Abstract
We identified 71 patients with AdvSM (aggressive SM [ASM], SM with an associated hematologic neoplasm [SM-AHN, e.g., acute myeloid leukemia, SM-AML], mast cell leukemia [MCL]) in two national registries (DRST/GREM) who received an allogeneic hematopoietic cell transplantation (alloHCT) performed in Germany from 1999–2021. Median overall survival (OS) of ASM/SM-AHN (n = 30, 45%), SM-AML (n = 28, 39%) and MCL ± AHN (n = 13, 19%) was 9.0, 3.3 and 0.9 years (P = 0.007). Improved median OS was associated with response of SM (17/41, 41%; HR 0.4 [0.2–0.9], P = 0.035) and/or of AHN (26/43, 60%, HR 0.3 [0.1–0.7], P = 0.004) prior to alloHCT. Adverse predictors for OS included absence of KIT D816V (10/61, 16%, HR 2.9 [1.2–6.5], P < 0.001) and a complex karyotype (9/60, 15%, HR 4.2 [1.8–10.0], P = 0.016). HLA-match, conditioning type or transplantation at centers reporting above-average alloHCTs (≥7) had no impact on OS. Taking into account competing events at years 1, 3 and 5, relapse-related mortality and non-relapse mortality rate were 15%/23%, 20%/30% and 23%/35%, respectively. Irrespective of subtype, subsequent treatment response was achieved in 13/30 (43%) patients and was highest on midostaurin/avapritinib (7/9, 78%). We conclude that outcome of alloHCT in AdvSM is more affected by disease phenotype and treatment response prior to transplant than by transplant characteristics.
Similar content being viewed by others
Introduction
Systemic mastocytosis (SM) is characterized by accumulation of clonal, neoplastic mast cells within the bone marrow and additional organ systems, e.g., skin and gastrointestinal tract [1, 2]. Advanced systemic mastocytosis (AdvSM) comprises aggressive systemic mastocytosis (ASM), SM with an associated hematologic or myeloid neoplasm (SM-AHN/SM-AMN) according to World Health Classification (WHO)-HAEM5 or International Consensus Classification (ICC), respectively, and mast cell leukemia (MCL) ± AHN as the most aggressive subtype impacting on overall survival (OS) [3, 4]. In >90% of patients, a somatic point mutation in KIT at codon 816 (KIT D816V) is the primary disease driver [5,6,7]. In AdvSM, 60–80% of patients harbor additional somatic mutations, some of which confer an adverse impact on prognosis, e.g., mutations in SRSF2, ASXL1, RUNX1 (S/A/R gene panel), EZH2, JAK2, and others [8,9,10,11,12].
In addition to conventional chemotherapy, e.g. to the purine analog cladribine [13,14,15,16], the recent development of targeted treatments, e.g. with the multikinase/KIT inhibitor midostaurin [17,18,19,20,21] or the specific KIT D816V inhibitor avapritinib, has substantially extended therapeutic alternatives [22,23,24,25]. However, with data from only one larger retrospective analysis on 57 patients available, timing, type of conditioning and post-transplant strategies of allogeneic hematopoietic cell transplantation (alloHCT) as the only curative treatment option remain elusive so far [26]. The advent of reduced intensity conditioning (RIC) [27] and alternate donor sources (e.g. haploidentical alloHCT) [28, 29], have expanded the availability of alloHCT to an increasing number of patients. However, outcome of alloHCT is affected by relapse and non-relapse morbidity and mortality (NRM).
We therefore sought to retrospectively analyze the impact of baseline characteristics, response status and various transplant settings on response, progression-free (PFS) and overall survival (OS) after alloHCT in patients with diagnosis of AdvSM and enrollment within the ‘German Stem Cell Transplantation Registry’ (DRST) or the ‘German Registry on Eosinophils and Mast Cells’ (GREM).
Methods
Data collection
The study cohort consisted of 71 patients who had undergone alloHCT for AdvSM in 20 German transplant centers between 1999 and 2021 accumulating into a 372 and 211 patient-years overall follow-up period since time of diagnosis and start of alloHCT, respectively. Patient data were collected from the DRST (n = 65) with additional data from the GREM (n = 6). Nine patients (8%) were previously reported by Ustun et al. [26]. Data collection from the registries was performed by query of ´SM + alloHCT‘ in June 2022. Eligibility criteria included: (i) diagnosis of ASM, SM-AHN, SM with an acute myeloid leukemia (AML) as subtype of SM-AHN or MCL ± AHN according to the WHO-HAEM5 criteria, (ii) alloHCT and (iii) enrollment in either the DRST and/or GREM registry (Fig. 1). Following approval from the respective institutional research boards, we collected transplant data from MED-A forms, and contacted the participating centers to obtain additional information on patients’ diagnosis, specific parameters of SM, e.g. bone marrow (BM) mast cell (MC) infiltration, serum tryptase level, KIT D816V variant allele frequency (VAF), treatment prior to and after alloHCT, and outcome data (response, PFS and OS). Individual information was collected pseudo-anonymously using a data collection form, and transferred to the data collection centers (University Hospitals Aachen and Mannheim). The mastocytosis reference and transplant centers Aachen and Mannheim carried out a post-hoc manual review of the data for identification of inconsistencies and outliers, which were confirmed or revised in collaboration with the reporting center. Classification of conditioning regimes in myeloablative (MAC) or reduced intensity conditioning (RIC) regimes followed proposed definitions based on the duration of cytopenia and need of stem cell support [30]. Informed patient consent was given by all patients via the two registries. The study design adhered to the principles outlined in the Declaration of Helsinki and was approved by the ethics committee of the Medical Faculties Aachen and Mannheim (Germany).
