Abstract
Background
Aim of our study was to review the current evidence on single port robot-assisted radical prostatectomy (SP-RARP) and SP robot-assisted simple prostatectomy (SP-RASP) procedures.
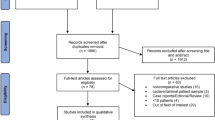
Methods
A comprehensive bibliographic search on multiple databases was conducted in July 2023. Studies were included if they assessed patients with non-metastatic prostate cancer or candidate for benign prostatic hyperplasia surgery (P) who underwent SP-RARP or SP-RASP, respectively, (I), compared or not with other surgical techniques (C), evaluating perioperative, oncological, or functional outcomes (O). Prospective and retrospective original articles were included (S). A meta-analysis of comparative studies between SP-RARP and MP-RARP was performed.
Results
A total of 21 studies investigating 1400 patients were included in our systematic review, 18 were related to SP-RARP while 3 to SP-RASP. Only 8 comparative studies were eligible for meta-analysis. Mean follow-up was 8.1 (±5.8) months. Similar outcomes were observed for SP-RARP and MP-RARP in terms of operative time, catheterization time, pain score, complications rate, continence and potency rates, positive surgical margin, and biochemical recurrence. Length of hospital stay was shorter in the SP group after sensitivity analysis (WMD −0.58, 95% IC −1.17 to −0.9, p < 0.05). Subgroup analysis by extraperitoneal approach did not show any statistical difference, except for a lower positive margins rate in the SP extraperitoneal technique compared to MP-RARP. Overall, SP-RASP exhibited shorter hospital stay and lower rate of de novo urinary incontinence when compared to other techniques, while no differences were reported in terms of postoperative International Prostate Symptom Score, post void residual and maximum flow.
Conclusions
Overall comparable oncological, functional, and perioperative outcomes can be achieved with SP platform. Subgroup analysis by different approaches did not reveal significant variations in outcomes. However, the retrospective nature of the studies, the limited follow-up, and the relatively small sample size of selected Centers may impact these results.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Sheets containing raw data (extracted variables, statistical analyses) are available upon request to the corresponding author.
References
Autorino R, Kaouk JH, Stolzenburg JU, Gill IS, Mottrie A, Tewari A, et al. Current status and future directions of robotic single-site surgery: a systematic review. Eur Urol. 2013;63. https://doi.org/10.1016/j.eururo.2012.08.028.
Pandolfo SD, Del Giudice F, Chung BI, Manfredi C, De Sio M, Damiano R, et al. Robotic assisted simple prostatectomy versus other treatment modalities for large benign prostatic hyperplasia: a systematic review and meta-analysis of over 6500 cases. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00616-4.
Ferretti M, Phillips J. Prostatectomy for benign prostate disease: open, laparoscopic and robotic techniques. Can J Urol. 2015;22. Suppl 1:60–6.
Sirisopana K, Jenjitranant P, Sangkum P, Kijvikai K, Pacharatakul S, Leenanupun C, et al. Perioperative outcomes of robotic-assisted laparoscopic radical prostatectomy, laparoscopic radical prostatectomy and open radical prostatectomy: 10 years of cases at Ramathibodi Hospital. Transl Androl Urol. 2019. https://doi.org/10.21037/tau.2019.09.03.
Mazzone E, Mistretta FA, Knipper S, Tian Z, Larcher A, Widmer H, et al. Contemporary national assessment of robot-assisted surgery rates and total hospital charges for major surgical uro-oncological procedures in the United States. J Endourol. 2019;33. https://doi.org/10.1089/end.2018.0840.
Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J Urol. 2018;200. https://doi.org/10.1016/j.juro.2018.05.048.
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015. https://doi.org/10.1016/j.eururo.2014.12.038.
Franco A, Pellegrino AA, De Nunzio C, Salkowski M, Jackson JC, Zukowski LB, et al. Single-port robot-assisted radical prostatectomy: where do we stand? Curr Oncol. 2023;30:4301–10.
Khalil MI, Joseph JV. extraperitoneal single-port robot-assisted radical prostatectomy. J Endourol. 2021;35: S-100-S-105.
