Abstract
Background:
N-terminal pro-B-type natriuretic peptide (nt-proBNP) is an established marker of heart failure in adult cardiology. We analyzed nt-proBNP in the circulation of fetuses with increased volume load secondary to anemia and investigated the effect of treatment on nt-proBNP concentration.
Methods:
Fetuses undergoing intrauterine transfusion (IUT) were examined. nt-proBNP was measured before IUT and correlated with hemoglobin concentrations, ultrasonographic findings, and Doppler measurements of the peak systolic velocity of the middle cerebral artery (MCA-PSV).
Results:
A total of 27 patients (7 with hydrops) and 78 controls were examined. nt-proBNP was markedly elevated in anemia (P < 0.001). Concentrations were highest in hydropic fetuses (P < 0.03); no differences were present in hemoglobin and MCA-PSV values between hydropic and nonhydropic cases. In fetuses undergoing multiple IUTs nt-proBNP normalized after the third IUT, whereas hemoglobin and MCA-PSV remained abnormal.
Conclusion:
Levels of circulating nt-proBNP correlate well with the degree of myocardial workload in the hyperdynamic state of fetal anemia. We hypothesize that normalization of nt-proBNP after serial transfusions is an indicator of myocardial adjustment to chronic anemia. nt-proBNP measurement may be useful in the management of fetal anemia, particularly in cases at risk of hydrops and fetuses requiring multiple transfusions.
Similar content being viewed by others
Main
Anemia increases workload on the fetal heart; in order to maintain tissue oxygenation, the combined cardiac output is increased. The hyperdynamic circulation is characterized by a rise in myocardial stretching and filling pressures, reduced afterload, and cardiomegaly (1). Myocardial perfusion in particular is dependent on oxygen supply. Adaptive mechanisms allow a four- to fivefold increase in coronary perfusion and include increased coronary perfusion pressure, decreased coronary resistance, and autoregulation (2). If these adaptations fail to meet oxygen demand, myocardial ischemic changes occur, eventually resulting in decreased myocardial function and dilated cardiomyopathy. Although the precise mechanisms are debated, the development of hydrops in fetal anemia heralds deterioration of the fetal status and impending death.
In adult cardiology brain natriuretic peptide (BNP) and its inactive cleavage product n-terminal pro-B-type natriuretic peptide (nt-proBNP) are established markers of heart failure supporting diagnosis, risk stratification, and treatment response monitoring (3,4). Elevated BNP concentrations result from re-expression of the cardiac embryonic gene program and induce cardiac remodeling and fibrosis (5,6). The natriuretic peptide system is functional by mid-gestation (7).
We hypothesized that the hyperdynamic circulation present in fetal anemia may result in increased levels of circulating nt-proBNP. Therefore, nt-proBNP was measured before intrauterine transfusion (IUT) and correlated to hemoglobin concentrations and ultrasonographic and Doppler findings. Furthermore, the effect of treatment on nt-proBNP concentration was assessed in cases with multiple IUTs.
Results
Patients
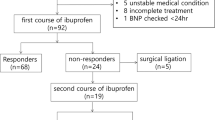
In total, 27 patients were recruited; hydrops was present in 7. Anemia was caused by the following conditions: Rhesus alloimunization (n = 10); parvovirus-B19 infection (n = 8); tumors with associated hemorrhage (n = 5); chronic fetomaternal hemorrhage (n = 2); and elliptocytosis and unknown (one case each). Cases with parvovirus-B19 infection were equally distributed in the nonhydropic and hydropic groups. Procedure-related complications and intrauterine or perinatal deaths did not occur. The median time between the first and second IUT was 6.0 d (range 1–21); the median number of IUTs per patient was 3.0 (range 1–7).
