Abstract
Background
Noninvasive neurally adjusted ventilator assist (NIV-NAVA) was introduced to our clinical practice via a pilot and a randomized observational study to assess its safety, feasibility, and short-term physiological effects.
Methods
The pilot protocol applied NIV-NAVA to 11 infants on nasal CPAP, high-flow nasal cannula, or nasal intermittent mandatory ventilation (NIMV), in multiple 2- to 4-h periods of NIV-NAVA for comparison. This provided the necessary data to design a randomized, controlled observational crossover study in eight additional infants to compare the physiological effects of NIV-NAVA with NIMV during 2-h steady-state conditions. We recorded the peak inspiratory pressure (PIP), FiO2, Edi, oxygen saturations (histogram analysis), transcutaneous PCO2, and movement with an Acoustic Respiratory Movement Sensor.
Results
The NAVA catheter was used for 81 patient days without complications. NIV-NAVA produced significant reductions (as a percentage of measurements on NIMV) in the following: PIP, 13%; FiO2, 13%; frequency of desaturations, 42%; length of desaturations, 32%; and phasic Edi, 19%. Infant movement and caretaker movement were reduced by 42% and 27%, respectively. Neural inspiratory time was increased by 39 ms on NIV-NAVA, possibly due to Head’s paradoxical reflex.
Conclusion
NIV-NAVA was a safe, alternative mode of noninvasive support that produced beneficial short-term physiological effects, especially compared with NIMV.
Similar content being viewed by others
Main
Neurally adjusted ventilatory assist (NAVA) is a relatively new mode of mechanical ventilation. NAVA assists the patient in proportion to the respiratory effort based on the detection of the electrical activity of the diaphragm (Edi) by an array of electrodes built into a modified feeding tube. The Edi is translated into proportional increases in airway pressure in synchrony with, and in proportion to, the patient’s respiratory effort. Thus, patients initiate their own breaths and regulate their own peak inspiratory pressures (PIPs) and inspiratory times (Ti). NAVA, therefore, represents a paradigm shift in ventilatory management, as the standard ventilator settings used in common practice are not used during NAVA.
The literature has recently been reviewed for older infants (1) and newborns (2), and practical application has been described by a group with the largest neonatal experience to date (3). The physiological effects of NAVA have been mainly described in intubated patients. In a retrospective study in intubated preterm infants, there was a reduction in PIP, FiO2, and arterial PCO2 (in infants with baseline PCO2>45) on NAVA compared with those on synchronized intermittent mandatory ventilation (SIMV) (4). These authors also performed a prospective, randomized crossover trial (5) that showed a reduction in PIP, FiO2, transcutaneous PCO2 (PtcCO2), peak Edi, and respiratory rate on NAVA compared with those on pressure support ventilation (PS). The reduction in the PIP but not in the FiO2 was confirmed in two randomized crossover studies of intubated preterm infants comparing NAVA with SIMV with PS (6), and NAVA with IMV or high-frequency oscillatory ventilation (7).
The effectiveness of NIV-NAVA was first demonstrated in rabbits (8). The first report of NIV-NAVA in preterm infants was a study performed immediately after extubation (9) that demonstrated an excellent correlation between the PIP and peak Edi in infants both when intubated and after they were extubated, with no correlation between the PIP and Edi on PS. A large clinical experience suggests that NIV-NAVA reduces the need for invasive ventilation (2). The first systematic study of NIV-NAVA was a randomized crossover study in infants immediately after extubation that demonstrated a reduction in PIP but not in FiO2 on NIV-NAVA vs. NIV-PS, significantly reduced trigger delay, and asynchrony events, even in the presence of large air leaks. (10)
We performed a pilot feasibility study in infants on various modes of noninvasive support to introduce NIV-NAVA to our practice. We were able to lower the PIP and FiO2 in a subset of these infants during NIV-NAVA compared with nasal intermittent mandatory ventilation (NIMV). The resulting data were used to design a randomized, crossover observational study to test the hypothesis that NIV-NAVA could reduce the PIP needed on NIMV while supporting the infant on the same mean airway pressure and overall gas exchange, as determined by pulse oximetry and PtcCO2. During both studies, we analyzed detailed recordings of electrocardiogram, oxygen saturation, PtcCO2, and infant and caretaker movement using an Acoustic Respiratory Movement Sensor (ARMS). Our secondary outcomes were a comparison of the FiO2 required to maintain the oxygen saturation in a target range, the character of episodes of desaturation, and infant comfort as reflected in the phasic Edi and the measurements of infant and caretaker movement, as these data have not been described. We chose to study noninvasive support, as it represented the majority of ventilatory assistance in our Neonatal Intensive Care Unit and it had the greatest potential to help neonates recover from respiratory distress syndrome without the need for intubation.
