Abstract
Background:
The preterm newborn is at high risk of developing cardiovascular compromise during the first day of life and this is associated with increased risk of brain injury. Standard treatments are volume expansion and administration of inotropes, typically dopamine and/or dobutamine, but there is limited evidence that inotropes improve clinical outcomes. This study investigated the efficacy of dopamine and dobutamine for the treatment of cardiovascular compromise in the preterm newborn using a piglet model.
Methods:
Preterm and term piglets were assigned to either dopamine, dobutamine or control infusions. Heart rate, left ventricular contractility, cardiac output, blood pressure, and cerebral and regional blood flows were measured during baseline, low (10 µg/kg/h), and high (20 µg/kg/h) dose infusions.
Results:
At baseline, preterm piglets had lower cardiac contractility, cardiac output, blood pressure, and cerebral blood flow compared to term piglets. The response of preterm piglets to either dopamine or dobutamine administration was less than in term piglets. In both preterm and term piglets, cardiac output and cerebral blood flow were unaltered by either inotrope.
Conclusion:
In order to provide better cardiovascular support, it may be necessary to develop treatments that target receptors with a more mature profile than adrenoceptors in the preterm newborn.
Similar content being viewed by others
Main
During the first day of life, preterm infants are at high risk of circulatory failure leading to inadequate tissue perfusion (1). Impaired cerebral perfusion in preterm infants could contribute to an increased risk of neurodevelopmental delay, cerebral palsy, deafness, and vision impairments (2). In attempt to prevent this, dopamine and/or dobutamine are commonly used to support preterm cardiovascular function. These adrenergic inotropes target β1-adrenoceptors in the myocardium to increase myocardial contractility and heart rate hence increasing cardiac output and tissue perfusion. Dopamine can also increase systemic vascular resistance, which results in an increase in blood pressure, via activation of α-adrenoceptors. In contrast, dobutamine can reduce vascular resistance by stimulating vasodilator β2-adrenoceptors. About 40% of preterm newborns fail to respond to either dopamine or dobutamine (3,4), and there is limited evidence that these inotropes improve clinical outcomes of preterm newborns (5). Indeed, a recent study suggests that dopamine treatment may be harmful (6).
In preterm animal models, the distribution of adrenoceptor subtypes in the myocardium and vasculature is strikingly different from that seen in term animals (7,8,9). Preterm piglets have about 50% fewer β-adrenoceptors in the left ventricle compared with term piglets (9). A low density of myocardial β1-adrenoceptors in the preterm heart could lead to a poor cardiac response to dopamine and dobutamine in preterm infants. In addition, the preterm peripheral vasculature has fewer α1-adrenoceptors than at term in lambs (7,8), and so, it is likely that dopamine will be a less effective vasoconstrictor in preterm newborns than in term infants or adults.
In the present study, we aimed to describe the cardiovascular physiology of preterm and term piglets, and to determine how the cardiovascular actions (including effects on cerebral blood flow) of dopamine and dobutamine differed between preterm and term piglets. Preterm piglets were used because many piglets experience cardiovascular failure that includes the features commonly seen in preterm babies, even in the absence of other pathologies.
Results
Demographics and Baseline Physiology
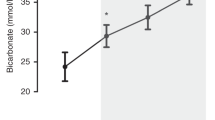
A total of 26 term and 24 preterm piglets were studied. The birthweight of piglets and the ratios of males and females in both term and preterm groups (P = 0.963), and in the treatment groups within each age were similar ( Table 1 ). Measures of cardiovascular function of term and preterm piglets prior to inotrope treatment are shown in Table 2 . Preterm piglets had significantly lower cardiac contractility and relaxation, cardiac output, blood pressures (mean, systolic, and diastolic), and cerebral blood flow (per 100 g) compared to term piglets despite a higher resting heart rate ( Table 2 ). Within each age group, cardiovascular function and organ blood flows were similar in control, dopamine and dobutamine-treated animals (P > 0.05) ( Figures 1 , 2 , 3 , 4 , 5 , and 6 ), except for preterm piglets used to study the effects of dobutamine. In these animals, baseline heart rate (P = 0.006, Figure 1 ) and diastolic blood pressure (P = 0.035) were significantly higher than in the control preterm group.
Heart rate, cardiac output, and mean arterial pressure (MAP) for control (a, d, and g), dopamine (b, e, and h) and dobutamine (c, f, and i) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose, and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. † indicates a significant difference between the magnitude of the term and preterm responses at that dose. n is 24 preterm and 26 term piglets for heart rate and MAP, and n is 15 preterm and 19 term piglets for cardiac output. Heart rate and MAP are expressed as mean ± SEM and cardiac output is expressed as median ± IQR.
