Abstract
Hepatotoxicity is a frequent complication during maintenance therapy of acute lymphoblastic leukemia (ALL) with 6-mercaptopurine and methotrexate. Elevated levels of methylated 6-mercaptopurine metabolites (MeMP) are associated with hepatotoxicity. However, not all mechanisms are known that lead to liver failure in patients with ALL. Variants in the POLG gene, which encodes the catalytic subunit of mitochondrial DNA polymerase gamma (POLG1), have been related to drug-induced hepatotoxicity, for example, by sodium valproate. The association of common POLG variants with hepatotoxicity during maintenance therapy was studied in 34 patients with childhood ALL. Of the screened POLG variants, four different variants were detected in 12 patients. One patient developed severe hepatotoxicity without elevated MeMP levels and harbored a heterozygous POLG p.G517V variant, which was not found in the other patients.

Similar content being viewed by others
Introduction
Treatment-related hepatotoxicity, ranging from mild symptoms to severe veno-occlusive disease, is common in acute lymphoblastic leukemia (ALL) [1, 2]. Hepatotoxicity during maintenance is related to the oral maintenance therapy drugs 6-mercaptopurine (6-MP) and methotrexate (MTX) and is usually associated with increased methylated 6-mercaptopurine metabolite (MeMP) levels and the wild-type thiopurine methyltransferase (TPMT) genotype involved in 6-MP metabolism [3, 4]. Still, maintenance therapy–associated hepatotoxicity shows wide inter-individual variation and is suggested to be associated with other genetic risk factors, especially in patients who do not show elevated MeMP levels.
Human DNA polymerase gamma (Pol γ) replicates, maintains, and repairs mitochondrial DNA (mtDNA), and it is a heterotrimer formed by the catalytic domain POLG1, encoded by POLG at chromosomal locus 15q25, and two accessory subunits of POLG2 [5]. Drug-induced damage to the mitochondrial genome, either by direct impact on the DNA or by impaired Pol γ function, leads to aberrant mitochondrial protein synthesis and respiratory chain function, resulting in oxidative stress, altered mitochondrial membrane properties, and impaired metabolic functions [6]. In hepatocytes, this mitochondrial dysfunction contributes to cell death and triglyceride accumulation (i.e., steatosis) and, thus, drug-induced liver injury [7]. The association of Pol γ deficiency with liver dysfunction was first described in patients with Alpers’ disease [8]. Since then, several studies have demonstrated that patients with homozygous or compound heterozygous pathogenic variants on POLG1 (e.g., p.W748S and p.A467T) are at greater risk of liver failure induced by sodium valproate (VPA) [9, 10].
In this study, we investigated the association of chemotherapy-related hepatotoxicity during maintenance with common variants of the catalytic POLG1 domain of Pol γ in 34 patients diagnosed with childhood ALL.
Patients and methods
Patient cohort
Nine common POLG1 variants (p.T251I, p.A467T, p.N468D, p.G517V, p.P587L, p.R722H, p.W748S, p.E1143G, and p.Q1236H) were analyzed in 34 Finnish patients (18 boys and 16 girls; median age at diagnosis: 5 years [range: 2–15 years]) who were diagnosed consecutively between 2008 and 2013 in a tertiary level hospital. Exclusion criteria were Down syndrome, stem cell transplantation, or infant leukemia. All patients were treated according to the Nordic Society of Pediatric Hematology and Oncology (NOPHO) ALL2008 treatment protocol, 16 according to the standard risk (SR) protocol, 15 according to the intermediate risk (IR) protocol [1], and three according to the high risk (HR) protocol [11].
Medical records of the patients were reviewed for clinical signs of hepatotoxicity during maintenance therapy. The highest serum alanine aminotransferase (ALT) and bilirubin levels were defined after the start of maintenance therapy at week 20 in SR, week 22 in IR, and week 36 in the HR treatment protocol. The levels were assessed before or at least two weeks after the administration of high-dose MTX (HD-MTX). A transient increase in ALT levels with no clinical significance is common after HD-MTX in patients with childhood ALL [12], and ALT levels should return to normal levels within two weeks [13]. Three patients’ highest ALT levels were observed at 916 or 917 days after diagnosis (Table 1), which is more than two and a half years (912 days). For those patients, it was confirmed from the medical records that maintenance therapy was, unusually, still ongoing but coming to an end, and the ALT levels were analyzed as a part of the investigations at the end of treatment. Aspartate aminotransferase, alkaline phosphatase, and gamma–glutamyl transferase levels were not available for all patients because the levels are not routinely followed during treatment and therefore are not reported. The TPMT genotype was specified in the patient’s medical records. MeMP levels were determined from the ALL2008 maintenance metabolite study [14], and they are not routinely analyzed during therapy. Data for severe adverse events (SAE) were collected from the NOPHO database [15].