Study endpoints
Primary study endpoints included PFS and OS defined as time from date of alloHCT to date of progression of the SM and/or the AHN component, death or date of last follow-up (if progression-free) and time from date of alloHCT to death or date of last follow-up (if alive), relapse-related mortality (RRM) and NRM. Secondary endpoints included changes in the BM MC infiltration, serum tryptase levels, and KIT D816V VAF. Exploratory endpoints considered type, number of lines and principal investigator-assessed response to treatment prior to and after alloHCT, assessed qualitatively (response vs. non-response), and reviewed by the data collection center. Due to the limitations of retrospective, multicentric data collection, standardized response criteria such as the modified Valent criteria, International Working Group-Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) ECNM criteria or Pure Pathological Response criteria could not be utilized [20, 31,32,33].
Statistical analysis
Statistical analyses performed on clinical, laboratory and molecular parameters were obtained at the time of diagnosis/first referral to the servicing center and throughout the disease course. Continuous variables were analyzed for statistical differences using the Student’s t-test. If the values were not normally distributed, a Wilcoxon rank-sum test was employed. For categorical variables, Fisher’s exact test was used. For the estimation of hazard ratios (HRs) and multivariable analyses, the cox proportional hazard regression model was used. Only variables that demonstrated statistical significance in univariate analyses were incorporated into the multivariable model. Survival probabilities (PFS and OS) were calculated by the Kaplan-Meier Method and compared by the log-rank test. The proportional hazards assumption was tested by the correlation of scaled Schoenfeld residuals with time. The cumulative incidence function was used to account for the presence of competing risks (RRM vs. NRM). In this hypothesis-driven, retrospective data set, analyses were not specifically powered for direct comparisons. In general, a test result with P less than .05 was considered as statistically significant. Statistical analyses were performed using R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria), SPSS version 29.0.1 (IBM Corporation, Armonk, NY) and GraphPad Prism version 10.1.1 software (GraphPad Software Inc., San Diego, CA, USA).
Results
Patient characteristics
At time of alloHCT, the median patient age was 59 years (range 21-84), with the majority of patients (49/71, 69%) being male. The median time between diagnosis of AdvSM and alloHCT was 1.2 (range 0.1-16.7) years. The Karnofsky performance score at time of alloHCT was ≥90% in 37/63 (59%) patients. The most common subtype close to alloHCT was ASM/SM-AHN in 30/71 (42%; ASM, n = 4, 6%; SM-AHN, n = 26, 37%), followed by SM-AML (Table S1) in 28/71 (39%, 18/28 [64%] with secondary AML) and MCL ± AHN (Table S2) in 13/71 (18%, 3/13 [23%] with secondary MCL). Diagnoses of (secondary) AML and MCL were mutually exclusive.
The detailed clinical characteristics of the various cohorts are reported in Table 1. Differences included significantly higher levels of BM MC infiltration (median 80% [range 30–100], P < 0.001) and numerically higher serum tryptase levels (median 429 µg/L [range 61–2660], P = 0.076) in MCL ± AHN while the relative frequency of the KIT D816V mutation (7/13, 54%, P < 0.001; Table S3) and of additional somatic mutations in S/A/R (2/10, 20%, P = 0.023) was significantly lower. The presence of an aberrant karyotype [23/62, 37%, including 2 patients with a t(8;21)(q22;q22)] was clustered in SM-AML (15/27, 56%, P = 0.008).
An upfront alloHCT (median time between AdvSM diagnosis and alloHCT 1.4 years, range 0.1–3.7) without prior SM- or AHN-directed treatment was performed in 9/71 (13%) patients (Table S4). All other patients received a median of 2 (range 1–5) treatment lines prior to alloHCT. Tyrosine kinase inhibitors (TKI) including midostaurin and avapritinib were less frequently used in SM-AML (9/28, 32%) than in ASM/SM-AHN (14/30, 47%, P = 0.259) or MCL ± AHN (12/13, 92%, P = 0.005) (Table 1).
