Abstract
Preterm birth and low birth weight have been associated with an increased risk of hypertension; postnatal growth and dietary salt intake may contribute to these associations. In adults, the change of blood pressure (BP) in response to modifications in salt intake, i.e., salt sensitivity of BP, has been independently associated with cardiovascular disease. Little is known about salt sensitivity in children. We hypothesize that it may partly explain the association between preterm birth and higher BP in later life. We assessed salt sensitivity of BP at age 8 years in 63 preterm-born children, and explored its association with postnatal growth, sodium intake, and body composition from infancy onwards. BP was measured at baseline and after a 7-day high-salt diet. The difference in mean arterial pressure (MAP) was calculated; salt sensitivity was defined as an increase in MAP of ≥5%. Ten children (16%) showed salt sensitivity of BP, which was associated with neonatal growth restriction as well as with lower fat mass and BMI from infancy onwards. At age 8 years, children classified as salt sensitive had a lower weight-for-age SD-score (−1.5 ± 1.3 vs. −0.6 ± 1.1) and BMI (13.8 ± 1.7 vs. 15.5 ± 1.8 kg/m2) compared to their salt resistant counterparts. Sodium intake was not associated with (salt sensitivity of) BP. Salt sensitivity of BP was demonstrated in preterm-born children at age 8 years and may contribute to the development of cardiovascular disease at later age. Long-term follow-up studies are necessary to assess reproducibility of our findings and to explore clustering with other cardiovascular risk factors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kajantie E, Hovi P. Is very preterm birth a risk factor for adult cardiometabolic disease? Semin Fetal Neonatal Med. 2014;19:112–7.
de Jong F, Monuteaux MC, van Elburg RM, Gillman MW, Belfort MB. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59:226–34.
Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens. 2000;18:815–31.
Rotteveel J, van Weissenbruch MM, Twisk JW, Delemarre-Van de Waal HA. Infant and childhood growth patterns, insulin sensitivity, and blood pressure in prematurely born young adults. Pediatrics. 2008;122:313–21.
Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Sipola-Leppanen M, Vaarasmaki M, Tikanmaki M, Hovi P, Miettola S, Ruokonen A, et al. Cardiovascular risk factors in adolescents born preterm. Pediatrics. 2014;134:e1072–81.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27(3 Pt 2):481–90.
Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37(2 Pt 2):429–32.
Felder RA, White MJ, Williams SM, Jose PA. Diagnostic tools for hypertension and salt sensitivity testing. Curr Opin Nephrol Hypertens. 2013;22:65–76.
de Boer MP, Ijzerman RG, de Jongh RT, Eringa EC, Stehouwer CD, Smulders YM, et al. Birth weight relates to salt sensitivity of blood pressure in healthy adults. Hypertension. 2008;51:928–32.
Simonetti GD, Raio L, Surbek D, Nelle M, Frey FJ, Mohaupt MG. Salt sensitivity of children with low birth weight. Hypertension. 2008;52:625–30.
Brion MJ, Ness AR, Davey Smith G, Emmett P, Rogers I, Whincup P, et al. Sodium intake in infancy and blood pressure at 7 years: findings from the Avon Longitudinal Study of Parents and Children. Eur J Clin Nutr. 2008;62:1162–9.
Geleijnse JM, Hofman A, Witteman JC, Hazebroek AA, Valkenburg HA, Grobbee DE. Long-term effects of neonatal sodium restriction on blood pressure. Hypertension. 1997;29:913–7.
Keijzer-Veen MG, Devos AS, Meradji M, Dekker FW, Nauta J, van der Heijden BJ. Reduced renal length and volume 20 years after very preterm birth. Pediatr Nephrol. 2010;25:499–507.
Schreuder M, Delemarre-van de Waal H, van Wijk A. Consequences of intrauterine growth restriction for the kidney. Kidney Blood Press Res. 2006;29:108–25.
Abitbol CL, Rodriguez MM. The long-term renal and cardiovascular consequences of prematurity. Nat Rev Nephrol. 2012;8:265–74.
Black MJ, Sutherland MR, Gubhaju L, Kent AL, Dahlstrom JE, Moore L. When birth comes early: effects on nephrogenesis. Nephrol (Carlton). 2013;18:180–2.
Luyckx VA, Compston CA, Simmen T, Mueller TF. Accelerated senescence in kidneys of low-birth-weight rats after catch-up growth. Am J Physiol Ren Physiol. 2009;297:F1697–705.
Luyckx VA, Brenner BM. Low birth weight, nephron number, and kidney disease. Kidney Int Suppl. 2005;68:S68–77.
Amesz EM, Schaafsma A, Cranendonk A, Lafeber HN. Optimal growth and lower fat mass in preterm infants fed a protein-enriched postdischarge formula. J Pediatr Gastroenterol Nutr. 2010;50:200–7.
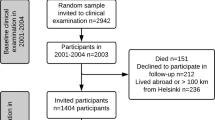
Ruys CA, van de Lagemaat M, Finken MJ, Lafeber HN. Follow-up of a randomized trial on postdischarge nutrition in preterm-born children at age 8 y. Am J Clin Nutr. 2017;106:549–58.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91.
