Abstract
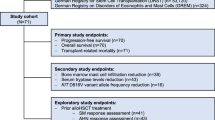
Systemic Mastocytosis (SM) is a multifaceted clinically heterogeneous disease. Advanced SM (AdvSM) comprises three entities: aggressive SM (ASM), mast cell leukaemia (MCL) and SM with an associated hematologic neoplasm (SM-AHN), the latter accounting for 60–70% of all AdvSM cases. Detection of a disease-triggering mutation in the KIT gene (esp. KIT D816V) in >90% of the patients with ASM or SM-AHN has led to a significant improvement in therapeutic options by the implementation of two KIT-targeting kinase inhibitors: midostaurin and avapritinib. Although complete remissions have been reported, neither of these targeted agents is ‘curative’ in all patients and the duration of responses varies. The median overall survival, depending on the WHO subtype and scoring result, is approximately 1 to 4 years. Although the European Competence Network on Mastocytosis (ECNM) and American Initiative in Mast Cell Diseases (AIM) consensus groups recommend allogeneic haematopoietic cell transplantation (allo-HCT) in drug-resistant and other high-risk patients, there is a relative lack of information to guide clinicians on which patients with AdvSM should be considered for transplant, and how KIT inhibitors may fit into the transplant algorithm, including their use pre- and post-transplant to optimise outcomes. Following the generation of an expert panel with a specialist interest in allo-HCT and mastocytosis, these best practice recommendations were generated according to the European Society for Blood and Marrow Transplantation (EBMT) Practice Harmonisation and guidelines and ECNM methodology. We aim to provide a practical, clinically relevant and up-to-date framework to guide allo-HCT in AdvsM in 2024 and beyond.
Similar content being viewed by others
Introduction to systemic mastocytosis and questions to be addressed in best practice paper
Mastocytosis comprises a spectrum of clonal disorders with a markedly heterogeneous clinical phenotype, and aberrant accumulation of neoplastic mast cells (MC) in various tissues, predominantly bone marrow and visceral organs [1,2,3,4,5,6,7]. Since 2001, mastocytosis has been divided into three major groups: cutaneous mastocytosis (CM), systemic mastocytosis (SM) and local mast cell neoplasms, namely mastocytoma and mast cell sarcoma [5,6,7]. The 2022 updates from the World Health Organisation (WHO) and the international consensus classification (ICC) retain these three main entities [3, 4]. SM is delineated from CM by extracutaneous manifestations defined by SM criteria occuring with or without cutaneous involvement [5,6,7]. Based on WHO criteria, SM is further subdivided into indolent SM (ISM), bone marrow mastocytosis (BMM), and smouldering SM (SSM) (all considered non-advanced forms), and the advanced SM (AdvSM) entities: SM with an associated hematologic neoplasm (SM-AHN), aggressive SM (ASM), and mast cell leukaemia (MCL) [4,5,6]. Clinical presentation is dependent on the type of organ involvement, extent of end-organ damage, the degree of MC mediator symptom burden, and the clinical impact and aggressiveness of the AHN if present [1]. Patients with AdvSM can show varying degrees of organ damage due to neoplastic MC infiltration, known as ‘C findings’, including cytopenia due to bone marrow (BM) infiltration or secondary to hypersplenism, liver function abnormalities with ascites, malabsorption with weight loss due to gastrointestinal involvement, or large osteolytic lesions with pathologic fractures. These C-findings are diagnostic criteria for ASM, SM-AHN, and are present in most patients with MCL.
Regarding AdvSM, the median overall survival (OS) for patients with ASM from two large cohorts is estimated to be 41–68 months and the prognosis for MCL is particularly poor, with survival estimates ranging from 2–18 months [8, 9]. Outcomes in SM-AHN are largely dependent upon subtype and individual prognosis of both SM and AHN.
The last decade has observed marked therapeutic advances in AdvSM, including pivotal data from clinical trials of the multi-kinase inhibitor midostaurin and more selective KIT D816V inhibitor, avapritinib [10,11,12]. Although both can induce amelioration in MC-related symptom burdens, responses of BM MC burden, tryptase and KIT D816V variant allelic frequency (VAF), potentially leading to improved survival, neither are curative in most patients and have variable response durations. Patients with AdvSM may also respond to other anti-neoplastic agents, such as cladribine (2CdA) or polychemotherapy. For patients with rapidly progressing ASM or MCL, induction polychemotherapy (plus/minus midostaurin) is usually recommended [6, 13,14,15]. For those who are drug-resistant and are eligible, the consensus group recommends that allogeneic haematopoietic stem cell transplantation (allo-HCT) be considered a potentially curative therapy in selected patients with AdvSM [13, 14, 16, 17]. However, not all patients are eligible and benefits from allo-HCT may be limited due to potential toxicity.
It is essential that physicians treating AdvSM have contemporary guidance on how best to approach allo-HCT for these patients. Practically, the allo-HCT decision-making process is often difficult due to the complexity and heterogeneity of the disease subtypes, the variable prognosis, the disparate duration of response to treatment and a relative lack of contemporary allo-HCT data. Moreover, there is a lack of information on the optimal timing, how KIT Inhibitors may fit into the transplant algorithm and optimisation of post-transplant monitoring. The most recent comprehensive consensus paper regarding allo-HCT for AdvSM was published over 7 years ago when KIT Inhibitors were not yet routinely available [13]. We hereby aim to provide a practical, clinically relevant and up-to-date framework to guide allo-HCT in AdvSM for the current era with these newly approved agents.
Current state of the art
Overview of molecular landscape in SM
More than 90% of patients with AdvSM harbour KIT mutations, commonly the classical KIT D816V gain of function mutation in exon 17 [18,19,20,21,22,23]. Highly sensitive techniques, such as allele-specific quantitative polymerase chain reaction (qPCR) or droplet digital PCR (ddPCR) are recommended by the European Competence Network on Mastocytosis (ECNM) for the detection and monitoring of the KIT D816V mutation [22, 24]. Recently, new techniques such as error-reduced deep sequencing methods have achieved sensitivity levels ranging from 0.01% to 0.1%, making them suitable for measurable residual disease (MRD) monitoring [25]. Rare KIT mutations not involving D816V can usually be identified by next-generation sequencing (NGS), most frequently alternative mutations at position D816, e.g. D816H or D816Y. Such mutations, and mutations in other codons of KIT (e.g., exon 8), are quite frequently detected in CM, MCL, some cases of well-differentiated SM, and paediatric patients. Moreover, in over 60% of patients with AdvSM, additional somatic mutations in other genes (alongside and often concomitant with mutations in KIT) have been observed, which can impact disease progression [26]. In particular, the presence and quantity of pathogenetic mutations in SRSF2, ASXL1, and RUNX1 (so-called S/A/R gene panel), DNMT3A and NRAS can significantly impact OS [27,28,29]. These mutations are detected almost always in patients with SM-AHN.
Treatment in advanced SM
Prior to the advent of the KIT inhibitors midostaurin and avapritinib, treatment for AdvSM was mainly limited to imatinib (in rare cases of KIT D816V negative SM), interferon alfa, 2CdA, and polychemotherapy if required [30]. Cytoreductive treatment in AdvSM is conventionally initiated in those patients where ‘C’ findings are present. Midostaurin, inhibiting both wild-type KIT and mutant KIT D816V, was evaluated at 100 milligrams (mg) twice daily in a phase 2 study in 89 evaluable patients with AdvSM, demonstrating an overall response rate (ORR) of 60% according to modified Valent response criteria and activity across the spectrum of AdvSM subtypes [12]. Notably, a post-hoc analysis utilising the International Working Group-Myeloproliferative Neoplasms Research and Treatment & ECNM (IWG-MRT-ECNM) criteria suggested a lower ORR. Durable haematological responses and non-haematological organ improvements were observed in responders. Midostaurin was approved by the U.S. Food and Drug Agency (FDA) and European Medicines Agency (EMA) in 2017. However, real-world data highlights that complete remissions (CR) are scarce, gastrointestinal adverse effects may reduce tolerability and both primary resistance and rapid progression can limit efficacy [24, 31,32,33]. It has been shown that a midostaurin-mediated reduction in KIT D816V RNA-expressed allele burden ≥25% by month 6 is predictive of superior OS, thus highlighting its value as an ‘on treatment’ response parameter [27]. A recent retrospect analysis comparing the efficacy of midostaurin and 2CdA in AdvSM from the German registry suggests the superiority of midostaurin and that the combination of baseline Mutation-Adjusted Risk Score (MARS) and molecular response could provide a three-tier risk stratification for OS [31].