Kaouk J, Sawczyn G, Wilson C, Aminsharifi A, Fareed K, Garisto J, et al. Single-port percutaneous transvesical simple prostatectomy using the SP robotic system: initial clinical experience. Urology. 2020. https://doi.org/10.1016/j.urology.2020.02.024.
Kaouk J, Bertolo R, Eltemamy M, Garisto J. Single-port robot-assisted radical prostatectomy: first clinical experience using the SP surgical system. Urology. 2019. https://doi.org/10.1016/j.urology.2018.10.025.
Balasubramanian S, Shiang A, Vetter JM, Henning GM, Figenshau RS, Kim EH. Comparison of three approaches to single-port robot-assisted radical prostatectomy: our institution’s initial experience. J Endourol. 2022;36:1551–58.
Khalil MI, Chase A, Joseph JV, Ghazi A. Standard multiport vs single-port robot-assisted simple prostatectomy: a single-center initial experience. J Endourol. 2022;36. https://doi.org/10.1089/end.2021.0510.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. https://doi.org/10.1136/bmj.n71.
Amir-Behghadami M, Janati A. Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37. https://doi.org/10.1136/emermed-2020-209567.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366. https://doi.org/10.1136/bmj.l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355. https://doi.org/10.1136/bmj.i4919.
Knoll T, Omar MI, Maclennan S, Hernández V, Canfield S, Yuan Y, et al. Key steps in conducting systematic reviews for underpinning clinical practice guidelines: methodology of the European association of urology. Eur Urol. 2018;73. https://doi.org/10.1016/j.eururo.2017.08.016.
Jeremy Howick IC (James LLPGTGCHALIMBPHTOG and MH). The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14. https://doi.org/10.1186/1471-2288-14-135.
Ma J, Liu W, Hunter A, Zhang W. Performing meta-analysis with incomplete statistical information in clinical trials. BMC Med Res Methodol. 2008;8. https://doi.org/10.1186/1471-2288-8-56.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21. https://doi.org/10.1002/sim.1186.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74. https://doi.org/10.1111/biom.12817.
Abaza R, Martinez O, Murphy C, Urkmez A, Davis J. Adoption of single-port robotic prostatectomy: two alternative strategies. J Endourol. 2020;34. https://doi.org/10.1089/end.2020.0425.
Abou Zeinab M, Beksac AT, Ferguson E, Kaviani A, Kaouk J. Transvesical versus extraperitoneal single-port robotic radical prostatectomy: a matched-pair analysis. World J Urol. 2022;40. https://doi.org/10.1007/s00345-022-04056-6.
Agarwal DK, Sharma V, Toussi A, Viers BR, Tollefson MK, Gettman MT, et al. Initial experience with da Vinci single-port robot-assisted radical prostatectomies. Eur Urol. 2020. https://doi.org/10.1016/j.eururo.2019.04.001.
Bassett JC, Salibian S, Crivellaro S. Single-port Retzius-sparing robot-assisted radical prostatectomy: feasibility and early outcomes. J Endourol. 2021;36:620–25.
Harrison R, Stifelman M, Billah M, Zaifman J, Lulla T, Sanchez De La Rosa R, et al. Propensity-score matched analysis between extraperitoneal single port and intraperitoneal multiport radical prostatectomy: a single-institutional experience. Urology. 2022;165. https://doi.org/10.1016/j.urology.2022.02.027.
Huang MM, Patel HD, Wainger JJ, Su ZT, Becker REN, Han M, et al. Comparison of perioperative and pathologic outcomes between single-port and standard robot-assisted radical prostatectomy: an analysis of a high-volume center and the pooled world experience. Urology. 2021. https://doi.org/10.1016/j.urology.2020.08.046.
Kim JE, Kaldany A, Lichtbroun B, Singer EA, Jang TL, Ghodoussipour S, et al. Single-port robotic radical prostatectomy: short-term outcomes and learning curve. J Endourol. 2022; 36. https://doi.org/10.1089/end.2021.0885.
Kim KH, Ahn HK, Kim M, Yoon H. Technique and perioperative outcomes of single-port robotic surgery using the da Vinci SP platform in urology. Asian J Surg. 2023;46. https://doi.org/10.1016/j.asjsur.2022.05.128.