Methods
Our pilot study was performed between October 2012 and November 2014. Our subsequent randomized observational study was performed between August 2014 and March 2016. Both studies were approved by the Institutional Review Board of the University of California, San Diego under separate protocols. Informed, written parental consent was obtained prior to enrollment.
Study Design
Our pilot study was performed in 11 preterm infants, ranging in study weights of 840–2,200 g, who were on NCPAP, NIMV, or high-flow nasal cannula. We applied NIV-NAVA for 2–4 h on each of 1–5 days during which time the NAVA catheters were in place, and compared the infants’ physiological response to NIV-NAVA with that of the other methods. We found that we were able to reduce the PIP of 33 ±12%, (P<0.01, N=10 recordings) in six infants on NIMV. From this limited data set, a power analysis indicated that this reduction could be verified with 14 crossovers in seven infants (α=0.05, β=0.8). We chose to study each infant on 2 days to produce data with more generalizability. We also observed that episodes of desaturation were frequently caused by handling of the infant; so this study was coordinated with the routine nursing care to eliminate handling the infants unless necessary during the NIV-NAVA or NIMV recording periods.
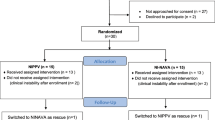
Premature infants were eligible for enrollment in the randomized observational study if they were on NIMV and considered clinically stable by the medical team. Infants were excluded if they had congenital airway anomalies, congenital heart disease, neuromuscular disease, feeding intolerance, or gastric or esophageal pathology. The protocol is shown in Figure 1, which was performed on 2 consecutive days. On study day 1, the feeding tube was replaced with a NAVA feeding catheter (49 or 50 cm, as directed by the manufacturer) using the positioning window on the Servo-i ventilator. After the initial set-up, we switched to NIV-NAVA for a period of up to 30 min to optimize the NIV-NAVA level for PtcCO2 and the FiO2 for the target saturation range of 88–94% as was our clinical policy. We then switched back to NIMV for 30 min and for the nursing care. Infants were randomized to begin the study with either NIMV with a crossover to NIV-NAVA or NIV-NAVA with a crossover to NIMV, which was started after the first nursing care. This randomized mode of ventilation was continued through the second nursing care, and then the mode was switched. There was a 1-h washout period after nursing care, followed by a 2-h recording period. The infants were then placed back on NIMV at the pre-study ventilator settings. The protocol was repeated on study day 2, starting with the opposite mode from study day 1. After the studies on study day 2, the Edi catheter was replaced with the usual feeding tube.
The randomized crossover design of the observational study. All infants were on NIMV at the start and finish of the protocol. After set up, NIV-NAVA was applied for up to 30 min to determine optimum parameters, followed by at least 30 min of NIMV. Infants were then randomized to either continue NIMV or NIV-NAVA for 3 h after nursing care and then crossed over to the alternate mode until after the next nursing care. A 2-h recording period was performed after a 1-h washout period following the nursing care. Infants were not handled during the recording unless care was necessary.