Transplant characteristics
Peripheral blood was used as graft source in 67/71 (94%), BM in 4/71 (6%) patients. Detailed donor information was available in 62/71 (87%) patients: 17 (27%) patients received a graft from an HLA-matched (10/10) related donor, 1 (2%) an HLA-mismatched related graft, 25 (40%) an HLA-matched (10/10) unrelated, 12 (19%) an HLA-mismatched unrelated, and 7 (11%) a related haploidentical graft. Overall, 24 different conditioning regimens were utilized with myeloablative conditioning accounting for 43/69 (62%) and reduced-intensity conditioning for 26/69 (38%) patients (Table S5). The most frequently administered conditioning regime consisted of fludarabine and treosulfan or fludarabine and TBI (each 9/68, 13%), followed by busulfan and cyclophosphamide (7/68, 10%).
Total body irradiation as part of the conditioning regimen, varying between 2 and 12 Gy ( ≥ 8 Gy, 11/17, 65%), was included in 17/69 (25%) patients (Table S6). The median time to neutrophil engraftment ( ≥ 0.5/nL) was 18 days (range 1–57). Primary graft failure was reported in two patients. Data about chimerism were available in 43/71 (61%) patients. Complete donor chimerism was achieved in 36/43 (84%) patients. Acute (grade I to IV) and chronic (mild to severe) GvHD occurred in 34/67 (51%) and 16/52 (31%) patients, respectively (Table 2).
Transplant outcome
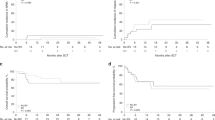
For the entire cohort, the median time of follow-up was 1.4 years (range 0–20.4). PFS and OS for all patients were 52% (standard deviation [SD] ± 6.1%) and 62% (SD ± 5.9%) at 1 year, and 39% (SD ± 6.3%) and 50% (SD ± 6.2%) at 3 years, respectively. Primary diagnosis of ASM/SM-AHN vs. SM-AML vs. MCL ± AHN delineated a three-tier risk stratification (median PFS, 4.5 vs. 0.7 vs. 0.3 years, P < 0.001, Fig. 2A; median OS, 9.0 vs. 3.3 vs. 0.9 years, P = 0.007, Fig. 2B). Median relative decreases in BM MC infiltration (−79% [range −100 to +233]), serum tryptase levels (−78% [range −99 to +385]) and KIT D816V VAF (-100% [range −100 to +10]) prior to post-alloHCT were not statistically different between the three subgroups (Fig. 3).
A Kaplan–Meier estimates of progression-free survival (PFS) and B overall survival (OS) depending on their most advanced disease subtype prior allogeneic stem cell transplantation (alloHCT). C Cumulative incidence function of relapse-related mortality and non-relapse mortality. ASM aggressive systemic mastocytosis, MCL±AHN mast cell leukemia with/without an associated hematologic neoplasm, SM-AHN systemic mastocytosis with an associated hematologic neoplasm, SM-AML systemic mastocytosis with an acute myeloid leukemia.
Waterfall plots of A bone marrow (BM) mast cell infiltration, B serum tryptase and C KIT D816V variant allele frequency in all available patients (relative changes prior to post alloHCT). A systemic mastocytosis with an acute myeloid leukemia, alloHCT allogeneic stem cell transplantation, AHN associated hematologic neoplasm, H systemic mastocytosis with/without an associated hematologic neoplasm (except AML), M mast cell leukemia with/without an associated hematologic neoplasm, SM systemic mastocytosis.
Taking into account competing events at years 1, 3, and 5, the RRM and the NRM rate was 15%/23%, 20%/30% and 23%/35%, respectively. Reasons for NRM included infections, GvHD, organ toxicity (cardiotoxicity) and combinations/not further specified in 8/22 (36%), 1/22 (5%), 1/22 (5%) and 11/22 (50%) patients, respectively. No statistical differences were observed in RRM (P = 0.400) and NRM (P = 0.200) based on the subtype of AdvSM (Fig. 2C, Table S7).
Predictors of transplant outcome
Univariate analysis revealed that PFS after alloHCT was adversely impacted by diagnosis of MCL ± AHN (HR 3.5 [95% CI 1.7–7.5], P < 0.001), absence of a KIT D816V mutation (HR 2.5 [95% CI 1.2–5.4], P = 0.021), presence of a complex karyotype (HR 3.0 [95% CI 1.4–6.6], P = 0.006) and absence of the use of TKI prior to alloHCT (HR 0.5 [95% CI 0.2-0.9], P = 0.014). Multivariable analysis revealed the absence of the use of TKI prior to alloHCT (HR 2.8 [95% CI 1.3–5.9], P = 0.007) and a complex karyotype (HR 3.3 [95% CI 1.5–7.2], P = 0.004) as independent predictors for PFS.
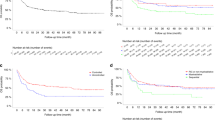
An adverse impact on OS was unveiled by univariate analyses upon lack of response on SM (response in 17/41, 41%; median OS 4.6 vs. 1.1 years; HR 2.5 [95% CI 1.1–6.0], P = 0.035) or AHN (response in 26/43, 60%, median OS not reached vs. 0.4 years; HR 0.302 [95% CI 0.132–0.687], P = 0.004) prior to alloHCT (Fig. 4). Transplant-associated OS was further adversely associated by the absence of a KIT D816V mutation (HR 2.8 [95% CI 1.2–6.5], P = 0.016) and a complex karyotype (HR 4.2 [95% CI 1.8–10.0], P = 0.001). Multivariable analysis revealed the lack of AHN response prior to alloHCT (HR 4.082 [95% CI 1.7–9.8], P = 0.002) and a complex karyotype (HR 8.0 [95% CI 2.3–27.1], P = 0.016) as independent adverse prognostic factors for OS.