Koukourikis P, Alqahtani AA, Han WK, Rha KH, Pure single‐port Retzius‐sparing robot‐assisted radical prostatectomy with the da Vinci SP: Initial experience and technique description. BJUI Compass. 2022. https://doi.org/10.1002/bco2.131.
Lenfant L, Sawczyn G, Aminsharifi A, Kim S, Wilson CA, Beksac AT, et al. Pure single-site robot-assisted radical prostatectomy using single-port versus multiport robotic radical prostatectomy: a single-institution comparative study. Eur Urol Focus. 2021. https://doi.org/10.1016/j.euf.2020.10.006.
Lenfant L, Garisto J, Sawczyn G, Wilson CA, Aminsharifi A, Kim S, et al. Robot-assisted radical prostatectomy using single-port perineal approach: technique and single-surgeon matched-paired comparative outcomes. Eur Urol. 2021. https://doi.org/10.1016/j.eururo.2020.12.013.
Moschovas MC, Loy D, Patel E, Sandri M, Moser D, Patel V. Comparison between intra- and postoperative outcomes of the da Vinci SP and da Vinci Xi robotic platforms in patients undergoing radical prostatectomy. J Robot Surg. 2023. https://doi.org/10.1007/s11701-023-01563-5.
Ng CF, Teoh JYC, Chiu PKF, Yee CH, Chan CK, Hou SSM, et al. Robot-assisted single-port radical prostatectomy: a phase 1 clinical study. Int J Urol. 2019;26. https://doi.org/10.1111/iju.14044.
Noh T Il, Kang YJ, Shim JS, Kang SH, Cheon J, Lee JG, et al. Single-port vs multiport robot-assisted radical prostatectomy: a propensity score matching comparative study. J Endourol. 2022;36. https://doi.org/10.1089/end.2021.0660.
Ramos-Carpinteyro R, Ferguson EL, Chavali JS, Geskin A, Kaouk J. First 100 cases of transvesical single-port robotic radical prostatectomy. Asian J Urol. 2023. https://doi.org/10.1016/j.ajur.2022.12.005.
Saidian A, Fang AM, Hakim O, Magi-Galluzzi C, Nix JW, Rais-Bahrami S. Perioperative outcomes of single vs multi-port robotic assisted radical prostatectomy: a single institutional experience. J Urol. 2020;204. https://doi.org/10.1097/JU.0000000000000811.
Vigneswaran HT, Schwarzman LS, Francavilla S, Abern MR, Crivellaro S. A comparison of perioperative outcomes between single-port and multiport robot-assisted laparoscopic prostatectomy. Eur Urol. 2020;77. https://doi.org/10.1016/j.eururo.2020.03.031.
Abou Zeinab M, Ramos R, Ferguson EL, Okhawere KE, Iarajuli T, Wilder S, et al. Single port versus multiport robot-assisted simple prostatectomy: a multi-institutional study from the single-port advanced research consortium (SPARC). Urology. 2023;176:94–101.
Palacios DA, Kaouk J, Abou Zeinab M, Ferguson EL, Abramczyk E, Wright HC, et al. Holmium laser enucleation of the prostate vs transvesical single-port robotic simple prostatectomy for large prostatic glands. Urology. 2023. https://doi.org/10.1016/j.urology.2023.07.020.
Talamini S, Lai A, Palmer C, van de Walle G, Zuberek M, Crivellaro S. Surgical treatment of benign prostatic hyperplasia: thulium enucleation versus single‐port transvesical robotic simple prostatectomy. BJUI Compass. 2023;4:549–55.
Bertolo R, Garisto J, Bove P, Mottrie A, Rocco B. Perioperative outcomes between single-port and “multi-port” robotic assisted radical prostatectomy: where do we stand? Urology. 2021. https://doi.org/10.1016/j.urology.2021.06.005.
Francavilla S, Veccia A, Dobbs RW, Zattoni F, Vigneswaran HT, Antonelli A, et al. Radical prostatectomy technique in the robotic evolution: from da Vinci standard to single port—a single surgeon pathway. J Robot Surg. 2022. https://doi.org/10.1007/s11701-021-01194-8.