NIMV was produced with a Servo-i ventilator (Maquet Critical Care AB, Solna, Sweden) via nasal prongs appropriate for weight (Fisher & Paykel Healthcare, Berkshire, UK). During NIMV, the Servo-i was set in the invasive SIMV mode with an inspiratory time of 0.35–0.45 s, with an NIMV rate of 10–30 (as set by the clinical team), and a backup rate of 30 breaths per minute after an apnea time of 10 s, which were the usual settings for clinical care. The research team made all ventilator adjustments during NIV-NAVA, and only adjusted the FiO2 during NIMV to keep the saturations in the target range of 88–94%. The NAVA trigger level was set to the default value of 0.5 μV to capture small breaths. The initial NAVA level was set at 1 cm H2O/μV, but usually needed to be increased to reduce the peak Edi to <12–15 μV. Apnea settings were set to 2–5 s, depending on the NIMV rate such that backup breaths during NAVA would be the same as the NIMV rate during NIMV. The NAVA level and/or the positive end-expiratory pressure (PEEP) was lowered as tolerated in infants whose FiO2 was reduced to 0.21 and whose oxygen saturations exceeded the target range. The ventilator settings were not adjusted during the study periods.
The frequency and depth of episodes of desaturation were determined from the bedside monitor during 12 h prior to the daily study. If the frequency of desaturations was greater than that in the 12-h pre-study period, or if the depth of any desaturation occurring during NIV-NAVA was lower than the lowest saturation in the 12-h pre-study period, the NIV-NAVA observation period was terminated and the infant was placed back on NIMV.
Measurements
We obtained the signals for the Edi, flow, and airway pressure from the Servo-i ventilator via an RS-232 interface by software (Servo-Tracker, Maquet Critical Care AB) whose output to a digital-to-analog converter (Analog Interface, Model USB 6212 BNC, National Instruments, Dallas, TX, USA) produced analog signals at 100 samples per second for recording. Preliminary tests demonstrated a lag of no >10 ms between the output of an independent airway pressure measurement system and the pressure derived from the Servo-i output for a step change in applied airway pressure.
Oxygen saturation and heart rate were measured with a standard pulse oximeter (Model Radical 7, Masimo, Irvine, CA). We recorded the ECG from the standard clinical monitor (IntelliVue MP70, Phillips, Carlsbad, CA). The PtcCO2 was measured with a standard probe (Model TINA, TCM4, Radiometer, Copenhagen, Denmark), with the temperature set to 41.5 °C, so that a single probe placement could be used for the entire protocol on each day. We measured the amount of infant and caretaker movement with an Acoustic Respiratory Movement Sensor (ARMS), a noninvasive device that was attached to the upper wall of the isolette or on a bracket on the open crib and transmitted and received a 40-kHz ultrasound signal to detect all movement in the area of insonation. The ARMS produced a continuous record of infant movement and caretaker movement with 90% and 98% accuracy, respectively (11).
All signals from the Servo-i ventilator, the physiological monitors, and the ARMS were simultaneously recorded with a laptop computer with a commercially available system (MP150 hardware with HL100 isolated connector system and AcqKnowledge system software, Version 4.2, BioPac, Goleta, CA). Data from all signals were collected at 1,000 points per second per channel and graphically displayed in real-time. Annotations to the physiological data file were added for clinical events that could affect the status of infants.
Data Processing
The physiological data were processed within the AcqKnowledge software system from the stored data files. Data were displayed graphically, and computations were made with standard software routines for thresholding, maxima and minima measurements, histogram generation, and respiratory cycle identification.
PIPs were computed on a breath-by-breath basis from the airway pressure signal. The peak airway pressure values for each breath were averaged for each mode of ventilation in each recording period. The mean airway pressure was calculated as the average value of the airway pressure in each recording period.
The proportion of oxygen saturation values in the range of >94, 88–94, and <85% was calculated in each recording period. Episodes of desaturation <85% were identified, and their length and minimum saturation were measured. Episodes that were multiple decreases below 85% saturation lasting <3 s were counted as single episodes. The frequency of episodes of desaturation was expressed as episodes per hour.
The peak, tonic, and phasic Edi were calculated on a breath-by-breath basis. The phasic Edi was calculated as the difference between the peak and tonic Edi for each breath. The mean values were calculated for each recording period.
