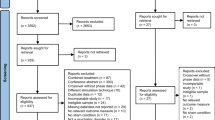
Abstract
More than any other brain region, the prefrontal cortex (PFC) gives rise to the singularity of human experience. It is therefore frequently implicated in the most distinctly human of all disorders, those of mental health. Noninvasive neuromodulation, including electroconvulsive therapy (ECT), repetitive transcranial magnetic stimulation (rTMS), and transcranial direct current stimulation (tDCS) among others, can—unlike pharmacotherapy—directly target the PFC and its neural circuits. Direct targeting enables significantly greater on-target therapeutic effects compared with off-target adverse effects. In contrast to invasive neuromodulation approaches, such as deep-brain stimulation (DBS), noninvasive neuromodulation can reversibly modulate neural activity from outside the scalp. This combination of direct targeting and reversibility enables noninvasive neuromodulation to iteratively change activity in the PFC and its neural circuits to reveal causal mechanisms of both disease processes and healthy function. When coupled with neuronavigation and neurophysiological readouts, noninvasive neuromodulation holds promise for personalizing PFC neuromodulation to relieve symptoms of mental health disorders by optimizing the function of the PFC and its neural circuits. ClinicalTrials.gov Identifier: NCT03191058.
Similar content being viewed by others
Introduction
The brain is an electrochemical organ. When neurons fire, the flux of ions through ion channels generates E-fields, which can be measured from the scalp via electroencephalography. In addition to generating E-fields, the brain responds to E-fields applied exogenously, as in the case of our oldest somatic therapy in psychiatry still in use today, electroconvulsive therapy (ECT). With advances in engineering, we now have a wide array of devices that can apply E-fields, and other forms of energy, to change brain function. Together, these tools to apply energy to the brain are referred to as neuromodulation devices. Tools that require surgical implantation (e.g., deep-brain stimulation (DBS), vagus nerve stimulation (VNS)) are referred to as “invasive neuromodulation,” while those that apply energy through the scalp (e.g., ECT, transcranial magnetic stimulation (TMS), and transcranial current stimulation (tCS)) are referred to as “noninvasive neuromodulation” [1]. Noninvasive neuromodulation is particularly useful in reversibly altering activity in targeted prefrontal cortex (PFC) networks in healthy volunteers as well as clinical populations, and thus is the focus of our paper.
As a family of interventions, neuromodulation devices are distinct from pharmacological therapies in several respects. While pharmacological agents target receptors and alter downstream regulatory mechanisms, neuromodulation devices target membrane potentials in axons and dendrites. Unlike medications that are distributed systemically throughout the body and brain, neuromodulation devices can target specific brain structures with varying degrees of spatial resolution, depending on the specific device used. Also, unlike medications, which reach a steady state in the blood, neuromodulation devices can apply stimulation at specific times relative to ongoing neural activity, yielding the ability to target specific phases of neural oscillations. This temporal specificity allows neuromodulation to be started and stopped abruptly, whereas medications require time to build up to a steady state and also a washout period, depending on the half-life of the specific agent.
Their unparalleled spatial and temporal specificity makes neuromodulation devices particularly useful in the study of specific brain areas, such as the PFC. Because neuromodulation can change brain function, it provides a means to probe brain/behavior relationships and move us from correlation to causation. This allows us to discover and validate causal mechanisms underlying mental disorders. It also allows us to translate knowledge of the neural basis of disease into circuit-based treatments. Given the central role of PFC in a variety of mental health disorders, a number of noninvasive neuromodulation tools have been developed to target the PFC therapeutically, and this has led to a number of Food and Drug Administration (FDA) approvals, such as TMS for the treatment of major depressive disorder (MDD), obsessive–compulsive disorder (OCD), and as an adjuvant to aid smoking cessation.
Recent advances in neural engineering have provided a broadening array of new tools to noninvasively alter brain function that extends the limits of their spatial and temporal resolution. With this proliferation in noninvasive neuromodulation tools, a review of their differences in their stimulation depth and focality, and their mechanisms of action are particularly timely. Here we review the state of the art with each and discuss the unique advantages and drawbacks in their ability to target PFC circuitry to treat mental disorders.
Electroconvulsive therapy (ECT)
Brief description, history, indications, and uses of ECT
Inducing seizures to treat mental illness dates back to at least the sixteenth century when Paracelsus used camphor to induce seizures in hopes of relieving the symptoms of mental illness [2]. ECT was developed as a safer, more reliable replacement for drugs as a means to induce therapeutic generalized seizures. It was first used in Rome in 1938 by Cerletti and Bini to treat a man who was thought to suffer from schizophrenia [3]. Although initially used to treat all forms of severe mental illness, ECT is most effective for mood disorders and catatonia. In its current form, ECT is the therapeutic, serial induction of generalized seizures under brief generalized anesthesia and neuromuscular blockade (paralysis) using alternating current applied through scalp electrodes. In the United States, a typical course is 6–12 treatments given thrice weekly over 2–4 weeks. Initially classified as “higher risk” class III medical devices, ECT devices were reclassified in 2018 as “moderate risk” class II devices when used in “the treatment of catatonia or a severe major depressive episode (MDE) associated with MDD or bipolar disorder in patients age 13 years and older who are treatment-resistant or who require a rapid response due to the severity of their psychiatric or medical condition” [4]. ECT is also used to treat manic and mixed episodes of bipolar disorder, schizoaffective disorder, treatment-resistant schizophrenia, and refractory-status epilepticus.
ECT and the PFC
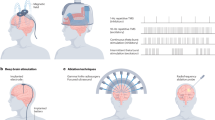
Although the immediate goal of ECT is to induce a generalized seizure, different scalp-electrode placements result in significant differences in the distribution of current density throughout the brain [5]. The original ECT scalp-electrode placement was bitemporal (BT); however, additional placements were developed in an attempt to optimize the balance of therapeutic and adverse cognitive effects. Current practice is largely limited to three placements—BT, right unilateral (RUL), and bifrontal (BF) (Fig. 1a–c). Most but not all research suggests that BF and RUL placements, by shunting current away from the dominant temporal lobe, are associated with less adverse cognitive effects than BT [6,7,8,9,10,11,12]. Magnetic resonance image (MRI)-derived realistic human head models reveal the distribution of the E-field generated by ECT stimulation based on the anatomical features of an individual’s head, the current amplitude of the ECT stimulus pulse, and the electrode placement [13]. Although all three electrode placements generate strong E-field distributions that include the PFC, only BF was designed, on the basis of human neuropsychological research, to improve mood by targeting the PFC while focusing current away from the temporal lobes to minimize adverse effects on learning and memory [14, 15]. The intended prefrontal activation and relative sparing of the temporal lobes of BF ECT has been confirmed by functional neuroimaging [5], and the memory-sparing effects have been supported by most studies comparing BF with BT ECT. While BF does focus more on the induced E-field in the PFC, it remains a relatively broad and diffuse field that still stimulates a number of off-target brain regions (Fig. 1c).
Realistic head modeling was used to simulate the electricl field strength and distribution for different ECT electrode placements and MST coil configurations. a Bitemporal ECT, b right unilateral ECT, c bifrontal ECT, d focal electrically administered seizure therapy (FEAST), e circular coil MST, f twin coil MST, E-field distribution on the cortex is shown relative to neuronal depolarization threshold, Eth [48]. ECT was simulated at current amplitude of 800 mA and an ultrabrief 0.3-ms pulse width; MST was simulated at 100% maximum stimulator output. The color map is saturated at an upper limit of 3 E/Eth for good visibility of the spatial distribution.
Most of the clinical research literature on the PFC and ECT comprises studies of individuals being treated for a MDE largely unipolar MDD, but often including some individuals with bipolar depression. Where MDD is specified below, the sample consisted exclusively of unipolar individuals with a MDE, otherwise the sample was either mixed unipolar/bipolar or unspecified in the report. There is a smaller, but significant PFC-related clinical literature on studies of individuals with schizophrenia. We will briefly review these studies followed by a discussion of investigation into experimental forms of ECT.
ECT and the PFC in individuals with major depressive episodes
We first discuss studies of brain regional structure and function followed by studies of brain network connectivity. Some of the earliest functional imaging studies of the therapeutic mechanism of ECT used quantitative EEG to assess brain regional activity before, during, and after a course of ECT. ECT was reported to induce a significant short-term enhancement in delta and theta power in patients with MDD receiving either BT or RUL ECT at either a high or a low dose [16, 17]. This enhanced slow-wave activity, which was noted in the PFC, was associated with the antidepressant effect of ECT and was no longer present at a 2-month post-course follow-up. Specifically, the increase in delta power in PFC from baseline to the end of ECT course was significantly greater in ECT responders than nonresponders, irrespective of electrode placement. Interestingly, low-dosage RUL ECT, which has since been proven to be therapeutically ineffective, induced significantly weaker increases in delta and theta power compared with the effective forms of ECT—high-dose RUL and low- and high-dose BT. The authors concluded that intense seizure expression in prefrontal regions resulting in enhanced prefrontal slow-wave activity rather than the extent of bilateral seizure generalization may be essential to the antidepressant effect of ECT. Using whole-scalp magnetoencephalographic recordings, Heikman et al. reported similar findings [18]. In “depressive inpatients” receiving high-dose RUL or BF ECT for MDD, they found that treatment induced an increase in theta activity in the left frontal cortex that correlated with antidepressant efficacy, irrespective of electrode placement.
Reports of slowed PFC activity with ECT were further supported by a positron emission tomography (PET) study of regional cerebral glucose metabolism in individuals with MDD receiving BT ECT [19]. The authors reported extensive, significant decreases in regional cerebral metabolic rate for glucose after the ECT course that included PFC regions—bilateral superior frontal lobe and bilateral dorsolateral and medial prefrontal cortices. Although they did not report a relationship to antidepressant response, they concluded that the antidepressant mechanism of ECT may involve suppression of functional brain activity, particularly in the PFC. Similarly, Qi et al., using functional magnetic resonance image (fMRI), observed that antidepressant response to a course of RUL or mixed RUL/BT ECT associated with decreased brain activity in the PFC [20]. Parallel to diminished prefrontal metabolic activity post ECT, one structural MRI study found a transient 1.4% volume reduction in the dorsolateral prefrontal cortex (DLPFC) 1 week after a course of BT ECT [21]. Interestingly, Miskowiak et al. found that a single BT ECT treatment session decreased fMRI-measured neural activity to unpleasant vs. pleasant pictures within a predefined medial PFC (mPFC) region that showed the greatest response in the most depressed MDD patients [22]. The authors concluded that “modulation of medial prefrontal hyperactivity during encoding of negative affective information may be a common mechanism of distinct biological depression treatments”.
