Abstract
Study Design
Cross-sectional validation study
Objectives
To cross-culturally translate and evaluate the psychometric properties of the Thai version of the Spinal Cord Independence Measure Self-Report (SCIM-SR-Thai) in Thai people with spinal cord injury (SCI)
Setting
Rehabilitation Ward at Maharaj Nakorn Chiang Mai Hospital
Methods
A cross-cultural forward and backward translation of the English version SCIM-SR into Thai was performed following the standard guideline. Sixty-one participants completed the SCIM-SR-Thai. On the same day, the rehabilitation medicine resident administered the Spinal Cord Independence Measure III (SCIM III) by observation. The Cronbach’s alpha, Pearson’s correlation coefficients and intraclass correlation coefficients (ICC) were used to assess internal consistency and concurrent validity, respectively. The Bland-Altman analysis and regression analysis evaluated the differences in scores between instruments. To explore the construct validity, confirmatory factor analysis (CFA) was conducted.
Results
The SCIM-SR-Thai provided excellent internal consistency (Cronbach’s alpha ≥ 0.96). The Pearson’s correlation coefficients and ICC revealed strong correlation with values of 0.93, 0.94, 0.95, and 0.97 in respiration and sphincter management, self-care, mobility, and total score, respectively. The regression analysis demonstrated that onset of injury of less than one year might be a possible predictor of the difference between the scores. CFA showed that the three-factor-model had an acceptable fit to the data but the unidimensional model fit the data better.
Conclusions
The SCIM-SR-Thai had excellent internal consistency and good validity for evaluating functional independence in Thai people with SCI. Persons with recent onset of injury might have limited ability for self-assessment of their functions.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) potentially causes various physical impairments resulting in activity limitations and declining independence [1]. Concerning an ultimate rehabilitation goal of improving functional level and independence [2], a valid and reliable instrument to evaluate functioning in activities of daily living relevant to persons with SCI is needed [3]. The third version of the Spinal Cord Independence Measure (SCIM III) has been used worldwide for assessment of the ability in performing basic daily tasks as well as the impact of the disability [4]. The SCIM III has demonstrated satisfactory validity and reliability in broad international study and is sensitive in detecting important functional changes in persons with SCI [4,5,6]. The main drawback of the SCIM III is the method of scoring that necessitates observation of the person’s performance by health professionals. Such observations are time-consuming (approximately 30-45 min) and mainly suitable in inpatient settings [7, 8].
To develop a self-administered questionnaire that requires less time and is applicable in both inpatient and outpatient settings [9], Fekete et al. developed the SCIM self-report (SCIM-SR) in 2013 [10]. The SCIM-SR has been validated and correlates well with the SCIM III [10]. It has also been cross-culturally adapted and translated into English [10], Italian [11], Spanish [12], French [13], and Thai languages [14]. Although the Thai version of SCIM-SR has recently been published by Wilartratsami et al., some limitations in their cross-cultural forward and backward translation process were noticed. They conducted only one back-translated English version which might limit the ability to compare wordings and identify ambiguous term in their Thai version of SCIM-SR. Also, their pre-final Thai version of SCIM-SR was tested in the healthy volunteers. In fact, pre-testing in the target population is recommended as they potentially provide useful suggestion based on their contexts to create the final version of the questionnaire [15]. Besides, they studied in an outpatient setting with a small sample size (32 participants) which might have been too small to give the statistical power needed to identify all significant differences and associations in subscale analysis. Additionally, the regression analysis for evaluating the predictor of discrepancy between scores of the SCIM III and SCIM-SR, and the factor analysis for testing the construct validity have not been conducted.
The purpose of this study was to translate the English version of SCIM-SR into another Thai version following the steps recommended by Beaton et al. [15] The cross-cultural adaptation of the items was considered to maintain the content validity of the instrument at a conceptual level across different cultures and languages. Also, the authors aimed to test the psychometric properties including internal consistency, concurrent validity, regression analysis and construct validity of the new version of SCIM-SR-Thai by comparing with the SCIM III.