This study was approved by the Regional Ethics Committee of the Northern Ostrobothnia Hospital District, Finland, and it was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the patients or their legal guardians before their participation in the study.
DNA extraction
DNA was extracted, depending on its availability for each patient, from diagnostic bone marrow samples (for 8 patients), from both diagnostic bone marrow and remission blood samples (for one patient), and from either blood or bone marrow samples at remission (for 25 patients; Supplementary Table S1), using the Gentra Puregene Blood Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions.
PCR and restriction fragment length polymorphism
The DNA samples were amplified by PCR to screen the nine common POLG variants, namely, c.752C>T, c.1399G>A, c.1402A>G, c.1550G>T, c.1760C>T, c.2165G>A, c.2243G>C, c.3428A>G, and c.3708G>T (p.T251I, p.A467T, p.N468D, p.G517V, p.P587L, p.R722H, p.W748S, p.E1143G, and p.Q1236H, respectively). PCR was performed using AmpliTaq Gold® DNA Polymerase (Applied Biosystems, Foster City, CA, USA) and Biotools DNA Polymerase (5U/µl; Biotools B&M Labs S.A., Madrid, Spain). Restriction fragment length polymorphism (RFLP) was performed using FastDigest (Thermo Fisher Scientific, Waltham, MA, USA) and NEB enzymes (New England Biolabs, Ipswich, MA, USA) and following the manufacturers’ instructions. For the p.W748S variant, DNA samples were amplified by allele-specific PCR with locked nucleic acid (LNA) primers (Exiqon A/S, Vedbaek, Denmark, and Sigma-Aldrich, St.Louis, MO, USA). PCR products were visualized using 1.5% agarose gel (Standard Agarose—Type LE, BioNordika, Helsinki, Finland) and a Safe Imager™ Blue-Light Transilluminator (Invitrogen, Carlsbad, CA, USA). The digested RFLP products were visualized using 1.5% agarose gel (Standard Agarose—Type LE, BioNordika, Helsinki, Finland), 2–3% MetaPhor gel (Lonza Rockland Inc., Rockland, ME, USA), or 3% 3:1 HRB™ agarose gel (Amresco Inc., Solon, OH, USA), depending on the fragment size.
Expand long-template PCR and sequencing
The DNA samples were also amplified using long PCR (expand long-template PCR) to screen possible mtDNA deletions [16]. Whole mtDNA amplification was carried out using Phusion High-Fidelity DNA Polymerase (2 U/µl; Thermo Fisher Scientific), and PCR products were electrophoresed using 0.7% agarose gel (Standard Agarose—Type LE, BioNordika, Helsinki, Finland) at 70 V for 4.5 h. Sanger sequencing [17] was performed to confirm the presence of the p.A467T/p.N468D variant detected by RFLP in patient 2 (Table 1) and to cover the 23 coding exons and the exon–intron boundaries of the POLG gene in two patients showing signs of clinical liver dysfunction (patient 18 and patient 31; Table 1). PCR products were purified using exonuclease I and shrimp alkaline phosphatase [18], and sequencing analysis was run using an Applied Biosystems 3500xL Genetic Analyzer (Biocenter Oulu, Finland) with a Big-Dye Terminator v1.1 Cycle Sequencing Kit (Applied Biosystems). The POLG sequences were aligned with a reference sequence NG_008218.1 (available in the National Center for Biotechnology Information [NCBI] database) using the Sequencher 5.0 sequence analysis software demo (Gene Codes Corporation, Ann Arbor, MI, USA).
Results
Patients with severe hepatotoxicity during maintenance therapy
Three patients (3/34; 9%) showed grade 4 ALT levels (20 times above the upper normal limit) based on the Common Terminology Criteria for Adverse Events v5.0 (CTCAE) [19] with peaks at 856, 1145, and 2094 (U/l) (Table 1). No other SAE appeared to associate with the POLG1 variants (Table 1).