The PtcCO2 was corrected for drift (12) over the entire daily study. The drift correction was <5% in all but one recording in which it was 14% over a 7-h period. The corrected PtcCO2 was averaged for each of the recording periods.
Infant and caretaker movement was calculated from the ARMS movement signal, and the proportions of both types of movement were calculated in each of the recording periods.
Timing intervals of the Edi, flow, and airway pressure were characterized by measurements of the time intervals shown in Figure 2. Figure 2a shows data of an infant on NIV-NAVA, and Figure 2b shows how we selected unassisted breaths that were not distorted by the airway pressure at the midpoints between the NIMV breaths. Point A was the inspiratory inflection in the Edi, and point B was the onset of inspiratory pressure. Point C was the end of neural inspiration, and point D was the start of pneumatic expiration that was abrupt and easily identified, despite the large and variable background flow from the leak in the airway. Point E was the end of neural expiration. The corresponding points A, C, and E were similarly identified for the unassisted breaths. Unassisted breaths eligible for analysis are marked with stars in the figure.
Timing relationships between the Edi, airway flow, and airway pressure (Paw) are shown during NIV-NAVA (a) and the Edi and Paw during NIMV (b). Shown are time points at the start of neural inspiration (A), the start of the ventilator breath (B), the end of neural inspiration (C), the start of pneumatic expiration (D), and the end of neural expiration (E). An unassisted breath is indicated by a star that was chosen for possible comparison, which was not affected by the random NIMV breaths. Time points A, C, and E were defined similarly for the unassisted breaths in b.
Intervals for timing were measured from point A. Interval A–B was the pneumatic delay in the NAVA system until the onset of inspiratory pressure (T delay). Interval A–C was the neural inspiratory time (Ti neural), measured to the peak Edi, and interval C–E was the neural expiratory time (Te neural). Interval A–D was the neuro-pneumatic inspiratory time (Ti neuro-pneumatic). Interval C–D was the cycling-off delay time (T cycling-off delay) due to the NAVA algorithm, which released the airway pressure at 70% of the phasic Edi. Interval B–D was the inspiratory pneumatic time (Ti pneumatic), and interval D–B of the subsequent breath was the expiratory pneumatic time (Te pneumatic). These time points were identified using a manual cursor moved in the graphical display. Values for these intervals were measured for 25 breaths that were selected randomly throughout the entire 2-h recording period in each mode of ventilation on each day of the study. This resulted in a total of 350 breaths in each mode for comparison across the 14 days of studies in the seven infants.
Statistical Analysis
We compared the mean value of the PIP, saturation histogram data, frequency, depth, and length of episodes of desaturations, peak, tonic and phasic Edi, PtcCO2, and infant and caretaker movement from the recording periods in each crossover by the paired t-test or rank-sum test in the case of data that were not normally distributed. The timing intervals were averaged for breaths in each mode in each recording period and compared with their corresponding average within each study day between NIV-NAVA and unassisted breaths by the paired t-test or rank-sum test if the data were not normally distributed.
Results
Table 1 summarizes the demographics of the eight infants at the start of the randomized study. Their study weights ranged from 980 to 1,280 g. Table 2 shows the ventilatory parameters on study day 1. Seven of the eight infants required supplemental oxygen, and all required significant amounts of noninvasive support.
We compared the data during the 2-h recording period between the two modes of ventilation each study day. We did not include data from infant #8, as there was a period of ~20 min on the second day where nasal CPAP was inadvertently applied instead of NIMV. Thus, we analyzed a total of 28 h of data in each mode, with 14 crossovers in infants #1–7.
Feasibility
We found that nurses, respiratory therapists, and physicians could easily place the Edi catheter in the appropriate position using the positioning window on the Servo-i ventilator. The total time that the Edi catheter was in place for the pilot and randomized studies was 81 patient days There were no episodes of gastric distention or suctioning malfunction, and Edi catheter did not require repositioning during the time it was in place in both studies.