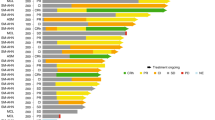
Remission rates in the EXPLORER and PATHFINDER trials, exploring the efficacy and safety of avapritinib, demonstrated markedly superior ORR and higher CR rates [10, 11, 34]. For the 53 AdvSM patients included in the phase I EXPLORER trial, a 75% ORR (36% CR) was achieved [10]. Interim analysis of the phase II PATHFINDER study highlighted an ORR of 75%, with 19% achieving CR with full or partial haematological recovery (CRh)[11]. Updated 2-year data was presented at the SOHO 2023 Annual Meeting, with an ORR of 73% for the entire cohort and highlighted rapid responses (median 2.3 months) [35]. Importantly, rates of progression appear low and are primarily related to the AHN component in SM-AHN patients. Data from both trials led to FDA approval of avapritinib for 1st line treatment in the USA in 2021, whereas EMA approval is, at present, limited to use after prior systemic therapy i.e., second line. Facial oedema is the most commonly observed adverse event and there is a risk of intracranial bleeding which occurred preferentially in patients with severe thrombocytopenia. Therefore, the use of avapritinib is only recommended for those who have a platelet count of >50 ×109/L.
In patients with rapidly progressing ASM or MCL, debulking chemotherapy with an AML-related polychemotherapy protocol, ideally combined with midostaurin (as in patients with FLT3 internal tandem duplication (ITD)-mutated AML) can be applied [36]. Such chemotherapy protocols may also include 2CdA. However, monotherapy with 2CdA (0.12 microgram subcutaneously for 3-5 days every 28 days for 1–6 cycles) is usually insufficient to induce major responses alone and is therefore not routinely recommended as a standard bridge to allo-HCT. Lübke et al. recently reported on 79 AdvSM patients who underwent therapy with 2CdA, documenting an ORR according to modified Valent criteria of 41% in the first line and 35% in 2nd line, where evaluable [37]. There are no data on combination approaches of 2CdA alongside KIT Inhibitors, but 2CdA is combined with AML-directed chemotherapy in some protocols used to treat high-risk AML patients [38]. Clinicians should be aware of significant myelosuppression and the risk of opportunistic infections. Nevertheless, in patients with rapidly progressing (TKI-resistant) ASM, SM-AHN or MCL, AML-like polychemotherapy protocols, including regimens containing ARA-C and daunorubicin, with or without additional 2CdA or gemtuzumab-ozogamicin, can be considered for pre-HCT debulking therapy in TKI-resistant AdvSM, as will be discussed in more detail below. New agents are also entering the therapeutic arena for SM, including bezuclastinib (CGT9486) and elenestinib (Blu-263), and how these will fit into the transplant algorithm remains unknown [39, 40].
Methodology
The EBMT is a non-profit, scientific society representing more than 600 transplant centres mainly in Europe. The present paper was generated according to the EBMT Practice Harmonisation and Guidelines methodology [41]. In addition, experts from the ECNM and AIM supported manuscript development. In the four months leading up to the two-day workshop, preparatory work was carried out by the group which comprised of key opinion leaders in the fields of mastocytosis and/or allo-HCT. All relevant literature in the PubMed database was reviewed by pairs/triplets of experts who generated summative conclusions. The expert group met and discussed the evidence in a series of virtual conferences, culminating in a 2-day in-person meeting in September 2023 in Lille, France. There was no external or industry funding for this work. Thereafter, a draft paper was generated and further circulated to additional disease and transplantation experts for revision and contribution. Given the absence of evidence from randomised trials and the paucity of data, it was not possible to grade these recommendations. They therefore represent the consensus views of all the authors.
Workshop recommendations
Transplant indications in advanced SM
Aggressive systemic mastocytosis (ASM)
With currently available KIT inhibitors, the vast majority of patients with KIT D816V + ASM who lack additional genetic abnormalities or morphological evidence of an AHN (pure ASM; a rare entity) demonstrate high-quality and durable responses and hence do not always routinely require an allo-HCT [34]. Achievement of response may allow delay in allo-HCT in eligible MARS-low risk patients. For those patients who fail to achieve an adequate partial response (PR)/CR, KIT inhibitor switch is the first action. If ineffective and the patient is progressing, bridging therapy such as AML-directed polychemotherapy (plus/minus midostaurin or 2CdA) or experimental chemotherapy (in clinical trials) should be considered before contemplating allo-HCT. The same holds true for patients with mast cell sarcoma (MCS) or MCS-like progression in ASM where multi-drug resistance is often seen. Considerations to the allo-HCT algorithm in ASM are summarised in Fig. 1.
Recommendations
-
In the current era, most KIT D816V + ASM patients without evidence of an AHN who tolerate KIT inhibitors exhibit deep and durable responses and will not require upfront allo-HCT. Achievement of a CR or PR may allow delay, or abrogate the need for, allo-HCT, especially in low-risk patients.
-
In case of suboptimal response (less than PR/CR) to first-line KIT Inhibitors, switching to another KIT inhibitor or chemotherapy should be the initial action prior to allo-HCT*
-
If suboptimal response or progression despite KIT inhibitor switch, polychemotherapy +/-midostaurin or 2CdA should be considered as bridging to allo-HCT if possible*.
*Disease status should always be re-assessed for the presence of an AHN component.
Systemic mastocytosis with an associated haematological neoplasm
AHN are predominantly of myeloid origin, most commonly myelodysplastic neoplasm/ myeloproliferative neoplasm (MDS/MPN) overlaps, MPN, myelodysplastic neoplasms (MDS), chronic eosinophilic leukaemia (CEL), or AML [1, 8]. To establish a diagnosis of SM-AHN, the patient must meet the WHO/ICC diagnostic criteria for both the SM and AHN components [3, 4]. Although lymphoid neoplasms or plasma cell dyscrasias (monoclonal gammopathy of uncertain significance, multiple myeloma) may be found in association with SM, they are rare and may often represent two independent clonal diseases. They do not appear to worsen the prognosis of SM in most patients, which is, in the majority of such cases, ISM. Thus, the role of allo-HCT in lymphoid AHN is not addressed in this paper.
In SM-AHN, it is important to evaluate each disease component individually. For SM-AHN, the transplant decision is guided by the nature and risk of both the AHN and/or the AdvSM. It can be challenging to appreciate the contribution of each component to the risk group; in this setting, an extensive clinical evaluation with selected examinations and/or procedures (e.g. organ biopsy) to assess which disease component is responsible for organ damage (C-findings) is strongly encouraged. Generally, the AHN should be assessed by disease-specific prognostic scores, while SM should be assessed using a validated SM-specific score such as the International prognostic scoring system for mastocytosis (IPSM), MARS, Global Prognostic score for Mastocytosis (GPSM) or Mayo Alliance Prognostic System (MAPS) (Table 1) [9, 28, 29, 42]. However, the non SM disease component-specific scores formally lack validated applicability in the setting of SM-AHN.
Regarding the prognosis of AHN, for patients with SM-MPN, the prognosis is variable, but mostly favorable [43]. For SM-chronic myelomonocytic leukaemia (CMML), comparisons to CMML alone revealed that over 50%-90% of those with SM-CMML had KIT mutations and trended towards worse OS [44, 45], prompting consideration of allo-HCT earlier in the disease course. SM-AML is typically given intensive chemotherapy, in eligible individuals, as primary treatment. In the case of AdvSM-AML and/or when most AML blasts appear to carry KIT D816V, the polychemotherapy protocol should also include midostaurin. In SM-AML, situations can vary markedly as regards prognosis e.g. a patient may have SM and clonally independent good risk AML (e.g. NPM1 mutated AML) with a markedly different prognosis compared to an individual with secondary AML with poor risk mutations such as SRSF2 and RUNX1 mutations progressing from SM-CMML. Jawhar and colleagues highlighted that cases of SM-AML which were KIT mutated and core binding factor negative had a particularly poor prognosis [46].
If the AHN requires consolidative allo-HCT, in patients with aggressive myeloid diseases (e.g, AML, high-risk MDS) after controlling it (e.g., achieving CR), treatment for SM may become necessary to reduce the SM burden (e.g. dependent on MC infiltration burden, KIT VAF, persistent ‘C’ findings etc), leading to initiation of KIT inhibitors as bridging therapy. However, this period should not cause relapse/progression of myeloid disease, therefore sequential or combination of hypomethylating agents (HMA)/chemotherapy with KIT inhibitors can be used for a certain period of time. If the SM burden is already low after induction therapy, allo-HCT should be performed without delay. In patients with intermediate-risk hematologic malignancy (e.g., intermediate-risk MDS) with moderate burden SM, a KIT inhibitor and/or an HMA in combination or sequentially can be considered (although no reliable clinical data is available on the safety and efficacy of these treatments as yet) until a donor is found.