Patient with severe hepatotoxicity during maintenance therapy without elevated MeMP levels
A four-year-old female diagnosed with precursor B-cell ALL with a somatic t(12;21) translocation developed symptomatic hepatotoxicity with jaundice and increased central and peripheral periportal echogenicity as evidenced by liver ultrasound (US) findings and had a grade 4 ALT value. She harbored a heterozygous POLG c.1550G>T (p.G517V) variant (background population frequency: 0.0047; https://gnomad.broadinstitute.org/) [20]. She did not have excessively elevated MeMP levels (median during the episode: 2230 nmol/mmol Hgb), and she had a wild-type TPMT genotype. The patient was otherwise healthy. She was treated according to the NOPHO-ALL2008 SR protocol, and she is currently in remission.
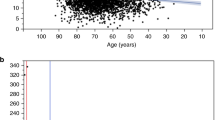
She developed hepatotoxicity at treatment week 82 during maintenance therapy after an increase in MTX and 6-MP doses to achieve the target leukocyte count (Fig. 1; Supplementary Table S2). Maintenance therapy was initiated at week 20 according to the SR protocol and consisted of daily doses of 6-MP (starting dose: 75 mg/m2) and weekly doses of MTX (starting dose: 20 mg/m2), which are set by the target leukocyte count and drug tolerance [1]. The patient reported nausea before elevation was detected in serum ALT levels, which peaked at 2094 U/l. The MeMP levels of the patient remained within the reference range (<20 000 nmol/mmol Hgb).
Hepatotoxicity occurred at treatment week 82, and the serum ALT levels peaked at 2094 U/l at week 86. MTX dose was increased from 14 mg/m2/w to 34 mg/m2/w before first cessation. At the same time 6-MP dose was gradually reduced from 43 mg/m2/d to 7 mg/m2/d, and then ceased. Both medications were recommenced at week 86, and the 6-MP dose was gradually increased to the pre-episode level (59 mg/m2/d) but MTX therapy was stopped completely because ALT levels started to rise again.
Liver US was performed at week 86, showing increased central and peripheral periportal echogenicity (Fig. 2A, B). A liver biopsy was not performed. Immunoglobulins, smooth muscle and antinuclear antibodies, and viral tests, including cytomegalovirus, Epstein–Barr virus, and hepatitis viruses, were all analyzed as normal. All medications, including sulfadiazine/trimethoprim, were discontinued. The patient’s ALT levels decreased after the cessation of chemotherapy. Liver US performed in week 90 showed a decrease in the periportal echogenicity but an increase in the parenchymal echogenicity of the liver compared with that of the kidneys, suggesting hepatotoxic medication-induced hepatic steatosis (Fig. 2C).
Liver US performed at week 86 during maintenance therapy showed increased periportal echogenicity in the main portal vein (A, arrow) and segmental portal branches (B, arrows). Liver US performed at week 90 demonstrated regression of periportal echogenicity (C), but it showed mild hyperechogenicity of liver parenchyma (arrow) compared with that of the kidney (arrowhead). Follow-up US one year after the first US still showed slight hyperechogenicity of liver parenchyma (D).
After normalization of the patient’s ALT levels, 6-MP and MTX treatments were reinitiated at week 88, with a decreased dose. However, the ALT levels elevated again, and the increase in MTX administration appeared to have a more negative effect than that of 6-MP, so MTX therapy was ended completely at week 101 (Fig. 1; Supplementary Table S2). In the same week, prednisolone and vincristine were added to the maintenance therapy to enable the dose reduction of 6-MP and to compensate for the cessation of MTX. The upper limit of the target leukocyte count for maintenance therapy was increased from 3.0 to 3.5 (E9/l). With these measurements, ALT levels could be maintained within an acceptable range. Prednisolone and vincristine therapy ceased at week 108. Pentamidine isethionate was substituted for sulfadiazine/trimethoprim until week 110. Mild hyperechogenicity of the liver parenchyma was observed one year after the first US (Fig. 2D).
Low doses of oral MTX combined with 6-MP during maintenance appeared intolerable for the patient. During the HD-MTX treatment, hepatotoxicity was not detected, and the liver enzymes remained within an acceptable range. The HD-MTX treatment resulted in mucositis, and because of that, the administration of HD-MTX was postponed once during induction.