A Response status (investigator-assessed) prior to allogeneic stem cell transplantation (alloHCT) regarding the systemic mastocytosis (SM) and associated hematologic neoplasm (AHN) compartment. B Kaplan–Meier estimates of overall survival (OS) depending on response status prior to alloHCT. AML acute myeloid leukemia, MCL mast cell leukemia, NonR nonresponse, R response.
HLA-matching (complete vs. incomplete), type of conditioning (myeloablative vs. dose-reduced intensity), the use of total body irradiation ( ≥ 8 Gy yes vs. no), transplantation at a center with an above-average number of alloHCT in AdvSM patients (center performed and reported ≥7 alloHCTs for AdvSM yes vs. no) or a transplantation in the year 2010 or later (Table S8) were not associated with differences in PFS or OS (Table 3).
Posttransplant treatment
During or after alloHCT, 30/71 (42%) patients showed either refractory (9/30, 30%) or relapsed (21/30, 70%; r/r) disease which was highest in MCL ± AHN (11/13, 85%) vs. ASM/SM-AHN (9/30, 30%) and SM-AML (10/28, 36%; P = 0.002). Primary refractory disease was predominantly observed in MCL ± AHN (8/9, 89%) vs. SM-AML (1/9, 11%) and ASM/SM-AHN, 0/9, 0%; (P < 0.001). The median time to relapse was 0.6 years (range 0.1–4.5) which was more frequent in ASM/SM-AHN (9/21, 43%) and SM-AML (9/21, 43%) vs. MCL ± AHN (3/21, 14%). Considering the two disease components, r/r SM was predominantly observed in MCL ± AHN (10/11, 91%), r/r AHN was higher in SM-AML (6/10, 60%) and ASM/SM-AHN (5/9, 56%).
Overall, 52 treatment lines have been applied in the r/r setting post-alloHCT with a median number of 2 (range 0–4) lines per individual patient. At least one treatment line was applied in 24/30 (80%) patients. Midostaurin/avapritinib, cladribine or other cytoreductive therapies were used in 9/30 (30%), 3/30 (10%) and 14/30 (47%) patients, respectively (Table 4). Donor lymphocyte infusions were applied in 18/30 (60%) patients (ASM/SM-AHN, 7/9, 78%; SM-AML, 7/10, 70%, MCL ± AHN, 4/11, 36%) while a second alloHCT was performed in 2/30 (7%) patients (both SM-AML). A response to treatment regimens after alloHCT was achieved in 13/30 (43%) patients (ASM/SM-AHN, 3/9, 33%, SM-AML, 5/10, 50%; MCL ± AHN, 5/11, 45%) and was highest in 9 patients receiving midostaurin and/or avapritinib (7/9, 78%).
Discussion
Despite the availability and efficacy of KIT targeted therapies, alloHCT remains the only curative treatment option for patients with AdvSM. Our data show that primary disease phenotype, karyotype and endpoints assessed during follow-up such as level of response as well as primary or secondary resistance are critical for outcome of subsequently performed alloHCT. So far, a retrospective multicenter analysis from 2014 including 57 patients (transplanted between 1990 and 2013) represents the only available data collection demonstrating a potential curative benefit of alloHCT in AdvSM [26]. Applying these reported findings into current clinical practice remains however challenging given the increasing complex molecular landscape of AdvSM, the efficacy of KIT inhibitors such as midostaurin and avapritinib, and the continuous developments of transplant procedures, GvHD prophylaxis and supportive care strategies [18,19,20, 22,23,24,25, 34]. A prospective clinical trial in order to assess the best alloHCT strategy will most likely not be performed given the rarity and heterogeneity of AdvSM. Ongoing clinical trials of new KIT inhibitors such as bezuclastinib (NCT04996875) or elenestinib (NCT05609942) pose additional potential challenges on the evaluation of optimal alloHCT integration into the overall treatment concepts. However, in order to address some of the actual questions in regard to alloHCT in AdvSM patients we performed an updated retrospective multicenter study on 71 AdvSM patients who underwent alloHCT in Germany between 1999 and 2021 with 89% of patients transplanted after 2010.
