Abstract
Background
Different strategies have been proposed to prevent lymphocele (LC) formation after radical prostatectomy (RARP) with pelvic lymph node dissection (PLND). According to several recently published randomized control trials (RCTs) on the topic, peritoneal reconfiguration appears to be associated with promising results. This systematic review aimed to assess the impact of peritoneal reconfiguration on LC formation in patients undergoing RARP and PLND.
Methods
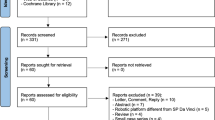
A comprehensive bibliographic search was conducted in August 2023. Studies assessing patients with prostate cancer undergoing RARP with PLND (P) and concomitant peritoneal reconfiguration (I) compared or not with other techniques (C) to prevent LC formation (O) were included. Original prospective and retrospective studies (S) were selected. LC and symptomatic LC rates were chosen as co-primary outcomes. Only RCTs were included in the meta-analysis.
Results
Eleven studies investigating 2991 patients were included in the systematic review, and five RCTs evaluating 1712 subjects were deemed eligible for meta-analysis. Peritoneal flap (PF) was the most common surgical technique used for LC prevention (9 studies). A significantly lower likelihood of LC was observed after PF (OR 0.82, 95% CI 0.27–1.37, I2 = 74.54%), with no significant difference in terms of symptomatic LC (OR 0.21, 95% CI −0.41–0.84, I2 = 0%). Probability of LC-related complications (OR 0.36, 95% CI 0.04–0.67, I2 = 0%), Clavien-Dindo ≥ 3 overall complications (OR 0.61, 95% CI 0.21–1.0, I2 = 0%), and Clavien-Dindo ≥ 3 LC-related complications (OR 0.98, 95% CI 0.29–1.67, I2 = 0%) were significantly lower after PF.
Conclusions
PF after RARP with PLND reduces LC formation, LC-related complications, and severe postoperative adverse events.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Sheets containing raw data (extracted variables, statistical analyses) are available upon request to the corresponding author.
References
Mottet N, Cornford P, Van den Bergh R, Eberli D, De Meerleer G, De Santis M, et al. EAU Guidelines on Prostate Cancer. Edn presented at the EAU Annual Congress Milan. 2023. ISBN 978-94-92671-19-6
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically Localized Prostate Cancer: AUA/ASTRO Guideline, Part II: Principles of Active Surveillance, Principles of Surgery, and Follow-Up. J Urol. 2022;208:19–25.
Fiori C, Checcucci E, Stura I, Amparore D, De Cillis S, Piana A, et al. Development of a novel nomogram to identify the candidate to extended pelvic lymph node dissection in patients who underwent mpMRI and target biopsy only. Prostate Cancer Prostatic Dis. 2023;26:388–94.
Masterson J, Luu M, Naser-Tavakolian A, Freedland S, Sandler H, Zumsteg Z, et al. Concurrent prognostic utility of lymph node count and lymph node density for men with pathological node-positive prostate cancer. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-022-00635-1
Creta M, Manfredi C, Arcaniolo D, Spirito L, Kaplan SA, Woo HH, et al. Functional and oncological outcomes after radical prostatectomy in patients with history of surgery for lower urinary tract symptoms related to benign prostatic enlargement: A systematic review with meta-analysis. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-023-00678-y
Briganti A, Chun FKH, Salonia A, Suardi N, Gallina A, Da Pozzo LF, et al. Complications and Other Surgical Outcomes Associated with Extended Pelvic Lymphadenectomy in Men with Localized Prostate Cancer. Eur Urol. 2006;50:1006–13.
Orvieto MA, Coelho RF, Chauhan S, Palmer KJ, Rocco B, Patel VR. Incidence of lymphoceles after robot-assisted pelvic lymph node dissection. BJU Int. 2011;108:1185–90.
Keskin MS, Argun ÖB, Öbek C, Tufek I, Tuna MB, Mourmouris P, et al. The incidence and sequela of lymphocele formation after robot-assisted extended pelvic lymph node dissection. BJU Int. 2016;118:127–31.