It is important to note that the hypothesis that the antidepressant mechanism of ECT involves decreased PFC activity seems to contradict resting-state functional MRI (rsfMRI) studies demonstrating lower activity in the dorsal PFC of individuals with depression compared with healthy volunteers. Although the reason for this apparent contradiction is unclear, the short delay, typically 1–7 days, between ECT treatment and post-treatment imaging is a possible explanation. Reduced PFC activity may be an acute effect of ECT that indicates therapeutically adequate seizures, but is a correlate or indirect causal factor rather than a direct causal factor in the antidepressant mechanism of ECT. For example, the antidepressant mechanism of ECT may involve an acute suppression of PFC glucose metabolism, which may evolve into an eventual enhancement or normalization of PFC metabolism. This is consistent with the aforementioned enhanced PFC slow-wave activity observed during and within 1 week following an ECT course, which was associated with the antidepressant effect of ECT, but was no longer present at 2 months post ECT course. Longer-term, prospective post-ECT imaging studies are needed to test this hypothesis.
Changes in PFC function have also been related to the adverse cognitive effects of ECT. Nobler et al. reported that greater post-ECT regional cerebral blood flow (rCBF) reductions in certain PFC regions were linked to greater retrograde amnesia for autobiographical events 1 week and 2 months following an ECT course for MDD, irrespective of BT or RUL electrode placement [23]. This differed from rCBF reductions in left superior and posterior temporal regions and the right frontal pole, which were associated with verbal anterograde amnesia, regardless of electrode placement.
In contrast to studies reporting decreased prefrontal brain activity with ECT, other studies using various functional imaging techniques have reported evidence of augmented prefrontal neural activity with ECT for a MDE. Hirano et al. used task-related functional near-infrared spectroscopy (NIRS) to show that reductions in bilateral frontal cortex concentrations of oxy-hemoglobin ([oxy-Hb]) compared with healthy controls during a letter verbal fluency task were improved by a course of BT ECT [24]. They also reported that the decrease in depression severity with ECT correlated significantly with an increase in [oxy-Hb] in right VLPFC. Similarly, a proton magnetic resonance spectroscopy (1H-MRS) study of the left DLPFC in individuals with melancholic MDD found reduced glutamate/glutamine levels pre-RUL ECT relative to those of age-matched controls that correlated negatively with depression severity and normalized post-RUL ECT [25]. Using fMRI, two studies found evidence of increased local neural activity of PFC regions following a course of ECT: in dorsomedial PFC (dmPFC) with BT ECT for a MDE [26] and in bilateral dmPFC, right DLPFC, and bilateral orbitofrontal cortex (OFC), after BF ECT for MDD [27]. The discrepancy between these findings suggesting enhanced post-ECT PFC neural activity and the aforementioned findings suggesting decreased PFC neural activity is unlikely to be explained by differences in the timing of post-ECT imaging as the post-ECT assessment window was generally also within a week of the last treatment in these studies. Rather, the most likely explanation for the varied findings is the diversity of methods of measuring PFC neural activity and the generally small number of individuals in each study, which limits the reliability of findings.
Studies of network connectivity in individuals with MDD receiving ECT have mostly used fMRI to assess resting-state functional connectivity (rsFC); however, two studies that used diffusion MRI to detect structural connectivity are worth noting. Lyden et al. used diffusion tensor imaging to examine changes in connectivity following a course of predominantly RUL ECT [28]. They found that patients with a MDE showed changes in white matter microstructure in dorsal frontolimbic circuits, including the anterior cingulum, forceps minor, and left superior longitudinal fasciculus, that connect PFC to other cortical and to limbic regions, suggestive of post-ECT increased fiber integrity in dorsal frontolimbic pathways involved in mood regulation. Tsolaki et al. used diffusion MRI and probabilistic tractography to examine subcallosal cingulate (SCC)–mPFC connectivity in individuals with a MDE receiving predominantly RUL ECT [29]. The authors found that SCC–mPFC structural connectivity was lower bilaterally in ECT responders than nonresponders before treatment and that responders had lower connectivity between SCC and right mPFC, but not between SCC and left mPFC after a course of ECT indicating a possibly lateralized effect of RUL ECT. The authors concluded that SCC–mPFC connectivity could be a biomarker of therapeutic outcome relevant for treatment selection.
fMRI studies of rsFC of individuals in a MDE receiving a course of ECT have generally asked the following questions: (1) Can neural activity in particular brain networks at baseline predict ECT response? (2) Does ECT have effects on network connectivity? (3) If ECT has effects on network connectivity, how are these related to therapeutic and adverse effects? We summarize below studies that have implicated network activity or connectivity of PFC regions. van Waarde et al. reported that the baseline activity of a network centered in dmPFC that included DLPFC, OFC, and posterior cingulate cortex, predicted post-ECT course remission with a sensitivity of 84% and specificity of 85% in individuals with MDD receiving a course of either RUL or BT ECT [30]. They also found that another network centered in the anterior cingulate cortex and including DLPFC, sensorimotor cortex, parahippocampal gyrus, and midbrain, showed a sensitivity of 80% and a specificity of 75% in predicting post-ECT remission. They concluded that resting-state networks may have potential as prognostic biomarkers to guide personalized treatment decisions. Sun et al. in a study of predominantly RUL ECT examined if pre-ECT whole-brain functional connectivity (FC) could predict depressive rating scale score changes and remission status after ECT in individuals with a MDE [31]. They found that the networks with the best predictive performance of ECT response were anticorrelated FC networks, which predicted post-ECT depression remission with 76% accuracy. These FC networks were concentrated in the prefrontal and temporal cortices and subcortical nuclei, and included the inferior frontal, superior frontal, superior temporal, and inferior temporal gyri, as well as the basal ganglia and thalamus.
Most studies of the effects of ECT on PFC connectivity have shown increases in connectivity, with some notable exceptions that found decreases or both. Increased intranetwork connections have been reported for the executive control network after BF ECT for MDD, with nodal analysis showing increased functional connection between the dmPFC and lateral PFC that correlated with antidepressant response [32]. BF ECT is reported to also enhance rsFC of the cognitive emotion regulation network (ERN) in individuals with MDD [33]. Within the ERN, and with respect to the PFC, FC between the PCC and left ventrolateral PFC (VLPFC) and the right angular gyrus and the left VLPFC increased after ECT, and negatively correlated with the changes in the Delayed Memory of Auditory Verbal Learning Test (AVLT)–Delayed Recall, indicating increased FC associated with worsening cognition. Increased degree centrality, a voxelwise measurement of whole-brain FC, was found for bilateral dmPFC, right DLPFC, left OFC, and right OFC after BF ECT, which correlated with improvement in anhedonia scores [27]. Moreno-Ortega et al. reported increased anticorrelation rsFC between DLPFC–subgenual anterior cingulate cortex (sgACC) and between DLPFC and anterior DMN that correlated with improvement in depressive symptoms over a course of RUL ECT for a MDE [34]. Cano et al. examined changes in FC at multiple time points before, during, and after a course of BT ECT for MDD [35]. They observed a decrease in limbic–prefrontal (amygdala–DLPFC) rsFC following the first BT ECT treatment, which then predicted a later, end-of-course increase in limbic–prefrontal rsFC, which in turn predicted antidepressant response. Studies finding an overall decrease in rsFC involving PFC reported attenuated rsFC between subgenual cingulate (SCC) and bilateral hippocampus, bilateral temporal pole, and vmPFC with BF ECT that did not correlate with antidepressant response [36], as well as decreased global FC of the left DLPFC (Brodmann areas 44, 45, and 46) with BT ECT with a marked improvement in symptoms, but no reported correlation with response [37].
ECT and the PFC in individuals with schizophrenia
Two-proton magnetic resonance spectroscopy (1H-MRS) studies compared the effects of ECT with pharmacotherapy in individuals with schizophrenia. Gan et al. compared BT ECT with atypical antipsychotic drug treatment and observed a reduction in NAA/creatine ratio (NAA/Cr) in the left PFC and left thalamus compared with healthy controls at baseline that was reversed by both BT ECT and drugs [38]. However, only the BT ECT group had a significant elevation in NAA/Cr post course compared with baseline, suggesting to the authors that BT ECT may have a greater neuroprotective effect on the PFC than antipsychotic drugs. Xia et al. compared BT ECT plus atypical antipsychotic drug treatment with atypical antipsychotic drug treatment alone and observed that the γ-aminobutyric acid (GABA) level in the medial prefrontal lobe was reduced at baseline compared with healthy controls and increased significantly in the BT ECT plus drug group but not in the drug-alone group [39]. A change in GABA level, however, did not correlate with clinical response.
Two fMRI studies of rsFC found rsFC changes with ECT, one a study of individuals with schizophrenia and the other a study that combined individuals with schizophrenia and individuals with MDD. Huang et al. compared BT ECT plus atypical antipsychotic drug treatment with atypical antipsychotic drug treatment alone in individuals with schizophrenia and observed an increase in global FC density in the dmPFC only in the BT ECT plus drug group [40]. Thomann et al. studied the effects of RUL ECT on rsFC in individuals with MD and schizophrenia and found an ECT-associated reduction in rsFC between right amygdala and the right temporo-parietal junction, the mPFC, the left posterior insula, and the right DLPFC that was not diagnosis-specific and did not correlate with clinical response [41]. These findings suggest a largely lateralized decrease in frontolimbic connectivity with RUL ECT.
Experimental forms of ECT and the PFC
Experimental forms of ECT have insufficient efficacy and safety data and require further study in randomized, controlled trials before becoming mainstream clinical practice. All are designed to minimize the adverse cognitive effects of ECT while maintaining its robust therapeutic effect. Focal electrically administered seizure therapy (FEAST) is a form of ECT that, as shown in Fig. 1d, attempts to spatially focus the E-field to initiate seizure activity in the right PFC [42], though as with other forms of ECT, the field still spreads broadly [13], and is more sensitive to individual differences in anatomy than less focal paradigms [43]. FEAST has shown promise recently through a nonrandomized, open-label trial that showed an antidepressant effect commensurate with RUL ECT and adverse cognitive effects that were numerically, though not significantly, less than RUL ECT [44]. Frontomedial (FM) is an experimental electrode placement designed to achieve better focality in the PFC than FEAST. Realistic head modeling demonstrates that FM can indeed target mPFC and frontal pole with less spread to other cortical areas than FEAST [45].