In patients with ISM with low-risk myeloid malignancy, allo-HCT upfront is not needed; however, disease progression for each component should be carefully monitored. Of note, it is unknown if KIT inhibitors will delay progression of SM, haematologic malignancy or both in such patients. Considerations to the allo-HCT algorithm in SM-AHN are summarised in Fig. 2.
Recommendations for allo-HCT in SM-AHN
Estimated OS is dependent predominantly on the AHN component but also the aggressiveness of the SM component hence:
-
Each AHN should be assessed using a disease-specific prognostic score*
-
SM should be assessed with a validated SM specific score, ideally a molecularly annotated one such as IPSM, MARS, GPSM or MAPS.
-
Allo-HCT should be considered in cases of SM-AHN with higher-risk CMML, MDS, MDS/MPN overlap and myelofibrosis according to current disease specific prognostic scores, recommendations provided by international consensus groups and societies, and patient specific variables.
-
For SM-AML, decision for allo-HCT should be considered according to contemporary AML prognostic scores, depth of treatment responses, and patient-specific variables, including co-morbidities etc. It is of pivotal importance to have molecular and cytogenetic annotation to accurately assign prognostic risk.
-
It is important to note that in the SM context (regardless of SM type), the majority of AHN should be considered as high risk and secondary, e.g., secondary AML, albeit there are specific exceptions.
*The impact of co-existing SM on the currently available validated disease specific risk scores remains unknown.
Mast Cell Leukaemia (MCL)
This heterogeneous disorder represents the least common form of AdvSM [2, 5, 7, 47]. Criteria for SM must be fulfilled and atypical immature MC must account for ≥20% of all cells in the BM smear [4, 5, 47]. ICC also recognises the utility of the trephine biopsy if the aspirate is suboptimal [3]. Rarely, ≥10% circulating atypical MC can be found in the peripheral blood (PB), leading to the designation of the ‘leukemic variant’ of MCL [5, 47]. MCL patients lack the typical KIT D816V mutation in about 20% of cases, associated with an aggressive clinical course. MCL can be either primary or secondary to an antecedent MC neoplasm and may occur in combination with an AHN [47]. The majority of patients have a frequently termed ‘acute’ aggressive form with organ involvement/damage whereas a minority have an initially stable, more indolent so-called ‘chronic’ form (defined by the absence of organ damage) that often progresses over a variable time to acute MCL [1, 5, 8, 28, 47, 48]. The presence of S/A/R mutations predicts poor survival. The largest retrospective ECNM registry series encompassed 92 MCL patients; one-third of whom had a morphologically visible AHN [48]. The most common front-line treatment was midostaurin. Patients with MCL-AHN had much worse outcomes compared to those with MCL alone. Inferior survival was associated with abnormal karyotype, evidence of circulating MCs in the PB, lack of the KIT D816V mutation and not receiving a KIT inhibitor. Only 4 patients in this cohort received avapritinib due to the time period evaluated.
In our opinion, transplant-eligible true ‘acute’ MCL patients, where the treating physician determines that there is rapidly progressive/kinetically active disease (consistent with the clinical pace of AML), should be treated to achieve the best response with ‘AML style’ poly-chemotherapy +/− midostaurin (protocols otherwise given to FLT3 ITD + AML patients), or, if this does not lead to major response/ remission, avapritinib and prepare for allo-HCT if possible. Of note, there may be some situations when a TKI is not available or the patient is intolerant. Polychemotherapy may vary e.g. standard induction regimens, azacytidine-based regimens (e.g venetoclax and azacytidine) etc based upon clinician choice, patient fitness/ co-morbidities and availability. These recommendations reflect the cumulative experience of the authors.
For patients diagnosed as acute MCL with ‘C findings’ that demonstrate relative clinical stability (e.g. not demonstrating rapidly proliferative white blood cell (WBC) counts, other haematological or non-haematological organ damage without clinical deterioration), TKI monotherapy should be considered as frontline therapy to bridge to allo-HCT. In addition, 2CdA, especially if there is a lack of access to KIT inhibitors or a contraindication, represents another potential therapeutic regimen. For those with MCL-AHN, given the dismal prognosis, both disease compartments should be treated, and if a response is demonstrated, allo-HCT should be considered without delay.
If ‘chronic’ MCL is present and the patient achieves a CR/PR with KIT inhibitor therapy, potential donors should be identified early, but allo-HCT may not be immediately necessary. However, if chronic MCL is progressive (progresses to acute MCL), poly-chemotherapy plus a KIT inhibitor (with the caveats as discussed above) could again be considered and the patient prepared for allo-HCT. The role of salvage allo-HCT in chemotherapy and KIT inhibitor refractory MCL patients, in our view, is limited. Enrolment in clinical trials for all cases should be considered. Considerations to the allo-HCT algorithm in MCL are summarised in Fig. 3.
Recommendations
-
Allo-HCT is indicated for patients with acute MCL and those with rapidly progressing ASM. For those with chronic MCL without AHN and/or poor prognostic somatic mutations, response to KIT inhibitors may permit delay. In addition, patients with ASM who have slow progression, no AHN and no high-risk profile may benefit from KIT inhibitor therapy over a longer time period.
-
Transplant-eligible patients with rapidly progressing/ kinetically active ‘acute’ MCL or rapidly progressing ASM could be treated to best response with poly-chemotherapy +/− midostaurin (all types) or with avapritinib (if KIT D816V is present, platelets > 50 × 109/L), and considered for allo-HCT if disease response is demonstrated.
-
For patients diagnosed as acute MCL with ‘C findings’ that demonstrate relative clinical stability (e.g. no rapidly proliferative WBC count, other haematological or non-haematological organ damage without clinical deterioration), TKI monotherapy could be considered as frontline therapy to bridge to allo-HCT. 2CdA can also be a viable option.
-
Patients with MCL-AHN have a significantly worse outcome so should undergo treatment to address both ‘compartments’ followed by allo-HCT without delay if response demonstrated.
-
For patients with a ‘chronic’ MCL phenotype who achieve a CR/PR to treatment, there is no immediate indication for allo-HCT. If progressive, we suggest a clinical trial or an ‘off label’ combination approach or debulking with chemotherapy plus midostaurin before considering allo-HCT.
-
In patients with acute or chronic MCL lacking the common KIT D816V mutation, treatment with KIT inhibitors alone is usually not beneficial and prognosis is poor, so consider for AML-like poly-chemotherapy therapy plus a KIT inhibitor followed by allo-HCT if response gained.
-
For MCL demonstrating resistance against multiple chemotherapy forms and KIT inhibitors, the beneficial role of allo-HCT, in our opinion, is limited.
-
Enrolment in clinical trials for all cases should be considered where available.
KIT Inhibitor management and AdvSM evaluation prior to allo-HCT
KIT Inhibitor Optimisation and Management peri-transplant
Ideally, optimisation of KIT inhibitor dose should be attempted e.g. 100 mg twice daily for midostaurin and avapritinib 200 mg once daily (ideally ≥100 mg daily). In those with a platelet count of <50 × 109/L, avapritinib should not be utilised. Deepest possible remission prior to allo-SCT would be desirable. Haematological toxicities of KIT inhibitor treatment may be overcome by supportive treatment to maintain higher doses of KIT Inhibitor treatment (e.g. G-CSF, consideration to thrombopoietin-agonists, recombinant human erythropoietin, transfusions etc.). While these are being used in some centres, it must be noted that no formal data exists in regard to their use or how they can optimize KIT-inhibitor ‘dosing density’ in patients/modify responses.
Despite a lack of clear data on the optimal timepoint for KIT inhibitor switch in AdvSM, the KIT VAF and tryptase level may be good surrogate parameters indicating suboptimal response. In our view, assessment should be performed regularly with KIT VAF assessment in both the PB and BM, together with the pure pathological response (PPR) and clinical response according to the modified (m) IWG-MRT-ECNM criteria [27, 31]. In cases of MCL with higher-risk features or SM-AHN, where the aim is to get to allo-HCT, regular assessment of KIT VAF and tryptase and degree of BM infiltration at month 3 and 6 could prompt KIT Inhibitor switch to second line KIT Inhibitor or to 2CdA, or to additional polychemotherapy (especially in rapidly progressing MCL and ASM), if response to TKI is suboptimal [49]. There are no data on how KIT Inhibitors should be managed immediately peri-transplant. Usually, TKI should be discontinued shortly before conditioning. Tapering the dose over a few days prior to the start of conditioning would appear pragmatic. Clinicians should be observant of mediator symptoms due to a ‘withdrawal syndrome’, which may necessitate use of steroid therapy. In addition, steroids should be considered shortly before the administration of chemotherapy or targeted drugs in those patients who are known to develop repeated anaphylaxis after drug exposure.