Cardiac contractility and relaxation for control (a and d), dopamine (b and e) and dobutamine (c and f) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. † indicates a significant difference between the magnitude of the term and preterm responses at that dose. n is 24 preterm and 26 term piglets. Values are expressed as mean ± SEM.
Cerebral blood flow and vascular conductance for control (a and d), dopamine (b and e) and dobutamine (c and f) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose, and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. n is 13 preterm and 19 term piglets. Values are expressed as median ± IQR.
Vascular conductance of skeletal muscle and skin for control (a and d), dopamine (b and e) and dobutamine (c and f) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose, and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. n is 15 preterm and 19 term piglets. Values are expressed as median ± IQR.
Vascular conductance of small intestine and large intestine for control (a and d), dopamine (b and e) and dobutamine (c and f) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. n is 15 preterm and 19 term piglets. Values are expressed as median ± IQR.
Left ventricular (LV) coronary blood flow and renal blood flow for control (a and d), dopamine (b and e) and dobutamine (c and f) treated term (solid line) and preterm (dashed line) piglets during baseline, low dose, and high dose infusions. * indicates that the response to that drug is significantly different to changes in the control group at the same gestation. † indicates a significant difference between the magnitude of the term and preterm responses at that dose. n is 15 preterm and 19 term piglets. Values are expressed as median ± IQR.
For all measures, significant drug responses are reported relative to changes in the control group at the same gestation. Where a significant response was detected, the magnitude of that response was compared between the term and preterm groups.
Heart Rate
Heart rate was significantly increased in term and preterm piglets at both low and high doses of dopamine and dobutamine (for term piglets: dopamine low dose P = 0.022, high dose P < 0.001, and dobutamine low dose P = 0.002, high dose P < 0.001; for preterm piglets: dopamine low dose P = 0.049, high dose P = 0.002, and dobutamine low dose P = 0.004 and high dose P = 0.002, Figure 1 ). There were no differences in the magnitude of the heart rate responses of term and preterm piglets (P = 0.372 to 0.958).
Cardiac Contractility and Relaxation
Cardiac contractility was significantly increased in term and preterm piglets at both low and high doses of dopamine and dobutamine (for term piglets: dopamine low dose P = 0.027 and high dose P < 0.001, dobutamine low dose P = 0.022 and high dose P = 0.001; for preterm piglets: dopamine low dose P = 0.022 and high dose P < 0.001, and dobutamine low dose P = 0.031 and high dose P = 0.005, Figure 2 ). The magnitude of the increases in contractility of preterm piglets was less than that of term piglets for both drugs (P = 0.014 to 0.001).
Cardiac relaxation was not significantly altered in term and preterm piglets at low doses of either dopamine or dobutamine (for term piglets: dopamine P = 0.244 and dobutamine P = 0.464; for preterm piglets: dopamine P = 0.073 and dobutamine P = 0.124, Figure 2 ). However, cardiac relaxation was significantly increased in term and preterm piglets at high doses of dopamine and dobutamine (for term piglets: dopamine P = 0.022 and dobutamine P = 0.044; for preterm piglets: dopamine P < 0.001 and dobutamine P = 0.035, Figure 2 ). The magnitude of the responses in the preterm group were less than in term animals for both dopamine (P = 0.002) and dobutamine (P = 0.004).
Cardiac Output
There were no significant changes in cardiac output in term or preterm piglets during treatment with either inotrope (P = 0.132 to 0.819, Figure 1 ).
Blood Pressures
In term piglets, mean arterial pressure (MAP) significantly increased during treatment with dopamine (low dose P < 0.001, high dose P < 0.001) and with dobutamine (low dose P = 0.001, high dose P < 0.001, Figure 1 ). In preterm piglets, MAP also significantly increased during treatment with dopamine (low dose P = 0.030, high dose P < 0.001). Dobutamine treatment was ineffective at the low dose (P = 0.072) whereas at the high dose the increase in MAP was greater than in control piglets (P = 0.047) but this equated to an average increase of only 2 mmHg. The magnitude of the MAP response by preterm piglets was significantly less than the response in term piglets for both inotropes at both doses (P = 0.008 to 0.001, Figure 1 ). Changes in systolic and diastolic blood pressures induced by inotropes were similar to the changes in MAP.