As expected, substantial disparities were noted between the various AdvSM subtypes with a median OS of approximately 1 and 3 years observed in MCL ± AHN and SM-AML, respectively. The most inherent characteristics contributing to this unfavorable prognosis include the absence of KIT D816V in approximately 50% of MCL patients and the presence of an aberrant karyotype in 56% or a complex karyotype in 15% of patients with SM-AML. Surprisingly, PFS/OS was not adversely affected by established high-risk mutations (HRM) such as SRSF2, ASXL or RUNX1 [8, 10, 11, 18, 34, 35]. In ASM/SM-AHN patients, a median OS of nine years was seen after exclusion of MCL and AML. These data clearly indicates that alloHCT can overcome poor prognosis conferred by HRM in KIT D816V positive AdvSM at least if MCL or AML are absent.
Similar to AML [36,37,38] or ALL [39], response of the SM and/or the AHN compartment to treatment prior alloHCT significantly prolonged transplant-associated OS. Our data also show that for patients with resistant or progressive disease before alloHCT, this procedure might not be a reasonable rescue option as the graft-versus-AdvSM effect does not seem to be sufficiently effective in patients with high disease burden, a phenomenon known from other myeloid neoplasms [40,41,42]. To optimize outcome in AdvSM, transplant eligible patients should therefore be transplanted at time of best response to pre-allo treatment; hence, close interdisciplinary cooperation between mastocytosis and transplant centers is warranted to define these time points. The use of tyrosine kinase inhibitors such as midostaurin or avapritinib prior to alloHCT was significantly associated with improved PFS. The use of 24 different conditioning regimens in 71 AdvSM patients demonstrates the lack of a standardized approach for AdvSM patients despite consensus opinions [43, 44]. This inconsistency becomes even more impressive when we consider that all transplantations have been conducted within one country.
Even after adjusting for pre-alloHCT treatment responses (data not shown), updated analyses could not confirm the previously reported superiority of myeloablative conditioning over reduced intensity regimens in terms of PFS [26]. This again highlights the fact, that other parameters such as pre-alloHCT response seem to be more important than conditioning intensity. Therefore, future strategies for older or more fragile patients should prioritize achieving an optimal treatment response before considering alloHCT to employ reduced-intensity conditioning regimens successfully.
Posttransplant treatment was exclusively used in patients with r/r disease status. As expected, the relative frequency of r/r patients with 85% was highest in patients with MCL ± AHN with most of these patients (62%) already suffering from refractory disease prior to alloHCT. As pointed out before, the use of myeloablative conditioning was insufficient to overcome this mast cell resistance. While in approximately 50% of patients with r/r MCL ± AHN, a partial response was achieved on midostaurin (n = 1), DLI (n = 1) or avapritinib (n = 3), future strategies might focus on maintenance therapy or measurable residual disease-based pre-emptive approaches using effective TKIs, e.g. similar to strategies used in AML patients with FLT3 mutation [45].
A major limitation of this analysis is insufficient information on post-transplant quantification of residual disease including BM MC infiltration (24/71, 34%), serum tryptase levels (33/71, 47%) and KIT D816V VAF (48/71, 68%) not being available in a significant number of patients. This lack of data - even as chimerism analyses on BM aspirates were regularly performed - was particular predominant in patients in which the AHN compartment was the primary driver for the alloHCT concept, e.g. SM-AML [6, 9, 18]. In consequence, residual MC disease may be inadvertently overlooked during follow-up. The lack of attention in regard to the MC component post-alloHCT could be a significant disadvantage especially given the availability of potent MC-directed treatment options such as midostaurin and avapritinib [18,19,20, 46,47,48,49].
Similarities and differences between the cohort reported by Ustun et al. and the current cohort are at least partly related to changes in the real-world practice of alloHCT over a 10-years period between the two reports. For example, direct comparisons across the various subtypes were not possible because advanced morphologic and genetic characterization conferred into a higher relative frequency of AHN (87% vs. 67%) in the current cohort. Moreover, the number of cases allowed the separation of SM-AML from SM-AHN because it is characterized by an inherent disease phenotype and different clinical trajectory. In the current cohort, patients were older (median age 59 vs. 46 years) and the relative frequencies of unrelated (60% vs. 31%) or haploidentical donors (11% vs. 2%) were higher while the relative frequencies on the use of MAC regimens (62% vs. 63%) and TBI (24% vs. 28%) were similar. Rates of NRM were 23% (based on cumulative incidence function) and 20% after 1 year and the subtype-independent OS was approximately 60% and 50% after 1 and 3 years in both cohorts. In this respect, it should be emphasized that the poor prognosis of MCL (with or without AHN) has not markedly improved over the last decade.
In conclusion, alloHCT can confer long-term PFS/OS in patients with AdvSM, especially when alloHCT will be performed at time of optimal response. To achieve the maximum benefit from pre- and post-allogeneic strategies and from the transplant itself, collaborative efforts between mastocytosis experts and transplant centers are essential. Adequate monitoring of residual disease could provide valuable guidance for the pre-emptive use of KIT inhibitors post-transplant. The rapidly evolving landscape of AdvSM treatment necessitates continuous adaptation in integrating alloHCT into patient care. To facilitate upcoming comprehensive data analysis, the implementation of a uniform transplantation data collection form encompassing key elements relevant to the specific characteristics and heterogeneities of AdvSM and alloHCT is of utmost importance.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Valent P, Akin C, Hartmann K, Alvarez-Twose I, Brockow K, Hermine O, et al. Updated diagnostic criteria and classification of mast cell disorders: a consensus proposal. Hemasphere. 2021;5:e646.