AdvSM response evaluation prior to Allo-HCT
Challenges in defining response in AdvSM are inherent to the heterogeneous and multifaceted nature of the disease, especially if an AHN component is present. The scenario may be even more complex, if there are discordant responses in the SM and AHN components. In the KIT inhibitor era, robust data on pre-transplant disease burden and allo-HCT outcomes are lacking. In the pre-KIT inhibitor study by Ustun et al. utilizing myeloablative conditioning (MAC) compared to reduced intensity conditioning (RIC) regimens and achieving initial response compared to stable disease/ progression were associated with improved post allo-HCT survival [16]. This may indicate a need for maximising pre-transplant responses.
Pragmatically, we suggest that the PPR criteria may be the most straightforward when assessing AdvSM prior to allo-HCT [50]. PPR criteria were generated to reflect the importance of response in terms of reduction in MC burden and incorporate a quantitative assessment of BM MC infiltration, serum tryptase levels, and CR/CRh [50]. Here ‘CR’ is defined as the absence of BM MC aggregates and serum tryptase <20 ng/mL with full or partial (CRh) haematologic recovery; PR is defined by a ≥ 50% reduction in BM MC infiltration and serum tryptase level’.
For SM-AHN, disease response should be assessed for both components and the timing of allo-HCT is likely dictated by the AHN component rather than the SM component, and both should ideally be in the best response at time of allo-HCT. For the AHN component, indications and timing of transplant should be guided by the generally accepted EBMT and American Society for Transplantation and Cellular Therapy (ASTCT) guidelines and pre-transplant management should follow recommendations for the particular entity [51, 52]. For the SM component, induction of best possible remission (ideally mIWG CR/CRh/PR) by KIT inhibitors and/or debulking chemotherapy plus KIT inhibitor (in case of rapidly progressing MCL or ASM even if negative for KIT D816V) should be applied. In our view, it would be beneficial to carefully document the response as per PPR criteria prior to allo-HCT.
Lastly, the potential risk of clonal evolution whilst on KIT inhibitors must be noted. Sriskandarajah reported on 3 cases of AdvSM-AHN successfully bridged to allo-HCT after treatment with avapritinib [53]. Of note, in 2 cases who achieved CR of the SM component, AHN clonal evolution to AML occurred whilst undergoing avapritinib therapy. Patients hence require careful monitoring to detect any signs of AHN progression.
Recommendations
-
SM-AHN requires close monitoring of tryptase, KIT VAF and additional mutation VAFs in addition to assessment of degree of bone marrow MC infiltration.
-
Optimisation of dose of KIT inhibitor should be attempted during disease management.
-
Peri-transplant, KIT inhibitor can be maintained until the start of conditioning or can be discontinued shortly (a few days) before conditioning. In case the patient is suffering from frequent mediator-related symptoms, a short course of low dose corticosteroids should be administered.
-
For SM-AHN, timing of allo-HCT may be dictated by the AHN and/or by the SM component. If both dictate, both should ideally be in the best response possible at time of allo-HCT.
-
For the SM component, induction of best possible remission (ideally mIWG CR/CRh/PR) should be the aim.
Mast cell symptom burden directed strategies
Irrespective of the cytoreductive treatment chosen, individualised symptomatic treatment is normally given to every AdvSM patient. Approaches vary and are prescribed to patients in a step-wise approach. The basis of therapy for all patients consists of histamine receptor 1 antagonists and histamine receptor 2 antagonists. If this therapy does not sufficiently bring mediator-related symptoms under control, MC stabilizers may be administered; in those with gastrointestinal problems, proton pump inhibitors (PPI) or oral diaminoxidase may be added; and in those with repeated severe mediator-related events, glucocorticosteroids may be required. In those with recurrent severe anaphylaxis, additional treatment with the monoclonal anti-immunoglobulin E antibody omalizumab may be considered, and in those with repeated anaphylaxis after bee or asp stings, continuous treatment with prophylactic immunotherapy is usually recommended. If all these treatments are not sufficient to bring mediator-related events under control, KIT inhibitor therapy with avapritinib (approved) or midostaurin (off-label) may be considered. Indeed, both drugs reportedly counteract IgE-mediated histamine secretion from basophils and MC, including KIT-mutated MC in SM [54, 55].
Symptomatic treatment should be continued throughout the peri allo-HCT period and maintained further as required, particularly for those with significant mediator symptom burdens. Reduction of symptomatic treatment might be feasible after allo-HCT but timing remains unclear and is likely individual-dependent. In our view, omalizumab should be discontinued prior to the commencement of conditioning. The incidence of anaphylaxis and severe mediator-related reactions were low in the study from Ustun et al but transplant clinicians should be alert to possible occurrence [16].
Recommendations
-
For AdvSM patients on symptom-directed treatment this should be continued peri-transplant.
-
Symptomatic treatment can be adjusted after allo-HCT as required, particularly for those with a significant mediator symptom burden.
-
If a patient had been receiving omalizumab, this should be discontinued prior to conditioning.
-
Anaphylactic reactions are rare but ‘EpiPens’ should be available in the patient room/ambulatory setting.
Assessing disease risk using prognostic scores
A number of risk scores have been developed to help clinicians estimate survival in SM (Table 1). These include the IPSM, MARS, MAPS and GPSM [9, 28, 29, 42]. Several require further validation in larger, contemporary cohorts in the era of targeted agents. Both the IPSM and MARS score are predictive for OS in midostaurin-treated patients [31]. A novel dynamic prognostic score (MARSv2.0) has been suggested through the combination of baseline MARS and dynamic KIT D816V molecular response at 6-months for midostaurin-treated patients [31]. Where possible, we encourage the use of molecular profile-enhanced scores such as MARS, GPSM and MAPS in transplant-eligible AdvSM patients. However, this information should always be in conjunction with the assessment of MC disease burden (BM MC infiltration, tryptase, KIT VAF) and disease risk estimation/ therapy response. For patients with SM-AHN, AHN-specific prognostic scores should also be considered. For example, in those with ISM-MDS, prognosis and outcome will be determined by the MDS portion of the disease, and IPSS-R, IPPS-M, and transplantation-related scores (such as the Haematopoietic Cell Transplantation (HCT)-specific Comorbidity Index (HCT-CI)) may help predict outcomes of patients before and after allo-HCT.
Recommendations
-
In our opinion, molecularly annotated SM specific scores such as IPSM, MARS, GPSM and MAPS should be utilised in all potential allo-HCT candidates. Of note, these have not been validated in the current KIT inhibitor era nor in the allo-HCT setting.
-
These scores must always be considered in conjunction with assessment of MC disease burden and cannot be used in isolation to determine the allo-HCT decision.
-
In patients with SM-AHN, additional application of AHN-related scores is recommended, especially when the AHN component rather than the SM component will dictate outcomes, such as in ISM-AML or ISM-MDS, etc.
Recipient age for allo-HCT in AdvSM
The majority of available data on allo-HCT in AdvSM derives from individuals aged less than 70-years [16]. In general, we would propose allo-HCT in patients ≤ 70 years of age with a transplant indication due to either ASM, SM-AHN or MCL [13]. This is an individual decision that should weigh the patient ‘fitness’ and comorbidities, patient preferences, and specific disease features. In those older than 70 years, individual risk assessment needs to be performed. Ideally, all patients should be discussed with centres experienced in AdvSM patient management.
Recommendations
-
In general, patients ≤ 70 years with AdvSM who have a transplant indication should be considered for allo-HCT. This is an individual decision that should weigh patient ‘fitness’ and comorbidities, patient preferences, and disease features.
-
In patients aged > 70 years, allo-HCT is an individual decision that should weigh patient ‘fitness’ and comorbidities, patient preferences, and disease features. Comorbidity scores and frailty assessments as well as chances to respond to less intensive therapies should also be considered.
-
Where possible, such patients should be reviewed in centres experienced in AdvSM management. A multidisciplinary approach is highly encouraged.