Cerebral Blood Flow and Vascular Conductance
Cerebral blood flow was not significantly altered by dopamine or dobutamine at either dose in term and preterm piglets (term piglets dopamine P = 0.107 and dobutamine P = 0.672: preterm piglets dopamine P = 0.412 and dobutamine P = 0.756, Figure 3 ). We also calculated vascular conductance because flow is affected by driving pressure as well as vessel diameter so flow alone may not indicate the degree of vasoconstriction/vasodilatation. An increase in conductance indicates an increase in blood flow that is independent of driving pressure. In term piglets, cerebral vascular conductance during both low (P = 0.004) and high (P = 0.004) dose dopamine infusion was significantly lower than controls, but not during dobutamine infusion (P = 0.119). In preterm piglets, cerebral conductance was unaltered by inotrope infusions (P > 0.05).
Peripheral Vascular Conductance
In term piglets, skeletal muscle vascular conductance decreased during dopamine (low dose P = 0.043, high dose P = 0.007) but not dobutamine (P = 0.857) treatment ( Figure 4 ). In preterm piglets, skeletal muscle conductance decreased during high-dose dopamine treatment only (P = 0.039) and not during dobutamine infusion (P = 0.223). In term piglets, skin vascular conductance decreased only during high-dose dopamine (low dose P = 0.064, high dose P = 0.003) and was unaltered during dobutamine infusions (P = 0.695) ( Figure 4 ). In preterm piglets, skin conductance decreased during high-dose dopamine (P = 0.002) and during both doses of dobutamine (low dose P = 0.036, high dose P = 0.025). In term and preterm piglets, small intestine vascular conductance was not significantly altered by inotrope infusions (P < 0.05, Figure 5 ). In term piglets, large intestine vascular conductance was decreased by dopamine (low dose P = 0.005, high dose P = 0.005) but was unaltered by dobutamine (P = 0.854) ( Figure 5 ). In preterm piglets, large intestine conductance was unaltered by dopamine (P = 0.089) or dobutamine (P = 0.909).
Left Ventricular Coronary Flow and Coronary Vascular Conductance
In term piglets, left ventricular coronary blood flow was significantly increased by dopamine (low dose P = 0.031, high dose P = 0.005) and dobutamine (low dose P = 0.014, high dose P = 0.012) however, in preterm piglets, there were no significant effects of either inotrope (dopamine P = 0.872, dobutamine P = 0.711) ( Figure 6 ). In term piglets, vascular conductance was unaltered by dopamine (P = 0.238) however was increased by dobutamine (low dose P = 0.049, high dose P = 0.029). In preterm piglets, conductance was unaltered by dopamine (P = 0.150) or dobutamine (P = 0.362).
Renal Blood Flow and Vascular Conductance
In term piglets, renal blood flow was not affected by either dopamine (P = 0.135) or dobutamine infusion (P = 0.481) at either dose ( Figure 6 ). Similarly, in preterm piglets, renal blood flow was not affected by either low-dose dopamine (P = 0.056), nor by either dose of dobutamine (P = 0.814); however, the high dose of dopamine was associated with a significant increase in renal blood flow, averaging 36% (P = 0.008). Renal vascular conductance in preterm piglets during high dose dopamine infusion was higher than in controls (P = 0.034) but there were no other changes in renal conductance.
Discussion
Cardiovascular function in preterm piglets was significantly compromised compared to term piglets. Baseline cardiac contractility in preterm piglets was about two-thirds of that in term piglets. Similar reductions in contractility have been reported in preterm babies (10,11). There is evidence that the preterm myocardium is structurally immature (12,13) limiting both baseline contractility (14,15) and the response to inotropes. Baseline cardiac output in preterm piglets was approximately half of that in term piglets. This result is similar to that found in preterm babies (16,17) and the isolated piglet heart (15). The lower contractility of the preterm piglets is likely to significantly contribute to their lower cardiac output. Mean arterial pressure was also lower in preterm piglets and again this is similar to preterm babies.
Baseline cerebral blood flow in preterm piglets was only 50% that of term piglets. Low cerebral blood flow has also been reported in preterm human neonates where flow can be as low as 20% of adult values (18,19,20). This may reflect a lower oxygen requirement of the preterm brain (18) although a lower cerebral oxygen venous saturation and increased cerebral oxygen extraction suggest that cerebral blood flow in some preterm infants is lower than that required for normal oxygen delivery (19,21). There is also evidence of a significant cerebral hypoxic burden in many preterm infants over the first days after birth (22). In addition, cerebral autoregulation is inconsistent in very preterm infants (20,23). Together, these factors suggest that low cerebral blood flow could contribute to the high disability rate experienced by preterm newborns (2).