Valent P, Horny HP, Escribano L, Longley BJ, Li CY, Schwartz LB, et al. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001;25:603–25.
Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36:1703–19.
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28.
Erben P, Schwaab J, Metzgeroth G, Horny HP, Jawhar M, Sotlar K, et al. The KIT D816V expressed allele burden for diagnosis and disease monitoring of systemic mastocytosis. Ann Hematol. 2014;93:81–8.
Naumann N, Lübke J, Baumann S, Schwaab J, Hoffmann O, Kreil S, et al. Adverse prognostic impact of the KIT D816V transcriptional activity in advanced systemic mastocytosis. Int J Mol Sci. 2021;22:2562.
Arock M, Sotlar K, Akin C, Broesby-Olsen S, Hoermann G, Escribano L, et al. KIT mutation analysis in mast cell neoplasms: recommendations of the European Competence Network on Mastocytosis. Leukemia. 2015;29:1223–32.
Jawhar M, Schwaab J, Alvarez-Twose I, Shoumariyeh K, Naumann N, Lübke J, et al. MARS: mutation-adjusted risk score for advanced systemic mastocytosis. J Clin Oncol. 2019;37:2846–56.
Jawhar M, Schwaab J, Naumann N, Horny HP, Sotlar K, Haferlach T, et al. Response and progression on midostaurin in advanced systemic mastocytosis: KIT D816V and other molecular markers. Blood. 2017;130:137–45.
Jawhar M, Schwaab J, Schnittger S, Meggendorfer M, Pfirrmann M, Sotlar K, et al. Additional mutations in SRSF2, ASXL1 and/or RUNX1 identify a high-risk group of patients with KIT D816V(+) advanced systemic mastocytosis. Leukemia. 2016;30:136–43.
Jawhar M, Schwaab J, Hausmann D, Clemens J, Naumann N, Henzler T, et al. Splenomegaly, elevated alkaline phosphatase and mutations in the SRSF2/ASXL1/RUNX1 gene panel are strong adverse prognostic markers in patients with systemic mastocytosis. Leukemia. 2016;30:2342–50.
Schwaab J, Schnittger S, Sotlar K, Walz C, Fabarius A, Pfirrmann M, et al. Comprehensive mutational profiling in advanced systemic mastocytosis. Blood. 2013;122:2460–6.
Lübke J, Naumann N, Metzgeroth G, Kreil S, Brand T, Horny HP, et al. Response and resistance to cladribine in patients with advanced systemic mastocytosis: a registry-based analysis. Ann Hematol. 2023;102:2077–85.
Tefferi A, Kittur J, Farrukh F, Begna KH, Patnaik MM, Al-Kali A, et al. Cladribine therapy for advanced and indolent systemic mastocytosis: Mayo Clinic experience in 42 consecutive cases. Br J Haematol. 2022;196:975–83.
Kluin-Nelemans HC, Oldhoff JM, Van Doormaal JJ, Van ‘t Wout JW, Verhoef G, Gerrits WB, et al. Cladribine therapy for systemic mastocytosis. Blood. 2003;102:4270–6.
Barete S, Lortholary O, Damaj G, Hirsch I, Chandesris MO, Elie C, et al. Long-term efficacy and safety of cladribine (2-CdA) in adult patients with mastocytosis. Blood. 2015;126:1009–16.
Singh A, Al-Kali A, Begna KH, Litzow MR, Larsen JT, Sher T, et al. Midostaurin therapy for advanced systemic mastocytosis: Mayo Clinic experience in 33 consecutive cases. Am J Hematol. 2022;97:630–7.
Lübke J, Schwaab J, Naumann N, Horny HP, Weiß C, Metzgeroth G, et al. Superior efficacy of midostaurin over cladribine in advanced systemic mastocytosis: a registry-based analysis. J Clin Oncol. 2022;40:1783–94.
DeAngelo DJ, George TI, Linder A, Langford C, Perkins C, Ma J, et al. Efficacy and safety of midostaurin in patients with advanced systemic mastocytosis: 10-year median follow-up of a phase II trial. Leukemia. 2018;32:470–8.
Gotlib J, Kluin-Nelemans HC, George TI, Akin C, Sotlar K, Hermine O, et al. Efficacy and safety of midostaurin in advanced systemic mastocytosis. N. Engl J Med. 2016;374:2530–41.
Chandesris MO, Damaj G, Canioni D, Brouzes C, Lhermitte L, Hanssens K, et al. Midostaurin in advanced systemic mastocytosis. N Engl J Med. 2016;374:2605–7.
Reiter A, Gotlib J, Álvarez-Twose I, Radia DH, Lübke J, Bobbili PJ, et al. Efficacy of avapritinib versus best available therapy in the treatment of advanced systemic mastocytosis. Leukemia. 2022;36:2108–20.