Physiological Effects of NIV-NAVA
We started with a NAVA level of 1, but needed to raise it to 1.5–2.5 cm H2O/μV, as the peak Edi was consistently >12–15 μV. At that NAVA level, limiting pressure was reached in 1.3±1% of the recording time; the remaining breaths were below the PIP used for NIMV management.
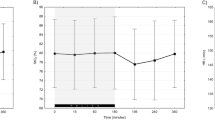
Figure 3 shows the differences of each parameter on NIV-NAVA expressed as a percentage of the value for each parameter while on NIMV. There were significant reductions in the PIP (13±1.8% (P<0.01) and FiO2 (−13±2.4%, P<0.01). There were no differences in the mean airway pressures between NIV-NAVA and NIMV.
Differences for each measurement while on NIV-NAVA expressed as a percentage of those while on NIMV. There were significant reductions in the peak inspiratory pressure and FiO2 with no difference in the distribution of saturations or the PtcCO2. There were significant reductions in the frequency and depth of desaturations, the phasic Edi, and in the amount of infant and caretaker movement. There were no differences in the mean airway pressures between modes of support. Significance, starred bars = P<0.01.
Overall gas exchange was the same in both modes, as there were no significant differences in the proportion of time in the three saturation ranges. The steady-state FiO2 was usually attained in the first 30 min of the washout periods and was stable during the recording periods. There was no difference in the average PtcCO2 between NIV-NAVA and NIMV. The infants controlled their overall ventilation similarly on NIV-NAVA to that provided by NIMV with the ventilator settings chosen for clinical care.
There was also a significant reduction in the FiO2 during the NIMV study periods than during clinical management (−8.4±2.2%, P<0.02), indicating that the FiO2 was managed similarly during NIV-NAVA and NIMV.
Backup ventilation during short periods of apnea had a positive impact on episodes of desaturation. There were significant reductions in the frequency of desaturations (−42±12%, P<0.006) and the length of desaturations (−33±10%, P<0.01). The average depth of desaturations was not reduced. Backup ventilation occurred during NIV-NAVA in 2.2±3.4% of the recording periods, and NIV-NAVA smoothly resumed when spontaneous effort was detected. There was significant unloading of the respiratory effort, even in the presence of a large airleak, as the phasic Edi was significantly reduced (−19±3.5%, P<0.01).
Although this was a limited data set, we did not detect any sequence or carry-over effects of the changes in the modes of ventilation in randomized study.
Both nurses and parents of infants subjectively felt that the infants were more comfortable on NIV-NAVA than on NIMV, and fought the ventilator less. This was corroborated by significant reductions in infant movement (−42±9%, P<0.01) and caretaker movement (−29±8% P<0.01) on NIV-NAVA. Caretaker movement was detected in <1.2% of the recording times, indicating that there was little handling of the infants during the recordings. There were no differences in the mean heart rates between NIMV and NIV-NAVA.
The profile of the Edi of the infants while on NIV-NAVA was different from that of their unassisted breaths, indicating a difference in the neural control of breathing. The timing intervals of the respiratory cycle are shown in Table 3. The Ti neural was significantly longer (39 ms) and less variable on NIV-NAVA than during unassisted breaths (NIV-NAVA, 329±52 vs. 290±82 ms, P=0.014). This absolute difference was corroborated by normalization of the Ti neural to the period of respiration (Ti/Ttot), wherein there was a significant increase in this ratio (NIV-NAVA 0.370±0.033 vs. 0.325±0.32, P=0.004). Both the absolute and relative increases were ~13% of the Ti neural of unassisted breaths.
The Te neural was more variable, both on NIV-NAVA and during unassisted breaths, and there was no significant difference in this interval. Because of this variability, there was no significant difference in the respiratory rate derived from the Edi between NIV-NAVA and unassisted breaths.