Individualized low-amplitude seizure therapy (iLAST) proposes several improvements over conventional ECT [46, 47]. While standard ECT uses two relatively large electrodes spaced widely apart on the scalp, leading to a nonfocal E-field distribution in the brain, iLAST uses an array of smaller electrodes to selectively target different regions of the brain. Standard ECT uses a high and fixed current amplitude (800–900 mA), which is much higher than needed to induce a seizure [48]. iLAST uses a dosing strategy whereby the stimulus is titrated by the current amplitude rather than by the stimulus duration or frequency, as done in ECT clinical practice [46]. The intended result is a current amplitude that is individualized to patient head anatomy to elicit a seizure at a lower amplitude and with a more focal electrode array that will expose less of the brain to a high-energy E-field.
Transcranial electric stimulation therapy (TEST), previously called nonconvulsive electrotherapy, involves BF electric brain stimulation at a dose below seizure threshold applied exactly as standard ECT, under anesthesia, with a FDA-cleared ECT device that can deliver a range of subseizure threshold stimulation doses [49]. Since TEST, like standard ECT, delivers pulses at a high current amplitude, it induces a brain E-field distribution like that of BF ECT (Fig. 1c). However, since the frequency and duration of the stimulus are very low compared with ECT, the stimulus lacks the energy to induce a generalized seizure. Therefore, rather than aiming to decrease adverse cognitive effects through lower amplitude and/or more focal stimulation, TEST intends to limit adverse cognitive effects by eliminating the seizure. This approach challenges the long-standing theory of ECT therapeutic mechanism, which holds that the generalized seizure is necessary for the beneficial effect of ECT. With a significantly lower dose stimulus than ECT and lacking generalized seizure induction, the rationale for the possible therapeutic effect is based on its BF stimulation and the robust evidence implicating frontal lobe regions and frontolimbic neural circuits in depression and in antidepressant treatment response [50,51,52,53,54]. As will be discussed later, this evidence also underlies the choice of stimulation site for the only other FDA-approved brain stimulation therapy for treatment-resistant depression (TRD)—rTMS. Randomized clinical trials showing that low-dose RUL ECT, in contrast to bilateral forms of ECT, can elicit a generalized seizure without being therapeutic, indicate that regional distribution of the stimulus within the brain is critical to antidepressant effect [10, 55]. To date, evidence for the safety and efficacy of TEST as an antidepressant treatment is limited to an open-label clinical trial with 11 completing participants with TRD who had thrice-weekly treatments [49]. In this study, there were no serious adverse events, and adverse cognitive effects were less than typically observed for standard BF ECT. TRD response and remission rates (73 and 55%, respectively) were comparable to those typically observed in ECT trials. Sham or ECT-controlled trials are needed to adequately assess the safety and antidepressant efficacy of TEST.
In sum, standard ECT approaches have broad effects throughout the brain, including changes in PFC activity and connectivity that are linked to therapeutic and adverse cognitive effects. Experimental approaches attempt to refine and personalize these effects toward improving the efficacy/safety profile of ECT. Further studies investigating how modulation of the PFC and its neural circuits affects this efficacy/safety profile are critical to the improvement and wider acceptance of this highly effective but underused procedure [56].
Magnetic seizure therapy (MST)
Brief description, history, indications, and uses of MST
First used in humans in 2000, MST, like the experimental forms of ECT, was developed to match the antidepressant efficacy of ECT without the significant adverse cognitive effects of ECT [57]. Like ECT, MST occurs under general anesthesia; however, unlike ECT, MST elicits a generalized seizure with a device that does not deliver an electric current, but rather creates rapidly alternating magnetic fields that can induce an electric current and thereby a seizure in the cerebral cortex [57]. As standard rTMS devices cannot generate sufficiently strong magnetic fields to reliably induce seizures, MST is performed with a customized rTMS stimulator with additional charging units enabling higher frequencies of stimulation. The site of stimulation is either over the vertex of the head with a single, circular coil (Fig. 1e), or with twin round coils (double-cone MST) placed on the vertex or over midline PFC (Fig. 1f). In contrast to electric current, magnetic fields can penetrate the head with no resistance from structures overlying the brain, allowing much greater control over the site of seizure initiation and the extent of cortical stimulation (Fig. 1e, f). This superficial targeting could potentially eliminate unwanted off-target adverse effects, such as amnesia, that are typical of standard ECT. Studies so far suggest that MST does induce less cognitive impairment than ECT [58,59,60]. A randomized double-blind controlled trial of ECT vs. MST in TRD found similar antidepressant efficacy in both groups, though it was underpowered to detect small differences [61], supporting earlier open-label controlled trials that also found comparable efficacy [62,63,64]. A randomized, double-blind confirmatory efficacy study is currently underway at the time of this writing to establish whether MST is noninferior to ECT in terms of antidepressant efficacy.
MST and the PFC
Realistic human head models of brain E-field distribution have confirmed that MST produces less intense and more superficial stimulation of the PFC than standard or experimental forms of ECT (Fig. 1) [45]. MST’s effects on the PFC have been illustrated by pre-/post-course PET imaging of individuals with TRD. Approximately 4 days after a course of dual-cone MST, Hoy et al. observed increased relative glucose metabolism in the basal ganglia, OFC, medial frontal cortex, and DLPFC; however, changes in regional metabolism did not distinguish responders from nonresponders [65]. Kayser et al. found enhanced metabolism compared with baseline after at least 7 days post-vertex MST in superior frontal gyrus, medial frontal gyrus, and orbital frontal cortex bilaterally, with increased metabolism in the right frontal cortex distinguishing responders from nonresponders [66]. The discrepancy in PET findings post MST (increased glucose metabolism) and post ECT (decreased glucose metabolism) can likely be explained by differences in time course. In the post-ECT PET studies, scans occurred within 1 week of the end of the ECT course, while increases in glucose metabolism post MST were observed only when scans occurred greater than 1 week post course, on average 30.3 days. A smaller MST subgroup of three participants was scanned within a week of the end of the MST course (average = 4.7 days), and at that point, only reductions in glucose metabolism were observed. It is also possible that MST and ECT have distinct mechanisms of action, given their differences in strength of the electric field and the resultant cognitive side effects. Further studies with larger sample sizes are needed to clarify MST effects on the PFC and its relationship to clinical response.
Transcranial magnetic stimulation (TMS)
Brief description, history, indications, and uses of TMS
Noninvasive magnetic stimulation of the human cortex using a TMS device was first reported in 1985 [67]. TMS uses powerful, rapidly alternating magnetic fields delivered through a magnetic coil held over the head to induce an electric current in cortical brain regions. TMS was initially used to investigate brain regional function and connectivity, as well as the pathophysiology of neuropsychiatric disorders. rTMS, the delivery of a repetitive train of magnetic pulses, has developed over decades as a treatment for a number of neuropsychiatric disorders. The effects of rTMS on the brain depend on both the site of stimulation and the frequency of stimulation. Depending on the frequency of rTMS, stimulation can have excitatory or inhibitory effects on cortical neurons. Stimulation above ~1 Hz enhances brain excitability, while at and below 1 Hz, it typically inhibits excitability.
The FDA has cleared the use and marketing of certain devices that deliver rTMS for various neuropsychiatric disorders or conditions. Approval began in 2008 with treatment-resistant (one failed, adequate trial of antidepressant medication) unipolar MDD, followed by migraine pain in 2013, OCD in 2018, and smoking addiction in 2020. The most commonly used magnetic coil is in the shape of a figure-8 and is most often placed over the left DLPFC in treating depression (Fig. 2). The left DLPFC was chosen based on accessibility and on functional imaging studies of brain areas involved in antidepressant response to ECT [68]. The TRD protocol originally approved by the FDA involves 3000 pulses of 10-Hz stimulation delivered through a figure-8-shaped coil to the left DLPFC over 37.5 min. A typical rTMS course is 4–6 weeks of 5 days per week treatment. Hesed (H) coils that can reach slightly deeper into the brain and are much less focal than the figure-8 coil [69] have also been approved by the FDA. Another important recent development in rTMS TRD therapy was the FDA clearance in 2019 of a newer rTMS method called intermittent theta burst stimulation (iTBS). The FDA approved an iTBS protocol, based on a noninferiority comparison to standard rTMS [70] that involves 5-Hz bursts of three pulses at 50 Hz for a total of 600 pulses given over ~3 min or around one-tenth of the usual duration of an rTMS session for TRD. Recent work has sought to accelerate response even further by giving all sessions over the course of 5 days [71]. The results of randomized controlled trials will be important to demonstrate whether these promising open results will be replicated, and whether response rates and durability of response are better than conventional treatment protocols.
The E-field distributions are normalized to their respective maximum values to allow for contrast of the relative focality among stimulation modalities. The absolute E-field (logarithmic) scale indicates the approximate range of field strengths induced by tCS (~0.5 V/m), TMS (~100 V/m), and ECT (~200 V/m) at typically therapeutic doses.
rTMS is mostly used to treat TRD and has several important advantages over ECT—it does not require a seizure or anesthesia and does not cause adverse cognitive effects. However, its efficacy for TRD is much less than ECT with rTMS vs. sham-effect sizes around 0.55 compared with 0.91 for ECT vs. sham [72, 73]. In addition to its approved uses, rTMS is being investigated for use in many neuropsychiatric disorders, including anxiety disorders, bipolar disorder, substance-use disorders, autism, schizophrenia, and cognitive disorders.
TMS and the PFC
The development of TMS as an investigative and therapeutic tool in neurology and psychiatry began in the early days of functional imaging of the brain. TMS targeting therefore benefitted from considerably more knowledge of the brain regions and circuits involved in disorders, therapeutic response, and adverse effects than did the development of ECT. Realistic human head models confirm that rTMS over the left DLPFC is able to generate an E-field in the left DLPFC that exceeds the neural activation threshold and is far more focal than that of ECT (Fig. 2). However, TMS can only directly stimulate superficial cortical tissue due to a limited maximum depth of ~3 cm from the scalp that can be reached by magnetic fields generated by the commonly used figure-8 coil. An additional centimeter of depth can be attained using deep TMS (dTMS) H coils.