Anemia was classified as mild in six, moderate in four, and severe in 12 fetuses. One case of known Rhesus alloimmunization received the first IUT at 23 wk of gestation; hemoglobin and peak systolic velocity of the middle cerebral artery (MCA-PSV) were within normal range before the first transfusion. Another patient with normal hemoglobin concentration had signs of hyperdynamic cardiac dysfunction at 14 wk of gestation, when the first IUT was undertaken. Subsequently, chronic fetomaternal hemorrhage was diagnosed and five more IUTs were performed. Samples for hemoglobin or nt-proBNP measurement could not be collected before the first transfusion in two and three fetuses, respectively. Median gestational age (GA) of the study group was 23.0 wk (range 14–33). There was no difference in GA between cases and controls nor between cases with and without hydrops.
nt-proBNP
Nt-proBNP concentrations before treatment are detailed in Table 1 . Plasma levels were higher in the anemic group and increased with disease severity. Hydropic fetuses had higher levels of circulating nt-proBNP as compared with nonhydropic cases (see Figure 1 ). On the basis of these findings, nt-proBNP <10,000 ng/l had a negative predictive value of 100% for identification of fetal hydrops, with a positive predictive value of 44.4%. Subgroup analysis revealed no difference in nt-proBNP levels of fetuses with parvovirus-B19-associated anemia.
Hemoglobin and MCA-PSV levels did not differ in hydropic and nonhydropic fetuses. Correlation between nt-proBNP and hemoglobin and between MCA-PSV and hemoglobin was good (r = −0.637 and r = −0.626, respectively); no correlation was present between nt-proBNP and MCA-PSV. Doppler flow velocity waveform indexes of the ductus venosus were within normal range for GA with the exception of two cases (both nonhydropic) showing increased pulsatility; indexes for umbilical artery and uterine artery were within normal range in all cases.
Cardiothoracic area ratio was increased in anemic fetuses before treatment (median 0.337, interquartile range 0.066); no difference was present between hydropic and nonhydropic cases. Correlation between cardiothoracic area ratio and nt-proBNP was moderate (r = 0.477); no correlation was detected between cardiothoracic area ratio and hemoglobin or MCV-PSV.
Changes in nt-proBNP, hemoglobin, and MCA-PSV levels during the course of treatment are detailed in Table 2 . After the first IUT, nt-proBNP levels dropped significantly; concentrations in initially hydropic cases were comparable with the remaining group. Pre- and posttransfusion values for hemoglobin and MCA-PSV did not change significantly, and no correlation was present between any of the variables after the first IUT. nt-proBNP normalized after the third IUT (P = 0.116). In contrast, hemoglobin and MCA-PSV values remained abnormal (see Table 2 ).
Discussion
We found elevated levels of circulating nt-proBNP in fetuses with high cardiac output secondary to anemia. Concentrations correlated well with the degree of anemia. Peak nt-proBNP levels were present in cases with hydrops. Treatment resulted in a significant decrease and eventually normalization of nt-proBNP values despite persistently abnormal hemoglobin and MCA-PSV measurements.
As compared with postnatal life, nt-proBNP concentrations are higher in the human fetus (8). The difference is not because of maternal/placental transfer or differences in metabolic pathways (7,9) but may be a consequence of the reduced compliance of the immature fetal myocardium. Parallel to the decrease in left-ventricular afterload with advancing gestation and maturation of the fetal myocardium, plasma levels gradually decrease (8). Placental expression of atrial natriuretic peptide, but not BNP, has been proven and may be involved in vasodilatation of the feto-placental vascular bed (7).
The longer half-life and higher stability make nt-proBNP a more reliable parameter as compared with BNP (10). However, values are assay-specific with limited comparability (11,12). In addition, cross-reactivity with pro-BNP, the precursor form with six- to eightfold lower biological activity, and glycosylated forms of BNP has been demonstrated (13). This is of particular importance as patients with heart failure have evidence of increased levels of circulating pro-hormone (14,15). Further studies are needed to address this subject.
A role of nt-proBNP in cardiovascular dysfunction during fetal life has been demonstrated by investigations of cases with growth restriction secondary to uteroplacental dysfunction and fetuses with structural cardiac defects. Fetal growth restriction results in increased left-ventricular output and decreased right-ventricular output, followed by diastolic dysfunction and cardiac compromise (16); a significant correlation of nt-proBNP and early markers of cardiac dysfunction in fetal growth restriction was found (17,18,19). Cardiac malformations have the potential to alter loading conditions during fetal life; increased levels of circulating nt-proBNP have been detected in fetal and umbilical cord blood samples (19,20). Concentrations were highest in cases with left- or right-ventricular outflow tract obstructions with intact ventricular septum; the associated rise in ventricular wall tension was assumed to be a potent stimulus for nt-proBNP secretion (21).