The NIV-NAVA system produced a pneumatic pressure profile that was different from the neural profile of unassisted breaths. The Ti neuro-pneumatic profile included the T cycling-off delay time, during which the NIV-NAVA algorithm maintained the airway pressure until the Edi fell below 70% of the maximum Edi. The T cycling-off delay averaged 113±24 ms, which when added to the Ti neural, averaged 442±71 ms. This was significantly greater than the Ti neural (P=0.001), and averaged 152 ms longer than the Ti neural of unassisted breaths as expected. The Ti pneumatic on NIV-NAVA averaged 318±71 ms, was highly variable, and was not significantly different from the Ti pneumatic of the ventilator on NIMV, as chosen by the clinical team.
The pneumatic response time on NIV-NAVA, or T delay pneumatic, averaged 124± 21 ms. The inspiratory pressure by NIV-NAVA was extended into neural expiration, such that the Ti pneumatic on NIV-NAVA was ~110% of the Ti neural of the unassisted breaths. Despite the differences in the pneumatic profile and the neural profile of the unassisted breaths, synchrony with the spontaneous respiratory rhythm was well maintained. During the transition from NIMV to NIV-NAVA, we noted that infants took large recruitment breaths, and frequently developed periodic breathing and longer expiratory pauses. This usually resolved within the first 15 min of the washout periods, was not seen in the recording periods, and did not contribute to the character of the episodes of desaturations.
Discussion
We have demonstrated the feasibility of NIV-NAVA with a substantial experience of 81 patient days. The Edi catheter could be placed by the nursing, respiratory therapy, and physician staff with limited experience. With the change to NIV-NAVA, we were able to significantly reduce the PIP and FIO2 at the same level of gas exchange and mean airway pressure. Short respiratory pauses were reliably detected, and backup breaths were delivered that resulted in a reduction in the frequency and duration of episodes of desaturation. The ventilator returned immediately back to the NAVA mode after providing backup breaths. Infants on NIV-NAVA appeared more comfortable, as previously reported (13), and had less movement and caretaker intervention, as quantified by the ARMS.
Our studies extend the observations of previous studies of NIV-NAVA. We made recordings over a longer duration than those reported previously (9, 10) with the infants in a relatively steady state during the 2-h recording periods following the 1-h washout periods. We needed to make minimal adjustments in the NAVA level to match the PtcCO2 during NIMV, as the infants controlled their own ventilation. The NAVA levels we used were generally lower than those reported for intubated infants, and were in the range below the “break-point” above which higher NAVA levels do not produce an increase in the PIP (14). Thus, our infants were treated with a range of NAVA levels that allowed them to maintain their desired ventilation and also to be assisted during larger recruitment breaths. There were no instances of over-pressure with large respiratory efforts. This may not be the case during invasive ventilation, wherein there is a much smaller airway leak, or if the limit pressure is set higher to allow sicker infants to have larger recruitment breaths. Our observations on NIV-NAVA should not be extrapolated to NAVA in intubated infants. The reductions in the PIP and phasic Edi were similar to those reported both during invasive and NIV-NAVA (5, 6, 10).
We did not design our studies to compare asynchronies between spontaneous breathing and the ventilator on NIV-NAVA vs. NIMV. The differences in the timing of the respiratory rhythm on NIV-NAVA vs. unassisted breaths on NIMV suggest an interaction of NAVA with the control of breathing. We did not see a shortening of inspiration and prolongation of expiration due to the Hering–Breuer reflex, but rather saw a prolongation of Ti neural and Ti/Ttot and no difference in the respiratory rate that was consistent with Head’s Paradoxical Reflex (15, 16). Our observed values for Ti/Ttot were similar to those reported in infants immediately after extubation on NIV-NAVA (9) and were similar for the unassisted breaths as reported for infants who were not on assistance (17). Elicitation of the HPR could explain the stimulation of earlier inspiratory efforts upon the release of inflation pressure late in expiration during steady-state NIV-NAVA, as well as the occasional large breaths followed by periodic breathing and apnea that we observed during the transition to NIV-NAVA (18).
