Abstract
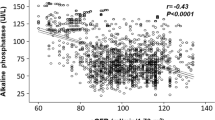
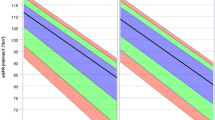
Data on the long term evolution of renal function in essential hypertensive patients are scarce, showing a low incidence of end stage renal diseases but without information on how the renal function evolves. Our aim is to describe the long term evolution of renal function and possible trajectories in hypertensive patients. We included patients from an ongoing cohort with essential hypertension, no proteinuria at baseline and no diabetes during follow-up and with at least two creatinine dosages 4 years apart. A long term (average 16 years) follow-up was available in 609 patients (baseline age 51.8 ± 11.1 years, 52 % male, mean office BP 156//95 mmHg). The trajectories of creatinine were modeled through a flexible latent class mixed model. The analysis identified three classes of significantly different trajectories. In the first (n = 560), there was no significant variation of creatinine over time. In the second (n = 40), there was a significant rise of creatinine (117 ± 20 vs 85 ± 17 µmol/l, p < 0.0001). The third class (n = 9) was very heterogeneous, mainly composed of outliers. Further analysis showed the nonlinearity of the evolution of creatinine in classes 2 and 3. So the model of progressive renal deterioration in essential hypertension does not fit with our results. A large majority (92%) of patients show no significant change in creatinine level with time. In the others 8%, the increase in creatinine is not progressive but conversely show one or more sudden bouts of elevation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
United States Renal Data System. 2018 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2018.
ERA-EDTA Registry: ERA-EDTA Registry Annual Report 2016. Amsterdam UMC, location AMC, Department of Medical Informatics, Amsterdam, the Netherlands, 2016.
Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D. Predictors of new-onset kidney disease in a community-based population. Jama 2004;291:844–50.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334:13–8.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165:923–8.
Siewert-Delle A. Long-term renal function in primary hypertension. An epidemiological and pathophysiological study. Scand J Urol Nephrol Suppl. 1999;199:1–36.
Eriksen BO, Stefansson VT, Jenssen TG, Mathisen UD, Schei J, Solbu MD, et al. Elevated blood pressure is not associated with accelerated glomerular filtration rate decline in the general non-diabetic middle-aged population. Kidney Int. 2016;90:404–10.
Gosse P, Promax H, Durandet P, Clementy J. ‘White coat’ hypertension. No harm for the heart. Hypertension. 1993;22:766–70.
Gosse P, Cremer A, Vircoulon M, Coulon P, Jan E, Papaioannou G, et al. Prognostic value of the extent of left ventricular hypertrophy and its evolution in the hypertensive patient. J Hypertens. 2012;30:2403–9.
Gosse P, Cremer A, Papaioannou G, Yeim S. Arterial stiffness from monitoring of timing of korotkoff sounds predicts the occurrence of cardiovascular events independently of left ventricular mass in hypertensive patients. Hypertension. 2013;62:161–7.
Gosse P, Cremer A, Boulestreau R, Gaillard P, Papaioannou G, Laine M. Long term variations of creatinine in essential hypertensives. J Hypertens. 2019. (In press) .
Proust C, Jacqmin-Gadda H. Estimation of linear mixed models with a mixture of distribution for the random effects. Comput Methods Prog Biomed. 2005;78:165–73.
Fitzmaurice G, Laird N, Ware J. Applied longitudinal analysis. John Wiley & Sons; 2004.
Proust-Lima C, Philipps V, Liquet B. Estimation of extendedmixed models using latent classes and latent processes: The R package lcmm. J Stat Sofw. 2017;48:1–56.
Siewert-Delle A, Ljungman S, Andersson OK, Wilhelmsen L. Does treated primary hypertension lead to end-stage renal disease? A 20-year follow-up of the Primary Prevention Study in Goteborg, Sweden. Nephrol Dial Transplant. 1998;13:3084–90.
Freedman BI, Iskandar SS, Appel RG. The link between hypertension and nephrosclerosis. Am J Kidney Dis. 1995;25:207–21.
Fahmy LM, Massie AB, Muzaale AD, Bagnasco SM, Orandi BJ, Alejo JL, et al. Long-term renal function in living kidney donors who had histological abnormalities at donation. Transplantation. 2016;100:1294–8.
Townsend RR, Reese PP, Lim MA. Should living kidney donors with hypertension be considered for organ donation? Curr Opin Nephrol Hypertens. 2015;24:594–601.
Kasiske BL. Relationship between vascular disease and age-associated changes in the human kidney. Kidney Int. 1987;31:1153–9.
Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152:561–7.
Meyrier A. Nephrosclerosis: a term in quest of a disease. Nephron. 2015;129:276–82.
Freedman BI, Cohen AH. Hypertension-attributed nephropathy: what’s in a name? Nat Rev Nephrol. 2016;12:27–36.
Li L, Astor BC, Lewis J, Hu B, Appel LJ, Lipkowitz MS, et al. Longitudinal progression trajectory of GFR among patients with CKD. Am J Kidney Dis. 2012;59:504–12.
Lamb EJ, Stevens PE. Estimating and measuring glomerular filtration rate: methods of measurement and markers for estimation. Curr Opin Nephrol Hypertens. 2014;23:258–66.
Shemesh O, Golbetz H, Kriss JP, Myers BD. Limitations of creatinine as a filtration marker in glomerulopathic patients. Kidney Int. 1985;28:830–8.
Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P. Predictive performance of the modification of diet in renal disease and Cockcroft–Gault equations for estimating renal function. J Am Soc Nephrol 2005;16:763–73.
Edmunds E, Beevers DG, Lip GY. What has happened to malignant hypertension? A disease no longer vanishing. J Hum Hypertens 2000;14:159–61.
Polgreen LA, Suneja M, Tang F, Carter BL, Polgreen PM. Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension 2015;65:1002–7.
Rubin S, Cremer A, Boulestreau R, Rigothier C, Kuntz S, Gosse P. Malignant hypertension:diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J Hypertens. 2019;37:316–24.
van den Born BJ, Koopmans RP, Groeneveld JO, van Montfrans GA. Ethnic disparities in the incidence, presentation and complications of malignant hypertension. J Hypertens 2006;24:2299–304.
Parati G, Liu X, Ochoa JE. Clinical relevance of visit-to-visit blood pressure variability: impact on renal outcomes. J Hum Hypertens 2014;28:403–9.
Kronish IM, Lynch AI, Oparil S, Whittle J, Davis BR, Simpson LM, et al. The association between antihypertensive medication nonadherence and visit-to-visit variability of blood pressure: findings from the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension 2016;68:39–45.
Hong K, Muntner P, Kronish I, Shilane D, Chang TI. Medication adherence and visit-to-visit variability of systolic blood pressure in African Americans with chronic kidney disease in the AASK trial. J Hum Hypertens 2016;30:73–8.
Acknowledgements
We thank Jeremy Reyburn for his rapid and efficient help in translating our paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gosse, P., Segalas, C., Rubin, S. et al. Long term evolution of renal function in essential hypertensive patients with no baseline proteinuria. J Hum Hypertens 34, 560–567 (2020). https://doi.org/10.1038/s41371-019-0245-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0245-4