Patient evaluation prior to allo-HCT section
The suggested approach to AdvSM patient evaluation is summarised in Table 2. Assessing MC burden-related organ impairment prior to transplantation is essential. Standard laboratory tests, including pre-transplant ferritin levels and a baseline PB serum tryptase level, should be recorded. If present, KIT VAF should be established as a baseline pre-allo-HCT in the PB and BM with a sensitive assay, e.g. ddPCR or allele-specific PCR and the same assay should hence be used prior to, during and in the post-allo-HCT period. BM aspirate and trephine biopsy should be performed, to include evaluation of MC, reticulin grading, and AHN component if present. Conventional karyotyping/SNP-A should be performed (particularly if AHN is present, including AHN-related Fluorescence in situ Hybridization (FISH) panels) alongside BM KIT VAF and extended quantitative myeloid mutational panel assessment/AHN-directed molecular assessment. Imaging to assess extent/absence of splenomegaly, hepatomegaly, lymph-node enlargement or ascites should be performed. If any evidence of liver impairment or portal hypertension, an assessment of liver ‘stiffness’ via techniques such as shear wave elastography and Doppler assessment of the portal vein may be needed [56, 57]. Bone densitometry may be considered if not performed within 12 months. In addition to assessing AdvSM disease activity and response, the patient’s eligibility for allo-HCT is evaluated through standard pre-transplant organ function assessment.
Donor choice, stem cell source, conditioning, GVHD prophylaxis and T cell depletion
Given the limited/absence of data concerning these variables in AdvSM allo-HCT in the current KIT inhibitor era, there is wide variation in approaches, often centre-dependent. The optimal conditioning intensity remains unknown. In SM-AHN, the choice of transplant regimen should conform to contemporary AHN guidance and risk assessment. In the retrospective analysis from Ustun, recipients undergoing MAC tended to fare better than those undergoing RIC protocols but this was prior to the KIT Inhibitor era and has not been confirmed in more recent analyses [16]. In that study, matched related and unrelated donors had similar outcomes. Of note, over the last decade haploidentical donor transplantation has significantly increased, but information in SM is lacking. In patients who do not have a HLA-full matched donor, a haploidentical family member should be considered in patients where allo-HCT is indicated given success in many other hematologic malignancies. Nakamura and colleagues reported on 3 patients with AdvSM undergoing nonmyeloablative conditioning using a matched sibling donor [16]. Despite adequate engraftment and full donor T cell chimerism, all progressed, with the longest response duration being 39 months. Clearly, the conditioning regimen should be tailored to each individual patient. In our opinion, in the case of younger, ‘fit’ AdvSM patients with a suboptimal response, we would recommend more intensive conditioning regimens and early immunosuppression wean.
Recommendations
-
Donor choice and stem cell source should follow centre-specific practice and in SM-AHN as indicated by AHN disease specific guidance and risk assessment.
-
The type and intensity of conditioning regimen and GVHD prophylaxis strategy should be tailored to each individual patient scenario as determined by centre specific protocols.
-
There is a lack of data to guide on RIC or MAC platforms in the current KIT inhibitor era. However, in case of younger, ‘fit’ AdvSM patients with suboptimal response, we would recommend more intensive conditioning regimens and early immunosuppression wean.
Drug interactions in the peri- and post allo-HCT setting
Clinicians should be aware that there is a risk of interaction between KIT inhibitors and other drugs that may be used in the peri-and post-transplant period. Concomitant use of moderate or strong CYP3A inhibitors (e.g. posaconazole, voriconazole, aprepritant) should be avoided in parallel as they can increase the plasma concentration of avapritinib or midostaurin whereas CYP3A inducers can lead to decreased plasma concentrations. Discussion with the clinical pharmacy team should occur to be alert to any potential drug interactions.
Disease monitoring after transplantation
Overview
Monitoring AdvSM after transplantation requires a comprehensive approach. This can be particularly complex in those with SM-AHN. Notably, long-term persistence of the MC component has been described and complete eradication of the MC clone is unusual during the first 6–12 months[16]. Conversely, the AHN component often exhibits an earlier response to treatment. In brief, for the MC component, the key indicators include monitoring of serum tryptase levels (very consistent with tumour burden, reflects response well, easy to perform), assessment of the BM MC burden, and MRD evaluation using high-sensitivity KIT mutation analysis in both PB and BM. Organ evaluation should occur as guided by initial disease involvement. AHN assessment, on the other hand, depends on the underlying disease. This includes BM biopsy (with detailed histologic assessment, including immunohistochemistry employing antibodies against KIT, CD34, CD25, CD30 and others depending on AHN variants) and aspirate, genomic profiling, and longitudinal monitoring of any molecular marker. Chimerism analysis should be performed at regular intervals according to centre policy. Table 3. suggests an approach for monitoring AdvSM patients post allo-HCT.
Measurable Residual Disease assessment post allo-HCT
Data on MRD following allo-HCT for AdvSM are rare. Even with successful allo-HCT, we envision slow clearance kinetics of KIT mutations, with reduction within the initial 12 months post-transplant, rather than complete early eradication. Data in this regard are warranted, particularly as MRD monitoring may potentially change clinical practice with the use of KIT inhibitors in the post-transplantation setting. Due to the different response times of the SM and AHN components, a separate evaluation of both is essential. Another potent MRD parameter is the basal serum tryptase level, especially when tryptase levels before therapy (debulking and/or allo-HCT) were very high and decreased to normal or near normal levels after allo-HCT. The sensitivity of tryptase as an MRD marker may be as high as molecular monitoring [58]. Without allergic reactions, consecutive measures showing a sustained increase should prompt disease re-evaluation. Therefore, we recommend tryptase as a MRD marker in these patients, especially when no molecular MRD markers are available, e.g. when MCL cells did not express a KIT mutation and bone marrow biopsy.
Chimerism analysis
Chimerism analysis is a standard tool post allo-HCT to monitor for imminent relapse. While total donor cell chimerism might provide a sensitivity of 1-5% with short tandem repeat (STR)-based approaches on whole PB or BM, the use of single nucleotide variants (SNVs) or ddPCR can achieve sensitivities as low as 0.1%. Whole blood chimerism is widely used, although lineage-specific analysis can also be examined, with CD3+ T-cell fraction and myeloid progenitor enrichment (CD34, CD33, or CD117) being the most widely adopted. For patients with SM-AHN, chimerism decline does not distinguish between relapse or progression in SM and/or AHN components, so comprehensive evaluation of both is crucial. However, bone marrow aspirates might be underestimating chimerism in myeloid compartments due to under presentation of mast cells. Similarly, myeloid chimerism in peripheral blood will not reflect accurately the mastocyte component.
Recommendations
-
For the SM component and KIT-mutated AHN component, KIT mutation monitoring should be performed using highly sensitive techniques.
-
BM yields higher sensitivity for detecting KIT mutations than PB in most cases, thus molecular CR status should be confirmed in BM samples.
-
For the AHN component, cytogenetics, and molecular evaluations (monitoring) as per disease specific guidelines should be followed, with recognition that some of the AHN variants (often CMML, sometimes also AML) may also display KIT D816V.
-
The use of extended NGS panels in MRD monitoring is currently not standardized in SM-AHN and hence remains a research tool, unless the AHN clone at diagnosis (before allo-HCT) expressed a NGS-relevant mutation.
Therapeutic intervention post allo-HCT
Use of KIT inhibitors post allo-HCT
Maintenance
There is no current evidence to support routine KIT Inhibitor use as maintenance therapy in AdvSM, especially if patients are in CR/CRh prior to allo-HCT. However, given non-negligible progression rates, and successful targeted maintenance therapies in other haematologic diseases after allo-HCT, consideration could be given in high-risk cases (moderate/high SM burden at allo-HCT, ASM, acute MCL or the presence of high molecular risk signature) and those who are at risk of develop imminent relapse (e.g., sequential increase in KIT D816V VAF or tryptase levels along with decrease in myeloid and/or T cell chimerism). Optimal doses of these KIT inhibitors post-allo-HCT are unknown, and adverse effects are expected: cytopenias, especially in the early phase after allo-HCT. Therefore robust neutrophil and platelet engraftment is pre-requisite to start a KIT inhibitor at lower doses. Doses can be ‘titrated up’ as tolerated and required.
Salvage for emergent/ frank relapse of MC component
Data here is limited to case reports. Martynova reported on the potential benefit of midostaurin in a single patient with early frank ASM relapse post allo-HCT [59]. Following dose titration, at time of report the patient had evidence only of MRD at 24 months, highlighting potential efficacy in this setting. Further data are required.
Recommendations
-
In case of CR/CRh prior to allo-HCT there is no routine requirement for KIT inhibitor maintenance for non MCL cases or patients with high risk molecular signatures unless reassessment after allo-HCT reveals an overt or imminent relapse.