Effects of dopamine and dobutamine in preterm pigs were similar to those seen in preterm infants. In preterm infants, effects of dopamine and dobutamine are limited compared to term infants (24,25). Dopamine treatment in preterm infants leads to small increases in blood pressure but dobutamine treatment does not increase blood pressure (3). Neither inotrope alters right ventricular output in preterm infants although dobutamine treatment results in significantly greater increases in superior vena cava flow compared to dopamine (3).
Although the effects of dopamine and dobutamine on heart rate were similar in term and preterm piglets, the increases in contractility and blood pressure were less in preterm piglets. In preterm piglets, contractility was increased to the term resting range in response to dopamine, suggesting that lack of contractile machinery is not the major factor limiting the preterm response. The response of preterm piglets to dobutamine was more limited, and although the mean contractility in response to high dose dobutamine was similar to that seen in untreated term piglets, half of the group did not even achieve a contractility equivalent to term baseline following high-dose dobutamine infusion.
The smaller contractility and blood pressure response to dobutamine compared to dopamine in preterm piglets and infants may be due to the different receptor targets of these drugs. Dopamine can stimulate both β- and α-adrenoceptors (26). Although β1-adrenoceptors are considered the primary target when using dopamine for inotropic purposes, α1A-adrenoceptors are also capable of mediating a positive inotropic response (27,28,29). On the other hand, dobutamine acts specifically on cardiac β-adrenoceptors (30). We have shown that the expression of β1-adrenoceptors in the preterm piglet heart is less than in the term heart; this would limit the magnitude of preterm responses to β-agonists (9). Dopamine could produce a greater increase in contractility than dobutamine in the preterm heart if α1A-adrenoceptors as well as β1-adrenoceptors were activated by the inotrope.
The observed increases in mean arterial pressure, especially during dopamine infusion, are consistent with the known α-adrenoceptor-mediated constrictor actions of dopamine. This effect is apparent in our results for skeletal muscle and large intestine where conductance was decreased in term piglets treated with dopamine but not in those treated with dobutamine. This response was reduced or absent in preterm piglets where there are fewer α-adrenoceptors in the vasculature (7,8). These differences in adrenoceptor profile along with the differing targets of dopamine and dobutamine explain why the preterm piglets had smaller increases in blood pressure than term piglets and why responses to dobutamine at both ages were smaller than responses to dopamine. We were not able to detect decreases in vascular conductance of the small intestine. The small intestine appears very sensitive to ischemia and is perhaps therefore protected from vasoconstriction to some extent.
Heart rate was increased by dopamine and dobutamine in both preterm and term piglets but this increase in heart rate was not associated with an increase in cardiac output suggesting that stroke volume was negatively affected. Tachycardia leads to decreased ventricular filling time (31); however, dopamine and dobutamine are said to maintain or improve ventricular filling time by accelerating ventricular relaxation (27). Relaxation was reduced in preterm compared to term hearts, and at both ages was only increased at the highest dose of inotrope. Thus, reduced ventricular filling due to tachycardia may account for the lack of increase in cardiac output in some term and preterm piglets.
In the adult, dopamine and dobutamine promote ventricular relaxation by accelerating the uptake of calcium by the sarcoplasmic reticulum during diastole (32). However, the sarcoplasmic reticulum is thought to be under-developed in the neonatal heart (12) limiting its ability to sequester calcium during diastole. The consequences of this are apparent in our observations on cardiac relaxation ( Figure 2 ). Trials for more effective support for preterm cardiovascular function could focus on treatments that provide inotropic effects without significant chronotropic effects.
The lack of increase in cardiac output may also have been the result of increased afterload as there were significant increases in mean arterial pressure. Several clinical trials have reported decreased left ventricular output during dopamine infusion in preterm newborns, and this has been attributed to the inability of the preterm heart to pump against the increased afterload resulting from vasoconstriction (3,10,33). Eiby et al. (15) report that cardiac output was compromised when mean arterial pressure was above 45 mmHg. Three out of 10 piglets in our preterm dopamine group reached pressures above this level.
Dopamine and dobutamine infusion resulted in significant increases in left ventricular coronary blood flow in term animals but flow was unchanged in preterm piglets. This difference in flow may be related to the greater myocardial oxygen demand due to greater increases in contractility in term piglets than in preterm piglets. Alternatively, in preterm piglets, coronary flow may be limited by impaired relaxation as coronary flow occurs during diastole. A failure to increase coronary flow could act to limit inotropic effects of both treatments in preterm piglets by failing to increase oxygen delivery in the face of increased myocardial workload (as demonstrated by the documented increases in both contractility and heart rate).