Lafeber HN, van Zoeren-Grobben D, van Beek R, Gerards L. Enteral and parenteral nutrition in newborns (In Dutch: Werkboek enterale en parenterale voeding bij pasgeborenen), 2nd edn. Amsterdam: VU University; 2004.
The Netherlands Nutrition Centre. Website: https://mijn.voedingscentrum.nl/nl/eetmeter/ (in Dutch). Accessed 15 December 2016.
Hovi P, Vohr B, Ment LR, Doyle LW, McGarvey L, Morrison KM, et al. Blood pressure in young adults born at very low birth weight: adults born preterm international collaboration. Hypertension. 2016;68:880–7.
Hemachandra AH, Howards PP, Furth SL, Klebanoff MA. Birth weight, postnatal growth, and risk for high blood pressure at 7 years of age: results from the Collaborative Perinatal Project. Pediatrics. 2007;119:e1264–70.
Lurbe E, Garcia-Vicent C, Torro MI, Aguilar F, Redon J. Associations of birth weight and postnatal weight gain with cardiometabolic risk parameters at 5 years of age. Hypertension. 2014;63:1326–32.
Lurbe E, Ingelfinger JR. Blood pressure in children and adolescents: current insights. J Hypertens. 2016;34:176–83.
Lava SA, Bianchetti MG, Simonetti GD. Salt intake in children and its consequences on blood pressure. Pediatr Nephrol. 2015;30:1389–96.
Yang Q, Zhang Z, Kuklina EV, Fang J, Ayala C, Hong Y, et al. Sodium intake and blood pressure among US children and adolescents. Pediatrics. 2012;130:611–9.
Elijovich F, Weinberger MH, Anderson CA, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–46.
Overlack A, Ruppert M, Kolloch R, Kraft K, Stumpe KO. Age is a major determinant of the divergent blood pressure responses to varying salt intake in essential hypertension. Am J Hypertens. 1995;8:829–36.
Kurtz TW, DiCarlo SE, Pravenec M, Morris RC Jr. An appraisal of methods recently recommended for testing salt sensitivity of blood pressure. J Am Heart Assoc. 2017;6:e005653.
Richardson SI, Freedman BI, Ellison DH, Rodriguez CJ. Salt sensitivity: a review with a focus on non-Hispanic blacks and Hispanics. J Am Soc Hypertens. 2013;7:170–9.
Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, et al. Individual blood pressure responses to changes in salt intake: results from the DASH-Sodium trial. Hypertension. 2003;42:459–67.
Wesseling S, Koeners MP, Joles JA. Salt sensitivity of blood pressure: developmental and sex-related effects. Am J Clin Nutr. 2011;94(6 Suppl):1928S–1932S.
Duncombe SL, Voss C, Harris KC. Oscillometric and auscultatory blood pressure measurement methods in children: a systematic review and meta-analysis. J Hypertens. 2017;35:213–24.
Chen J, Gu D, Huang J, Rao DC, Jaquish CE, Hixson JE, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009;373:829–35.
Yatabe MS, Yatabe J, Yoneda M, Watanabe T, Otsuki M, Felder RA, et al. Salt sensitivity is associated with insulin resistance, sympathetic overactivity, and decreased suppression of circulating renin activity in lean patients with essential hypertension. Am J Clin Nutr. 2010;92:77–82.
Kurtz TW, DiCarlo SE, Pravenec M, Morris RC Jr. The American Heart Association Scientific Statement on salt sensitivity of blood pressure: Prompting consideration of alternative conceptual frameworks for the pathogenesis of salt sensitivity? J Hypertens. 2017;35:2214–25.
Kurtz TW, DiCarlo SE, Pravenec M, Morris RC Jr. The pivotal role of renal vasodysfunction in salt sensitivity and the initiation of salt-induced hypertension. Curr Opin Nephrol Hypertens. 2017;27:83–92.
Boegehold MA. The effect of high salt intake on endothelial function: reduced vascular nitric oxide in the absence of hypertension. J Vasc Res. 2013;50:458–67.
Titze J, Machnik A. Sodium sensing in the interstitium and relationship to hypertension. Curr Opin Nephrol Hypertens. 2010;19:385–92.
Funding
The original randomized controlled trial was supported by an unrestricted research grant from Friesland Campina, Amersfoort, The Netherlands. Friesland Campina also provided the formulas. CR was supported by an unrestricted research grant, provided by Hero Benelux, Breda, The Netherlands. Neither Friesland Campina nor Hero Benelux had a role in the design and execution of the studies, or in the analysis and interpretation of the results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ruys, C.A., Rotteveel, J., van de Lagemaat, M. et al. Salt sensitivity of blood pressure at age 8 years in children born preterm. J Hum Hypertens 32, 367–376 (2018). https://doi.org/10.1038/s41371-018-0045-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0045-2
This article is cited by
-
Salt sensitivity of blood pressure in childhood and adolescence
Pediatric Nephrology (2022)
-
Birth weight modifies the association between a healthy Nordic diet and office blood pressure in old age
Journal of Human Hypertension (2021)
-
Association of circulating uric acid and angiotensin-(1–7) in relation to higher blood pressure in adolescents and the influence of preterm birth
Journal of Human Hypertension (2020)
-
Is too much salt harmful? Yes
Pediatric Nephrology (2020)