Abstract
Objective
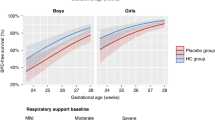
To compare survival without BPD among extremely preterm infants (EPI) who received prophylactic early low-dose hydrocortisone (PEH) with those who did not (non-PEH).
Study design
This single-center retrospective study compared risk-adjusted rates of survival without BPD, BPD, bowel perforation, and late-onset sepsis among infants (22–27 weeks’ gestation at birth) who received PEH (n = 82) and who did not (n = 205).
Results
Infants in the PEH group were of lower gestational age, lower birthweight, and higher day-1 risk of death/BPD. After adjusting for risk of death/BPD, PEH-treated infants demonstrated increased survival without BPD (aOR 2.04, 95%CI 1.1–3.7), and lower BPD rates (aOR 0.46, 95%CI 0.25–0.87). Importantly, bowel perforation or sepsis rate were similar among both groups.
Conclusion
After risk adjustment, PEH-treated infants demonstrated improved survival without BPD and did not increase rates of bowel perforation or sepsis. In our cohort of infants, PEH was safe and effective among the sickest preterm neonates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, et al. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013-2018. JAMA. 2022;327:248–63.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2007;357:1946–55.
Day CL, Ryan RM. Bronchopulmonary dysplasia: new becomes old again! Pediatr Res. 2017;81:210–13.
DeMauro SB. The Impact of Bronchopulmonary Dysplasia on Childhood Outcomes. Clin Perinatol. 2018;45:439–52.
Harris C, Morris S, Lunt A, Peacock J, Greenough A. Influence of bronchopulmonary dysplasia on lung function in adolescents who were born extremely prematurely. Pediatr Pulmonol. 2022;57:3151–7.
Van Marter LJ, Kuban KC, Allred E, Bose C, Dammann O, O’Shea M, et al. Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch Dis Child Fetal Neonatal Ed. 2011;96:F20–9.
Yallapragada SG, Savani RC, Goss KN. Cardiovascular impact and sequelae of bronchopulmonary dysplasia. Pediatr Pulmonol. 2021;56:3453–63.
Álvarez-Fuente M, Arruza L, Muro M, Zozaya C, Avila A, López-Ortego P, et al. The economic impact of prematurity and bronchopulmonary dysplasia. Eur J Pediatr. 2017;176:1587–93.
Gilfillan M, Bhandari A, Bhandari V. Diagnosis and management of bronchopulmonary dysplasia. BMJ. 2021;375:n1974.
Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183:1715–22.
Jensen EA, Foglia EE, Schmidt B. Evidence-Based Pharmacologic Therapies for Prevention of Bronchopulmonary Dysplasia: Application of the Grading of Recommendations Assessment, Development, and Evaluation Methodology. Clin Perinatol. 2015;42:755–79.
Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387:1827–36.
Shaffer ML, Baud O, Lacaze-Masmonteil T, Peltoniemi OM, Bonsante F, Watterberg KL. Effect of Prophylaxis for Early Adrenal Insufficiency Using Low-Dose Hydrocortisone in Very Preterm Infants: An Individual Patient Data Meta-Analysis. J Pediatr. 2019;207:136–42.e5.
Owen LS, Manley BJ, Davis PG, Doyle LW. The evolution of modern respiratory care for preterm infants. Lancet. 2017;389:1649–59.
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL. Bronchopulmonary dysplasia: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc. 2014;11:S146–53.
Wright CJ, Kirpalani H. Targeting inflammation to prevent bronchopulmonary dysplasia: can new insights be translated into therapies? Pediatrics. 2011;128:111–26.
Cummings JJ, Pramanik AK, FAAP; COMMITTEE ON FETUS AND NEWBORN. Postnatal Corticosteroids to Prevent or Treat Chronic Lung Disease Following Preterm Birth. Pediatrics; 2022;149:e2022057530.
Watterberg KL, Scott SM. Evidence of early adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics. 1995;95:120–5.