Patients with severe hepatotoxicity during maintenance therapy with elevated MeMP levels
The remaining two patients with grade 4 ALT levels had high MeMP levels (>20 000 nmol/mmol Hgb), and both were TPMT wild type. One of them had a solitary high ALT value (856 U/l) at the end of treatment (day 902) and was asymptomatic, having previous ALT levels mainly below 200 U/l. This patient harbored none of the screened POLG variants.
The second patient had a POLG c.3708G>T (p.Q1236H) variant with a peak ALT level of 1145 U/l, which did not influence the maintenance drug doses and was not associated with liver failure. After two weeks, the patient’s ALT levels had dropped to 350 U/l. In the earlier phase of maintenance therapy, the patient developed hypoglycemia and nausea, with subsequent hyperbilirubinemia, jaundice, and itch. These symptoms are consistent with common side effects associated with 6-MP treatment and elevated MeMP levels [4]. During the episode, the US revealed cholecystitis (irritated gall bladder) but no dilated bile ducts and normal liver parenchyma. Bilirubin rose to 341 µmol/l (CTCAE grade 4; Table 1), but the ALT level was low (14–155 U/l), alkaline phosphatase was normal (276 U/l), and gamma–glutamyl transferase was CTCAE grade 1 (100 U/l). Platelets decreased to 66 E9/l and hemoglobin to 103 g/l, but total white blood cell (2.5 E9/l at the lowest) and neutrophil (1.45 E9/l) counts were within the target range. 6-MP was ceased for 4 weeks, and MTX was increased concurrently.
POLG variants
Of the nine common POLG1 variants screened in this study, four different variants, all heterozygous, were detected in 12 of the 34 patients (Table 1). Eight patients had only diagnostic bone marrow samples available, and of them, four patients had a POLG1 variant. The p.G517V variant was found only in the patient with clinically significant hepatotoxicity. To rule out a somatic variant, the p.G517V variant was detected in both diagnostic bone marrow and blood at follow-up. In addition to one patient with grade 4 ALT and bilirubin levels, seven patients harbored the p.Q1236H variant and had grade 3 ALT levels but showed no signs of clinical liver dysfunction. Of those, three had high MeMP levels. In addition, one patient harbored the p.A467T variant with grade 3 ALT with no available MeMP data. Two patients harbored the p.E1143G variant with normal or low ALT levels. In total, 21 of the 34 (62%) study patients had a grade 3 ALT level.
Mitochondrial DNA deletions
None of the study patients showed mtDNA deletions, indicating that the chemotherapy did not affect the integrity of mtDNA in blood and bone marrow cells. However, mtDNA deletions were not analyzed in the patients’ hepatocytes.
Discussion
We identified a patient who developed severe hepatotoxicity during ALL maintenance therapy with a wild-type TPMT allele and without concomitant elevated MeMP levels. She harbored a heterozygous POLG c.1550G>T (p.G517V) variant, which was not detected in the other patients.
The p.G517V variant locates in the spacer region of POLG1, which lies between the exonuclease and polymerase domains [5]. The spacer region is involved in multiple functions, including protein–protein interactions, enzyme activity, and DNA-binding affinity, and homozygous or compound heterozygous variants in the spacer region are disease associated [21, 22]. POLG1-related diseases present variable clinical manifestations, from infantile-onset epilepsy and liver failure to late-onset myopathy and ataxia [5]. The p.G517V variant has been associated with hepatocerebral syndromes, myopathy, peripheral neuropathy, and progressive external ophthalmoplegia syndrome [5, 23]. However, it is debated whether the p.G517V variant is a frequent single nucleotide polymorphism or a disease-associated pathogenic variant [5, 23]. Biochemical analysis has indicated that recombinant human POLG1 with the p.G517V variant retains 80–90% of its wild-type activity [24].
POLG1 variants cause variable phenotypes, and one considered mechanism is that the variability arises from ecogenetic variants (i.e., silent variants) that, under certain conditions, such as medication or epigenetic changes, present the clinical phenotype of POLG1 dysfunction [25]. This genetic modifier role, where different POLG alleles induce risk for clinical phenotypes, is present in VPA-induced mitochondrial liver failure [25]. The p.G571V variant may act as a genetic modifier that introduces mitochondrial toxicity and impairs Pol γ activity under specific medication or in combination with other gene variants. Staropoli et al. describe a patient with CLN5-associated neuronal ceroid lipofuscinosis harboring an additional heterozygous POLG1 p.G517V variant with decreased mtDNA copy number resulting in an atypical clinical phenotype [26]. Our hypothesis is that the genetic modifier role of the p.G517V variant may explain the hepatotoxicity triggered by maintenance drugs MTX and 6-MP in our study patient.