Our study is the first to report nt-proBNP levels in volume load secondary to anemia during intrauterine life. We have no direct measurements of cardiac stress, strain, or performance but inferred myocardial behavior from studies cited above. The close correlation between hemoglobin and nt-proBNP values allows the conclusion that nt-proBNP is secreted in response to the increased cardiac output required to compensate for the reduced oxygen-carrying capacity of the blood.
The development of hydrops is associated with worse fetal outcome. Current concepts on the pathophysiology of hydrops in anemia include genuine myocardial failure, high cardiac output failure, reduced plasmatic colloid-oncotic pressure, increased capillary permeability, and obstruction of venous and subsequently lymphatic flow. We found significantly higher nt-proBNP concentrations in hydropic fetuses; these results support a myocardial cause of hydrops development in anemia. The increased total feto-placental blood volume present only in hydropic fetuses with anemia (22) may exceed the myocardial capacity, resulting in high cardiac output failure; on the other hand increased end-diastolic ventricular pressure and reduced coronary perfusion pressure may induce hypoxic myocardial dysfunction. Our data do not allow a differentiation between these mechanisms. Investigating parameters of myocardial injury may help to clarify this issue.
This study confirms previous results of ductus venosus blood flow indexes in fetal anemia (1,23). A rise in precordial vein pressure is likely to be a late finding, confirming the adaptability of the fetal myocardium to the hyperdynamic circulation. Parvovirus-B19-associated myocarditis may impair myocardial function (24). We could not detect an impact of infection on nt-proBNP concentrations.
The normalization of circulating nt-proBNP after three IUTs despite persistently abnormal hemoglobin levels is remarkable given that the oxygen dissociation curve is more unfavorable for adult red blood cells (RBCs), and consequently a higher cardiac output is required for tissue oxygenation. This finding may be an indicator of the myocardial adjustment to increased workload, illustrating the plasticity of the fetal heart. Adaptive cardiac mechanisms to chronic anemia have been investigated in animals. Chronically anemic sheep fetuses show increases in myocardial mass and vascularization as well as changes in the expression of various angiogenic, hypoxia-related, and glycolytic genes (25,26). Furthermore, cardiac remodeling induced by chronic intrauterine anemia results in increased contractile response and coronary conductance in adult animals (27,28). Rheological changes secondary to the presence of adult RBCs in the fetal circulation may be an alternative explanation for the normalization of nt-proBNP despite persistent anemia. As compared with fetal RBCs, adult RBCs are smaller with less rigid cell membranes; in addition, the proportion of nucleated RBCs is lower. These factors may alleviate cardiac workload even in the presence of increased cardiac output.
The number of cases is small, limiting the significance of our findings. However, cases were carefully selected and fetuses with conditions that potentially exert an effect on any of the variables under investigation were excluded. We therefore assume our results to be valid. In addition, hemoglobin levels in the control group were not available, so comparisons were performed with calculated reference values. As fetuses in the control group did not have any malformation with potential impact on hemoglobin concentration or MCA-PSV levels and because echocardiographic and Doppler investigations were normal, we are confident that a systematic error was avoided.
Although an invasive procedure measurement of nt-proBNP provides insight into myocardial function and may be a useful adjunct in the management of fetal anemia. Noninvasive tests such as myocardial performance indexes (Doppler and tissue Doppler) and those of myocardial velocity, strain, and strain rates (speckle tracing) can give clues to cardiac dysfunction, but their clinical relevance for fetal monitoring and surveillance requires further evaluation (29). In severely anemic fetuses, hemoglobin and MCA-PSV measurements are not able to predict hydrops (30). Likewise, the decreasing sensitivity of MCA-PSV to detect fetal anemia after a previous IUT precludes its application in the management of cases with multiple IUTs (31). In these situations, nt-proBNP may provide valuable information given its high negative predictive value.
In conclusion, nt-proBNP correlates well with the degree of myocardial workload in the hyperdynamic state of fetal anemia. The normalization of circulating nt-proBNP after serial IUTs despite persistent anemia may indicate myocardial adjustment to increased workload. Incorporation of nt-proBNP measurement may be a useful tool for the management of fetal anemia, particularly in cases at risk of hydrops and after multiple transfusions.