Materials and Methods
The SCIM III and SCIM-SR
The SCIM III comprises 19 daily tasks organized in three functional subscales which are “Self-care” (6 items, range 0-20), “Respiration and sphincter management” (4 items, range 0-40), and “Mobility” (9 items, range 0-40). The total score ranges from 0 to 100 with higher scores indicating a higher level of functional independence. Scoring the SCIM III by observation is preferred over an interview [16]. The SCIM III has been translated into many languages, including Thai [17].
The self-report version of the SCIM III (SCIM-SR) consists of all 19 items classified into the same three subscales as in the SCIM III with equivalent scoring. Certain words or phrases in 19 items were adapted by using personal pronouns and avoiding technical terms. The complex items were decomposed to simplify self-reporting [10]. All the previous translated versions of SCIM-SR had been tested and revealed good validity related to the SCIM III [10,11,12, 14].
Translation and cross-cultural adaptation into the SCIM-SR-Thai
Permission to translate the English version of SCIM-SR into Thai was obtained from Professor Christine Fekete, one of the SCIM-SR developmental committee via electronic mail. The SCIM-SR-Thai was translated through forward and backward translation according to the recommendation by Beaton et al. [15]
Forward translation
Two drafts of the SCIM-SR-Thai were independently translated by a Thai physiatrist at Maharaj Nakorn Chiang Mai Hospital, an expert in spinal cord rehabilitation medicine, and a native Thai, uninformed, English specialist. The authors analyzed and composed the items of both draft versions with consideration of the suggestions from physical therapists and occupational therapists who work with people with SCI. The single draft of the SCIM-SR-Thai was then synthesized.
Backward Translation
The draft version of the SCIM-SR-Thai was independently translated back into two English versions by a nonmedical, native English speaker who is fluent in the Thai language and a nonmedical, English professional translator. Both translators were unaware of the original version of the questionnaire. The two back-translated versions were sent to Professor Christine Fekete and another native English speaker by electronic mail for feedback on understanding and discrepancy. Then, the draft version of the SCIM-SR-Thai was revised into the pre-final version of the SCIM-SR-Thai.
Pilot Study
The pre-final version of the SCIM-SR-Thai was completed by five participants with SCI (10% of the sample required for a full study) [18]. The Pearson’s correlation coefficients and intraclass correlation coefficients (ICC) were calculated to assess the association and agreement between scores of the SCIM III and the pre-final version of the SCIM-SR-Thai. The study revealed high Pearson’s correlation coefficients which were 0.95, 0.94, 0.94, and 0.98, and high ICC values which were 0.95, 0.93, 0.94, and 0.97 in the subscales of self-care, respiration and sphincter management, mobility, and total score, respectively. Each participant was interviewed about what he or she thought was meant by each questionnaire item and the chosen response [15]. The interview and feedback from participants revealed that items in the questionnaire were understandable with minor suggested adjustments. The final version of the SCIM-SR-Thai was obtained after revision based on all the suggestions. The SCIM-SR-Thai is in Supplementary Appendix 1.
Data Collection and Validation of the SCIM-SR-Thai
Participants
The sample size was calculated using the Bland-Altman method (MedCalc version 18.10) resulting in a minimum required number of 51 pairs of assessments between the SCIM-III and SCIM-SR-Thai scores. In the study, 61 participants who were admitted to the Rehabilitation Ward at Maharaj Nakorn Chiang Mai Hospital from June 2019 to August 2020 were recruited. The criteria for eligibility included a traumatic or non-traumatic SCI, age of 20 years old or older, and proficient Thai language skills required for independently reading and answering the self-report questionnaire. A history of brain disorder, traumatic brain injury, or disease affecting cognitive function was excluded. The participants gave written-informed consent before completing the questionnaire.