Our patient with the p.G517V variant seemed not to tolerate low-dose oral MTX, as an increase in the MTX dose with a concomitant decrease in the 6-MP dose resulted in clinical hepatotoxicity with elevated transaminases. The liver is a highly energy-dependent organ and, as such, is susceptible to drug-induced mitochondrial dysfunction, which is common in drug-induced liver failure [7, 27]. MTX has been shown to impair mitochondrial respiratory chain function [7]. In addition, oxidative stress caused by increased reactive oxygen species (ROS) and reduced glutathione levels may be a mechanism for MTX-induced mitochondrial toxicity [28,29,30]. MTX-induced impairment of the mitochondrial respiratory chain leads to reduced fatty acid oxidation and increased fatty acid accumulation (i.e., macrovacuolar steatosis), thus resulting in drug-induced hepatic steatosis [7]. This is in line with our patient, whose US revealed hepatic steatosis. Non-alcoholic steatohepatitis (NASH) has been observed in liver biopsies of patients with rheumatoid arthritis receiving low doses of oral MTX, although those patients had additional risk factors for NASH [31]. A recent study showed that therapeutic levels of low-dose MTX resulted in the accumulation of ROS and impairment of the mitochondrial respiratory chain on human hepatoma and hepatic stellate cells [30]. VPA-induced liver failure associated with POLG1 variants usually requires 2–3 months of VPA administration, ranging from 4 to 26 weeks, before the onset of symptoms [25, 32, 33]. Our study patient showed signs of hepatotoxicity after 62 weeks of oral antimetabolite therapy, and the symptoms occurred rapidly after increasing the MTX dose. The HD-MTX treatment did not cause clinically noticeable liver dysfunction for our patient. We hypothesize that the p.G517V variant imposes a risk for hepatotoxicity with long-term administration of low-dose oral MTX in connection with 6-MP during maintenance. However, this needs to be validated in further studies.
Pol γ has been shown to be affected by drugs used to treat ALL, especially thiopurines; chemotherapeutic drugs such as 6-thioguanine (6-TG) are incorporated into mtDNA, where they are oxidized [34]. These oxidized forms of DNA-incorporated 6-TG effectively inhibit Pol γ, thus decreasing mitochondrial replication, transcription, and protein synthesis [34]. Impaired protein synthesis and respiratory chain function cause depletion of adenosine triphosphate for energy usage [35]. Gene variants disrupting mitochondrial function may be risk factors for antimetabolite (6-MP, 6-TG, and MTX) therapy-induced hepatotoxicity in ALL. In previous genome-wide association or single-nucleotide polymorphism studies, POLG has not been associated with hepatotoxicity [36,37,38]. Liu et al. found that the PNPLA3 I148M variant is associated with elevated transaminases in pediatric ALL patients, and the gene has been linked to ALT elevations in other populations [36]. Known factors for 6-MP-related toxicity and hepatotoxicity are TPMT and NUDT15 variants [39, 40]. NUDT15 variants are more common in Asian populations [39]. In addition, polymorphisms of ITPA and ABCB1 have been associated with 6-MP-related hepatoxicity [41, 42]. As part of the NOPHO-ALL2008 treatment protocol, only TPMT genotyping was performed [40]. In this study, only POLG variants were analyzed, in addition to routine genotyping of TPMT, excluding other genetic variants that may cause drug-induced hepatotoxicity.
Aside from one patient with p.G517V and clinically severe hepatotoxicity, no significant correlation between POLG1 variants and ALT or bilirubin levels was observed in the patient cohort. One patient with the p.Q1236H variant developed clinical liver failure but conversely had high MeMP levels and hyperbilirubinemia with low ALT levels during the episode. The patient also had hypoglycemia during the episode, which has been associated with POLG1-related liver failure in Alpers patients with impaired mitochondrial respiratory chain activity [25], but it is also a common adverse effect of 6-MP treatment and high MeMP levels [4]. The p.Q1236H variant is common in Northern European populations, with a 14.8–15.9% prevalence in the Finnish population [21, 43]. It is considered a polymorphism, but it may have a role as a genetic modifier [21, 25]. Recently, the p.Q1236H variant has been shown not to associate with VPA-induced liver toxicity [33], in contrast to previously published studies [44].