Methods
Study Population
Women referred to our Center of Prenatal Medicine between May 2006 and February 2010 with a suspected diagnosis of fetal anemia were eligible. Cases with anemia confirmed by fetal blood sampling who underwent IUT into the extra-abdominal part of the umbilical vein were included. Hydrops was defined as fluid accumulation in at least two of the following fetal compartments: skin, serous cavities (pleural or pericardial effusion), ascites, or polyhydramnios. Serologic tests were obtained in cases with suspected infection. None of the fetuses had any structural malformation, and all were appropriate for GA (estimated fetal birth weight >10th percentile). GA was confirmed by first-trimester ultrasonographic examination.
Previously established reference values served as controls (8). They were taken from fetuses that underwent fetocide within the context of termination of advanced pregnancy or cordocentesis for fetal platelet analysis in cases with human platelet antigen alloimmunization. Due to ongoing recruitment, 78 samples were available. Fetuses in the control group presented none of the following conditions that potentially exert an influence on nt-proBNP concentration: cardiac, urogenital, thoracic, skeletal or gastrointestinal malformations; neuromuscular disorders; tumors; hydrops; infections; and fetal growth restriction (estimated fetal birth weight <10th percentile). Monochorionic twin pregnancies were also excluded. Doppler indexes for umbilical artery, ductus venosus, and MCA were within normal range, and no fetus had any evidence of cardiac dysfunction by echocardiography. Hemoglobin values were not available for the control group. The study was conducted in accordance with human subject research guidelines and the Declaration of Helsinki and was approved by the University Bonn Review Board. Informed consent was obtained from all subjects.
Ultrasonographic and Echocardiographic Evaluation
High-resolution ultrasound equipment was used in all cases. The high-pass-filter was set at 60 Hz, and the spatial peak temporal average power output was kept at <100 W/cm2, applying only the fetal-use-adapted ultrasound machine settings. A detailed assessment of the fetal anatomy and cardiovascular status including echocardiography and Doppler examination was performed in subjects and controls. Doppler recordings of blood flow in the MCA and umbilical artery were obtained at an insonation angle between 0° and 10° to flow and <30° for ductus venosus and uterine arteries, using standard positioning of the sample volume; angle correction was not performed. At least five consecutive uniform Doppler velocity waveforms with the highest velocities and a narrow band of frequencies were recorded, and one cycle was analyzed. Indexes were calculated accordingly; abnormal values were defined as umbilical artery pulsatility index >90th percentile for GA or absent or reversed end-diastolic flow; ductus venosus pulsatility index for veins >90th percentile for GA or negative a-wave; uterine artery resistance index >90th percentile for GA or bilateral notching; MCA-PSV >1.28 times the median for GA. All examinations were performed before invasive intervention.
Diagnosis and Treatment Protocol for Fetal Anemia
Our center’s management protocol for suspected anemia stipulates establishing a diagnosis by ultrasound and Doppler studies. GA-adjusted multiples of median (MoMs) for MCA-PSV are applied to assess the degree of anemia (30). On the basis of these findings, arrangements for IUT are undertaken. Packed red cells are prepared to a hematocrit level of 72 and a hemoglobin level of 23–24 mg/dl. The transfusion volume is calculated (30–40 ml/kg), aiming for maximum blood volume expansion of 30–40 ml/kg fetal estimated weight per IUT. Our policy is to limit the transfusion volume to 50 ml per IUT to avoid acute volume overload, particularly in hydropic fetuses. In cases with severe anemia we prepare for a second IUT 2 d later. Fetal blood sampling and IUT are performed in one procedure, without fetal sedation or muscle relaxation. The umbilical vein in the umbilical cord is punctured under ultrasound control, if possible near its placental insertion site. After the procedure the patient remains under observation for 24 h. Thereafter, a control ultrasound examination is performed and further management is decided, taking the underlying diagnosis and degree of anemia into consideration. Subsequent IUTs follow the same protocol.
