Abstract
Background:
Proadrenomedullin (pro-ADM) for the diagnosis of proven and clinical sepsis in a newborn cohort including preterm newborns has not been investigated. We aimed to investigate the value of pro-ADM as a new marker by comparing it with conventional markers in neonatal sepsis (NS).
Methods:
Participants were stratified into three groups; proven sepsis (Group 1a), clinical sepsis (Group 1b), and the control group (Group 2), which consisted of newborns of matched gestational age and birth weight. Sequential measurements of white blood cell count, C-reactive protein (CRP), interleukin-6 (IL-6), and pro-ADM were compared.
Results:
A total of 76 patients with NS (31 with proven sepsis and 45 with clinical sepsis) and 52 healthy controls were enrolled. Mean baseline serum levels of CRP, IL-6, and pro-ADM were significantly higher in both Group 1a and Group 1b as compared with healthy controls (P < 0.001 for both). Although mean baseline CRP and IL-6 levels were similar between groups, mean baseline pro-ADM level was higher in the proven sepsis group than in the clinical sepsis group (P < 0.001).
Conclusion:
The use of pro-ADM in combination with other acute-phase reactants such as CRP and IL-6 for the diagnosis and follow-up of patients with NS has high sensitivity and specificity.
Similar content being viewed by others
Main
Neonatal sepsis (NS) is a potentially life-threatening clinical condition that requires early intervention. NS is associated with high morbidity and mortality rates if not treated promptly. Although ideally antibiotic therapy should be directed against the causative agent, results of cultures take around 48–72 h to be processed, and any delay in the initiation of treatment for sepsis may be catastrophic (1,2). Several acute-phase reactants such as C-reactive protein (CRP) and interleukin-6 (IL-6) have proven helpful in the diagnosis of an ongoing infection. However, the rate at which each marker begins to show elevations and the time to normalization differs with each marker (3,4,5,6,7).
Human adrenomedullin (ADM) is an immunomodulator with various described metabolic and vascular modulatory effects, and elevations in tissue levels of the peptide have been reported to occur as a response to disrupted blood circulation. It plays an important role in regulating blood volume; it also has potential antimicrobial effects, which have a protective effect against organ damage, particularly in the setting of sepsis (8,9,10). Its serum levels show rapid elevations during sepsis, followed by rapid clearance from the circulation, which makes it difficult to detect because of its half-life of 22 min. Pro-ADM (pro-ADM), a more stable precursor molecule to ADM, was reported to correlate well with other markers such as IL-6 and CRP as a predictor of prognosis in patients with sepsis (10). Elevations of pro-ADM have been reported in systemic inflammatory response syndrome (SIRS), sepsis, and septic shock in adults (11,12).
The aim of this study was to investigate the presence of any correlation between pro-ADM and IL-6 and CRP in NS, as well as to evaluate the value of pro-ADM measurement in the follow-up of this disorder. To the best of our knowledge, this is the first clinical study in which pro-ADM was evaluated for its potential role as a marker in NS of both preterm and term newborns.
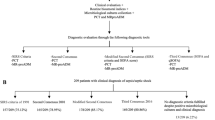
Results
A total of 80 newborns fulfilling the criteria for a diagnosis of sepsis were enrolled in the study, four of whom died before conclusion of all study proceedings. Of the remaining 76 patients, 31 had proven sepsis (Group 1a) and 45 had clinical sepsis (Group 1b). The control group (Group 2) consisted of 52 healthy controls. The demographic characteristics of the study population are summarized in Table 1 . The differences between patients with sepsis (Group 1) and healthy controls (Group 2) with regard to each of maternal age, gestational age, birth weight, gender, and mode of delivery were statistically insignificant. However, none of the healthy controls were born to mothers with premature rupture of membranes (PROM), but 13 (17.1%) of the newborns who developed sepsis were born following PROM.
A comparison of markers of sepsis obtained at baseline revealed white blood cell (WBC), CRP, IL-6, and pro-ADM levels to be significantly higher in newborns with sepsis as compared with healthy controls (P < 0.05, P < 0.001, P < 0.001, and P < 0.001, respectively). When patients were divided into two groups based on gestational age, no statistically significant difference in terms of baseline WBCs, CRP, IL-6, or pro-ADM were observed between preterm newborns (<37 gestational wk; n = 47) and term newborns (≥37 gestational wk; n = 29).