Data Collection Procedure
The participants completed a paper-pencil version of the SCIM-SR-Thai. If they had limited hand function, their caregiver helped with writing but did not explain the items or guide the answers. Assistance with questionnaire completion and the time required were recorded. On the same day, the SCIM III was completed through observation by one out of five rehabilitation medicine residents. Before the data collection procedure, all five residents were tested for the inter-rater reliability which demonstrated the ICC values of above 0.9 for the total and all subscale scores indicating excellent inter-rater reliability. The participant and the resident were blinded to each other’s scores. Sociodemographic data (age, gender, education level), lesion characteristics (time since injury, etiology, severity of SCI), and reason for admission were collected using the international SCI core data set [19, 20].
Statistical Analysis
The data was analyzed using SPSS version 22.0 and MedCalc version 19.5.3. The descriptive statistics were applied to describe the characteristics of the study population and the scores of the SCIM III and the SCIM-SR-Thai. The frequency and percentage were used to describe categorical variables, mean with standard deviation (SD) for normally distributed numerical variables, and median with interquartile range (IQR) for non-normally distributed numerical variables. The floor or ceiling effects were considered to be present if more than 15% of participants reported the lowest or highest possible scores in each scale, respectively [21].
For the psychometric properties, the internal consistency was assessed using Cronbach’s alpha coefficients. Values of 0.7 or higher were considered adequate [22]. The Pearson’s correlation coefficients were calculated to examine the association between the SCIM III and the SCIM-SR-Thai scores which were described as follows: ±0.1 indicating poor, ±0.3 indicating fair, ±0.6 indicating moderate, and ±0.8 indicating very strong correlation [23]. ICC were used to evaluate the agreement between instruments. Coefficient values of less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and greater than 0.9 were indicative of poor, moderate, good, and excellent agreement, respectively [24].
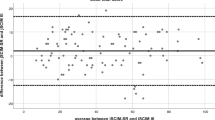
The Bland-Altman method was used to analyze the mean differences and limits of agreement (LOA) to describe the agreement between instruments. The Bland-Altman plots showed the differences of scores between instruments against the mean scores of both instruments for each participant, which were useful for detecting the outliers. The stratified mean differences between total scores in association with variable categories (gender, age, education level, time since injury, etiology, severity of SCI, assistance for questionnaire completion, and reason for admission) were calculated. In linear regression analysis, the authors used the mean differences of the total scores as continuous outcomes and regressed them on variables categories. A p-value of less than 0.05 was considered statistically significant.
The construct validity of the SCIM-SR-Thai was investigated using confirmatory factor analysis (CFA). Both the three-factor-model and unidimensional model of the SCIM-SR-Thai were analyzed. The goodness of fit indices was described as a comparative fit index (CFI) of ≥ 0.95, Tucker-Lewis index (TLI) of ≥ 0.9, and a root-mean-square error of approximation (RMSEA) of ≤ 0.06 (0.08). Chi-square/degree of freedom (χ2/df) of < 3 indicating acceptably fit [25]. The CFA was performed using AMOS version 22.
Results
Translation and cross-cultural adaptation
A minor adaptation was made to give more examples of specific equipment or specific settings which were commonly used by Thai people with SCI to describe the items in the questionnaire. In item no. 2 “Bathing”, a shower bench and a commode wheelchair were added as examples of the specific equipment. In item no. 3 “Dressing”, for the specific setting, the authors added bed railings, a wheelchair, or a bed if they need to position a wheelchair or a bed to enable them to dress. In item no. 8 “Using the toilet”, the authors described the need for a specific setting as if they need to do bowel routine in a commode wheelchair, on a bed, or a shower bench. In item no. 11 “Transfer from the wheelchair to toilet/tub”, more examples of shower surface, the choices of which including a shower bench, a shower chair, or a commode wheelchair were added because they were used more frequently than a tub among Thai people with SCI.
Characteristics of the study population
Sixty-one individuals with SCI were recruited. Most participants were male (43/61, 70.5%). The mean (SD) age was 52.2 (15.4) with median (IQR) time since SCI of 1.0 (0.0-4.5) years. Most of the participants were diagnosed with AIS group D (24/61, 39.4%). The median (IQR) time needed to complete the questionnaire was 10.0 (10.0-15.0) minutes. The characteristics of the study population are presented in Table 1.