Cerebral blood flow was not significantly changed in response to either inotrope in either term or preterm piglets. In term piglets treated with dopamine, there was a reduction in cerebral vascular conductance suggesting vasoconstriction. We are unable to determine if this is an autoregulatory response to the increase in blood pressure, to maintain a constant cerebral blood flow, or if dopamine has had a direct vasoconstrictor effect on the cerebral blood vessels, as has been suggested in other studies (34). This response did not occur where increases in blood pressure were smaller—during dobutamine infusion or in response to either drug in preterm piglets. If the aim of inotropic support is to increase cerebral blood flow, this was not achieved in our piglet cohort.
When assessing the efficacy of an intervention, it is important to consider whether routine measures are the best indicators of the relevant outcome. There was no increase in cerebral blood flow despite increases in mean arterial pressure. This may be due to autoregulation although several clinical studies have suggested that autoregulation does not occur in the blood pressure range commonly observed in very preterm infants (20,23). Alternatively, the absence of an increase in cerebral blood flow may be due to the lack of change in cardiac output. Cerebral blood flow and developmental outcomes may be more closely related to systemic blood flow than to blood pressure underlining the idea that normal or altered blood pressure should not be taken as an indication that cerebral flow is normal or altered (6,35). Likewise, urine output is often taken as an indicator of cardiovascular function. In our study, renal blood flow in preterm piglets was not different from that of term piglets and this may lead to preservation of urine production, incorrectly suggesting similar cardiovascular function. Similarly, renal blood flow was increased in dopamine-treated preterm pigs. This increase in renal blood flow, along with dopamine’s action to block sodium reabsorption, could lead to an increase in urine output and in isolation may erroneously be interpreted as an indication that other aspects of cardiovascular function have improved. In the preterm piglet, neither arterial blood pressure nor renal blood flow appear to be good indicators of cardiac output or cerebral blood flow. This may also be the case in preterm babies, even at the extremes of blood pressure and urine output.
Measurements of blood flow obtained using coloured microspheres could have been affected by blood flow through the ductus arteriosus. A left-to-right shunt would act as an additional organ in the system, but would not introduce any errors into the measurements of flow to other organs. A right-to-left shunt would reduce the concentration of microspheres in the descending aorta, thus reducing the number of microspheres in the reference blood sample. The calculation of blood flow to postductal organs would not be affected as all organs receive blood with the same reduced concentration of microspheres as the reference sample. Calculation of flow to preductal organs such as the brain would be artificially elevated, as the concentration of microspheres in the blood received by the brain would be greater than that in the reference sample. Measurement of cardiac output would similarly be affected. For baseline flows, this means that cardiac output and cerebral blood flow in preterm pigs, where shunting may be more common, are possibly lower than our results suggest—thus the differences between term and preterm piglets may be even larger than those we have reported. The lack of effect of dopamine and dobutamine on cardiac output and cerebral blood flow may be the result of a reduction in right-to-left ductal flow during inotrope infusion however, the observed lack of decrease in oxygen requirements during treatment would make this very unlikely.
Our findings are unlikely to be the result of interactions between inotropes and the sedation used. Propofol levels can fall when cardiac output goes up (36). However, cardiac output did not change and responses were not different between preterm and term piglets. Therefore, differences in response to inotropes are unlikely to be due to differing interactions between sedation and inotropes.
In conclusion, cardiovascular function in preterm piglets is impaired relative to term piglets. Significantly, the likelihood that either dopamine or dobutamine will increase blood pressure and cardiac contractility is much less in preterm than in term piglets. These reduced responses may be the result of low β-adrenoceptor density in the preterm heart and low α-adrenoceptor density in the preterm vasculature. Cerebral blood flow and cardiac output in preterm piglets were lower than in term piglets and were not altered by treatment with dopamine or dobutamine. In order to provide better cardiovascular support and improve outcomes, it may be necessary to develop treatments that target receptors with a more mature profile than adrenoceptors in the preterm newborn, or treatments that target other mechanisms entirely.
Methods
This study was carried out in accordance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes (7th edition 2004) and was approved by The University of Queensland Animal Ethics Committee (AEC Approval Number: UQCCR/060/12). All surgery was performed under general anesthesia and all efforts were made to minimize suffering. All animals were euthanized with Lethabarb intravenous (i.v.) (162mg/kg Pentobarbitone Sodium; Virbac, Australia).