Kaouk JH, Haber GP, Autorino R, Crouzet S, Ouzzane A, Flamand V, et al. A novel robotic system for single-port urologic surgery: first clinical investigation. Eur Urol. 2014;66:1033–43.
Kaouk J, Valero R, Sawczyn G, Garisto J. Extraperitoneal single-port robot-assisted radical prostatectomy: initial experience and description of technique. BJU Int. 2020. https://doi.org/10.1111/bju.14885.
Crivellaro S. In favor of extraperitoneal robotic radical prostatectomy: back to the future through a single-port approach. J Endourol. 2021. https://doi.org/10.1089/end.2021.0294.
Abou Zeinab M, Kaviani A, Ferguson E, Beksac AT, Schwen Z, Gill B, et al. Single-port transvesical versus open simple prostatectomy: a perioperative comparative study. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00566-x.
Li K, Yu X, Yang X, Huang J, Deng X, Su Z, et al. Perioperative and oncologic outcomes of single-port vs multiport robot-assisted radical prostatectomy: a meta-analysis. J Endourol. 2022. https://doi.org/10.1089/end.2021.0210.
Fahmy O, Fahmy UA, Alhakamy NA, Khairul-Asri MG. Single-port versus multiple-port robot-assisted radical prostatectomy: a systematic review and meta-analysis. J Clin Med. 2021. https://doi.org/10.3390/jcm10245723.
Hinojosa-Gonzalez DE, Roblesgil-Medrano A, Torres-Martinez M, Alanis-Garza C, Estrada-Mendizabal RJ, Gonzalez-Bonilla EA, et al. Single-port versus multiport robotic-assisted radical prostatectomy: a systematic review and meta-analysis on the da Vinci SP platform. Prostate. 2022. https://doi.org/10.1002/pros.24296.
Kaouk J, Aminsharifi A, Wilson CA, Sawczyn G, Garisto J, Francavilla S, et al. Extraperitoneal versus transperitoneal single port robotic radical prostatectomy: a comparative analysis of perioperative outcomes. J Urol. 2020. https://doi.org/10.1097/JU.0000000000000700.
Wilson CA, Aminsharifi A, Sawczyn G, Garisto JD, Yau R, Eltemamy M, et al. Outpatient extraperitoneal single-port robotic radical prostatectomy. Urology. 2020. https://doi.org/10.1016/j.urology.2020.06.029.
Abou Zeinab M, Beksac AT, Ferguson E, Kaviani A, Moschovas MC, Joseph J, et al. Single-port extraperitoneal and transperitoneal radical prostatectomy: a multi-institutional propensity-score matched study. Urology. 2023;171:140–45.
Soputro NA, Ferguson EL, Ramos-Carpinteyro R, Chavali JS, Kaouk J. The transition toward opioid-sparing outpatient radical prostatectomy: a single institution experience with three contemporary robotic approaches. Urology. 2023;180:140–50. https://doi.org/10.1016/j.urology.2023.07.001.
Ganesan V, Steinberg RL, Garbens A, Trivedi H, Sorokin I, Roehrborn CA, et al. Single-port robotic-assisted simple prostatectomy is associated with decreased post-operative narcotic use in a propensity score matched analysis. J Robot Surg. 2022;16. https://doi.org/10.1007/s11701-021-01236-1.
Noël J, Moschovas MC, Sandri M, Bhat S, Rogers T, Reddy S, et al. Patient surgical satisfaction after da Vinci® single-port and multi-port robotic-assisted radical prostatectomy: propensity score-matched analysis. J Robot Surg. 2022. https://doi.org/10.1007/s11701-021-01269-6.
Lenfant L, Corrigan D, Beksac AT, Schwen Z, Kaouk J. Learning curve analysis of single-port robot-assisted extraperitoneal prostatectomy using the cumulative sum (CUSUM) method. BJU Int. 2021;128. https://doi.org/10.1111/bju.15588.