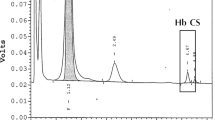
Sample Collection and Processing
Specimens were collected during the IUT procedure, after collection of the full blood count sample, and before commencement of transfusion. One milliliter of fetal venous blood was withdrawn. nt-proBNP was measured with a commercially available chemiluminescence immunoassay on a Dimension Vista 1500 (Siemens Healthcare Diagnostics, Eschborn, Germany) according to the manufacturer’s instructions. All samples were processed within 2 h. Inter- and intra-assay coefficients of variation were 3.5 and 2.3%, respectively. Fetal full blood count was analyzed on a KX21 hematology analyzer (Sysmex, Norderstedt, Germany).
Statistical Analysis
To adjust for the effect of GA, hemoglobin values were transformed into MoMs (30). Expected hemoglobin values were calculated with the following formula: e(2.84–8.55/GA). MoMs were then calculated by dividing the measured values by the expected values. Anemia was classified as mild (0.84–0.65 MoM), moderate (0.64–0.55 MoM), or severe (<0.55 MoM) (30). Values for MCA-PSV were MoM-transformed accordingly, using the following formula for expected MCA-PSV values: e(2.31+0.046 GA). Anemia according to MCA-PSV values was classified as mild (1.29–1.49 MoM), moderate (1.50–1.54 MoM), and severe (≥1.55 MoM) (30). For normally distributed values, between-group comparisons of continuous variables were performed by independent samples t-test. Otherwise, Mann–Whitney-U or Kruksal–Wallis test was used. Within-group comparisons were performed by paired samples t-test and Wilcoxon signed-rank test was applied to the post-ante differences. For correlation analysis, Spearman’s coefficient was calculated. Unless indicated otherwise, results are reported as median and interquartile range.
Statement of Financial Support
No financial assistance was received to support this study.
Disclosure
The authors declare no conflict of interest.
References
Hecher K, Snijders R, Campbell S, Nicolaides K . Fetal venous, arterial, and intracardiac blood flows in red blood cell isoimmunization. Obstet Gynecol 1995;85:122–8.
Baschat AA, Muench MV, Gembruch U . Coronary artery blood flow velocities in various fetal conditions. Ultrasound Obstet Gynecol 2003;21:426–9.
Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 2005;112:e154–235.
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388–442.
McGrath MF, de Bold AJ . Determinants of natriuretic peptide gene expression. Peptides 2005;26:933–43.
Potter LR, Yoder AR, Flora DR, Antos LK, Dickey DM . Natriuretic peptides: their structures, receptors, physiologic functions and therapeutic applications. Handb Exp Pharmacol 2009;191:341–66.
Cameron VA, Ellmers LJ . Minireview: natriuretic peptides during development of the fetal heart and circulation. Endocrinology 2003;144:2191–4.
Merz WM, Kübler K, Albers E, Stoffel-Wagner B, Gembruch U . Reference values for N-terminal pro-B-type natriuretic peptide in fetal circulation between 20 and 34 weeks of gestation. Clin Biochem 2010;43:519–21.
Fortunato G, Carandente Giarrusso P, Martinelli P, et al. Cardiac troponin T and amino-terminal pro-natriuretic peptide concentrations in fetuses in the second trimester and in healthy neonates. Clin Chem Lab Med 2006;44:834–6.
Ordonez-Llanos J, Collinson PO, Christenson RH . Amino-terminal pro-B-type natriuretic peptide: analytic considerations. Am J Cardiol 2008;101(3A):9–15.
Clerico A, Emdin M . Diagnostic accuracy and prognostic relevance of the measurement of cardiac natriuretic peptides: a review. Clin Chem 2004;50:33–50.
Ala-Kopsala M, Magga J, Peuhkurinen K, et al. Molecular heterogeneity has a major impact on the measurement of circulating N-terminal fragments of A- and B-type natriuretic peptides. Clin Chem 2004;50:1576–88.
Luckenbill KN, Christenson RH, Jaffe AS, et al. Cross-reactivity of BNP, NT-proBNP, and proBNP in commercial BNP and NT-proBNP assays: preliminary observations from the IFCC Committee for Standardization of Markers of Cardiac Damage. Clin Chem 2008;54:619–21.
Liang F, O’Rear J, Schellenberger U, et al. Evidence for functional heterogeneity of circulating B-type natriuretic peptide. J Am Coll Cardiol 2007;49:1071–8.