Psychometric properties of the SCIM-SR-Thai
The descriptive statistics of the SCIM III and the SCIM-SR-Thai scores are listed in Table 2. The floor and ceiling effects of the SCIM-SR-Thai were less than 15%. There was no missing value in the study.
For the internal consistency, the Cronbach’s alpha values for the subscale of self-care, respiration and sphincter management, mobility, and the total score were 0.96, 0.96, 0.97, and 0.98, respectively. Pearson’s correlation coefficients, ICC, and the Bland–Altman differences between the SCIM III and the SCIM-SR-Thai scores are shown in Table 3. The Bland-Altman plots in Fig. 1 showed a few outliers for each scale.
Stratified differences and linear regression on mean differences between the total score of the SCIM III and the SCIM-SR-Thai are shown in Table 4. For stratified differences, the 95% confidence interval in all categories contained the 0 value. Thus, there was no significant difference between the total scores of the SCIM III and the SCIM-SR-Thai in any category. However, the study demonstrated a significant difference of agreement for total group regression with the unstandardized coefficients of 0.062, SD = 0.031 (p-value = 0.048). To investigate the source of bias, outlier identification was performed. After one outlier was excluded, the unstandardized coefficients converted to 0.039, SD = 0.032 (p-value = 0.226), indicating no significant difference of agreement for the total group regression. When analyzed the relationship of the outlier and the regression analysis in variable categories, it revealed that time since the injury of less than one year might be a possible significant predictor of the difference between the total score of two questionnaires as the p-value was 0.048 (using time since injury of ≥15 years as the reference).
The results of CFA are in Supplementary Appendix 2. The three-factor solution tended to be acceptably fit the data with the CFI of 0.928, TLI of 0.902, RMSEA of 0.101 (90% CI = 0.074–1.126), chi-square (χ2) of 200.598, and degree of freedom (df) of 126 (χ2/df = 1.60). However, the unidimensional model fitted the data better with the CFI of 0.948, TLI of 0.927, RMSEA of 0.092 (90% CI = 0.061–0.120), χ2 of 164.254, and df of 109 (χ2/df = 1.50). The fit statistics for both models were based on the fact that the error terms of the indicators within the same subscale were correlated.
Discussion
In the cross-cultural translation process, the added examples of specific equipment or specific settings which were commonly used by Thai people with SCI made the current version of SCIM-SR-Thai different from the Thai version by Wilartratsami et al. [14] The authors were confident that all the examples were relevant to the recommendation for using SCIM III and SCIM-SR [7] to keep the original meaning of the questionnaire. There were some other differences between the two versions of the Thai translated SCIM-SR. For the word “laces” in item no. 3, the Thai version of SCIM-SR by Wilartratsami et al. used the word “laces” in English but in the current version, this word was translated into the Thai language. Another difference was the word “wheelchair”, the Thai version by Wilartratsami et al. translated this word into Thai but in our questionnaire, the word wheelchair written in Thai was used instead.
The mean and median of the SCIM III and the SCIM-SR-Thai scores were similar for all scales, indicating that the participants and the observers rated the participants’ performance to be the same. This might be resulted from the added examples of the items in the questionnaire which facilitated understanding and self-reporting. Also, the study in IPD setting provided enough time for the observers to observe the participants’ function. The similarity in mean and median scores of the SCIM III and the SCIM-SR was also reported in the studies validating the Italian version [11], Spanish version [12], and the Thai version of SCIM-SR by Wilartratsami et al. [14]. However, the study by Fekete et al. [10] found that the participants rated their function higher than health professionals particularly in the subscale of mobility. The floor and ceiling effects were acceptable in our study contrary to the study of the Thai version of SCIM-SR by Wilartratsami et al. which showed the floor effect of up to 21.9% in the mobility subscale [14].