Piglet Delivery, Intensive Care, and Physiological Monitoring
Preterm piglets were delivered and cared for as previously described (37,38). In brief, preterm piglets were exposed to maternal glucocorticoid treatment (betamethasone 0.19 mg/kg, intramuscular (i.m.); Celestone Chronodose, Schering-Plough) at 48 and 24 h prior to delivery according to standard clinical practice for women with threatened preterm labour. All piglets were delivered by cesarean section either “preterm” at 97 d (developmentally similar to a human neonate at 27 wk gestation) or near “term” at 113 d (full term = 115 d). A loading dose of 5 mg/kg of propofol (Provive MCT-LCT 1%; AFT Pharmaceuticals, NZ) was given at birth. Term piglet sedation was maintained throughout the experiment using 4–20 mg/kg/h of propofol and 0.02–0.11 mg/kg/h of fentanyl (Sublimaze; Janssen-Cilag, AUS). Preterm piglet sedation was maintained using 6–10 mg/kg/h of propofol and 0.03–0.06 mg/kg/h fentanyl. The infusion rate was titrated to achieve a heart rate of 120–160 bpm and was always in the lower part of the range during experiments. Piglets were intubated with a 2.5–3.0 cuffed/un-cuffed endotracheal tube and surfactant administered to preterm piglets (2.5 ml endotracheal; Survanta; Abbott Australasia, Australia).
A 16-channel Power Lab and LabChart 7 (AD Instruments Pty Ltd, Australia) was used to record all physiological variables (sampling frequency of 1 kHz). Arterial blood pressure was monitored using a pressure transducer (Transpac, Hospira, Dunedin, New Zealand) connected to an umbilical artery catheter. Heart rate was calculated from the arterial blood pressure wave. To measure cardiac contractility and relaxation, a dual lumen catheter containing a pressure catheter (Transonic SciSense, Canada) was inserted into the left ventricle via the left carotid artery. Contractility (dP/dtmax) and relaxation (dP/dtmin) were calculated using LabChart.
Oxygen saturation (measured using pulse oximetry) and intermittent arterial blood gas analysis (ABL800Flex Blood Gas Analyser; Radiometer, DK) were used to monitor ventilation adequacy. Fractional inspired oxygen and peak inspiratory pressure were adjusted to target PaO2 80–120 mmHg and PaCO2 35–45 mmHg. Skin blood flow (SBF) was measured using a laser Doppler flowmetry (LDF) surface probe (AD Instruments Pty Ltd) adhered to the hindquarter.
Regional Blood Flow
Coloured microspheres (Dye-Trak 15 µm microspheres, Triton Technology) were injected into the left ventricle via the ventricular catheter to provide intermittent measures of regional blood flow at three time points (39). A reference blood sample was collected in accordance with the validated method (40). Microspheres were extracted from the tissue using the filtration method. Organ blood flows (cerebral hemispheres, gluteal muscle, abdominal skin, small intestine, large intestine, left ventricle, kidney) were calculated by comparison of the number of microspheres in the tissue with that in the reference blood sample. Cardiac output was calculated using the formula:
Cardiac output = total number of microspheres injected × reference sample withdrawal rate/number of microspheres in reference sample (41).
Organ blood flows were used to calculate vascular conductance (blood flow/mean arterial blood pressure).
Experimental Design
Piglets were assigned to receive intravenous dopamine (Hamlen Pharmaceuticals, DE; 10% glucose), dobutamine (Sandoz, Australia; 10% glucose), or control (10% glucose). Siblings of the same sex were assigned to different treatment groups. Baseline measurements were recorded for 30 min. Low-dose inotrope (10 µg/kg/min) was infused for 40 min via the umbilical vein then high-dose inotrope infusion (20 µg/kg/min) for 40 min. Microspheres were injected at the end of baseline, low-dose and high-dose infusions. All piglets were euthanized (sodium pentobarbital 60 ml i.v.) following the inotrope infusions.
Data Processing and Statistical Analyses
Cardiac contractility and relaxation, heart rate, arterial pressures, and skin blood flow were calculated over a 2 min period immediately before microsphere injections, providing three timepoints; baseline, low dose, and high dose. All data were analyzed using SPSS version 22, IBM. Differences in sex ratios between age groups, and differences between treatment groups within age groups, were assessed using Chi-square tests. Cardiac output and blood flow data were log transformed prior to analysis using parametric tests. Difference in baseline measures between preterm and term piglets were sought using Student’s independent samples t-tests. To test for differences in baseline measures between treatment groups within an age group, one-way ANOVAs with treatment as a fixed factor were used. To test for treatment effects within each age group, univariate repeated measures ANOVAs with two fixed factors—dose/time (baseline, low dose and high dose) and treatment (control and drug)—were used separately for dopamine and dobutamine. Where there was no significant overall interaction, this means control and drug-treated groups changed similarly across time, i.e., there was effect of drug treatment. Where there was a significant overall interaction, simple contrasts were used to determine at which dose drug responses differed to the control group. To determine if the preterm response for a particular drug differed from the term response, similar tests were used except the two fixed factors were dose (baseline, low dose and high dose) and gestational age (preterm and term). A P value <0.05 was considered statistically significant.