Bagnoli F, Mori A, Fommei C, Coriolani G, Badii S, Tomasini B. ACTH and cortisol cord plasma concentrations in preterm and term infants. J Perinatol. 2013;33:520–4.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. 2019;200:751–9.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004;114:1305–11.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics. 2004;114:1649–57.
Watterberg KL, Walsh MC, Li L, Chawla S, D’Angio CT, Goldberg RN, et al. Hydrocortisone to Improve Survival without Bronchopulmonary Dysplasia. N. Engl J Med. 2022;386:1121–31.
Onland W, Cools F, Kroon A, Rademaker K, Merkus MP, Dijk PH, et al. Effect of Hydrocortisone Therapy Initiated 7 to 14 Days After Birth on Mortality or Bronchopulmonary Dysplasia Among Very Preterm Infants Receiving Mechanical Ventilation: A Randomized Clinical Trial. JAMA. 2019;321:354–63.
Demauro SB, Dysart K, Kirpalani H. Stopping the swinging pendulum of postnatal corticosteroid use. J Pediatr. 2014;164:9–11.
Cuna A, Lagatta JM, Savani RC, Vyas-Read S, Engle WA, Rose RS, et al. Association of time of first corticosteroid treatment with bronchopulmonary dysplasia in preterm infants. Pediatr Pulmonol. 2021;56:3283–92.
Harmon HM, Jensen EA, Tan S, Chaudhary AS, Slaughter JL, Bell EF, et al. Timing of postnatal steroids for bronchopulmonary dysplasia: association with pulmonary and neurodevelopmental outcomes. J Perinatol. 2020;40:616–27.
Huysman MW, Hokken-Koelega AC, De Ridder MA, Sauer PJ. Adrenal function in sick very preterm infants. Pediatr Res. 2000;48:629–33.
Wu G, Jaeger LA, Bazer FW, Rhoads JM. Arginine deficiency in preterm infants: biochemical mechanisms and nutritional implications. J Nutr Biochem. 2004;15:442–51.
Watterberg KL, Scott SM, Backstrom C, Gifford KL, Cook KL. Links between early adrenal function and respiratory outcome in preterm infants: airway inflammation and patent ductus arteriosus. Pediatrics. 2000;105:320–24.
Clyman RI, Mauray F, Roman C, Rudolph AM, Heymann MA. Glucocorticoids alter the sensitivity of the lamb ductus arteriosus to prostaglandin E2. J Pediatr. 1981;98:126–28.
Greenberg RG, McDonald SA, Laughon MM, Tanaka D, Jensen E, Van Meurs K, et al. Online clinical tool to estimate risk of bronchopulmonary dysplasia in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2022:fetalneonatal-2021-323573. https://doi.org/10.1136/archdischild-2021-323573. Epub ahead of print.
Cuna A, Liu C, Govindarajan S, et al. Usefulness of an online risk estimator for bronchopulmonary dysplasia in predicting corticosteroid treatment in infants born preterm. J Pediatr. 2018;197:23–28.e2.
Baud O, Laughon M, Lehert P. Survival without bronchopulmonary dysplasia of extremely preterm infants: a predictive model at birth. Neonatology. 2021;118:385–93.
Author information
Authors and Affiliations
Contributions
SDS participated in methodology, collected data, analyzed data, drafted the initial manuscript, and critically reviewed and revised the manuscript. SS, PSN, SV participated in methodology, collected data, and critically reviewed the manuscript. ME collected and verified data, and critically reviewed the manuscript. SG analyzed data, critically reviewed and revised the manuscript. MLH reviewed and revised the manuscript critically. JC conceptualized and designed the study, coordinated and verified data collection, analyzed data, and critically reviewed and revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shah, S.D., Shukla, S., Nandula, P.S. et al. Prophylactic early low-dose hydrocortisone and survival without bronchopulmonary dysplasia among extremely preterm infants born at 22–27 weeks’ gestation. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01923-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01923-5