The Cronbach’s alpha values in all subscales indicated excellent internal consistency. The Pearson’s correlation coefficients and ICC values denoted excellent association and strong agreement between the SCIM III and the SCIM-SR-Thai in all subscales. The greatest correlation in the mobility subscale was similar to the study of the Thai version of SCIM-SR by Wilartratsami et al. which showed Pearson’s correlation coefficient of 0.96 [14]. The lowest correlation was found in the subscale of respiration and sphincter management which was comparable to all the previous translated versions (ICC ranging from 0.78 to 0.80, Pearson’s correlation coefficients ranging from 0.80 to 0.85) [10, 11, 14]. The small mean differences which were close to 0 according to Bland-Altman analysis supported the agreement between two instruments, especially in the mobility subscale. The strongest correlation and agreement in this subscale might be since it was the most obvious area to be noticed by both external raters and participants.
Furthermore, it was found that possible significant predictor of the difference between the SCIM III and the SCIM-SR-Thai scores was persons with time since injury of less than one year. This might be attributed to the doubts about their functions, whether they had recently changed or there were still some possible clinical changes which could vary their function at the time. In other words, it would be easier for persons with longer experience with SCI to assess their functional independence. The study of the original SCIM-SR by Fekete et al. revealed that persons who got assistance for questionnaire completion showed less difference in scoring than those who filled in the questionnaire alone. Besides, it was found that persons who were hospitalized because of acute health conditions (e.g., pressure ulcer) did not report on their current situation [10]. This was not observed in our study which might be owing to a clearer introductory text that emphasized the relation to the current situation as suggested from their study.
The CFA demonstrated that the unidimensional model fit the data better than the three-factor-model. It might imply that even though the original version of the questionnaire divided the items into three subscales, it was better not to divide the items into any subscale at all because all the items tended to measure the same construct of independence. Thus, the total score might be more accurately representing functional independence, or it was more reasonable to apply the total score than to use the score of each subscale alone. However, our sample size was quite small for the study of CFA and it might give some different results from a study with a larger sample size. Moreover, no previous studies of the SCIM-SR had reported the CFA for comparison.
There were some limitations in the study. The study was carried out only in IPD setting. Many participants were hospitalized due to health conditions that temporarily limited their functional independence. Therefore, the authors could not assess the sensitivity of the questionnaire to improvement in functional level. Also, the reliability testing of the SCIM-SR-Thai was not performed. For further study, the reliability of the questionnaire (e.g., test-retest study) and its responsiveness should be performed. Additionally, to confirm the CFA result, the authors suggest using a larger sample size of at least 10 times the total number of the items [26]. More study to define unnecessary items of the SCIM-SR-Thai might also be useful for an appropriate adaptation of the questionnaire.
About strengths, the regression analysis revealed that differences in educational level did not significantly affect the difference in scoring. Therefore, the authors believed that wording of the SCIM-SR-Thai was simple and understandable. For the participants, a broad spectrum of sociodemographic and lesion characteristics was included with sufficient sample size for a validation study and sensitivity analysis. Studying in IPD setting allowed enough time for the rehabilitation medicine residents to truly observe the participants’ function and did not rely on the data from the participants in scoring. In the data collection process, the exact time which participants used to complete the questionnaire was recorded. This supported the benefit of using the self-reporting questionnaire as it required less time to complete.
In conclusion, the SCIM-SR-Thai provided excellent internal consistency and good validity for evaluating functional independence in Thai people with SCI. Our findings signified the usefulness of the SCIM-SR-Thai for assessing the hospitalized individuals and the likelihood to be applicable for a continuous evaluation of the community-dwelling people. These would be beneficial in defining individual specific care needs and guiding appropriate rehabilitation planning. Persons with recent onset of injury might have limited ability for self-assessment of their current functions and independence.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rahman MH. Spinal cord injury and importance of patient assessment based on international classification of functioning, disability and health (ICF). Int Phys Med Rehab J. 2017;2:190.