TMS and the PFC in individuals with MDD
Accumulating brain imaging research of MDD and other psychiatric disorders reveals that these disorders are associated with functional and structural abnormalities of brain circuits rather than abnormalities of specific brain regions [74, 75]. Research on TMS effects on the PFC and the relationship of the PFC to rTMS treatment response has therefore mainly focused on investigating brain circuits, often frontolimbic circuits, their connectivity, and changes in connectivity with rTMS. This focus is consistent with the view that the characteristics and function of a cortical region can be understood only in the context of its connections with other structures [76] and with the definition of the PFC, across mammalian species, as that region of the cerebral cortex that receives projections from the mediodorsal nucleus of the thalamus [77]. We review and summarize this research below, emphasizing the largest body of literature, which pertains to circuit connectivity in individuals before and after rTMS treatment for MDD.
Multiple studies have found that DLPFC connectivity is associated with treatment response to left DLPFC rTMS. Higher baseline FC between the left DLPFC and the right cerebellum measured by SPECT [78] and between the left DLPFC and the striatum measured by rsfMRI [79] predicted treatment response to left DLPFC rTMS treatment for MDD. Eshel et al. found that higher DLPFC global rsFC following a course of rTMS correlated with treatment response [80].
Another important body of research has focused on FC of the left DLPFC stimulation site to the sgACC, which has been implicated as a possibly hyperactive node in neural circuitry underlying MDD [81]. The clinical efficacy of rTMS for MDD has been reported to depend on the extent of negatively correlated (anticorrelated) rsFC between the left DLPFC stimulation site and the SCC [82,83,84]. The Stanford Accelerated Intelligent Neuromodulation Therapy trial used rsfMRI to individually target the region of the left DLPFC most anticorrelated with the sgACC in each participant and achieved an unusually high MDD remission rate of 86% with twenty sessions of iTBS rTMS over 4 days [84].
TMS and the PFC in individuals with OCD and smoking addiction
Targeting with rTMS for OCD differs from that of rTMS for MDD. The initial FDA-approved coil for OCD was a H coil that enables deeper and broader brain penetration of the TMS electromagnetic stimulation into the brain [85]. This type of dTMS coil (H7 coil) resembles a double-cone coil and was designed to directly target the mPFC and ACC [86]. A figure-8 coil that targets the dmPFC has also been FDA- approved for rTMS OCD treatment. fMRI study of imaging correlates of treatment response has revealed that dmPFC–striatal rsFC is implicated in OCD response. In a treatment course of right and left dmPFC stimulation within each session at 10 Hz for 20 daily sessions over 4 weeks, responders were found to have hyperconnectivity between dmPFC and caudate at baseline relative to healthy controls, which normalized after treatment [87]. Another dTMS H coil received FDA approval for smoking cessation in 2020. This coil targets the PFC and the insula in treatments performed daily, 5 days a week for 3 weeks, followed by an additional 3 sessions once a week for 3 weeks.
Experimental forms of rTMS and the PFC
In contrast to ECT, experimental forms of rTMS intend to boost the modest therapeutic efficacy of rTMS while maintaining its minimal adverse-effect profile. One approach is to enhance the individualization and precision of spatial targeting of PFC regions that are most salient in circuits controlling therapeutic effects. For TRD, this PFC region may be the dmPFC rather than the standard left DLPFC [88]. rTMS targeting the dmPFC shows promise as an alternate form of rTMS for TRD. Its antidepressant effects may be bimodal based on the extent of anhedonic symptoms, with prominent anhedonia predicting nonresponse. Anhedonic nonresponders have shown lower baseline connectivity through a classical reward circuit comprising ventral tegmentum, striatum, and a ventromedial PFC region on rsfMRI [89]. Further rsfMRI studies have revealed that therapeutic response is associated with enhanced dmPFC–thalamic connectivity and decreased SCC cortex–caudate connectivity following 20 sessions (4 weeks) of treatment [90].
Transsynaptic TMS (tsTMS) is another approach to more precise spatial targeting, but with a view to deeper, subcortical targets within a circuit. tsTMS uses connectivity-based targeting to reach brain regions and circuits that are beyond the superficial depth of standard figure-8 or H coils. Thus, tsTMS holds potential for modulating brain circuits in ways only thought possible with invasive techniques like DBS. rsfMRI can be used to assess the rsFC of potential cortical stimulation sites to deeper brain regions, such as the SCC, and to select the superficial cortical site with the greatest rsFC to the subcortical region of interest for a specific individual.
The ability of 10-Hz rTMS to modulate activity in deeper brain regions within a circuit monosynaptically connected to the prefrontal region directly stimulated has been proven through studies using PET to show modulated dopamine release in the ipsilateral caudate, ACC, and OFC, through rTMS of the left DLPFC [91, 92]. Importantly, Dowdle et al. added a sham condition that enabled sensory features of stimulation while preventing entry of the magnetic field into the brain [93]. Using single-pulse TMS interleaved with fMRI, they showed that left DLPFC stimulation caused enhanced blood oxygen level-dependent (BOLD) signal in subcortical, anatomically connected regions, including anterior cingulate, caudate, and thalamus, with active, but not sham TMS. Weigand et al. illustrated the therapeutic potential of targeting deeper brain regions by individualizing the 10- or 20-Hz rTMS stimulation site to a region in the DLPFC region with highest connectivity to SCC (BA 25), which has been reliably modulated only by DBS [82]. Stimulating with a standard figure-8 coil over the individualized left DLPFC region resulted in an antidepressant response that varied directly with the degree of stimulation site—SCC anticorrelation connectivity.
Synchronized transcranial magnetic stimulation (sTMS) and closed-loop TMS are techniques that aim to boost therapeutic efficacy through precise and individualized temporal targeting. sTMS uses rotating neodymium magnets positioned close to the head in the sagittal line to provide low-field sinusoidal waveform TMS through magnetic induction in frontal and central cortical regions [94, 95]. sTMS stimulates at an intensity below the neural firing threshold and is timed to be delivered at each individual alpha frequency as determined by EEG prior to treatment. Six weeks of sTMS resulted in a significant improvement in depression-scale score in a subgroup of per-protocol (PP) completers with MDD but not in the larger intent-to-treat sample of a double-blind sham-controlled treatment trial [94]. Of interest, changes over treatment course in alpha current source density at anterior and central midline regions, including PFC regions, correlated with changes in depressive symptoms in the active but not the sham sTMS group [96].
Closed-loop TMS goes a step beyond the temporal targeting of sTMS by administering pulses simultaneously with neural feedback that can modify the TMS stimulus in real time. The intention is to enhance TMS therapeutic efficacy by individualizing treatment through synchronizing TMS pulses with instantaneous brain oscillations, thereby boosting TMS-induced plasticity. In a feasibility trial with individuals with TRD, Zrenner et al. found that alpha-synchronized rTMS of left DLPFC is feasible, safe, and has specific single-session neuromodulatory effects, including reduced resting-state alpha activity in left DLPFC and increased TMS-induced beta oscillations over frontocentral EEG channels [97].
Another promising approach to enhancing rTMS efficacy is to enrich the context of stimulation by simultaneously administering psychotherapy. Based on neuroimaging data suggesting that rTMS and psychotherapy target similar mood-regulating networks, Donse et al. administered cognitive behavioral therapy (CBT) simultaneous with 10-Hz left DLPFC or 1-Hz right DLPFC rTMS and boosted the remission rate to 56% in a large, open-label naturalistic study [98]. In a small, proof-of-concept study, Neacsiu et al. took this approach a step further by individualizing the left PFC rTMS stimulation site to target the neural circuit most engaged during a baseline fMRI task designed to reveal the neurocircuitry involved in a specific type of CBT [99]. This method, termed cognitive paired associative stimulation, aims to induce a Hebbian-like synergistic interaction between the plasticity induced by the TMS and the neural circuitry activated in response to the CBT [100, 101].
There is significant research on TMS and its effects on the PFC in other disorders, including schizophrenia and cognitive disorders. TMS is an investigative and potential therapeutic tool for schizophrenia. For example, rTMS has been used to ameliorate the notoriously treatment-resistant negative symptoms of schizophrenia. Using fMRI, Brady et al. found that disrupted connectivity between the right DLPFC and the midline cerebellar node in the default mode network (DMN) predicted negative symptom severity in individuals with schizophrenia [102]. They then modulated the network with 5 days of twice-daily iTBS rTMS to the cerebellar midline, resulting in improved network connectivity and decreased negative symptom severity.
Recent research suggests that TMS can enhance both healthy and disordered cognition by engaging circuits that include the PFC [101]. The DLPFC plays an important role in circuits underlying working memory [103] and relational memory binding for long-term memory (LTM) [104]. Wang et al. applied 5-Hz rTMS for 10 min over the left DLPFC, which is important in controlling relational memory binding, prior to an associative LTM task and observed changes in memory circuit excitability and connectivity with fMRI in healthy older adults [105]. They showed that increased local PFC excitability can have measurable influences on upstream semantic representations in earlier temporal memory regions of a memory circuit. In a further, sham-controlled trial, 25 pulses of 5-HZ rTMS over the left DLPFC given during a delayed response alphabetization working memory task resulted in increased accuracy relative to sham in a group of healthy younger and older adults [106]. In older adults with amnestic mild cognitive impairment, often a harbinger of Alzheimer’s disease, ten daily sessions over 2 weeks of 1500 pulses of 10-Hz rTMS over the right DLPFC led to decreased FC within the DMN that correlated with improved AVLT-recognition scores in a sham-controlled trial [107].
Transcranial current stimulation
tCS uses scalp electrodes to deliver sub-action-potential-threshold current to the brain [108]. Two common forms of tCS are transcranial direct current stimulation (tDCS), which delivers constant current, and transcranial alternating current stimulation (tACS), which delivers charged–balanced sinusoidal current. The mechanism of tDCS is thought to be a polarity-dependent shift in the neuronal membrane voltage caused by the externally applied constant E-field, thus biasing neuronal excitability [109]. On the other hand, tACS is thought to engage the resonance dynamics of neural networks and entrain oscillatory activity [110]. The neuronal effects of these techniques therefore differ from those of rTMS, which directly induces neuronal actional potentials. When performed with bilateral DLPFC electrode placement, the induced E-field distribution of tCS resembles that of BF ECT, but with strengths two orders of magnitude lower (Fig. 2). Numerous studies, including several randomized controlled trials, have been conducted to investigate the efficacy of tDCS for the treatment of MDD. Overall, bilateral DLPFC (left anodal, right) cathodal tDCS, was found to be effective in the treatment of depression, albeit with a small-to-moderate effect size [111]. One potential source of clinical variability is the variable E-field distribution in the brain across individuals with different head anatomy. A post hoc analysis showed that in depressed patients receiving 2-mA tDCS, the negative-effect score was inversely correlated with the simulated E-field strength in bilateral ACC and DLPFC [112]. This result motivates individualizing tDCS electrode montage and dose to achieve more targeted stimulation and more consistent clinical response. The work on tACS for depression treatment is less developed. A preliminary trial used 10-Hz, 40-Hz, and sham tACS, delivered at 4-mA peak to peak through bilateral DLPFC anode (F3 and F4 EEG sites) and vertex cathode in patients with MDD [113]. At the 2-week follow-up period, the 10-Hz tACS group had more responders compared with the 40-Hz and sham groups. However, the groups did not separate at the completion of the treatment at 4 weeks. There was, however, a reduction in resting-state EEG alpha power over the left frontal regions for the 10-Hz tACS group post treatment [113].