Conclusion
This research may be considered a pilot study for the role of POLG1 variants in ALL maintenance therapy. The p.G517V variant was detected in the patient who developed clinically severe hepatotoxicity during oral maintenance therapy with MTX and 6-MP, which was not associated with 6-MP metabolism, as indicated by the presence of a wild-type TPMT variant and normal MeMP levels. The p.G517V variant was not detected in other cohort patients, but a limitation of this study was its small patient cohort. These findings call for larger studies of the impact of POLG1 variants on hepatotoxicity during maintenance therapy, including interactions with other variants influencing 6-MP and MTX drug disposition and tolerance.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Toksvang LN, de Pietri S, Nielsen SN, Nersting J, Albertsen BK, Wehner PS, et al. Hepatic sinusoidal obstruction syndrome during maintenance therapy of childhood acute lymphoblastic leukemia is associated with continuous asparaginase therapy and mercaptopurine metabolites. Pediatr Blood Cancer. 2017;64:e26519.
Ebbesen MS, Nygaard U, Rosthøj S, Sørensen D, Nersting J, Vettenranta K, et al. Hepatotoxicity during maintenance therapy and prognosis in children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2017;39:161–66.
Adam de Beaumais T, Fakhoury M, Medard Y, Azougagh S, Zhang D, Yakouben K, et al. Determinants of mercaptopurine toxicity in paediatric acute lymphoblastic leukemia maintenance therapy. Br J Clin Pharm. 2011;71:575–84.
Schmiegelow K, Nielsen SN, Frandsen TL, Nersting J. Mercaptopurine/methotrexate maintenance therapy of childhood acute lymphoblastic leukemia: clinical facts and fiction. J Pediatr Hematol Oncol. 2014;36:503–17.
Rahman S, Copeland WC. POLG-related disorders and their neurological manifestations. Nat Rev Neurol. 2019;15:40–52.
Vuda M, Kamath A. Drug induced mitochondrial dysfunction: Mechanisms and adverse clinical consequences. Mitochondrion 2016;31:63–74.
Begriche K, Massart J, Robin MA, Borgne-Sanchez A, Fromenty B. Drug-induced toxicity on mitochondria and lipid metabolism: mechanistic diversity and deleterious consequences for the liver. J Hepatol. 2011;54:773–94.
Naviaux RK, Nyhan WL, Barshop BA, Poulton J, Markusic D, Karpinski NC, et al. Mitochondrial DNA polymerase deficiency and mtDNA depletion in a child with Alpers’ Syndrome. Ann Neurol. 1999;45:54–8.
Uusimaa J, Hinttala R, Rantala H, Päivärinta M, Herva R, Röyttä M, et al. Homozygous W748S mutation in the POLG1 gene in patients with juvenile-onset Alpers syndrome and status epilepticus. Epilepsia 2008;49:1038–45.
Tzoulis C, Engelsen BA, Telstad W, Aasly J, Zeviani M, Winterthun S, et al. The spectrum of clinical disease caused by the A467T and W748S POLG mutations: a study of 26 cases. Brain 2006;129:1685–92.
Toft N, Birgens H, Abrahamsson J, Bernell P, Griškevičius L, Hallböök H, et al. Risk group assignment differs for children and adults 1-45 yr with acute lymphoblastic leukemia treated by the NOPHO ALL-2008 protocol. Eur J Haematol. 2013;90:404–12.
Howard SC, McCormick J, Pui CH, Buddington RK, Harvey RD. Preventing and managing toxicities of high-gose methotrexate. Oncologist. 2016;21:1471–82.
Weber BL, Tanyer G, Poplack DG, Reaman GH, Feusner JH, Miser JS, et al. Transient acute hepatotoxicity of high-dose methotrexate therapy during childhood. NCI Monogr. 1987;5:207–12.
Nielsen SN, Grell K, Nersting J, Abrahamsson J, Lund B, Kanerva J, et al. DNA-thioguanine nucleotide concentration and relapse-free survival during maintenance therapy of childhood acute lymphoblastic leukaemia (NOPHO ALL2008): a prospective substudy of a phase 3 trial. Lancet Oncol. 2017;18:515–24.