-
Post allo-HCT, KIT inhibitor maintenance (provided that haematological reconstitution or at least platelet reconstitution >50 to 75 × 109/L has occurred) can be considered if patient is in less than CR after allo-HCT, for cases of MCL, and for those with high molecular risk signatures. While the dosing strategy remains unknown, we would recommend starting in the lower-dose range (e.g., avapritinib 50-100 mg daily or midostaurin 50 mg twice daily), as guided by haematological parameters and disease status. Duration is determined by individual patient response. In those who are negative for KIT D816V, post-HCT treatment with KIT D816V-targeting drugs may also be considered for high-risk patients but is not considered standard. Prospective clinical trials are required to define whether patients with or without residual KIT-mutated disease (SM and/or AHN) can benefit from such post-HCT therapy.
-
Monitoring of KIT VAF post allo-HCT can guide subsequent KIT inhibitor introduction and dose adjustment. Incomplete clearance or re-emergence of detectable persistent KIT (KIT D816V) would trigger initiation of KIT inhibitors. However, there is no current evidence to suggest at what KIT MRD threshold we should consider introducing KIT Inhibitor or if persistence of detectable MRD associates with higher risk of disease reoccurrence or progression. Further studies are needed to clarify these points.
-
In cases of frank SM relapse, KIT inhibitors should be introduced as guided by haematological parameters and molecular results.
Donor lymphocyte infusions
Spyridonidis and colleagues reported on a DLI-induced graft-versus-mast cell (GvMC) benefit in a case of MCL allo-HCT. In the Ustun study, 10 patients received DLI for mixed recipient/ donor chimerism and/or persistence of ‘stable SM disease’ [60]. Responses, of variable duration, were observed in 6 patients. As expected, approaches were heterogeneous and included DLI alone, DLI and KIT inhibitors, DLI and 2CdA and DLI followed by second allo-HCT. More recently, Hägglund et al. reported on a successful GvMC effect following escalating dose DLI in a patient with SM-AHN (aleukaemic MCL-MPN) [61]. Akin to other diseases, the utility of DLI can be considered in three individual settings: prophylactic, pre-emptive, and salvage. It must be noted that in cases of SM-AHN, either component or indeed both, may drive the decision on DLI use.
Prophylactic
At present, there is no evidence available to support the consideration of routine prophylactic DLI based on a disease-risk assessment of AdvSM or an AHN if present.
Pre-emptive
For the MC component, this is a complex area due to a lack of clarity on the role of KIT and other associated mutations, as markers of MRD in this setting and no data on the relapse predictive value of clearance kinetics and MC persistence. The use of pre-emptive DLI is most straightforward for increasing recipient chimerism as demonstrated by PB or BM sample assessment.
Salvage
Pre-emptive strategies should ideally take precedence over salvage approaches where efficacy is likely lower.
Combination of other therapies with DLI
There is no data to support the routine use of HMA, KIT inhibitors, or intensive chemotherapy with DLI. However, in our opinion, these agents may be considered dependent on clinical phenotype e.g. if there is a relapse of AML or MDS or CMML etc as the AHN component (HMA, intensive chemotherapy etc) or if the MC component is demonstrating increased activity as demonstrated by rapidly rising basal tryptase levels over time or impaired organ function due to rapid MC expansion (avapritinib or midostaurin). Prospective data collection of such approaches is clearly required to inform future decisions.
Recommendations
-
Evidence supporting the use of adoptive immunotherapy with DLI following allo-HCT for AdvSM is, at present, limited.
-
In cases of SM-AHN, either component, or indeed both, may drive the decision on DLI use. The goal of DLI use has to be clear and end point well defined as determined by indication e.g. achievement of full donor chimerism or clearance of MRD (AHN).
-
There is no evidence to support consideration to routine prophylactic DLI.
-
Use of pre-emptive DLI is most straightforward for increasing recipient chimerism as demonstrated by PB or BM sample analysis or persistence/re-occurrence of AHN molecular/ cytogenetic abnormalities. Monitoring of KIT VAF post allo-HCT may guide the DLI decision, especially when the VAF is rapidly increasing, but there is no current evidence to suggest at what KIT MRD threshold we should consider introducing DLI. Further studies are needed.
-
Pre-emptive strategies should ideally take precedence over salvage approaches used in the setting of frank disease relapse where efficacy is likely lower.
Role of second allo-HCT for relapse or graft failure
In the study from Ustun, only 3 patients underwent a 2nd allo-HCT procedure for differing indications: relapse of myelomastocytic leukaemia at 4-months (MAC), relapse of AML at 5-months (RIC) and progression of both MDS and SM (RIC) at 44 months post the first allo-HCT [16]. All were reported as achieving CR but longer-term outcomes remain unknown. The main indications in clinical practice would be graft failure or relapse of the AHN or SM not responsive to DLI or nonavailability of DLI. Clearly, candidates should be ‘fit’ for a second procedure. Bridging therapy depends on the compartment of focus (AHN versus SM component) but ideally should aim for deep response and take into consideration lines of therapy, responses gained previously, and expression of KIT D816V and other targets in the cells of the relapsing disease (SM and/or AHN).
Future directions and unanswered questions
Further data in this field is clearly required to guide and refine our recommendations. Further collaborations between centres of excellence for SM and transplant units is required to harmonise approaches and collect data prospectively. Key unanswered questions in the field are many but we suggest prioritisation of the following:
-
1.
Howmolecular annotated scores influence the allo-HCT decision and determine post-allo-HCT outcomes, if at all?
-
2.
What is the ideal donor for allo-HCT in AdvSM when lacking a matched sibling donor?
-
3.
Optimization of conditioning: now that we are getting deeper CRs with KIT Inhibitors, how best to choose between transplant conditioning intensity and regimens?
-
4.
How should KIT Inhibitors be used optimally peri-transplant? Understanding the impact upon immune reconstitution would also be pivotal.
-
5.
What is the optimal debulking therapy in rapidly progressing ASM, MCL, and SM-AHN prior to allo-HCT?
-
6.
What TKI could be applied after allo-HCT, at what dose, and for how long?
-
7.
A clearer understanding of KIT and other mutations as MRD markers, and to guide DLI; kinetics and timing remain unclear.
-
8.
Determining long-term outcomes of allo-HCT in the KIT Inhibitors era.
Conclusions
These proposed best practice recommendations are predominantly based on agreed expert opinion given the lack of high-quality data in the arena of SM and allo-HCT. Moreover, although we have tried to be comprehensive, we are aware that they will not cover all possible clinical scenarios. Nonetheless, our suggested guidelines provide a contemporary and practical approach to allo-HCT in AdvSM for clinicians and may provide the basis for more consistent monitoring and reporting and, hence, more informed decisions in future clinical practice as such data is collated. Multi-centre, prospective trials are encouraged to address these knowledge gaps for these rare diseases.
References
Pardanani A. Systemic mastocytosis in adults: 2023 update on diagnosis, risk stratification and management. Am J Hematol. 2023;98:1097–116.
Valent P, Akin C, Sperr WR, Horny HP, Arock M, Metcalfe DD, et al. New insights into the pathogenesis of mastocytosis: emerging concepts in diagnosis and therapy. Annu Rev Pathol Mech Dis. 2023;18:361–86.
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood 2022;140:1200–28.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia. 2022;36:1703–19.
Valent P, Horny HP, Escribano L, Longley BJ, Li CY, Schwartz LB, et al. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001;25:603–25.
Valent P, Akin C, Metcalfe DD. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood. 2017;129:1420–7.
Valent P, Akin C, Hartmann K, Alvarez-Twose I, Brockow K, Hermine O, et al. Updated diagnostic criteria and classification of mast cell disorders: a consensus proposal. HemaSphere. 2021;5:e646.
Lim KH, Tefferi A, Lasho TL, Finke C, Patnaik M, Butterfield JH, et al. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood. 2009;113:5727–36.
Sperr WR, Kundi M, Alvarez-Twose I, Van Anrooij B, Oude Elberink JNG, Gorska A, et al. International prognostic scoring system for mastocytosis (IPSM): a retrospective cohort study. Lancet Haematol. 2019;6:e638–49.
DeAngelo DJ, Radia DH, George TI, Robinson WA, Quiery AT, Drummond MW, et al. Safety and efficacy of avapritinib in advanced systemic mastocytosis: the phase 1 EXPLORER trial. Nat Med. 2021;27:2183–91.
Gotlib J, Reiter A, Radia DH, Deininger MW, George TI, Panse J, et al. Efficacy and safety of avapritinib in advanced systemic mastocytosis: interim analysis of the phase 2 PATHFINDER trial. Nat Med. 2021;27:2192–9.