Transcutaneous vagus nerve and trigeminal nerve stimulation (TNS)
Two other classes of techniques that rely on electrical stimulation are VNS and TNS. The implantable version of VNS is currently FDA-approved for the treatment of depression and epilepsy [114]. Noninvasively, the vagus nerve can be accessed via the cervical branch by placing bipolar electrodes at the neck [115], or via the auricular branch by placing electrodes on the concha areas of the ear [116]. A device for transcutaneous cervical VNS was approved by the US FDA for the treatment of cluster headaches [117] and an electroauricular device was approved for the treatment of opioid withdrawal. In Europe, several devices have been cleared to treat epilepsy, pain, and depression. Fang et al. [118] used transcutaneous auricular VNS (taVNS) in patients with MDD in a nonrandomized, sham-controlled study. Stimulation was applied for 30 min twice daily at a maximally tolerable current amplitude (4–6 mA), with 20-Hz sinusoidal waveform. After 4 weeks of treatment, patients in the active group showed greater reduction of Hamilton Depression Scale (HAM-D) score compared with the sham group. Compared with sham stimulation, active taVNS showed a decrease in FC between the DMN and anterior insula and parahippocampus, and increase in connectivity between the DMN and OFC and precuneus that is associated with the HAM-D reduction [118].
External trigeminal nerve stimulation (eTNS) uses scalp electrodes placed on bilateral forehead to target the V1 branches of the trigeminal nerve. Current is delivered at 120 Hz, 250-µs pulse width, 30-s on/off duty cycle, and up to 6-mA peak amplitude. eTNS has been used for the treatment of drug-resistant epilepsy [119], MDD [120], and migraine [121]; one eTNS device is FDA-cleared for treatment of attention- deficit hyperactivity disorder. Neuroimaging studies showed that eTNS can induce a decrease in fMRI BOLD response in the right anterior cingulate cortex (rACC) [121], and reduce metabolic activity in OFC and rACC as measured by FDG-PET [122]. However, given that the BF electrode placement and peak current amplitude in eTNS are similar compared with other transcranial stimulation modalities, the relative effects of the induced E-field on the cranial nerve and the underlying PFC have not been characterized.
Photobiomodulation
Transcranial laser stimulation (TLS), or low-level light therapy, is a form of photobiomodulation that uses light from lasers or light-emitting diodes (LEDs) to modulate brain function. This is achieved with low-power, high radiant exposure, far-red to near-infrared wavelength light, which is absorbed by the enzyme cytochrome c oxidase, a photoacceptor that catalyzes oxygen consumption in mitochondrial respiration process [123, 124]. In an in vivo animal study [125], TLS was delivered using 600-nm-wavelength LEDs to the PFC of rats, cortical oxygen consumption was measured using fiber-optic fluorometric oxygen quenching. A dose-dependent increase in cortical oxygen consumption by TLS was observed, and there was also facilitated PFC-based extinction memory in the rats treated with low-dose TLS. In humans, an increase in oxygenated hemoglobin with a decrease in deoxygenated hemoglobin concentrations was measured with NIRS following stimulation using a 1064-nm laser applied to bilateral medial frontal regions [126]. The hemodynamic changes sustained for several minutes after the initial 10-min stimulation.
TLS of the PFC has been used in several cognitive and therapeutic applications. Barrett and Gonzalez-Lima conducted the first controlled study in healthy human participants by applying a 1064-nm laser, with 0.25 W/cm2 irradiance, over the right frontal pole (Fp2 EEG site) for 8 min. Compared with sham stimulation, the active group showed an improvement in performance on the psychomotor vigilance and delayed match-to-sample tasks immediately post stimulation, and reported a higher positive-to-negative effect 2 weeks after the session [127]. Extension studies performed by Blanco et al. using similar stimulation parameters found improved executive function as assessed by the Wisconsin Card Sorting task [128], and PFC-mediated, rule-based category learning [129] in healthy volunteers. There is also preliminary clinical evidence suggesting the efficacy of TLS for treatment of MDD. A pilot study conducted by Schiffer et al. administered a single, 4-min TLS treatment using 810-nm, 0.25 W/cm2 irradiance light, targeted over left or right DLPFC (F3/F4 EEG sites) in ten patients with MDD and anxiety. Two weeks post treatment, six out of ten patients achieved remission on the HAM-D, and seven out of ten achieved remission on the Hamilton Anxiety Rating Scale [130]. Another study that combined TLS with attention bias modification training in 51 adult participants with elevated depressive symptoms, showed that with the right prefrontal target, those with stronger negative attention bias prior to TLS, benefit more from the stimulation [131].
Transcranial ultrasound (TUS)
TUS uses acoustic waves at frequencies beyond the human hearing range (20 kHz to 20 MHz), traversing through superficial head tissue, including the skull, to modulate brain activity. TUS can be delivered in a focused or unfocused manner, and the dose depends on acoustic frequency and power density. At low intensities (frequency up to ~1 MHz and 200 mW/cm2), focused ultrasound (LIFUS) can be used to modulate neuronal excitability via mechanical vibrations that produce a change in neuronal membrane potential without damage or tissue heating [132, 133]. Compared with electromagnetic or optical-based stimulation, LIFUS has the advantage of reaching deep-brain regions with relatively high spatial precision. Ai et al. demonstrated that LIFUS of the primary motor cortex and left head of the caudate during 3T and 7T fMRI can induce a BOLD signal in the respective regions [134, 135]. Sanguinetti et al. [136] applied 500-kHz LIFUS to the right inferior frontal gyrus (rIFG), an area implicated in emotional regulation and depression [137]. Sonification for up to 2 min increased self-reported global affect (visual analog mood scale) in healthy participants. There was also a corresponding decrease in rsFC between the rIFG and the subgenual cortex, OFC, inferior prefrontal gyrus, dorsal anterior cingulate cortex, and entorhinal cortex, regions of the DMN [136]. Unfocused ultrasound has also been found to alter subjective mood. In a double-blind, sham-controlled crossover study, Hameroff et al. used a 8-MHz, 15-s, unfocused ultrasound to target the posterior frontal cortex in patients with chronic pain. There was a significant improvement in the self-reported global effect for up to 40 min post active treatment compared with sham [138].
Future directions and clinical implications
The ability of noninvasive neuromodulation tools to target regions of the PFC has been crucial in establishing causal brain/behavior relationships, allowing the field to interrogate specific networks and their role in mediating higher cognitive and affective functions of the PFC in health and disease. In this way, noninvasive neuromodulation tools are particularly useful in identifying and validating circuit-based targets for subsequent therapeutic intervention. Moreover, because these tools can exert lasting changes in the functioning of PFC networks, they are extremely promising as therapeutic interventions that can translate emerging targets into circuit-guided therapies. Indeed, the FDA clearance of TMS applied to the DLPFC to treat depression in 2008 represented the clinical translation of decades of research implicating the DLPFC in depression and in antidepressant response. The ability to translate circuit discovery into circuit-guided treatments has the potential to be transformative in the care of patients with mental illnesses where PFC circuits are implicated.
As exciting as this potential is, there remain challenges in realizing the full potential of noninvasive neuromodulation to transform care. Questions remain as to how to select the patients most likely to respond (including identifying objective biomarkers to characterize patient heterogeneity), and how to optimize and individualize the dosage. Each of these tools differ in terms of their depth of penetration, degree of focality, impact on neural activity acutely and chronically, and the parameters that define their dosage. Dosing of neuromodulation is particularly complex, in comparison with dosing of psychopharmacology, and includes the spatial distribution of the induced fields, the temporal aspects of the stimulation paradigm, and the state of the brain during stimulation. Aspects of the delivered dose can be rigorously quantified by documenting the electrode/coil size and placement, coil shape/orientation/placement, and parameters of stimulation (frequency, pulse shape, train duration, etc.), but studies do not always report all of these parameters posing a challenge to replication. Even when all of these parameters are documented as recommended in reporting standards [139], replication is still challenging because the dose that the patient actually receives is further impacted by individual variation in anatomy, which determines the distribution of the E-fields induced in the brain, and individual variation in neural dynamics and brain state at the time of stimulation, which determines the effect of the delivered field on neural activity. Increasingly studies are employing E-field modeling to capture the impact of anatomy on what is actually being targeted, and neurophysiological measures to capture the impact on neural activity.
An exciting and relatively unexplored potential of noninvasive neuromodulation is the prospect of targeting neurodevelopmental processes to alter trajectories of PFC development and ultimately improve mental health outcomes later in life. Given that major mental illnesses are increasingly understood as neurodevelopmental disorders that result from pathological processes that begin early in life while the PFC is still developing, often years before symptoms manifest, early intervention to interrupt these processes in the development of the PFC could offer hope for preventing later manifestations of mental illness. Challenges to this approach include the need to identify neurodevelopmental targets that could be amenable to intervention via neuromodulation (such as neuroplasticity, excitation/inhibition balance, etc.) and the need to identify the sensitive periods in development when intervention may be selectively beneficial, among others. Nevertheless, the payoff could be high given that pediatric patients should lack the cumulative effects of decades of chronic illness and treatment exposures that adults have.
As we look into the future, advances in neuroengineering continue to yield new tools that push the envelope of what can be accomplished with noninvasive neuromodulation tools, and the pace of that advancement has been accelerated by the NIH BRAIN Initiative [140]. Next-generation TMS devices enable user control of the pulse shape with the prospect of enhanced efficacy and cell-type-specific targeting [141, 142]. Next-generation seizure therapy devices induce more focal fields with the prospect of sparing memory [143]. Next-generation drug delivery devices allow focal drug delivery deep in the brain using ultrasonic uncaging of nanospheres carrying pharmacological payloads [144]. Next-generation intervention paradigms are increasingly multimodal and individualized [145]. One could argue that the potential of these tools is limited mainly by our own imaginations, and of course, by the laws of physics.