Anderson K, Aito S, Atkins M, Biering-Sorensen F, Charlifue S, Curt A, et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2008;31:133–44.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM–spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K, et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2011;49:880–5.
Rick Hansen Institute. Toolkit for Spinal Cord Independence Measure III (SCIM III) [Internet]. 2016 [cited 2020 Nov 14]. Available from: https://scireproject.com/wp-content/uploads/SCIM_Toolkit _Printable-1.pdf.
Dorevitch M. The ‘questionnaire’ versus the ‘direct observation’ approach to functional assessment. Br J Rheumatol. 1988;27:326–7.
Hoenig H, McIntyre L, Sloane R, Branch LG, Truncali A, Horner RD, et al. The reliability of a self-reported measure of disease, impairment, and function in persons with spinal cord dysfunction. Arch Phys Med Rehabil. 1998;79:378–87.
Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Luthi H, et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2013;51:40–7.
Bonavita J, Torre M, China S, Bressi F, Bonatti E, Capirossi R, et al. Validation of the Italian version of the Spinal Cord Independence Measure (SCIM III) Self-Report. Spinal Cord. 2016;54:553–60.
Aguilar-Rodriguez M, Pena-Paches L, Grao-Castellote C, Torralba-Collados F, Hervas-Marin D, Giner-Pascual M, et al. Adaptation and validation of the Spanish self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2015;53:451–4.
Prodinger B, Ballert CS, Brinkhof MW, Tennant A, Post MW. Metric properties of the Spinal Cord Independence Measure - Self Report in a community survey. J Rehabil Med. 2016;48:149–64.
Wilartratsami S, Luksanapruksa P, Santipas B, Thanasomboonpan N, Kulprasutdilok P, Chavasiri S, et al. Cross-cultural adaptation and psychometric testing of the Thai version of the Spinal Cord Independence Measure III-Self Report. Spinal Cord. 2021;59:291–7.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–91.
Itzkovich M, Shefler H, Front L, Gur-Pollack R, Elkayam K, Bluvshtein V, et al. SCIM III (Spinal Cord Independence Measure version III): reliability of assessment by interview and comparison with assessment by observation. Spinal Cord. 2018;56:46–51.
Wannapakhe J, Saensook W, Keawjoho C, Amatachaya S. Reliability and discriminative ability of the Spinal Cord Independence Measure III (Thai version). Spinal Cord. 2016;54:213–20.
Connelly LM. Pilot studies. Medsurg Nurs. 2008;17:411–2.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International spinal cord injury core data set. Spinal Cord. 2006;44:535–40.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0) including standardization of reporting. Spinal Cord. 2017;55:759–64.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42.
Taber KS. The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48:1273–96.
Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18:91–3.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Hu LBP. Cut off criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55.
Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology. 2018;9:2207–30.
Acknowledgements
The authors would like to acknowledge Assoc. Prof. Apichana Kovindha, M.D., FRCPhysiatrT; Ms. Oyporn Chingchayanurux; Assoc. Prof. Jan Theo De Vleeschauwer; and Mr. Clayton Shuttleworth for translating the SCIM-SR; Assoc. Prof. Jakkrit Klaphajone, M.D., FRCPhysiatrT; and Ms. Ruth Leatherman for English proofreading; and Ms. Rodchana Janpueak for providing statistical advice.
Author information
Authors and Affiliations
Contributions
ST, TW, and CS designed the research questions. ST and CS collected the data. TW and CS analyzed the data. CS drafted the manuscript and wrote the final version of the manuscript. ST and TW commented on the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study protocol was approved by the institutional Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. The study number is REH-2562-06383. The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during all courses of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tongprasert, S., Wongpakaran, T. & Soonthornthum, C. Validation of the Thai version of the Spinal Cord Independence Measure Self-Report (SCIM-SR-Thai). Spinal Cord 60, 361–367 (2022). https://doi.org/10.1038/s41393-022-00779-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00779-w