK. Primary responsibility for final paper: ADK, CE. Supervision of YW for statistical coding and Mendelian randomization analyses: ADK, CE. Interpretation, critical revision, and final approval of the manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kjaergaard, A.D., Wu, Y., Ming, WK. et al. Homocysteine and female fertility, pregnancy loss and offspring birthweight: a two-sample Mendelian randomization study. Eur J Clin Nutr 76, 40–47 (2022). https://doi.org/10.1038/s41430-021-00898-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00898-2