Funding and disclosure
This work was supported by the Intramural Research Program of the National Institute of Mental Health (NIMH) (Grant no. 1ZIAMH002955-05 to SHL). The views expressed in this article do not necessarily represent the views of the National Institutes of Health, the Department of Health and Human Services, or the United States Government. ZDD and SHL are inventors on a patent on TMS coil design, assigned to Columbia University, and receive no royalties. WTR has no disclosures.
References
Deng Z-D, McClintock SM, Oey NE, Luber B, Lisanby SH. Neuromodulation for mood and memory: from the engineering bench to the patient bedside. Curr Opin Neurobiol. 2015;30:38–43.
Mowbray RM. Historical aspects of electric convulsant therapy. Scott Med J. 1959;4:373–8.
Endler NS. The origins of electroconvulsive-therapy (ECT). Convul Ther. 1988;4:5–23.
Food and Drug Administration, HHS. Neurological Devices; Reclassification of Electroconvulsive Therapy Devices; Effective Date of Requirement for Premarket Approval for Electroconvulsive Therapy Devices for Certain Specified Intended Uses. Final order. Fed Regist. 2018;83:66103–24.
Blumenfeld H, McNally KA, Ostroff RB, Zubal IG. Targeted prefrontal cortical activation with bifrontal ECT. Psychiatry Res. 2003;123:165–70.
Halliday AM, Davison K, Browne MW, Kreeger LC. A comparison of the effects on depression and memory of bilateral E.C.T. and unilateral E.C.T. to the dominant and non-dominant hemispheres. Br J Psychiatry. 1968;114:997–1012.
Weiner RD, Rogers HJ, Davidson JR, Squire LR. Effects of stimulus parameters on cognitive side effects. Ann N. Y Acad Sci. 1986;462:315–25.
Letemendia FJ, Delva NJ, Rodenburg M, Lawson JS, Inglis J, Waldron JJ, et al. Therapeutic advantage of bifrontal electrode placement in ECT. Psychol Med. 1993;23:349–60.
Bailine SH, Rifkin A, Kayne E, Selzer JA, Vital-Herne J, Blieka M, et al. Comparison of bifrontal and bitemporal ECT for major depression. Am J Psychiatry. 2000;157:121–3.
Sackeim HA, Prudic J, Devanand DP, Nobler MS, Lisanby SH, Peyser S, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral electroconvulsive therapy at different stimulus intensities. Arch Gen Psychiatry. 2000;57:425–34.
Kellner CH, Knapp R, Husain MM, Rasmussen K, Sampson S, Cullum M, et al. Bifrontal, bitemporal and right unilateral electrode placement in ECT: randomised trial. Br J Psychiatry. 2010;196:226–34.
Su L, Jia Y, Liang S, Shi S, Mellor D, Xu Y. Multicenter randomized controlled trial of bifrontal, bitemporal, and right unilateral electroconvulsive therapy in major depressive disorder. Psychiatry Clin Neurosci. 2019;73:636–41.
Lee WH, Deng Z-D, Kim TS, Laine AF, Lisanby SH, Peterchev AV. Regional electric field induced by electroconvulsive therapy in a realistic finite element head model: influence of white matter anisotropic conductivity. Neuroimage. 2012;59:2110–23.
Inglis J. Shock, surgery and cerebral asymmetry. Br J Psychiatry. 1970;117:143–8.
Abrams R, Taylor MA. Anterior bifrontal ECT: a clinical trial. Br J Psychiatry. 1973;122:587–90.
Sackeim HA, Luber B, Katzman GP, Moeller JR, Prudic J, Devanand DP, et al. The effects of electroconvulsive therapy on quantitative electroencephalograms. Relatsh Clin outcome Arch Gen psychiatry. 1996;53:814–24.
Luber B, Nobler MS, Moeller JR, Katzman GP, Prudic J, Devanand DP, et al. Quantitative EEG during seizures induced by electroconvulsive therapy: relations to treatment modality and clinical features. II. Topographic analyses J ECT. 2000;16:229–43.
Heikman P, Tuunainen A, Sailas E, Kuoppasalmi K. Seizures induced by low-dose right unilateral and bifrontal electroconvulsive stimuli. J ECT. 2003;19:189–93.
Nobler MS, Oquendo MA, Kegeles LS, Malone KM, Campbell CC, Sackeim HA, et al. Decreased regional brain metabolism after ECT. Am J Psychiatry. 2001;158:305–8.
Qi S, Abbott CC, Narr KL, Jiang R, Upston J, McClintock SM, et al. Electroconvulsive therapy treatment responsive multimodal brain networks. Hum brain Mapp. 2020;41:1775–85.
Jorgensen A, Magnusson P, Hanson LG, Kirkegaard T, Benveniste H, Lee H, et al. Regional brain volumes, diffusivity, and metabolite changes after electroconvulsive therapy for severe depression. Acta Psychiatr Scand. 2016;133:154–64.
Miskowiak KW, Macoveanu J, Jorgensen MB, Ott CV, Stottrup MM, Jensen HM, et al. Effect of electroconvulsive therapy on neural response to affective pictures: a randomized, sham-controlled fMRI study. Eur Neuropsychopharmacol. 2018;28:915–24.
Nobler MS, Sackeim HA. Neurobiological correlates of the cognitive side effects of electroconvulsive therapy. J ECT. 2008;24:40–5.
Hirano J, Takamiya A, Yamagata B, Hotta S, Miyasaka Y, Pu S, et al. Frontal and temporal cortical functional recovery after electroconvulsive therapy for depression: a longitudinal functional near-infrared spectroscopy study. J Psychiatr Res. 2017;91:26–35.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B. Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychological Med. 2003;33:1277–84.
Bai T, Wei Q, Zu M, Xie W, Wang J, Gong-Jun J, et al. Functional plasticity of the dorsomedial prefrontal cortex in depression reorganized by electroconvulsive therapy: Validation in two independent samples. Hum Brain Mapp. 2019;40:465–73.
Zhang T, He K, Bai T, Lv H, Xie X, Nie J, et al. Altered neural activity in the reward-related circuit and executive control network associated with amelioration of anhedonia in major depressive disorder by electroconvulsive therapy. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110193.
Lyden H, Espinoza RT, Pirnia T, Clark K, Joshi SH, Leaver AM, et al. Electroconvulsive therapy mediates neuroplasticity of white matter microstructure in major depression. Transl Psychiatry. 2014;4:e380.
Tsolaki E, Narr KL, Espinoza R, Wade B, Hellemann G, Kubicki A, et al. Subcallosal cingulate structural connectivity differs in responders and nonresponders to electroconvulsive therapy. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:10–9.
van Waarde JA, Scholte HS, van Oudheusden LJ, Verwey B, Denys D, van Wingen GA. A functional MRI marker may predict the outcome of electroconvulsive therapy in severe and treatment-resistant depression. Mol Psychiatry. 2015;20:609–14.
Sun H, Jiang R, Qi S, Narr KL, Wade BS, Upston J, et al. Preliminary prediction of individual response to electroconvulsive therapy using whole-brain functional magnetic resonance imaging data. Neuroimage Clin. 2020;26:102080.
Wang J, Wei Q, Yuan X, Jiang X, Xu J, Zhou X, et al. Local functional connectivity density is closely associated with the response of electroconvulsive therapy in major depressive disorder. J Affect Disord. 2018;225:658–64.
Xu J, Wei Q, Bai T, Wang L, Li X, He Z, et al. Electroconvulsive therapy modulates functional interactions between submodules of the emotion regulation network in major depressive disorder. Transl Psychiatry. 2020;10:271.
Moreno-Ortega M, Prudic J, Rowny S, Patel GH, Kangarlu A, Lee S, et al. Resting state functional connectivity predictors of treatment response to electroconvulsive therapy in depression. Sci Rep. 2019;9:5071.
Cano M, Cardoner N, Urretavizcaya M, Martínez-Zalacaín I, Goldberg X, Via E, et al. Modulation of limbic and prefrontal connectivity by electroconvulsive therapy in treatment-resistant depression: a preliminary study. Brain Stimul. 2016;9:65–71.
Argyelan M, Lencz T, Kaliora S, Sarpal DK, Weissman N, Kingsley PB, et al. Subgenual cingulate cortical activity predicts the efficacy of electroconvulsive therapy. Transl Psychiatry. 2016;6:e789.
Perrin JS, Merz S, Bennett DM, Currie J, Steele DJ, Reid IC, et al. Electroconvulsive therapy reduces frontal cortical connectivity in severe depressive disorder. Proc Natl Acad Sci USA. 2012;109:5464–8.
Gan JL, Duan HF, Cheng ZX, Yang JM, Zhu XQ, Gao CY, et al. Neuroprotective effect of modified electroconvulsive therapy for schizophrenia: a proton magnetic resonance spectroscopy study. J Nerv Ment Dis. 2017;205:480–6.
Xia M, Wang J, Sheng J, Tang Y, Li C, Lim K, et al. Effect of electroconvulsive therapy on medial prefrontal gamma-aminobutyric acid among schizophrenia patients: a proton magnetic resonance spectroscopy study. J ECT. 2018;34:227–32.
Huang H, Jiang Y, Xia M, Tang Y, Zhang T, Cui H, et al. Increased resting-state global functional connectivity density of default mode network in schizophrenia subjects treated with electroconvulsive therapy. Schizophr Res. 2018;197:192–9.
Thomann PA, Wolf RC, Nolte HM, Hirjak D, Hofer S, Seidl U, et al. Neuromodulation in response to electroconvulsive therapy in schizophrenia and major depression. Brain Stimul. 2017;10:637–44.
Spellman T, Peterchev AV, Lisanby SH. Focal electrically administered seizure therapy: a novel form of ECT illustrates the roles of current directionality, polarity, and electrode configuration in seizure induction. Neuropsychopharmacology. 2009;34:2002–10.
Deng Z-D, Lisanby SH, Peterchev AV. Effect of anatomical variability on electric field characteristics of electroconvulsive therapy and magnetic seizure therapy: a parametric modeling study. IEEE Trans Neural Syst Rehabil Eng. 2015;23:22–31.
Sahlem GL, McCall WV, Short EB, Rosenquist PB, Fox JB, Youssef NA, et al. A two-site, open-label, non-randomized trial comparing Focal Electrically-Administered Seizure Therapy (FEAST) and right unilateral ultrabrief pulse electroconvulsive therapy (RUL-UBP ECT). Brain Stimul. 2020;13:1416–25.