Lebeis C, Canes D, Sorcini A, Moinzadeh A. Novel technique prevents lymphoceles after transperitoneal robotic-assisted pelvic lymph node dissection: Peritoneal flap interposition. Urology. 2015;85:1505–9.
Stolzenburg JU, Wasserscheid J, Rabenalt R, Do M, Schwalenberg T, McNeill A, et al. Reduction in incidence of lymphocele following extraperitoneal radical prostatectomy and pelvic lymph node dissection by bilateral peritoneal fenestration. World J Urol. 2008;26:581–6.
Naselli A, Andreatta R, Introini C, Fontana V, Puppo P. Predictors of Symptomatic Lymphocele After Lymph Node Excision and Radical Prostatectomy. Urology. 2010;75:630–5.
Waldert M, Remzi M, Klatte T, Klingler HC. Floseal reduces the incidence of lymphoceles after lymphadenectomies in laparoscopic and robot-assisted extraperitoneal radical prostatectomy. J Endourol. 2011;25:969–73.
Grande P, Di Pierro GB, Mordasini L, Ferrari M, Würnschimmel C, Danuser H, et al. Prospective Randomized Trial Comparing Titanium Clips to Bipolar Coagulation in Sealing Lymphatic Vessels During Pelvic Lymph Node Dissection at the Time of Robot-assisted Radical Prostatectomy. Eur Urol. 2017;71:155–8.
Yılmaz K, Ölçücü MT, Arı Ö, Karamik K, Aktaş Y, Savaş M, et al. The Results of Peritoneal Re-Approximation Methods on Symptomatic Lymphocele Formation in Robot-Assisted Laparoscopic Radical Prostatectomy and Extended Pelvic Lymphadenectomy. Arch Esp Urol. 2022;75:447–52.
Student V, Tudos Z, Studentova Z, Cesak O, Studentova H, Repa V, et al. Effect of Peritoneal Fixation (PerFix) on Lymphocele Formation in Robot-assisted Radical Prostatectomy with Pelvic Lymphadenectomy: Results of a Randomized Prospective Trial. Eur Urol. 2023;83:154–62.
Neuberger M, Kowalewski K, Simon V, von Hardenberg J, Siegel F, Wessels F, et al. Peritoneal Flap for Lymphocele Prophylaxis Following Robotic-assisted Radical Prostatectomy with Lymph Node Dissection: The Randomised Controlled Phase 3 PELYCAN Trial. Eur Urol Oncol. 2023; https://doi.org/10.1016/j.euo.2023.07.009 S2588-931100152-9.
Bründl J, Lenart S, Stojanoski G, Gilfrich C, Rosenhammer B, Stolzlechner M, et al. Peritoneal flap in robot-assisted radical prostatectomy: Results of a multicenter, randomized, single-blind study (PIANOFORTE) of the efficacy in reducing postoperative lymphocele. Dtsch Arztebl Int 2020;117:243–50.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst Rev. 2017;6:245.
Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37:387.
Motterle G, Morlacco A, Zanovello N, Ahmed ME, Zattoni F, Karnes RJ, et al. Surgical Strategies for Lymphocele Prevention in Minimally Invasive Radical Prostatectomy and Lymph Node Dissection: A Systematic Review. J Endourol. 2020;34:113–20.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberatiet A, al. The Oxford 2011 Levels of Evidence. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Last access: August 12, 2023.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Ma J, Liu W, Hunter A, Zhang W. Performing meta-analysis with incomplete statistical information in clinical trials. BMC Med Res Methodol. 2008;8:56.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74:785–94.
Wagner J, McLaughlin T, Pinto K, Tortora J, Gangakhedkar A, Staff I. The Effect of a Peritoneal Iliac Flap on Lymphocele Formation After Robotic Radical Prostatectomy: Results From the PLUS Trial. Urology. 2023;173:104–10.