Frandsen TL, Heyman M, Abrahamsson J, Vettenranta K, Åsberg A, Vaitkeviciene G, et al. Complying with the European Clinical Trials Directive while surviving the administrative pressure—an alternative approach to toxicity registration in a cancer trial. Eur J Cancer. 2014;50:251–9.
Remes AM, Majamaa-Voltti K, Kärppä M, Moilanen JS, Uimonen S, Helander H, et al. Prevalence of large-scale mitochondrial DNA deletions in an adult Finnish population. Neurology 2005;64:976–81.
Sanger F, Nicklen S, Coulson AR. DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA. 1977;74:5463–7.
Werle E, Schneider C, Renner M, Völker M, Fiehn W. Convenient single-step, one tube purification of PCR products for direct sequencing. Nucleic Acids Res. 1994;22:4354–5.
U.S. Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. National Cancer Institute. 2017. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm [cited 2022 Jan 25].
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 2020;581:434–43.
Luoma PT, Luo N, Löscher WN, Farr CL, Horvath R, Wanschitz J, et al. Functional defects due to spacer-region mutations of human mitochondrial DNA polymerase in a family with an ataxia-myopathy syndrome. Hum Mol Genet. 2005;14:1907–20.
Nurminen A, Farnum GA, Kaguni LS. Pathogenicity in POLG syndromes: DNA polymerase gamma pathogenicity prediction server and database. BBA Clin. 2017;7:147–56.
Tang S, Wang J, Lee NC, Milone M, Halberg MC, Schmitt ES, et al. Mitochondrial DNA polymerase γ mutations: an ever expanding molecular and clinical spectrum. J Med Genet. 2011;48:669–81.
Kasiviswanathan R, Copeland WC. Biochemical analysis of the G517V POLG variant reveals wild-type like activity. Mitochondrion 2011;11:929–34.
Saneto RP, Cohen BH, Copeland WC, Naviaux RK. Alpers-Huttenlocher syndrome. Pediatr Neurol. 2013;48:167–78.
Staropoli JF, Xin W, Barone R, Cotman SL, Sims KB. An atypical case of neuronal ceroid lipofuscinosis with co-inheritance of a variably penetrant POLG1 mutation. BMC Med Genet. 2012;13:50.
Han D, Dara L, Win S, Than TA, Yuan L, Abbasi SQ, et al. Regulation of drug-induced liver injury by signal transduction pathways: critical role of mitochondria. Trends Pharm Sci. 2013;34:243–53.
al Maruf A, O’Brien PJ, Naserzadeh P, Fathian R, Salimi A, Pourahmad J. Methotrexate induced mitochondrial injury and cytochrome c release in rat liver hepatocytes. Drug Chem Toxicol. 2018;41:51–61.
Tabassum H, Parvez S, Pasha ST, Banerjee BD, Raisuddin S. Protective effect of lipoic acid against methotrexate-induced oxidative stress in liver mitochondria. Food Chem Toxicol. 2010;48:1973–9.
Schmidt S, Messner CJ, Gaiser C, Hämmerli C, Suter-Dick L. Methotrexate-induced liver injury is associated with oxidative stress, impaired mitochondrial respiration, and endoplasmic reticulum stress in vitro. Int J Mol Sci. 2022;23:15116.
Mori S, Arima N, Ito M, Fujiyama S, Kamo Y, Ueki Y. Non-alcoholic steatohepatitis-like pattern in liver biopsy of rheumatoid arthritis patients with persistent transaminitis during low-dose methotrexate treatment. PLoS ONE. 2018;13:e0203084.
Hynynen J, Komulainen T, Tukiainen E, Nordin A, Arola J, Kälviäinen R, et al. Acute liver failure after valproate exposure in patients with POLG1 mutations and the prognosis after liver transplantation. Liver Transplant. 2014;20:1402–12.
Hynynen J, Pokka T, Komulainen-Ebrahim J, Myllynen P, Kärppä M, Pylvänen L, et al. Variants p.Q1236H and p.E1143G in mitochondrial DNA polymerase gamma POLG1 are not associated with increased risk for valproate-induced hepatotoxicity or pancreatic toxicity: a retrospective cohort study of patients with epilepsy. Epilepsia 2018;59:2125–36.
Daehn I, Brem R, Barkauskaite E, Karran P. 6-thioguanine damages mitochondrial DNA and causes mitochondrial dysfunction in human cells. FEBS Lett. 2011;585:3941–6.