Lee WH, Lisanby SH, Laine AF, Peterchev AV. Comparison of electric field strength and spatial distribution of electroconvulsive therapy and magnetic seizure therapy in a realistic human head model. Eur Psychiatry. 2016;36:55–64.
Deng Z-D, Lisanby SH, Peterchev AV. Controlling stimulation strength and focality in electroconvulsive therapy via current amplitude and electrode size and spacing: comparison with magnetic seizure therapy. J ECT. 2013;29:325–35.
Peterchev AV, Krystal AD, Rosa MA, Lisanby SH. Individualized low-amplitude seizure therapy: minimizing current for electroconvulsive therapy and magnetic seizure therapy. Neuropsychopharmacology. 2015;40:2076–84.
Deng Z-D, Lisanby SH, Peterchev AV. Electric field strength and focality in electroconvulsive therapy and magnetic seizure therapy: a finite element simulation study. J Neural Eng. 2011;8:016007.
Regenold WT, Noorani RJ, Piez D, Patel P. Nonconvulsive electrotherapy for treatment resistant unipolar and bipolar major depressive disorder: a proof-of-concept trial. Brain Stimul. 2015;8:855–61.
Mayberg HS. Modulating dysfunctional limbic-cortical circuits in depression: towards development of brain-based algorithms for diagnosis and optimised treatment. Br Med Bull. 2003;65:193–207.
Holmes AJ, Pizzagalli DA. Response conflict and frontocingulate dysfunction in unmedicated participants with major depression. Neuropsychologia 2008;46:2904–13.
Price JL, Drevets WC. Neurocircuitry of mood disorders. Neuropsychopharmacology. 2010;35:192–216.
Pizzagalli DA. Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology. 2011;36:183–206.
Liao C, Feng Z, Zhou D, Dai Q, Xie B, Ji B, et al. Dysfunction of fronto-limbic brain circuitry in depression. Neuroscience. 2012;201:231–8.
Sackeim HA, Prudic J, Devanand DP, Kiersky JE, Fitzsimons L, Moody BJ, et al. Effects of stimulus intensity and electrode placement on the efficacy and cognitive effects of electroconvulsive therapy. N. Engl J Med. 1993;328:839–46.
Wilkinson ST, Agbese E, Leslie DL, Rosenheck RA. Identifying recipients of electroconvulsive therapy: data from privately insured Americans. Psychiatr Serv. 2018;69:542–8.
Lisanby SH, Schlaepfer TE, Fisch HU, Sackeim HA. Magnetic seizure therapy of major depression. Arch Gen Psychiatry. 2001;58:303–5.
McClintock SM, Dewind NK, Husain MM, Rowny SB, Spellman TJ, Terrace H, et al. Disruption of component processes of spatial working memory by electroconvulsive shock but not magnetic seizure therapy. Int J Neuropsychopharmacol. 2013;16:177–87.
McClintock SM, Tirmizi O, Chansard M, Husain MM. A systematic review of the neurocognitive effects of magnetic seizure therapy. Int Rev Psychiatry. 2011;23:413–23.
Moscrip TD, Terrace HS, Sackeim HA, Lisanby SH. Randomized controlled trial of the cognitive side-effects of magnetic seizure therapy (MST) and electroconvulsive shock (ECS). Int J Neuropsychopharmacol. 2006;9:1–11.
Fitzgerald PB, Hoy KE, Elliot D, McQueen S, Wambeek LE, Chen L, et al. A pilot study of the comparative efficacy of 100 Hz magnetic seizure therapy and electroconvulsive therapy in persistent depression. Depression Anxiety. 2018;35:393–401.
Daskalakis ZJ, Dimitrova J, McClintock SM, Sun Y, Voineskos D, Rajji TK, et al. Magnetic seizure therapy (MST) for major depressive disorder. Neuropsychopharmacology. 2020;45:276–82.
El-Deeb FA, Gad EA, Kandeel AA, Haiba AA, Fathy SM, Petterson MM, et al. Comparative effectiveness clinical trial of magnetic seizure therapy and electroconvulsive therapy in major depressive disorder. Ann Clin Psychiatry. 2020;32:239–48.
Kayser S, Bewernick BH, Grubert C, Hadrysiewicz BL, Axmacher N, Schlaepfer TE. Antidepressant effects, of magnetic seizure therapy and electroconvulsive therapy, in treatment-resistant depression. J Psychiatr Res. 2011;45:569–76.
Hoy KE, Thomson RH, Cherk M, Yap KS, Daskalakis ZJ, Fitzgerald PB. Effect of magnetic seizure therapy on regional brain glucose metabolism in major depression. Psychiatry Res. 2013;211:169–75.
Kayser S, Bewernick BH, Wagner S, Schlaepfer TE. Effects of magnetic seizure therapy on anterograde and retrograde amnesia in treatment-resistant depression. Depress Anxiety. 2020;37:125–33.
Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1:1106–7.
George MS. Whither TMS: a one-trick pony or the beginning of a neuroscientific revolution? Am J Psychiatry. 2019;176:904–10.
Deng Z-D, Lisanby SH, Peterchev AV. Electric field depth–focality tradeoff in transcranial magnetic stimulation: simulation comparison of 50 coil designs. Brain Stimul. 2013;6:1–13.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391:1683–92.
Cole EJ, Stimpson KH, Bentzley BS, Gulser M, Cherian K, Tischler C, et al. Stanford accelerated intelligent neuromodulation therapy for treatment-resistant depression. Am J Psychiatry. 2020;177:716–26.
Slotema CW, Blom JD, Hoek HW, Sommer IE. Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry. 2010;71:873–84.
Group UER. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23:28–38.
Creutzfeldt OD. Generality of the functional structure of the neocortex. Naturwissenschaften. 1977;64:507–17.
Fuster JM. The prefrontal cortex. 5th ed. Cambridge, MA: Academic press; 2015.
Richieri R, Verger A, Boyer L, Boucekine M, David A, Lançon C, et al. Predictive value of dorso-lateral prefrontal connectivity for rTMS response in treatment-resistant depression: a brain perfusion SPECT study. Brain Stimul. 2018;11:1093–7.
Avissar M, Powell F, Ilieva I, Respino M, Gunning FM, Liston C, et al. Functional connectivity of the left DLPFC to striatum predicts treatment response of depression to TMS. Brain Stimul. 2017;10:919–25.
Eshel N, Keller CJ, Wu W, Jiang J, Mills-Finnerty C, Huemer J, et al. Global connectivity and local excitability changes underlie antidepressant effects of repetitive transcranial magnetic stimulation. Neuropsychopharmacology. 2020;45:1018–25.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–60.
Weigand A, Horn A, Caballero R, Cooke D, Stern AP, Taylor SF, et al. Prospective validation that subgenual connectivity predicts antidepressant efficacy of transcranial magnetic stimulation sites. Biol Psychiatry. 2018;84:28–37.
Fox MD, Buckner RL, White MP, Greicius MD, Pascual-Leone A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol Psychiatry. 2012;72:595–603.
Cash RFH, Cocchi L, Lv J, Fitzgerald PB, Zalesky A. Functional magnetic resonance imaging-guided personalization of transcranial magnetic stimulation treatment for depression. JAMA Psychiatry. 2021;78:337–9.
Carmi L, Tendler A, Bystritsky A, Hollander E, Blumberger DM, Daskalakis J, et al. Efficacy and safety of deep transcranial magnetic stimulation for obsessive-compulsive disorder: a prospective multicenter randomized double-blind placebo-controlled trial. Am J Psychiatry. 2019;176:931–8.
Popa T, Morris LS, Hunt R, Deng Z-D, Horovitz S, Mente K, et al. Modulation of resting connectivity between the mesial frontal cortex and basal ganglia. Front Neurol. 2019;10:587.
Dunlop K, Woodside B, Olmsted M, Colton P, Giacobbe P, Downar J. Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive-compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology. 2016;41:1395–403.
Downar J, Daskalakis ZJ. New targets for rTMS in depression: a review of convergent evidence. Brain Stimul. 2013;6:231–40.
Downar J, Geraci J, Salomons TV, Dunlop K, Wheeler S, McAndrews MP, et al. Anhedonia and reward-circuit connectivity distinguish nonresponders from responders to dorsomedial prefrontal repetitive transcranial magnetic stimulation in major depression. Biol Psychiatry. 2014;76:176–85.
Salomons TV, Dunlop K, Kennedy SH, Flint A, Geraci J, Giacobbe P, et al. Resting-state cortico-thalamic-striatal connectivity predicts response to dorsomedial prefrontal rTMS in major depressive disorder. Neuropsychopharmacology. 2014;39:488–98.
Cho SS, Strafella AP. rTMS of the left dorsolateral prefrontal cortex modulates dopamine release in the ipsilateral anterior cingulate cortex and orbitofrontal cortex. PLoS One. 2009;4:e6725.
Strafella AP, Paus T, Barrett J, Dagher A. Repetitive transcranial magnetic stimulation of the human prefrontal cortex induces dopamine release in the caudate nucleus. J Neurosci. 2001;21:RC157.
Dowdle LT, Brown TR, George MS, Hanlon CA. Single pulse TMS to the DLPFC, compared to a matched sham control, induces a direct, causal increase in caudate, cingulate, and thalamic BOLD signal. Brain Stimul. 2018;11:789–96.
Leuchter AF, Cook IA, Feifel D, Goethe JW, Husain M, Carpenter LL, et al. Efficacy and safety of low-field synchronized transcranial magnetic stimulation (sTMS) for treatment of major depression. Brain Stimul. 2015;8:787–94.
Deng Z-D, Lisanby SH. Electric field characteristics of low-field synchronized transcranial magnetic stimulation (sTMS). Ann Int Conf IEEE Eng Med Biol Soc. 2017;2017:1445–8.
Cook IA, Wilson AC, Corlier J, Leuchter AF. Brain activity and clinical outcomes in adults With depression treated With synchronized transcranial magnetic stimulation: an exploratory study. Neuromodulation. 2019;22:894–7.
Zrenner B, Zrenner C, Gordon PC, Belardinelli P, McDermott EJ, Soekadar SR, et al. Brain oscillation-synchronized stimulation of the left dorsolateral prefrontal cortex in depression using real-time EEG-triggered TMS. Brain Stimul. 2020;13:197–205.
Donse L, Padberg F, Sack AT, Rush AJ, Arns M. Simultaneous rTMS and psychotherapy in major depressive disorder: clinical outcomes and predictors from a large naturalistic study. Brain Stimul. 2018;11:337–45.