Kim M, Yoo D, Pyo J, Cho W. Clinicopathological significances of positive surgical resection margin after radical prostatectomy for prostatic cancers: a meta-analysis. Medicina. 2022;58. https://doi.org/10.3390/medicina58091251.
Asimakopoulos AD, Annino F, Mugnier C, Lopez L, Hoepffner JL, Gaston R, et al. Robotic radical prostatectomy: analysis of midterm pathologic and oncologic outcomes: a historical series from a high-volume center. Surg Endosc. 2021;35. https://doi.org/10.1007/s00464-020-08177-0.
Menon M, Bhandari M, Gupta N, Lane Z, Peabody JO, Rogers CG, et al. Biochemical recurrence following robot-assisted radical prostatectomy: analysis of 1384 patients with a median 5-year follow-up. Eur Urol. 2010;58. https://doi.org/10.1016/j.eururo.2010.09.010.
Ficarra V, Rossanese M, Gilante M, Foti M, Macchione L, Mucciardi G, et al. Retzius-sparing vs. standard robot-assisted radical prostatectomy for clinically localised prostate cancer: a comparative study. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00625-3.
Liu J, Zhang J, Yang Z, Liu Q, Zhang W, Qing Z, et al. Comparison of Retzius-sparing and conventional robot-assisted laparoscopic radical prostatectomy regarding continence and sexual function: an updated meta-analysis. Prostate Cancer Prostatic Dis. 2022;25. https://doi.org/10.1038/s41391-021-00459-5.
Chang Y, Xu W, Lu X, Zhou Y, Ji M, Xiao YT, et al. Robotic perineal radical prostatectomy: initial experience with the da Vinci Si robotic system. Urol Int. 2020;104. https://doi.org/10.1159/000505557.
Vitarelli A, De Rienzo G, Pagliarulo V, Lucia L, Minafra P, Vulpi M, et al. Robot-assisted radical perineal prostatectomy: our experience with a new Retzius-sparing approach. Eur Urol Open Sci. 2020;19. https://doi.org/10.1016/s2666-1683(20)34195-1.
Tuğcu V, Ekşi M, Sahin S, Çolakoğlu Y, Simsek A, Evren İ, et al. Robot-assisted radical perineal prostatectomy: a review of 95 cases. BJU Int. 2020;125. https://doi.org/10.1111/bju.15018.
Abou Zeinab M, Beksac AT, Corse T, Talamini S, Morgantini L, Kaviani A, et al. The multi-institutional experience in single-port robotic transvesical simple prostatectomy for benign prostatic hyperplasia management. J Urol. 2022;208. https://doi.org/10.1097/JU.0000000000002692.
Kordan Y, Canda AE, Köseoğlu E, Balbay D, Laguna MP, de la Rosette J. Robotic-assisted simple prostatectomy: a systematic review. J Clin Med. 2020;9:1798.
Lenfant L, Sawczyn G, Kim S, Aminsharifi A, Kaouk J. Single-institution cost comparison: single-port versus multiport robotic prostatectomy. Eur Urol Focus. 2021. https://doi.org/10.1016/j.euf.2020.06.010.
Moschovas MC, Helman T, Bhat S, Sandri M, Rogers T, Noel J, et al. Does type of robotic platform make a difference in the final cost of robotic-assisted radical prostatectomy? J Robot Surg. 2022;16. https://doi.org/10.1007/s11701-021-01359-5.
Acknowledgements
None.
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
Conceptualization and supervision: RA, SC; Study screening, article selection, data extraction, and risk of bias assessment: AF, AP; Data analysis and interpretation: FD, CM; Manuscript drafting: FD, CM, AF; Statistical review: AC; Scientific and grammatical review: AA, CDN, MDS. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Jhiad Kaouk: Speaker, Intuitive; Consultant to Method AI and VTI; Research sponsorship PI, Medtronics
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Franco, A., Ditonno, F., Manfredi, C. et al. Single port robot-assisted radical and simple prostatectomy: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis (2024). https://doi.org/10.1038/s41391-024-00787-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-024-00787-2
This article is cited by
-
Implementation of single-port robotic urologic surgery: experience at a large academic center
Journal of Robotic Surgery (2024)