A comparison of patients with sepsis on the basis of the age of diagnosis revealed newborns with late-onset NS (LOS; n = 30) to have been born at significantly lesser gestational ages (29.9 ± 4.2 vs. 35.2 ± 4.8 wk) with lower birth weights (1,371 ± 728 vs. 2,437 ± 1,052 g) than patients with early-onset NS (EOS) (n = 46) (P < 0.001 for both). Furthermore, significantly more subjects in the LOS group had proven sepsis as compared with the EOS group (P < 0.001). Mean baseline serum levels of CRP and pro-ADM were higher in patients with LOS than in patients with EOS (P = 0.012 and P = 0.047, respectively). After 48 and 120 h, statistically significant elevations of CRP levels only were observed in the LOS group as compared with patients with EOS (P = 0.026). The observed trend for CRP levels was to remain elevated for longer time period and to return to normal later in patients with LOS than those with EOS.
Subgroup comparisons revealed patients with clinical sepsis to have significantly higher baseline WBC levels than healthy controls (P = 0.015). Similarly, mean baseline serum levels of CRP, IL-6, and pro-ADM were significantly higher in both Group 1a and Group 1b as compared with healthy controls (P < 0.001 for all). Comparisons between patients with proven and clinical sepsis revealed a statistical significance only with regard to mean baseline pro-ADM level, which was higher in the proven sepsis group (P < 0.001). Pro-ADM was found to be positively correlated, albeit weakly, with CRP (r = 0.468; P = 0.01) and IL-6 (r = 0.386; P = 0.01). Results of subgroup analysis have been summarized in Table 2 .
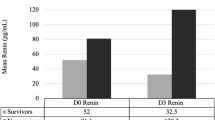
The microorganisms that were isolated from the blood cultures of patients with sepsis were Staphylococcus epidermidis in 14 cases (45.1%), Escherichia coli in six cases (19.3%), Klebsiella pneumonia in six cases (19.3%), and Acinetobacter baumannii in two cases (6.5%). Growths of Klebsiella oxytoca, Pseudomonas aeruginosa, and Serratia marcescens were observed in one case each (3.25%). Overall, Gram-positive bacteria were isolated in 14 (45%) patients with proven sepsis as compared with a Gram-negative growth in 17 (55%) patients. Baseline serum levels of IL-6 and pro-ADM were significantly higher in newborns with confirmed Gram-negative sepsis as compared with those infected with Gram-positive bacteria (P = 0.013 and P = 0.003, respectively). Changes in serum levels of CRP, IL-6, and pro-ADM from baseline are depicted in Figure 1 , which shows a relatively slower decline in CRP levels as compared with the other markers.
Receiver operating characteristic (ROC) analysis was used to determine the power of variables to differentiate groups, and the area under the curve (AUC) was calculated. The optimal cutoff values for WBCs, CRP, IL-6, and pro-ADM were identified by plotting ROC curves. ROC curves of all patients with sepsis vs. healthy controls are depicted in Figure 2 . The AUC, specificity, sensitivity, positive predictive value (PPV), negative predictive value, and cutoff levels are listed in Table 3 . The calculated cutoff values for CRP, IL-6, and pro-ADM in distinguishing patients with sepsis group were 4.87 mg/l, 26 pg/ml, and 3.9 nmol/l, respectively, with specificities and PPVs of 100% for all three markers. Respective sensitivities of these cutoff values were 84.2%, 84.2%, and 86.8%; negative predictive values were 81.2%, 81.2%, and 83.9%, respectively. AUC analysis for comparing patients with proven sepsis and healthy controls once again revealed the set cutoff values for CRP, IL-6, and pro-ADM to have specificities and PPVs of 100%, with respective sensitivities of 96.7%, 93.5%, and 93.5%; negative predictive values for the three markers were 98.1%, 96.2%, and 96.2%, respectively.