Statement of Financial Support
The project was funded by a National Health and Medical Research Council project grant (GNT1028888) and a Royal Brisbane and Womens Hospital Foundation project grant (2014002740).
Disclosure
The authors have no conflicts of interest to declare.
References
Osborn DA. Diagnosis and treatment of preterm transitional circulatory compromise. Early Hum Dev 2005;81:413–22.
Hunt RW, Evans N, Rieger I, Kluckow M. Low superior vena cava flow and neurodevelopment at 3 years in very preterm infants. J Pediatr 2004;145:588–92.
Osborn D, Evans N, Kluckow M. Randomized trial of dobutamine versus dopamine in preterm infants with low systemic blood flow. J Pediatr 2002;140:183–91.
Valverde E, Pellicer A, Madero R, Elorza D, Quero J, Cabañas F. Dopamine versus epinephrine for cardiovascular support in low birth weight infants: analysis of systemic effects and neonatal clinical outcomes. Pediatrics 2006;117:e1213–22.
Osborn DA, Paradisis M, Evans N The effect of inotropes on morbidity and mortality in preterm infants with low systemic or organ blood flow. Cochrane Database Syst Rev 2007 24:CD005090.
Batton B, Li L, Newman NS, et al.; Eunice Kennedy Shriver National Institute of Child Health & Human Development Neonatal Research Network. Early blood pressure, antihypotensive therapy and outcomes at 18-22months’ corrected age in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed 2016;101:F201–6.
Su C, Bevan JA, Assali NS, Brinkman CR 3rd . Regional variation of lamb blood vessel responsiveness to vasoactive agents during fetal development. Circ Res 1977;41:844–8.
Shaul PW, Magness RR, Muntz KH, DeBeltz D, Buja LM. Alpha 1-adrenergic receptors in pulmonary and systemic vascular smooth muscle. Alterations with development and pregnancy. Circ Res 1990;67:1193–200.
Kim MY, Finch AM, Lumbers ER, et al. Expression of adrenoceptor subtypes in preterm piglet heart is different to term heart. PLoS One 2014;9:e92167.
Osborn DA, Evans N, Kluckow M. Left ventricular contractility in extremely premature infants in the first day and response to inotropes. Pediatr Res 2007;61:335–40.
Takahashi Y, Harada K, Kishkurno S, Arai H, Ishida A, Takada G. Postnatal left ventricular contractility in very low birth weight infants. Pediatr Cardiol 1997;18:112–7.
Smolich JJ. Ultrastructural and functional features of the developing mammalian heart: a brief overview. Reprod Fertil Dev 1995;7:451–61.
Kim MY, Eiby YA, Lumbers ER, et al. Effects of glucocorticoid exposure on growth and structural maturation of the heart of the preterm piglet. PLoS One 2014;9:e93407.
Kawamura Y, Ishiwata T, Takizawa M, Ishida H, Asano Y, Nonoyama S. Fetal and neonatal development of Ca2+ transients and functional sarcoplasmic reticulum in beating mouse hearts. Circ J 2010;74:1442–50.
Eiby YA, Lumbers ER, Headrick JP, Lingwood BE. Left ventricular output and aortic blood flow in response to changes in preload and afterload in the preterm piglet heart. Am J Physiol Regul Integr Comp Physiol 2012;303:R769–77.
Groves AM, Chiesa G, Durighel G, et al. Functional cardiac MRI in preterm and term newborns. Arch Dis Child Fetal Neonatal Ed 2011;96:F86–91.
Kluckow M, Evans N. Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 2000;82:F182–7.
Altman DI, Perlman JM, Volpe JJ, Powers WJ. Cerebral oxygen metabolism in newborns. Pediatrics 1993;92:99–104.
Greisen G, Børch K. White matter injury in the preterm neonate: the role of perfusion. Dev Neurosci 2001;23:209–12.
Munro MJ, Walker AM, Barfield CP. Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004;114:1591–6.
Andersen CC, Stark MJ. Haemoglobin transfusion threshold in very preterm newborns: a theoretical framework derived from prevailing oxygen physiology. Med Hypotheses 2012;78:71–4.
Hyttel-Sorensen S, Pellicer A, Alderliesten T, et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ 2015;350:g7635.
Peeples ES, Mehic E, Mourad PD, Juul SE. Fast Doppler as a novel bedside measure of cerebral perfusion in preterm infants. Pediatr Res 2016;79:333–8.