Reiter A, Schwaab J, DeAngelo DJ, Gotlib J, Deininger MW, Pettit KM, et al. Efficacy and safety of avapritinib in previously treated patients with advanced systemic mastocytosis. Blood Adv. 2022;6:5750–62.
DeAngelo DJ, Radia DH, George TI, Robinson WA, Quiery AT, Drummond MW, et al. Safety and efficacy of avapritinib in advanced systemic mastocytosis: the phase 1 EXPLORER trial. Nat Med. 2021;27:2183–91.
Gotlib J, Reiter A, Radia DH, Deininger MW, George TI, Panse J, et al. Efficacy and safety of avapritinib in advanced systemic mastocytosis: interim analysis of the phase 2 PATHFINDER trial. Nat Med. 2021;27:2192–9.
Ustun C, Reiter A, Scott BL, Nakamura R, Damaj G, Kreil S, et al. Hematopoietic stem-cell transplantation for advanced systemic mastocytosis. J Clin Oncol. 2014;32:3264–74.
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood. 1998;91:756–63.
Luznik L, O’Donnell PV, Fuchs EJ. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin Oncol. 2012;39:683–93.
Shouval R, Fein JA, Labopin M, Kröger N, Duarte RF, Bader P, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol. 2019;6:e573–84.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Gotlib J, Pardanani A, Akin C, Reiter A, George T, Hermine O, et al. International Working Group-Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) & European Competence Network on Mastocytosis (ECNM) consensus response criteria in advanced systemic mastocytosis. Blood 2013;121:2393–401.
Gotlib J, Schwaab J, Shomali W, George TI, Radia DH, Castells M, et al. Proposed European Competence Network on Mastocytosis-American Initiative in Mast Cell Diseases (ECNM-AIM) response criteria in advanced systemic mastocytosis. J Allergy Clin Immunol Pr. 2022;10:2025–38.e1.
Shomali W, Gotlib J. Response criteria in advanced systemic mastocytosis: evolution in the Era of KIT inhibitors. Int J Mol Sci. 2021;22:2983.
Jawhar M, Schwaab J, Naumann N, Kluger S, Horny H-P, Sotlar K, et al. Impact of molecular markers on response and resistance in midostaurin-treated patients with advanced systemic mastocytosis. Blood. 2016;128:945.
Lübke J, Naumann N, Kluger S, Schwaab J, Metzgeroth G, Evans E, et al. Inhibitory effects of midostaurin and avapritinib on myeloid progenitors derived from patients with KIT D816V positive advanced systemic mastocytosis. Leukemia. 2019;33:1195–205.
Buckley SA, Wood BL, Othus M, Hourigan CS, Ustun C, Linden MA, et al. Minimal residual disease prior to allogeneic hematopoietic cell transplantation in acute myeloid leukemia: a meta-analysis. Haematologica. 2017;102:865–73.
Anthias C, Dignan FL, Morilla R, Morilla A, Ethell ME, Potter MN, et al. Pre-transplant MRD predicts outcome following reduced-intensity and myeloablative allogeneic hemopoietic SCT in AML. Bone Marrow Transpl. 2014;49:679–83.
Walter RB, Gyurkocza B, Storer BE, Godwin CD, Pagel JM, Buckley SA, et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative allogeneic hematopoietic cell transplantation. Leukemia. 2015;29:137–44.
Woolfrey AE, Anasetti C, Storer B, Doney K, Milner LA, Sievers EL, et al. Factors associated with outcome after unrelated marrow transplantation for treatment of acute lymphoblastic leukemia in children. Blood. 2002;99:2002–8.
Sriskandarajah P, McLornan DP, Oni C, Wilson AJ, Woodley C, Ciesielska M, et al. Advanced systemic mastocytosis with associated haematological neoplasm: treatment with avapritinib can facilitate successful bridge to allogeneic haematopoietic cell transplant. Curr Res Transl Med. 2023;71:103398.
de Witte T, Bowen D, Robin M, Malcovati L, Niederwieser D, Yakoub-Agha I, et al. Allogeneic hematopoietic stem cell transplantation for MDS and CMML: recommendations from an international expert panel. Blood. 2017;129:1753–62.
Jentzsch M, Geus U, Grimm J, Vucinic V, Pönisch W, Franke GN, et al. Pretreatment CD34(+)/CD38(-) cell burden as prognostic factor in myelodysplastic syndrome patients receiving allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2019;25:1560–6.
Ustun C, Gotlib J, Popat U, Artz A, Litzow M, Reiter A, et al. Consensus opinion on allogeneic hematopoietic cell transplantation in advanced systemic mastocytosis. Biol Blood Marrow Transpl. 2016;22:1348–56.
Gyurkocza B, Sandmaier BM. Conditioning regimens for hematopoietic cell transplantation: one size does not fit all. Blood. 2014;124:344–53.
Kreidieh F, Abou Dalle I, Moukalled N, El-Cheikh J, Brissot E, Mohty M, et al. Relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia: an overview of prevention and treatment. Int J Hematol. 2022;116:330–40.