Harland N, Alfarra M, Erne E, Maas M, Amend B, Bedke J, et al. A Peritoneal Purse-String Suture Prevents Symptomatic Lymphoceles in Retzius-Sparing Robot-Assisted Radical Prostatectomy. J Clin Med. 2023;12:791.
Gloger S, Ubrig B, Boy A, Leyh-Bannurah SR, Siemer S, Arndt M, et al. Bilateral Peritoneal Flaps Reduce Incidence and Complications of Lymphoceles after Robotic Radical Prostatectomy with Pelvic Lymph Node Dissection - Results of the Prospective Randomized Multicenter Trial ProLy. J Urol. 2022;208:333–40.
Boğa MS, Sönmez MG, Karamik K, Yilmaz K, Savaş M, Ateş M. The effect of peritoneal re-approximation on lymphocele formation in transperitoneal robot-assisted radical prostatectomy and extended pelvic lymphadenectomy. Turk J Urol. 2020;46:460–7.
Lee M, Lee Z, Eun DD. Utilization of a Peritoneal Interposition Flap to Prevent Symptomatic Lymphoceles after Robotic Radical Prostatectomy and Bilateral Pelvic Lymph Node Dissection. J Endourol. 2020;34:821–7.
Dal Moro F, Zattoni F. P.L.E.A.T.—Preventing Lymphocele Ensuring Absorption Transperitoneally: A Robotic Technique. Urology. 2017;110:244–7.
Pose RM, Knipper S, Würnschimmel C, Tennstedt P, Michl U, Maurer T, et al. Significant reduction of lymphoceles after radical prostatectomy and pelvic lymph node dissection. BJU Int. 2021;128:728–33.
Kallappan S, Manickam R, Nachimuthu S, Ganesapandi T. Unusual lymphocele following radical cystectomy with orthotopic neobladder. Indian J Urol. 2019;35:168–9.
Basourakos SP, Zhu A, Lewicki PJ, Ramaswamy A, Cheng E, Dudley V, et al. Clipless Robotic-assisted Radical Prostatectomy and Impact on Outcomes. Eur Urol Focus. 2022;8:1176–85.
Danuser H, Di Pierro GB, Stucki P, Mattei A. Extended pelvic lymphadenectomy and various radical prostatectomy techniques: Is pelvic drainage necessary? BJU Int. 2013;111:963–9.
Territo A, Baboudjian M, Diana P, Gallioli A, Verri P, Uleri A, et al. To drain or not to drain in uro-oncological robotic surgery? A systematic review and meta-analysis. Minerva Urol Nephrol. 2023;75:144–53.
Capitanio U, Pellucchi F, Gallina A, Briganti A, Suardi N, Salonia A, et al. How can we predict lymphorrhoea and clinically significant lymphocoeles after radical prostatectomy and pelvic lymphadenectomy? Clinical implications. BJU Int. 2011;107:1095–101.
Seetharam Bhat KR, Onol F, Rogers T, Ganapathi HP, Moschovas M, Roof S, et al. Can we predict who will need lymphocele drainage following robot assisted laparoscopic prostatectomy (RALP)? J Robot Surg. 2020;14:439–45.
May M, Gilfrich C, Bründl J, Ubrig B, Wagner JR, Gloger S, et al. Impact of Peritoneal Interposition Flap on Patients Undergoing Robot-assisted Radical Prostatectomy and Pelvic Lymph Node Dissection: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur Urol Focus. 2023. https://doi.org/10.1016/j.euf.2023.07.007 S2405-456900181-5.
Author information
Authors and Affiliations
Contributions
Conceptualization and supervision: RA; Study screening, paper selection, data extraction, and risk of bias assessment: FD, AF; Data analysis and interpretation: FD, CM; Paper drafting: FD, CM, AF; Drawing: FDM; Statistical review: AV; Scientific and grammatical review: AA, CDN, MDS. All authors approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ditonno, F., Manfredi, C., Franco, A. et al. Impact of peritoneal reconfiguration on lymphocele formation after robot-assisted radical prostatectomy with pelvic lymph node dissection: a systematic review and meta-analysis of randomized controlled trials. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00744-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00744-5