Discussion
The goal of this study was to investigate the value of pro-ADM measurements for making a diagnosis of NS by comparing it with CRP and IL-6. An ideal marker would need to have a sensitivity of 100% with negative predictive values and PPVs of >85%, to avoid unnecessary use of antibiotics (13,14,15). With this study, we managed to demonstrate a specificity and PPV of 100% for pro-ADM, similar to the other acute-phase reactants. The sensitivity and negative predictive value of pro-ADM were 86.8% and 83.9%, respectively, values that were higher than those obtained for the other markers.
ADM has bactericidal activity, which is further enhanced by its regulation and modulation of complement activity (9,16). Not surprisingly, serum levels of ADM were shown to be increased in sepsis (17). There are two primary mechanisms that might be responsible for the marked increase in circulating ADM in sepsis. First, ADM is widely expressed and extensively synthesized during sepsis, similar to other calcitonin peptides including procalcitonin and calcitonin-gene related peptides, because ADM is a member of the CALC gene family (18). In a second potential mechanism, decreased clearance by the kidneys may be responsible in part for increased levels in sepsis (17). Pro-ADM is the stable active substance and has a longer half-life than ADM. Therefore, in this study we chose pro-ADM for evaluation of NS.
In a study on 53 adult patients with sepsis and 48 patients with SIRS, pro-ADM levels of the sepsis group were found to be higher than those in the SIRS and control group (P < 0.001). These patients with sepsis, severe sepsis, and septic shock demonstrated progressively higher pro-ADM levels (19). In a similar study in adults (20), progressively higher levels of pro-ADM were observed in patients with SIRS, sepsis, severe sepsis, and septic shock (P < 0.05). Reported AUC values for pro-ADM in both these studies after ROC curve analysis were 0.81 and 0.87, respectively. We, on the other hand, reported on a value of 0.97. However, unlike the former studies, we did not distinguish between patients with SIRS, sepsis, sever sepsis, and septic shock. However, considering that the endothelial damage is more extensive, pro-ADM would be expected to be higher in such patients. Instead, we performed comparisons between patients with clinical and proven sepsis and between patients with EOS and LOS, with statistically significant elevations in pro-ADM levels of subjects with positive culture results.
In a clinical study involving 40 full-term newborns, pro-ADM levels were significantly higher in the severe sepsis group as compared with the mild sepsis group (P < 0.05). The limitations of this study were the smaller sample size, the fact that only full-term newborns were enrolled, the lack of sequential measurements of pro-ADM, and non-disclosure of blood culture results (21). In our study, we enrolled 76 patients with sepsis, 61.8% of whom were born at <37 wk of gestation. Subgroup analysis revealed significantly higher levels of pro-ADM as compared with those of healthy controls in patients with either proven or clinical sepsis (P < 0.001 for both). Furthermore, patients with proven sepsis also had significantly higher levels of pro-ADM as compared with those with clinical sepsis (P < 0.001).
In a study by Miguel et al. (22) in which cord blood pro-ADM levels of newborns born after high-risk pregnancies/deliveries were compared with healthy controls, a statistically significant difference was not observed. The high-risk group consisted of neonates who experienced severe asphyxia or were born to mothers who were carriers for group B streptococcus or who experienced PROM, intrapartum maternal fever, or chorioamnionitis. In our study, a comparison of pro-ADM levels of the 13 newborns (17.1%) delivered after PROM with those without PROM did not reveal a statistically significant difference. None of the other aforementioned risk factors were encountered in our study population. A recent study that investigated the perinatal factors affecting midregional-proADM (MR-proADM) plasma concentrations in newborns demonstrated that MR-proADM concentrations were elevated especially in those born very preterm. The authors concluded that immaturity and infection, which both feature low systemic vascular resistance, were related to increase in MR-proADM concentrations (23).
Our study has some limitations. First, we enrolled both term and preterm newborns in the study population. This limitation did not affect the results but reveals the lack of homogeneity. Second, there was no statistically significant difference between patients with or without PROM in the sepsis group, and this might affect biochemical results. Further studies are needed to evaluate only preterm newborns without maternal infectious factors. Third, patients with clinical sepsis had significantly higher levels of WBCs than controls, but patients with culture-proven sepsis did not; as this does not seem logical given the rest of the data. However, this may be result of more patients with leukopenia in the proven sepsis group.