Schwaab J, Cabral do OHN, Naumann N, Jawhar M, Weiß C, Metzgeroth G, et al. Importance of adequate diagnostic work-up for correct diagnosis of advanced systemic mastocytosis. J Allergy Clin Immunol Pract. 2020;8:3121–27.
Jawhar M, Schwaab J, Horny HP, Sotlar K, Naumann N, Fabarius A, et al. Impact of centralized evaluation of bone marrow histology in systemic mastocytosis. Eur J Clin Invest. 2016;46:392–7.
DeAngelo DJ, Quiery AT, Radia D, Drummond MW, Gotlib JR, WA, Hexner E, et al. Clinical activity in a Phase 1 study of BLU-285, a potent, highly-selective inhibitor of KIT D816V in advanced systemic mastocytosis. American Society of Hematology Annual Meeting, Atlanta. 2017.
Gotlib J. World Health Organization-defined eosinophilic disorders: 2017 update on diagnosis, risk stratification, and management. Am J Hematol. 2017;92:1243–59.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
JL and DC have assessed and verified the data. JL, DC, AR and JP contributed to concept and design. JL, DC, AR and JP were involved in acquisition of data. JL and DC contributed to statistical analysis. JL, DC, JS, EJ, AR and JP were involved in interpretation of data. All authors were involved in manuscript writing. All authors contributed to critical revision of the manuscript and for important intellectual content. All authors read and approved the final manuscript. All authors are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
DC received consulting fees from Blueprint Medicines, Novartis, Pfizer and BeiGene, honoraria from Blueprint Medicines, Novartis and AstraZeneca and travel support from Amgen and Janssen. JS received consulting fees from Blueprint Medicines and GlaxoSmithKline, honoraria from Blueprint Medicines, GlaxoSmithKline and Novartis and research funding from GlaxoSmithKline. KS received consulting fees from Blueprint Medicines, honoraria from Astra Zeneca and Novartis and participated in the speakers bureau of BMS. MJ received consulting fees from Novartis and honoraria from Amgen, Blueprint Medicines, BMS, Jazz Pharmaceuticals, Novartis and Pfizer. KS received consulting fees and honoraria from Blueprint Medicines, BMS and Novartis, lecture fees from GlaxoSmithKline and research support from Active Biotech. IK received consulting fees from Novartis, honoraria from AbbVie, Medac, Novartis and Takeda and travel support from Medac, Amgen, BeiGene, Jazz Pharmaceuticals, Janssen and Fondation Internationale Menarini. ES received consulting fees from Jazz Pharmaceuticals, BMS, Kite Gilead and Takeda, honoraria from Jazz Pharmaceuticals, BMS, Kite Gilead and Novartis and support for meeting attendance from Jazz Pharmaceuticals and Kite Gilead. SS received honoraria from Prothena, Janssen, Takeda and Pfizer, research funding from Prothena, Janssen and Sanofi and travel support from Prothena, Janssen, Celgene, Binding Site and Jazz Pharmaceuticals. MR received honoraria from BMS, Novartis, Takeda, Incyte, Corat, Cogent Biosciences, TEVA, Otsuka, Lilly, Abbvie, Pfizer, Beigene and GlaxoSmithKline, research funding from Novartis and travel support from BMS, Novartis, Abbvie, Jazz Pharmaceuticals, Daiichi Sankyo, Amgen, Astellas, SOBI and AOP. THB received consulting fees from Gilead, Janssen, Merck, Novartis and Pfizer, honoraria from Janssen, Merck and Novartis, research funding from Novartis and Pfizer, participated in the speakers bureaus of Gilead, Janssen, Merck, Novartis and Pfizer and was paid for patents and royalties from Novartis. SK received honoraria from Amgen. EJ received honoraria from BMS, Jazz Pharmaceuticals and Amgen and travel support from Medac. AR received consulting fees, honoraria and research funding from Abbvie, AOP Orphan Pharmaceuticals, Blueprint Medicines Corporation, BMS, GlaxoSmithKline, Incyte and Novartis and was member on an entity’s Board of Directors or advisory committees of Abbvie, AOP Orphan Pharmaceuticals, Blueprint Medicines, BMS, GSK, Incyte and Novartis. JP received consulting fees from Amgen, Apellis Pharmaceuticals, BMS, MSD and Sanofi and was member on an entity’s Board of Directors or advisory committees and Speakers Bureau of Alexion, AstraZeneca Rare Disease, Boehring Ingelheim, Blueprint Medicines, Novartis, Pfizer, Samsung Bioepis, SOBI and F. Hoffmann-La Roche Ltd. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lübke, J., Christen, D., Schwaab, J. et al. Allogeneic Hematopoietic Cell Transplantation in Advanced Systemic Mastocytosis: A retrospective analysis of the DRST and GREM registries. Leukemia 38, 810–821 (2024). https://doi.org/10.1038/s41375-024-02186-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-024-02186-x