Bravo MC, López-Ortego P, Sánchez L, et al. Randomized, Placebo-Controlled Trial of Dobutamine for Low Superior Vena Cava Flow in Infants. J Pediatr 2015;167:572–8.e1–2.
Mahoney L, Shah G, Crook D, Rojas-Anaya H, Rabe H. A Literature Review of the Pharmacokinetics and Pharmacodynamics of Dobutamine in Neonates. Pediatr Cardiol 2016;37:14–23.
Seri I, Rudas G, Bors Z, Kanyicska B, Tulassay T. Effects of low-dose dopamine infusion on cardiovascular and renal functions, cerebral blood flow, and plasma catecholamine levels in sick preterm neonates. Pediatr Res 1993;34:742–9.
Lin F, Owens WA, Chen S, et al. Targeted alpha(1A)-adrenergic receptor overexpression induces enhanced cardiac contractility but not hypertrophy. Circ Res 2001;89:343–50.
Sjaastad I, Schiander I, Sjetnan A, et al. Increased contribution of alpha 1- vs. beta-adrenoceptor-mediated inotropic response in rats with congestive heart failure. Acta Physiol Scand 2003;177:449–58.
Terzic A, Pucéat M, Vassort G, Vogel SM. Cardiac alpha 1-adrenoceptors: an overview. Pharmacol Rev 1993;45:147–75.
Ruffolo RR Jr . The pharmacology of dobutamine. Am J Med Sci 1987;294:244–8.
Trinity JD, Pahnke MD, Lee JF, Coyle EF Interaction of hyperthermia and heart rate on stroke volume during prolonged exercise. J Appl Physiol (1985) 2010 109:745–51.
Cucchini F, Bolognesi R, Javernaro A, Zeppellini R, De Domenico R, Visioli O. Do inotropic drugs always induce a positive lusitropic effect? A comparison between k-strophanthidin and dobutamine in patients with coronary artery disease. Eur Heart J 1994;15:1666–72.
Rozé JC, Tohier C, Maingueneau C, Lefèvre M, Mouzard A. Response to dobutamine and dopamine in the hypotensive very preterm infant. Arch Dis Child 1993;69(1 Spec No):59–63.
Eriksen VR, Hahn GH, Greisen G. Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatr 2014;103:1221–6.
Logan JW, O’Shea TM, Allred EN, et al.; ELGAN Study Investigators. Early postnatal hypotension and developmental delay at 24 months of age among extremely low gestational age newborns. Arch Dis Child Fetal Neonatal Ed 2011;96:F321–8.
Kurita T, Morita K, Kazama T, Sato S. Influence of cardiac output on plasma propofol concentrations during constant infusion in swine. Anesthesiology 2002;96:1498–503.
Eiby YA, Wright LL, Kalanjati VP, et al. A pig model of the preterm neonate: anthropometric and physiological characteristics. PLoS One 2013;8:e68763.
Eiby YA, Lumbers ER, Staunton MP, et al. Endogenous angiotensins and catecholamines do not reduce skin blood flow or prevent hypotension in preterm piglets. Physiol Rep 2014;2:e12245.
Walter B, Bauer R, Gaser E, Zwiener U. Validation of the multiple colored microsphere technique for regional blood flow measurements in newborn piglets. Basic Res Cardiol 1997;92:191–200.
Makowski EL, Meschia G, Droegemueller W, Battaglia FC. Measurement of umbilical arterial blood flow to the sheep placenta and fetus in utero. Distribution to cotyledons and the intercotyledonary chorion. Circ Res 1968;23:623–31.
McDevitt DG, Nies AS. Simultaneous measurement of cardiac output and its distribution with microspheres in the rat. Cardiovasc Res 1976;10:494–8.
Acknowledgements
The authors wish to acknowledge the important role of the large team involved in the intensive care of the piglets, particularly Nicole Weatherley, Sonia Sam, Kelsey Heng, Layne Wright, Melissa Lai, Shimodi Kuruneru, Alexander Kanon and of the veterinary team primarily involved in the cesarean sections, Cora Lau, Helen Keates, and Ranald Cameron.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eiby, Y., Shrimpton, N., Wright, I. et al. Inotropes do not increase cardiac output or cerebral blood flow in preterm piglets. Pediatr Res 80, 870–879 (2016). https://doi.org/10.1038/pr.2016.156
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.156
This article is cited by
-
Red cell infusion but not saline is effective for volume expansion in preterm piglets
Pediatric Research (2023)
-
Dobutamine treatment reduces inflammation in the preterm fetal sheep brain exposed to acute hypoxia
Pediatric Research (2018)