Russell OM, Gorman GS, Lightowlers RN, Turnbull DM. Mitochondrial diseases: hope for the future. Cell 2020;181:168–88.
Liu Y, Fernandez CA, Smith C, Yang W, Cheng C, Panetta JC, et al. Genome-wide study links PNPLA3 variant with elevated hepatic transaminase after acute lymphoblastic leukemia therapy. Clin Pharm Ther. 2017;102:131–40.
Choi R, Sohn I, Kim MJ, Woo HI, Lee JW, Ma Y, et al. Pathway genes and metabolites in thiopurine therapy in Korean children with acute lymphoblastic leukaemia. Br J Clin Pharm. 2019;85:1585–97.
Cao M, Yin D, Qin Y, Liao F, Su Y, Xia X, et al. Screening of novel pharmacogenetic candidates for mercaptopurine-induced toxicity in patients with acute lymphoblastic leukemia. Front Pharm. 2020;11:267.
Tanaka Y, Kato M, Hasegawa D, Urayama KY, Nakadate H, Kondoh K, et al. Susceptibility to 6-MP toxicity conferred by a NUDT15 variant in Japanese children with acute lymphoblastic leukaemia. Br J Haematol. 2015;171:109–15.
Wahlund M, Nilsson A, Kahlin AZ, Broliden K, Myrberg IH, Appell ML, et al. The role of TPMT, ITPA, and NUDT15 variants during mercaptopurine treatment of Swedish pediatric patients with acute lymphoblastic leukemia. J Pediatr. 2020;216:150–57.
Lee Y, Jang EJ, Yoon HY, Yee J, Gwak HS. Effect of ITPA polymorphism on adverse drug reactions of 6-mercaptopurine in pediatric patients with acute lymphoblastic leukemia: a systematic review and meta-analysis. Pharmaceuticals 2022;15:416.
Milosevic G, Kotur N, Krstovski N, Lazic J, Zukic B, Stankovic B, et al. Variants in TPMT, ITPA, ABCC4 and ABCB1 genes as predictors of 6-mercaptopurine induced toxicity in children with acute lymphoblastic leukemia. J Med Biochem. 2018;37:320–27.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 2016;536:285–91.
Stewart JD, Horvath R, Baruffini E, Ferrero I, Bulst S, Watkins PB, et al. Polymerase γ gene POLG determines the risk of sodium valproate-induced liver toxicity. Hepatology 2010;52:1791–6.
Acknowledgements
We thank Laura Kytövuori, Ph.D. (Research Unit of Clinical Medicine, University of Oulu, Finland), Pirjo Keränen, and Anja Heikkinen for their help in the laboratory; Kirsi Kvist-Mäkelä (NordLab Oulu, Oulu University Hospital, Finland) for preparing patient samples; and Biocenter Oulu Sequencing Center (Finland) for their services. This work was supported by the Foundation for Pediatric Research; Special State Grants for Health Research in the Department of Pediatrics and Adolescence, Oulu University Hospital, Finland; the Alma and K.A. Snellman Foundation, Oulu, Finland; the Väre Foundation for Pediatric Cancer Research; the Finnish Medical Foundation; the Oulu University Grant Fund, Finland; Medical Research Center Oulu’s doctoral program, Oulu University Hospital and the University of Oulu, Finland; and the Danish Childhood Cancer Foundation, Denmark. The funders had no role in the study design, data collection, analysis, the decision to publish, or the preparation of the paper.
Funding
Open Access funding provided by University of Oulu including Oulu University Hospital.
Author information
Authors and Affiliations
Contributions
RN, JU, RH, and AH-S were the principal investigators who conceived the study; AH-N performed laboratory analyses; TH and AH-N wrote the paper; AH-N and RH analyzed laboratory data; AH-S and RN were involved in patient recruitment; TH and RN analyzed the clinical data of the patients; TH produced the clinical tables and figures; MS-P analyzed US results and wrote the text for the figures and the radiological content, and SNN and KS collected data on the MeMP levels of the patients. All the authors agreed with the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Harju, T., Hurme-Niiranen, A., Suo-Palosaari, M. et al. DNA polymerase gamma variants and hepatotoxicity during maintenance therapy of childhood acute lymphoblastic leukemia: is there a causal relationship?. Pharmacogenomics J 23, 105–111 (2023). https://doi.org/10.1038/s41397-023-00303-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-023-00303-0