Gotlib J, Kluin-Nelemans HC, George TI, Akin C, Sotlar K, Hermine O, et al. Efficacy and safety of Midostaurin in advanced systemic mastocytosis. N. Engl J Med. 2016;374:2530–41.
Ustun C, Gotlib J, Popat U, Artz A, Litzow M, Reiter A, et al. Consensus opinion on allogeneic hematopoietic cell transplantation in advanced systemic mastocytosis. Biol Blood Marrow Transpl. 2016;22:1348–56.
Valent P, Hartmann K, Schwaab J, Alvarez-Twose I, Brockow K, Bonadonna P, et al. Personalized management strategies in mast cell disorders: ECNM-AIM User’s guide for daily clinical practice. J Allergy Clin Immunol Pr. 2022;10:1999–2012.e6.
Valent P, Akin C, Arock M, Gleixner KV, Greinix H, Hermine O, et al. Antibody-based and cell therapies for advanced mastocytosis: established and novel concepts. Int J Mol Sci. 2023;24:15125.
Ustun C, Reiter A, Scott BL, Nakamura R, Damaj G, Kreil S, et al. Hematopoietic stem-cell transplantation for advanced systemic mastocytosis. J Clin Oncol. 2014;32:3264–74.
Valent P, Akin C, Hartmann K, Nilsson G, Reiter A, Hermine O, et al. Advances in the classification and treatment of mastocytosis: current status and outlook toward the future. Cancer Res. 2017;77:1261–70.
Nagata H, Worobec AS, Oh CK, Chowdhury BA, Tannenbaum S, Suzuki Y, et al. Identification of a point mutation in the catalytic domain of the protooncogene c-kit in peripheral blood mononuclear cells of patients who have mastocytosis with an associated hematologic disorder. Proc Natl Acad Sci. 1995;92:10560–4.
Reiter A, George TI, Gotlib J. New developments in diagnosis, prognostication, and treatment of advanced systemic mastocytosis. Blood. 2020;135:1365–76.
Kristensen T, Vestergaard H, Møller MB. Improved detection of the KIT D816V mutation in patients with systemic mastocytosis using a quantitative and highly sensitive real-time qPCR assay. J Mol Diagn. 2011;13:180–8.
Erben P, Schwaab J, Metzgeroth G, Horny HP, Jawhar M, Sotlar K, et al. The KIT D816V expressed allele burden for diagnosis and disease monitoring of systemic mastocytosis. Ann Hematol. 2014;93:81–8.
Arock M, Sotlar K, Akin C, Broesby-Olsen S, Hoermann G, Escribano L, et al. KIT mutation analysis in mast cell neoplasms: recommendations of the European Competence Network on Mastocytosis. Leukemia. 2015;29:1223–32.
Arock M, Hoermann G, Sotlar K, Hermine O, Sperr WR, Hartmann K, et al. Clinical impact and proposed application of molecular markers, genetic variants, and cytogenetic analysis in mast cell neoplasms: Status 2022. J Allergy Clin Immunol. 2022;149:1855–65.
Gotlib J, Schwaab J, Shomali W, George TI, Radia DH, Castells M, et al. Proposed European Competence Network on Mastocytosis—American Initiative in Mast Cell Diseases (ECNM-AIM) Response Criteria in Advanced Systemic Mastocytosis. J Allergy Clin Immunol Pr. 2022;10:2025–2038.e1.
Stasik S, Schuster C, Ortlepp C, Platzbecker U, Bornhäuser M, Schetelig J, et al. An optimized targeted Next-Generation Sequencing approach for sensitive detection of single nucleotide variants. Biomol Detect Quantif. 2018;15:6–12.
Schwaab J, Schnittger S, Sotlar K, Walz C, Fabarius A, Pfirrmann M, et al. Comprehensive mutational profiling in advanced systemic mastocytosis. Blood. 2013;122:2460–6.
Jawhar M, Schwaab J, Naumann N, Horny HP, Sotlar K, Haferlach T, et al. Response and progression on midostaurin in advanced systemic mastocytosis: KIT D816V and other molecular markers. Blood. 2017;130:137–45.
Pardanani A, Shah S, Mannelli F, Elala YC, Guglielmelli P, Lasho TL, et al. Mayo alliance prognostic system for mastocytosis: clinical and hybrid clinical-molecular models. Blood Adv. 2018;2:2964–72.
Muñoz-González JI, Álvarez-Twose I, Jara-Acevedo M, Zanotti R, Perkins C, Jawhar M, et al. Proposed global prognostic score for systemic mastocytosis: a retrospective prognostic modelling study. Lancet Haematol. 2021;8:e194–204.
Alvarez-Twose I, Matito A, Morgado JM, Sánchez-Muñoz L, Jara-Acevedo M, García-Montero A, et al. Imatinib in systemic mastocytosis: a phase IV clinical trial in patients lacking exon 17 KIT mutations and review of the literature. Oncotarget. 2017;8:68950–63.
Lübke J, Schwaab J, Naumann N, Horny HP, Weiß C, Metzgeroth G, et al. Superior efficacy of midostaurin over cladribine in advanced systemic mastocytosis: a registry-based analysis. J Clin Oncol. 2022;40:1783–94.
Tzogani K, Yu Y, Meulendijks D, Herberts C, Hennik P, Verheijen R, et al. European Medicines Agency review of midostaurin (Rydapt) for the treatment of adult patients with acute myeloid leukaemia and systemic mastocytosis. ESMO Open. 2019;4:e000606.
FDA. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/207997Orig1Orig2s000MedR.pdf.
Reiter A, Gotlib J, Álvarez-Twose I, Radia DH, Lübke J, Bobbili PJ, et al. Efficacy of avapritinib versus best available therapy in the treatment of advanced systemic mastocytosis. Leukemia. 2022;36:2108–20.
Gotlib J. Avapritinib in patients with Advanced Systemic Mastocytosis (AdvSM): Efficacy and safety analyses from the Phase 2 PATHFINDER study with 2‑year follow‑up. In. Available from: https://clml-soho2023.elsevierdigitaledition.com/388/index.html.
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl J Med. 2017;377:454–64.
Lübke J, Naumann N, Metzgeroth G, Kreil S, Brand T, Horny HP, et al. Response and resistance to cladribine in patients with advanced systemic mastocytosis: a registry-based analysis. Ann Hematol. 2023;102:2077–85.
Wrzesień‐Kuś A, Robak T, Lech‐Marańda E, Wierzbowska A, Dmoszyńska A, Kowal M, et al. A multicenter, open, non‐comparative, phase II study of the combination of cladribine (2‐chlorodeoxyadenosine), cytarabine, and G‐CSF as induction therapy in refractory acute myeloid leukemia – a report of the Polish Adult Leukemia Group (PALG). Eur J Haematol. 2003;71:155–62.
DeAngelo DJ, Pullarkat V, Piris-Villaespesa M, George TI, Patel JL, Ustun C, et al. P1049: A phase 2 study of Bezuclastinib (CGT9486), A novel, highly selective, potent KIT D816V, inhibitor in adults with advanced systemic mastocytosis (APEX): Methods, baseline data, and early insights. HemaSphere. 2022;6:939–40.
DeAngelo DJ, Reiter A, George TI, Radia DH, Devlin M, Dimitrijević S, et al. AZURE: A phase 1/2 study of BLU-263 as monotherapy and in combination with Azacitidine in PATIENTS WITH ADVANCED SYSTEMIC Mastocytosis. Blood. 2022;140:6877–8.
Yakoub-Agha I, Greco R, Onida F, De La Cámara R, Ciceri F, Corbacioglu S, et al. Practice harmonization workshops of EBMT: an expert-based approach to generate practical and contemporary guidelines within the arena of hematopoietic cell transplantation and cellular therapy. Bone Marrow Transpl. 2023;58:696–700.
Jawhar M, Schwaab J, Álvarez-Twose I, Shoumariyeh K, Naumann N, Lübke J, et al. MARS: Mutation-adjusted risk score for advanced systemic mastocytosis. J Clin Oncol. 2019;37:2846–56.
Naumann N, Lübke J, Baumann S, Schwaab J, Hoffmann O, Kreil S, et al. Adverse prognostic impact of the KIT D816V Transcriptional Activity in Advanced Systemic Mastocytosis. Int J Mol Sci. 2021;22:2562.
Patnaik, Rangit Vallapureddy MM, Lasho TL, Hoversten KP, Finke CM, Ketterling RP, et al. A comparison of clinical and molecular characteristics of patients with systemic mastocytosis with chronic myelomonocytic leukemia to CMML alone. Leukemia. 2018;32:1850–6.