Conclusion
Pro-ADM is a novel marker that may be used especially for early diagnosis of NS. The fact that pro-ADM levels showed more rapid decreases as compared with CRP in our study suggests that rather than being used alone, use of pro-ADM in combination with conventional acute-phase reactants may be more useful in diagnosis and follow-up of patients with NS.
Methods
Patient Selection
The study was conducted in the neonatal intensive care unit of Zekai Tahir Burak Maternity Teaching Hospital, Ankara, Turkey, between May and September 2011. This unit has 150 incubators and serves as a referral Level III neonatal intensive care unit with about 4,000 newborn admissions per year. This trial was approved by Zekai Tahir Burak Maternity Teaching Hospital Ethics Committee, and newborns were enrolled in the study after written parental consent.
Suggested diagnostic criteria for sepsis in neonates (two or more of the following clinical features) were used to identify patients for sepsis evaluations (24): (i) respiratory compromise includes the following: tachypnea, increased apnea, severe apnea, increased ventilatory support, or desaturation; (ii) cardiovascular compromise, including bradycardia, pallor, decreased perfusion, or hypotension; (iii) metabolic changes including hypothermia, hyperthermia, feeding intolerance, glucose instability, or metabolic acidosis; or (iv) neurologic changes consists of lethargy, hypotonia, or decreased activity (25), in addition to laboratory results showing elevated levels of CRP or IL-6. Patients with culture positivity were accepted as proven sepsis (24). Patients with findings supporting the presence of heart failure, maternal preeclampsia, or severe intracranial bleeding (III–IV), in all of which conditions elevations in plasma ADM have been reported (12,17,26,27,28), were excluded from the study.
Patients with sepsis (Group 1) were further divided into two subgroups based on whether they had proven (Group 1a: newborns with positive blood cultures, clinical findings in agreement with the diagnosis, and elevated IL-6 and/or CRP levels during the clinical course) or clinical (Group 1b: newborns with clinical findings of infection plus a significant rise in IL-6 and/or CRP levels during the clinical course, but with negative blood cultures) sepsis. The control group (Group 2) consisted of healthy newborns who were admitted to neonatal intensive care unit for other than sepsis.
Patients were further subdivided into two groups based on the time of development of sepsis; patients diagnosed within the first 72 h of life were considered to have EOS, whereas the development of sepsis in newborns older than 72 h was described as LOS.
Laboratory Analyses
The day the a clinical diagnosis of sepsis was made was considered day 1, and venous blood sampling was performed within the first 6 h after first presentation. Blood sampling was repeated after 48 and 120 h after first presentation. From each sample obtained, determination of WBC count and CRP and IL-6 levels was performed immediately, with the remaining supernatant stored at −70 °C pending collective determination of pro-ADM levels at the end of the study period.
Complete blood counts were obtained using a twice-daily calibrated Cell-Dyn 3700 automated hemocytometer (Abbott, Abbott Park, IL). Serum concentrations of CRP were measured by a Tina-quant CRP (Latex; Roche Diagnostics, Mannheim, Germany) high sensitivity immune turbidimetric assay on a Roche Modular P analyzer (Roche kit, Roche Diagnostics, Mannheim, Germany) according to manufacturer instructions. Normal range of CRP was 0–5 mg/l. Plasma levels of IL-6 were determined by IL-6 solid phase, enzyme labeled, chemiluminescent sequential immunometric assay on an IMMULITE 2000 analyzer, (Siemens Diagnostic Product Corporation, Los Angeles, CA) per manufacturer instructions. IL-6 levels >25 pg/ml were regarded as abnormal (13).