The Hering–Breuer reflex has been suggested as a limiting factor in creating synchrony. This has important implications when comparing NIV-NAVA with SIMV. NAVA is the only technology at present to produce synchrony for noninvasive ventilation in both older (19) and preterm (5, 10) infants. The former SIMV system based on the Graseby capsule (StarSynch) had clinical success during noninvasive ventilation even though it used an abrupt inspiratory pressure profile that should have induced the Hering–Breuer reflex. The synchrony it obtained was probably due to its short (60 ms) and reliable response time (20). In addition, it was seldom used at rates above 20 breaths per minute, which allowed an adequate time for passive expiration to avoid active expiration and “fighting the ventilator”. The randomly applied breaths during NIMV and PS cause a variety of asynchronies and poorer gas exchange compared with NIV-NAVA (10). The reduced movement of the infants we observed on NIV-NAVA was consistent with a reduction in active expiration. However, we cannot separate the effects of synchrony alone from its effect in conjunction with the proportional assistance provided by NAVA. The proportional assistance provided by NAVA is more like natural breathing and may in itself prevent disruption of the infant’s respiratory rhythm that leads to active expiration.
The increase in the Ti neural in conjunction with the delay of pneumatic inspiration and the off-cycle time after the peak Edi may have recruited lung volume, which may partly explain the improvement in oxygenation. Synchrony may also promote lung recruitment that is not reflected in the airway pressure, as the infant’s spontaneous breathing increases the transpulmonary pressure that is added to the airway pressure, which improves inspiration rather than opposing inflation with the recoil pressure of the respiratory system during nonsynchronized breaths.
The limitations of our study include the selection of unassisted breaths between the NIMV breaths for the timing comparisons. We feel that the random selection of breaths throughout the recording period was representative, and the number of breaths selected for comparison (350 total for NIV-NAVA and 350 for unassisted breaths) were sufficient for this purpose. The infants had the same overall gas exchange and mean airway pressure during NIV-NAVA and NIMV during the study periods. Our washout period of 1 h should have been sufficient to attain a steady state, as in a previous report (6). Our studies were also limited to the short-term effects of changing between NIMV and NIV-NAVA, and they did not address clinical outcomes.
The improvements in oxygenation at lower levels of support and the reduction in the frequency and severity of episodes of desaturation, if sustained on NIV-NAVA, could make a difference in the long-term outcomes of BPD or retinopathy of prematurity. The safety of NIV-NAVA and its possible longer-term physiological benefits make it a feasible alternate therapy to all current modalities of noninvasive support. A large, randomized clinical trial is needed to determine the effect of NIV-NAVA on important long-term outcomes.
References
Beck J, Emeriaud G, Liu Y, Sinderby C . Neurally adjusted ventilatory assist (NAVA) in children: a systematic review. Minerva Anestesiol 2016;82:874–83.
Stein H, Beck J, Dunn M . Non-invasive ventilation with neurally adjusted ventilatory assist in newborns. Semin Fetal Neonatal Med 2016;21:154–61.
Stein H, Firestone K . NAVA ventilation in neonates: clinical guidelines and management strategies. Neonatol Today 2012;7:1–8.
Stein H, Howard D . Neurally adjusted ventilatory assist in neonates weighting <1500 grams: a retrospective analysis. J Pediatr 2012;160:786–789.
Stein H, Alosh H, Ethington P, White DB . Prospective crossover comparison between NAVA and pressure control ventilation in premature neonates less than 1500 grams. J Perinatol 2013;33:452–6.
Lee J, Kim HS, Sohn JA et al, Randomized crossover study of neurally adjusted ventilatory assist in preterm infants. J Pediatr 2012;161:808–13.
Kallio M, Koskela U, Peltoniemi O et al, Neurally adjusted ventilatory assist (NAVA) in preterm newborn infants with respiratory distress syndrome-a randomized controlled trial. Eur J Pediatr 2016;175:1175–83.
Beck J, Brander L, Slutsky AS, Reilly MC, Dunn MS, Sinderby C . Non-invasive neurally adjusted ventilatory assist in rabbits with acute lung injury. Intensive Care Med 2008;34:316–23.