Sotlar K, Colak S, Bache A, Berezowska S, Krokowski M, Bültmann B, et al. Variable presence of KIT D816V in clonal haematological non-mast cell lineage diseases associated with systemic mastocytosis (SM-AHNMD). J Pathol. 2010;220:586–95.
Jawhar M, Döhner K, Kreil S, Schwaab J, Shoumariyeh K, Meggendorfer M, et al. KIT D816 mutated/CBF-negative acute myeloid leukemia: a poor-risk subtype associated with systemic mastocytosis. Leukemia. 2019;33:1124–34.
Valent P, Sotlar K, Sperr WR, Escribano L, Yavuz S, Reiter A, et al. Refined diagnostic criteria and classification of mast cell leukemia (MCL) and myelomastocytic leukemia (MML): a consensus proposal. Ann Oncol. 2014;25:1691–700.
Kennedy VE, Perkins C, Reiter A, Jawhar M, Lübke J, Kluin-Nelemans HC, et al. Mast cell leukemia: clinical and molecular features and survival outcomes of patients in the ECNM Registry. Blood Adv. 2023;7:1713–24.
Heiblig M, Gourguechon C, Guilpain P, Livideanu CB, Barete S, Agopian J, et al. Prognostic characterization of advanced mastocytosis patients treated with Midostaurin according to diagnosis and mutation-adjusted risk score: a nation-wide Ceremast Study of 170 patients. Blood. 2023;142:1837.
Gotlib J, Radia DH, George TI, Robinson WA, Quiery AT, Drummond MW, et al. Pure pathologic response is associated with improved overall survival in patients with advanced systemic mastocytosis receiving Avapritinib in the Phase I EXPLORER Study. Blood. 2020;136:37–8.
Snowden JA, Sánchez-Ortega I, Corbacioglu S, Basak GW, Chabannon C, De La Camara R, et al. Indications for haematopoietic cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2022. Bone Marrow Transpl. 2022;57:1217–39.
Kanate AS, Majhail NS, Savani BN, Bredeson C, Champlin RE, Crawford S, et al. Indications for hematopoietic cell transplantation and immune effector cell therapy: Guidelines from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transpl. 2020;26:1247–56.
Sriskandarajah P, McLornan DP, Oni C, Wilson A, Woodley C, Ciesielska M, et al. Advanced Systemic Mastocytosis with associated haematological neoplasm: treatment with avapritinib can facilitate successful bridge to allogeneic haematopoietic cell transplant. Curr Res Transl Med. 2023;71:103398.
Degenfeld-Schonburg L, Gamperl S, Stefanzl G, Schruef AK, Sadovnik I, Bauer K, et al. Antineoplastic efficacy profiles of avapritinib and nintedanib in KIT D816V+ systemic mastocytosis: a preclinical study. Am J Cancer Res. 2023;13:355–78.
Krauth M‐T, Mirkina I, Herrmann H, Baumgartner C, Kneidinger M, Valent P. Midostaurin (PKC412) inhibits immunoglobulin E‐dependent activation and mediator release in human blood basophils and mast cells. Clin Exp Allergy. 2009;39:1711–20.
Cavazos K, Eswaran S, Maidlow C, Keklik Karadag F, Idilman R, Idilman I, et al. Liver fibrosis and its response to avapritinib in 2 patients with systemic mastocytosis. Blood Adv. 2022;6:5630–3.
Ustun C, Smith A, Cayci Z, Courville EL, Corbacioglu S, Akin C, et al. Allogeneic hematopoietic cell transplantation in systemic mastocytosis: is there a high risk for veno‐occlusive disease? Eur J Haematol. 2016;96:655–7.
Sperr WR, Drach J, Hauswirth AW, Ackermann J, Mitterbauer M, Mitterbauer G, et al. Myelomastocytic leukemia: evidence for the origin of mast cells from the leukemic clone and eradication by allogeneic stem cell transplantation. Clin Cancer Res. 2005;11:6787–92.
Martynova A, Nael A, O’Neill C, Ramsingh G, Merchant A, Yaghmour B, et al. Aggressive systemic mastocytosis: midostaurin is safe, feasible and associated with durable response post‐haploidentical allogeneic stem cell transplant. Br J Haematol. 2019;186:e139–e141. https://onlinelibrary.wiley.com/doi/10.1111/bjh.15980.
Spyridonidis A, Thomas AK, Bertz H, Zeiser R, Schmitt-Gräff A, Lindemann A, et al. Evidence for a graft-versus-mast-cell effect after allogeneic bone marrow transplantation. Bone Marrow Transpl. 2004;34:515–9.
Hägglund H, Yavuz AS, Dreimane A, Malm C, Sundin A, Sander B, et al. Graft-versus-mastocytosis effect after donor lymphocyte infusion: Proof of principle. Eur J Haematol. 2021;106:290–3.
Author information
Authors and Affiliations
Contributions
DPM, DR, ISO, RG, FO and IYA designed the initial project concept. DPM, TC, GD, ME, CG, JHB, NP, JS, KS, IYA, ISO and DHR met for the two-day in-person workshop meeting in Lille. GB, CE, JG, AR, JR, CU and PV gave expert opinions on the first drafts, and wrote sections and summary points of topics raised. All authors contributed to the subsequent consensus development, contributed by writing sections and reviewing the article drafts. All authors reviewed and agreed on the final draft and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
There was no external funding associated with this consensus-based expert opinion paper. For each individual author, declarations of interest are as below: Donal P McLornan: Advisory boards and research funding from Novartis. Educational events on behalf of Novartis. Tomasz Czerw: No relevant disclosures. Gandhi Damaj: Travel expenses from Novartis and speakers bureau/ advisory boards on behalf of Blueprint Medicines Corporation. Mark Ethell: No relevant disclosures. Carmelo Gurnari: No relevant disclosures. Juan Carlos Hernández-Boluda: No relevant disclosures. Nicola Polverelli: No relevant disclosures. Juliana Schwaab: No relevant disclosures. Katja Sockel: Advisory boards and received lecture fees from Novartis, BMS/Celgene and Blueprint Medicines Corporation. Raffaella Greco: Discloses speaking honoraria from Biotest, Pfizer, Medac, Neovii and Magenta. Francesco Onida: No relevant disclosures. Isabel Sánchez-Ortega: No relevant disclosures. Giorgia Battipaglia: No relevant disclosures. Chiara Elena: Advisory Boards for Cogent Biosciences, Blueprint Medicines Corporation, Istituto Gentili. Jason Gotlib: Incyte: Consultancy, Honoraria, Research Funding; Deciphera: Consultancy, Honoraria, Research Funding; PharmaEssentia: Consultancy, Honoraria, Research Funding; Blueprint Medicines Corporation: Consultancy, Honoraria, Research Funding; Kartos: Honoraria, Advisory committees, Research Funding; BMS: Research Funding; Abbvie: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Novartis: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Cogent Biosciences: Consultancy, Research Funding; Allakos: Consultancy, Membership on an entity’s Board of Directors or advisory committees, Research Funding. Andreas Reiter: AbbVie: Consultancy, Honoraria, Research Funding; Blueprint Medicines Corporation: Consultancy, Honoraria, Research Funding; AOP Orphan Pharmaceuticals: Consultancy, Honoraria, Research Funding, Incyte Corporation: Consultancy, Honoraria, Research Funding; BMS: Consultancy, Honoraria, Research Funding; GSK: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding. Julien Rossignol: served on an advisory board for Blueprint Medicines Corporation; and has received research grants from Blueprint Medicines Corporation, BMS, and Novartis. Celalettin Ustun: Speaker Bureau honoraria: Takeda and Blueprint Medicines Corporation. Peter Valent: Project-Related: none. Project-Independent but Related to Mastocytosis in General: Ad-Board Honoraria: Novartis, Blueprint Medicines Corporation, Cogent. Ibrahim Yakoub-Agha: No relevant disclosures. Deepti H Radia: Clinical advisory board/study steering group member (EXPLORER/PATHFINDER) for Blueprint Medicines Corporation; a study steering committee member for Cogent Biosciences; and involved in educational events and advisory boards for Novartis. Author fees for Medscape cases. Royalties for Fast Facts: Systemic Mastocytosis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McLornan, D.P., Czerw, T., Damaj, G. et al. Allogeneic haematopoietic cell transplantation for advanced systemic mastocytosis: Best practice recommendations on behalf of the EBMT Practice Harmonisation and Guidelines Committee. Leukemia 38, 699–711 (2024). https://doi.org/10.1038/s41375-024-02182-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-024-02182-1