Pro-ADM Assay
Pro-ADM levels were measured using a commercial human pro-ADM radioimmunoassay kit (Cusabio Biotech, Wilmington, DE). Standards or samples were then added to the appropriate microtiter plate wells with a biotin-conjugated antibody preparation specific for pro-ADM and Avidin (Innova Biosciences, Cambridge, UK) conjugated to horseradish peroxidase was added to each microplate well and incubated. This was followed by addition of a 3,3′,5,5′ tetramethyl-benzidine substrate solution to each well. Only wells that contained pro-ADM, biotin-conjugated antibody, and enzyme-conjugated Avidin exhibited a change in color. The enzyme–substrate reaction was terminated by the addition of a sulfuric acid solution and the color change was measured spectrophotometrically at a wavelength of 450 nm ± 2 nm. Values of pro-ADM were provided as nmol/l.
Blood Culture
Blood cultures were performed on newborns when NS was suspected. Blood culture was not taken from healthy controls. The Bactec microbial detection system (Becton-Dickinson, Sparks, MD) was used to detect positive blood cultures. Two positive blood culture tests were required to confirm S. epidermidis sepsis.
Statistical Analyses
Statistical analyses were performed using the SPSS for Windows (version 15.0) statistical package. χ2 test was used to compare categorical variables between groups. The Kolmogorov–Smirnov test was used to evaluate the normal distribution assumption for numerical variables. Difference between two groups was examined by independent samples t-test for normally distributed variables and Mann Whitney U test for nonnormally distributed variables. Difference among more than two groups was examined by ANOVA and Kruskal–Wallis test for normally and nonnormally distributed variables, respectively. Discriminatory performance of variables was determined by area under the ROC curve and best cutoff values were calculated using the Youden index. Spearman correlation coefficient was used to examine the relationship between numerical variables. A P value of <0.05 was considered indicative of statistical significance.
References
Osrin D, Vergnano S, Costello A . Serious bacterial infections in newborn infants in developing countries. Curr Opin Infect Dis 2004;17:217–24.
Gerdes JS . Diagnosis and management of bacterial infections in the neonate. Pediatr Clin North Am 2004;51:939–59, viii–ix.
Khassawneh M, Hayajneh WA, Kofahi H, Khader Y, Amarin Z, Daoud A . Diagnostic markers for neonatal sepsis: comparing C-reactive protein, interleukin-6 and immunoglobulin M. Scand J Immunol 2007;65:171–5.
Kao PC, Shiesh SC, Wu TJ . Serum C-reactive protein as a marker for wellness assessment. Ann Clin Lab Sci 2006;36:163–9.
Buck C, Bundschu J, Gallati H, Bartmann P, Pohlandt F . Interleukin-6: a sensitive parameter for the early diagnosis of neonatal bacterial infection. Pediatrics 1994;93:54–8.
Pourcyrous M, Bada HS, Korones SB, Baselski V, Wong SP . Significance of serial C-reactive protein responses in neonatal infection and other disorders. Pediatrics 1993;92:431–5.
Onal EE, Kitapçi F, Dilmen U, Adam B . Interleukin-6 concentrations in neonatal sepsis. Lancet 1999;353:239–40.
Hinson JP, Kapas S, Smith DM . Adrenomedullin, a multifunctional regulatory peptide. Endocr Rev 2000;21:138–67.
Pio R, Martinez A, Unsworth EJ, et al. Complement factor H is a serum-binding protein for adrenomedullin, and the resulting complex modulates the bioactivities of both partners. J Biol Chem 2001;276:12292–300.
Ehlenz K, Koch B, Preuss P, Simon B, Koop I, Lang RE . High levels of circulating adrenomedullin in severe illness: correlation with C-reactive protein and evidence against the adrenal medulla as site of origin. Exp Clin Endocrinol Diabetes 1997;105:156–62.
Ueda S, Nishio K, Minamino N, et al. Increased plasma levels of adrenomedullin in patients with systemic inflammatory response syndrome. Am J Respir Crit Care Med 1999;160:132–6.
Eto T . A review of the biological properties and clinical implications of adrenomedullin and proadrenomedullin N-terminal 20 peptide (PAMP), hypotensive and vasodilating peptides. Peptides 2001;22:1693–711.
Celik IH, Demirel FG, Uras N, et al. What are the cut-off levels for IL-6 and CRP in neonatal sepsis? J Clin Lab Anal 2010;24:407–12.