Xu-Cai YO, Wu Q . Molecular forms of natriuretic peptides in heart failure and their implications. Heart 2010;96:419–24.
Baschat AA, Gembruch U, Harman CR . The sequence of changes in Doppler and biophysical parameters as severe fetal growth restriction worsens. Ultrasound Obstet Gynecol 2001;18:571–7.
Girsen A, Ala-Kopsala M, Mäkikallio K, Vuolteenaho O, Räsänen J . Cardiovascular hemodynamics and umbilical artery N-terminal peptide of proB-type natriuretic peptide in human fetuses with growth restriction. Ultrasound Obstet Gynecol 2007;29:296–303.
Crispi F, Hernandez-Andrade E, Pelsers MM, et al. Cardiac dysfunction and cell damage across clinical stages of severity in growth-restricted fetuses. Am J Obstet Gynecol 2008;199:254.e1–8.
Kocylowski RD, Dubiel M, Gudmundsson S, et al. Biochemical tissue-specific injury markers of the heart and brain in postpartum cord blood. Am J Obstet Gynecol 2009;200:273.e1–25.
Lechner E, Wiesinger-Eidenberger G, Wagner O, et al. Amino terminal pro B-type natriuretic peptide levels are elevated in the cord blood of neonates with congenital heart defect. Pediatr Res 2009;66:466–9.
Merz WM, Kübler K, Albers E, Stoffel-Wagner B, Gembruch U . N-terminal pro-B-type natriuretic peptide in the circulation of fetuses with cardiac malformations. Clin Res Cardiol 2012;101:73–9.
Pasman SA, van den Brink CP, Kamping MA, Adama van Scheltema PN, Oepkes D, Vandenbussche FP . Total blood volume is maintained in nonhydropic fetuses with severe hemolytic anemia. Fetal Diagn Ther 2009;26:10–5.
Tongsong T, Tongprasert F, Srisupundit K, Luewan S . Venous Doppler studies in low-output and high-output hydrops fetalis. Am J Obstet Gynecol 2010;203:488.e1–6.
Lamont RF, Sobel JD, Vaisbuch E, et al. Parvovirus B19 infection in human pregnancy. BJOG 2011;118:175–86.
Jonker SS, Giraud MK, Giraud GD, et al. Cardiomyocyte enlargement, proliferation and maturation during chronic fetal anaemia in sheep. Exp Physiol 2009;95:131–9.
Mascio CE, Olison AK, Ralphe JC, Tomanek RJ, Scholz TD, Segar JL . Myocardial vascular and metabolic adaptations in chronically anemic fetal sheep. Am J Physiol Regul Integr Comp Physiol 2005;289:R1736–45.
Broberg CS, Giraud GD, Schultz JM, Thornburg KL, Hohimer AR, Davis LE . Fetal anemia leads to augmented contractile response to hypoxic stress in adulthood. Am J Physiol Regul Integr Comp Physiol 2003;285:R649–55.
Davis L, Thornburg KL, Giraud GD . The effects of anaemia as a programming agent in the fetal heart. J Physiol (Lond) 2005;565(Pt 1):35–41.
Van Mieghem T, DeKoninck P, Steenhaut P, Deprest J . Methods for prenatal assessment of fetal cardiac function. Prenat Diagn 2009;29:1193–203.
Mari G, Deter RL, Carpenter RL, et al. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative Group for Doppler Assessment of the Blood Velocity in Anemic Fetuses. N Engl J Med 2000;342:9–14.
Moise KJ . The usefulness of middle cerebral artery Doppler assessment in the treatment of the fetus at risk for anemia. Am J Obstet Gynecol 2008;198:161.e1–e4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merz, W., Kübler, K., Fimmers, R. et al. Circulating N-terminal pro-B-type natriuretic peptide in fetal anemia before and after treatment. Pediatr Res 72, 174–178 (2012). https://doi.org/10.1038/pr.2012.53
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.53
This article is cited by
-
Fetal NT-proBNP levels and their course in severe anemia during intrauterine treatment
Archives of Gynecology and Obstetrics (2023)
-
NT-proBNP: A Useful Biochemical Marker for Prognosis in Rh-Isoimmunized Pregnancies
The Journal of Obstetrics and Gynecology of India (2019)