Neacsiu AD, Luber BM, Davis SW, Bernhardt E, Strauman TJ, Lisanby SH. On the concurrent use of self-system therapy and functional magnetic resonance imaging-guided transcranial magnetic stimulation as treatment for depression. J ECT. 2018;34:266–73.
Hebb DO. The organization of behavior: a neuropsychological theory. New York: Wiley; 1949.
Luber B, Lisanby SH. Enhancement of human cognitive performance using transcranial magnetic stimulation (TMS). Neuroimage. 2014;85:961–70. Pt 3.
Brady ROJ, Gonsalvez I, Lee I, Öngür D, Seidman LJ, Schmahmann JD, et al. Cerebellar-prefrontal network connectivity and negative symptoms in schizophrenia. Am J Psychiatry. 2019;176:512–20.
Owen AM, Evans AC, Petrides M. Evidence for a two-stage model of spatial working memory processing within the lateral frontal cortex: a positron emission tomography study. Cereb Cortex. 1996;6:31–8.
Blumenfeld RS, Ranganath C. Prefrontal cortex and long-term memory encoding: an integrative review of findings from neuropsychology and neuroimaging. Neuroscientist. 2007;13:280–91.
Wang WC, Wing EA, Murphy DLK, Luber BM, Lisanby SH, Cabeza R, et al. Excitatory TMS modulates memory representations. Cogn Neurosci. 2018;9:151–66.
Beynel L, Davis SW, Crowell CA, Hilbig SA, Lim W, Nguyen D, et al. Online repetitive transcranial magnetic stimulation during working memory in younger and older adults: a randomized within-subject comparison. PLoS One. 2019;14:e0213707.
Cui H, Ren R, Lin G, Zou Y, Jiang L, Wei Z, et al. Repetitive transcranial magnetic stimulation induced hypoconnectivity within the default mode network yields cognitive improvements in amnestic mild cognitive impairment: a randomized controlled study. J Alzheimers Dis. 2019;69:1137–51.
Bikson M, Brunoni AR, Charvet LE, Clark VP, Cohen LG, Deng Z-D, et al. Rigor and reproducibility in research with transcranial electrical stimulation: An NIMH-sponsored workshop. Brain Stimul. 2018;11:465–80.
Stagg CJ, Nitsche MA. Physiological basis of transcranial direct current stimulation. Neuroscientist. 2011;17:37–53.
Ali MM, Sellers KK, Fröhlich F. Transcranial alternating current stimulation modulates large-scale cortical network activity by network resonance. J Neurosci. 2013;33:11262–75.
Fregni F, El-Hagrassy MM, Pacheco-Barris K, Carvalho S, Leite J, Simis M, et al. Evidence-based guidelines and secondary meta-analysis for the use of transcranial direct current stimulation (tDCS) in neurological and psychiatric disorders. Int J Neuropsychopharmacol. 2021;24:256–313.
Suen PJC, Doll S, Batistuzzo MC, Busatto G, Razza LB, Padberg F, et al. Association between tDCS computational modeling and clinical outcomes in depression: data from the ELECT‑TDCS trial. Eur Arch psychiatry Clin Neurosci. 2021;271:101–10.
Alexander ML, Alagapan S, Lugo CE, Mellin JM, Lustenberger C, Rubinow DR, et al. Double-blind, randomized pilot clinical trial targeting alpha oscillations with transcranial alternating current stimulation (tACS) for the treatment of major depressive disorder (MDD). Transl Psychiatry. 2019;9:106.
Johnson RL, Wilson CG. A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res. 2018;11:203–13.
Mourdoukoutas AP, Truong DQ, Adair DK, Simon BJ, Bikson M. High-resolution multi-scale computational model for non-invasive cervical vagus nerve stimulation. Neuromodulation. 2018;21:261–8.
Rong P, Liu J, Wang L, Liu R, Fang J, Zhao J, et al. Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder: a nonrandomized controlled pilot study. J Affect Disord. 2016;195:172–9.
Silberstein SD, Mechtler LL, Kudrow DB, Calhoun AH, McClure C, Saper JR, et al. Non-invasive vagus nerve stimulation for the ACute Treatment of Cluster Headache: findings from the randomized, double-blind, sham-controlled ACT1 study. Headache. 2016;56:1317–32.
Fang J, Rong P, Hong Y, Fan Y, Liu J, wang H, et al. Transcutaneous vagus nerve stimulation modulates default mode network in major depressive disorder. Biol Psychiatry. 2016;79:266–73.
DeGiorgio CM, Soss J, Cook IA, Markovic D, Gornbein J, Murray D, et al. Randomized controlled trial of trigeminal nerve stimulation for drug-resistant epilepsy. Neurology. 2013;80:786–91.
Cook IA, Schrader LM, DeGiorgio CM, Miller PR, Maremont ER, Leuchter AF. Trigeminal nerve stimulation in major depressive disorder: acute outcomes in an open pilot study. Epilepsy Behav. 2013;28:221–6.
Russo A, Tessitore A, Esposito F, Di Nardo F, Silvestro M, Trojsi F, et al. Functional changes of the perigenual part of the anterior cingulate cortex after external trigeminal neurostimulation in migraine patients. Front Neurol. 2017;8:282.
Magis D, D’Ostillo K, Thibaut A, De Pasqua V, Gerard P, Hustinx R, et al. Cerebral metabolism before and after external trigeminal nerve stimulation in episodic migraine. Cephalagia. 2017;37:881–91.
Karu TI, Pyatibrat LV, Kolyakov SF, Afanasyeva NI. Absorption measurements of a cell monolayer relevant to phototherapy: reduction of cytochrome c oxidase under near IR radiation. J Photochem Photobio B. 2005;81:98–106.
Wong-Riley MTT, Liang HL, Eells JT, Chance B, Henry MM, Buchmann E, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005;280:4761–71.
Rojas JC, Bruchey AK, Gonzalez-Lima F. Low-level light therapy improves cortical metabolic capacity and memory retention. J Alzheimers Dis. 2012;32:741–52.
Tian F, Hase SN, Gonzalez-Lima F, Liu H. Transcranial laser stimulation improves human cerebral oxygenation. Lasers Surg Med. 2016;48:343–9.
Barrett DW, Gonzalez-Lima F. Transcranial infrared laser stimulation produces beneficial cognitive and emotional effects in humans. Neuroscience. 2013;230:13–23.
Blanco NJ, Maddox WT, Gonzalez-Lima F. Improving executive function using transcranial infrared laser stimulation. J Neuropsychol. 2017;11:14–25.
Blanco NJ, Saucedo CL, Gonzalez-Lima F. Transcranial infrared laser stimulation improves rule-based, but not information-integration, category learning in humans. Neurobiol Learn Mem. 2017;139:69–75.
Schiffer F, Johnston AL, Ravichandran C, Polcari A, Teicher MH, Webb RH, et al. Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety. Behav Brain Funct. 2009;5:46.
Disner SG, Beevers CG, Gonzalez-Lima F. Transcranial laser stimulation as neuroenhancement for attention bias modification in adults with elevated depression symptoms. Brain Stimul. 2016;9:780–7.
Bystritsky A, Korb AS, Douglas PK, Cohen MS, Melega WP, Mulgaonkar AP, et al. A review of low-intensity focused ultrasound pulsation. Brain Stimul. 2011;4:125–36.
Gavrilov LR, Tsirulnikov EM, Davies IA. Application of focused ultrasound for the stimulation of neural structures. Ultrasound Med Biol. 1996;22:179–92.
Ai L, Bansal P, Mueller JK, Legon W. Effects of transcranial focused ultrasound on human primary motor cortex using 7T fMRI: a pilot study. BMC Neurosci. 2018;19:56.
Ai L, Mueller JK, Grant A, Eryaman Y, Legon W. Transcranial focused ultrasound for BOLD fMRI signal modulation in humans. Ann Int Conference IEEE Eng Med Biol Soc. 2016 Aug;2016:1758–61.
Sanguinetti JL, Hameroff S, Smith EE, Sato T, Daft CM, Tyler WJ, et al. Transcranial focused ultrasound to the right prefrontal cortex improves mood and alters functional connectivity in humans. Front Hum Neurosci. 2020;14:52.
Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct. 2009;213:93–118.
Hameroff S, Trakas M, Duffield C, Annabi E, Gerace MB, Boyle P, et al. Transcranial ultrasound effects on mental state: a pilot study. Brain Stimul. 2013;6:409–15.
Peterchev AV, Wagner TA, Miranda PC, Nitsche MA, Paulus W, Lisanby SH, et al. Fundamentals of transcranial electric and magnetic stimulation dose: definition, selection, and reporting practices. Brain Stimul. 2012;5:435–53.
Koroshetz W, Gordon J, Adams A, Beckel-Mitchener A, Churchill J, Farber G, et al. The state of the NIH BRAIN initiative. J Neurosci. 2018;38:6427–38.
Goetz SM, Luber B, Lisanby SH, Murphy DL, Kozyrkov IC, Grill WM, et al. Enhancement of neuromodulation with novel pulse shapes generated by controllable pulse parameter transcranial magnetic stimulation. Brain Stimul. 2016;9:39–47.
Halawa I, Shirota Y, Neef A, Sommer M, Paulus W. Neuronal tuning: selective targeting of neuronal populations via manipulation of pulse width and directionality. Brain Stimul. 2019;12:1244–52.
Kallioniemi E, McClintock SM, Deng Z-D, Husain MM, Lisanby SH. Magnetic seizure therapy: towards personalized seizure therapy for major depression. Personalized Med Psychiatry. 2019;17-18:37–42.
Wang JB, Di Ianni T, Vyas DB, Huang Z, Park S, Hosseini-Nassab N, et al. Focused ultrasound for noninvasive, focal pharmacologic neurointervention. Front Neurosci. 2020;14:675.
Luber BM, Davis SW, Bernhardt E, Neacsiu A, Kwapil L, Lisanby SH, et al. Using neuroimaging to individualize TMS treatment for depression: toward a new paradigm for imaging-guided intervention. Neuroimage. 2017;148:1–7.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing and editing, and approved the final version of the paper. ZDD performed the computational modeling and created the figures.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Regenold, W.T., Deng, ZD. & Lisanby, S.H. Noninvasive neuromodulation of the prefrontal cortex in mental health disorders. Neuropsychopharmacol. 47, 361–372 (2022). https://doi.org/10.1038/s41386-021-01094-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01094-3
This article is cited by
-
How electroconvulsive therapy works in the treatment of depression: is it the seizure, the electricity, or both?
Neuropsychopharmacology (2024)