Ng PC, Li K, Wong RP, Chui KM, Wong E, Fok TF . Neutrophil CD64 expression: a sensitive diagnostic marker for late-onset nosocomial infection in very low birthweight infants. Pediatr Res 2002;51:296–303.
Erdeve O, Celik IH, Uras N, Demirel FG, Oguz SS, Dilmen U . CRP as a predictive of neonatal sepsis and its role in differentiating the aetiologies. Acta Paediatr 2011;100:160–1.
Marutsuka K, Nawa Y, Asada Y, et al. Adrenomedullin and proadrenomudullin N-terminal 20 peptide (PAMP) are present in human colonic epithelia and exert an antimicrobial effect. Exp Physiol 2001;86:543–5.
Hirata Y, Mitaka C, Sato K, et al. Increased circulating adrenomedullin, a novel vasodilatory peptide, in sepsis. J Clin Endocrinol Metab 1996;81:1449–53.
Becker KL, Nylén ES, White JC, Müller B, Snider RH Jr . Clinical review 167: Procalcitonin and the calcitonin gene family of peptides in inflammation, infection, and sepsis: a journey from calcitonin back to its precursors. J Clin Endocrinol Metab 2004;89:1512–25.
Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Müller B . Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care 2005;9:R816–24.
Kang FX, Wang RL, Yu KL, Wei Q . (The study on pro-adrenomedullin as a new biomarker in sepsis prognosis and risk stratification). Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2008;20:452–5.
Hagag AA, Elmahdy HS, Ezzat AA . Prognostic value of plasma pro-adrenomedullin and antithrombin levels in neonatal sepsis. Indian Pediatr 2011;48:471–3.
Miguel D, Prieto B, Costa M, Coto D, Alvarez FV . Cord blood plasma reference intervals for potential sepsis markers: pro-adrenomedullin, pro-endothelin, and pro-atrial natriuretic peptide. Clin Biochem 2011;44:337–41.
Admaty D, Benzing J, Burkhardt T, et al. Plasma midregional proadrenomedullin in newborn infants: impact of prematurity and perinatal infection. Pediatr Res 2012;72:70–6.
Haque KN . Definitions of bloodstream infection in the newborn. Pediatr Crit Care Med 2005;6:Suppl 3:S45–9.
Gonzalez BE, Mercado CK, Johnson L, Brodsky NL, Bhandari V . Early markers of late-onset sepsis in premature neonates: clinical, hematological and cytokine profile. J Perinat Med 2003;31:60–8.
Senna AA, Zedan M, el-Salam GE, el-Mashad AI . Study of plasma adrenomedullin level in normal pregnancy and preclampsia. Medscape J Med 2008;10:29.
Klip IT, Voors AA, Anker SD, et al. Prognostic value of mid-regional pro-adrenomedullin in patients with heart failure after an acute myocardial infarction. Heart 2011;97:892–8.
Gazzolo D, Marinoni E, Giovannini L, Letizia C, Serra G, Di Iorio R . Circulating adrenomedullin is increased in preterm newborns developing intraventricular hemorrhage. Pediatr Res 2001;50:544–7.
Acknowledgements
We are grateful to Erdem Karabulut in the Department of Biostatistics, Hacettepe University, for his help in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oncel, M., Dilmen, U., Erdeve, O. et al. Proadrenomedullin as a prognostic marker in neonatal sepsis. Pediatr Res 72, 507–512 (2012). https://doi.org/10.1038/pr.2012.106
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.106
This article is cited by
-
Mid-Regional Proadrenomedullin Levels in Primary Immunodeficiencies Complicated with Pulmonary Manifestations
Indian Journal of Clinical Biochemistry (2023)
-
Diagnostic value of mid-regional pro-Adrenomedullin as a biomarker of invasive bacterial infection in children: a systematic review
BMC Pediatrics (2022)
-
Diagnosis of neonatal sepsis: the past, present and future
Pediatric Research (2022)
-
Proadrenomedullin and neonatal sepsis: a systematic review and meta-analysis of diagnostic accuracy
European Journal of Pediatrics (2022)
-
Mid-regional pro-adrenomedullin for diagnosing evolution after cardiac surgery in newborns: the PRONEW study
European Journal of Pediatrics (2022)