Beck J, Reilly M, Grasselli G et al, Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res 2009;65:663–8.
Lee J, Kim HS, Jung YH et al, Non-invasive neurally adjusted ventilatory assist in preterm infants: a randomised phase II crossover trial. Arch Dis Child Fetal Neonatal 2015;100:F507–13.
Heldt GP, Ward RJ 3rd . Evaluation of ultrasound-based sensor to monitor respiratory and nonrespiratory movement and timing in infants. IEEE Trans Biomed Eng 2016;63:619–29.
Berlowitz DJ, Spong J, O'Donoghue FJ et al, Transcutaneous measurement of carbon dioxide tension during extended monitoring: evaluation of accuracy and stability, and an algorithm for correcting calibration drift. Respir Care 2011;56:442–8.
Soukka H, Grönroos L, Leppäsalo J, Lehtonen L . The effects of skin-to-skin care on the diaphragmatic electrical activity in preterm infants. Early Hum Dev 2014;90:531–4.
Firestone KS, Fisher S, Reddy S, White DB, Stein HM . Effect of changing NAVA levels on peak inspiratory pressures and electrical activity of the diaphragm in premature neonates. J Perinatol 2015;35:612–6.
Head H . On the regulation of respiration. J Physiol 1889;10:1–70.
Baumann C . Henry Head in Ewald Hering’s laboratory in Prague 1884-1886: an early study on the nervous control of breathing. J Hist Neurosci 2005;14:322–33.
Beck J, Reilly M, Grasselli G et al, Characterization of neural breathing pattern in spontaneously breathing preterm infants. Pediatr Res 2011;70:607–13.
Cross KW, Klaus M, Tooley WH, Weisser K . The response of the new-born baby to inflation of the lungs. J Physiol 1960;161:551–65.
Bordessoule A, Emeriaud G, Morneau S, Jouvet P, Beck J . Neurally adjusted ventilatory assist improves patient–ventilator interaction in infants as compared with conventional ventilation. Pediatr Res 2012;72:194–202.
Bernstein G, Cleary JP, Heldt GP, Rosas JF, Schellenberg LD, Mannino FL . Response time and reliability of three neonatal patient-triggered ventilators. Am Rev Respir Dis 1993;148:358–64.
Acknowledgements
Maquet provided the Servo-Tracker software on loan, and provided no financial support for this effort. The ARMS was provided by BioData Innovation Systems.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
RW is the CEO of BioData Innovation Systems that has a patent pending for the ARMS technology. Future commercial uses of the ARMS technology may provide financial benefit to RW. The remaining authors declare no conflict of interest.
Additional information
STATEMENT OF FINANCIAL SUPPORT
This work was supported in part by 1 R41 HL 102940 from National Heart, Lung, and Blood Institute, Bethesda, MD, USA. The results from the pilot study were presented in part at the Pediatric Academic Society meeting in Vancouver BC in May 2014.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Gibu, C., Cheng, P., Ward, R. et al. Feasibility and physiological effects of noninvasive neurally adjusted ventilatory assist in preterm infants. Pediatr Res 82, 650–657 (2017). https://doi.org/10.1038/pr.2017.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.100
This article is cited by
-
NIV-NAVA versus non-invasive respiratory support in preterm neonates: a meta-analysis of randomized controlled trials
Journal of Perinatology (2024)
-
Improved nutritional outcomes with neurally adjusted ventilatory assist (NAVA) in premature infants: a single tertiary neonatal unit’s experience
European Journal of Pediatrics (2022)
-
Effects of heliox and non-invasive neurally adjusted ventilatory assist (NIV-NAVA) in preterm infants
Scientific Reports (2021)
-
Evaluating peak inspiratory pressures and tidal volume in premature neonates on NAVA ventilation
European Journal of Pediatrics (2021)
-
Comparison of NIV-NAVA and NCPAP in facilitating extubation for very preterm infants
BMC Pediatrics (2019)