Abstract
Objective
No single test can accurately identify neonatal late-onset sepsis (LOS). Our aim was to use clinical evaluation with laboratory tests to rapidly assess sepsis risk.
Study design
A retrospective case-control study was performed in a tertiary Neonatal Center during the years 2016–2019. Infants with bacteriologically confirmed LOS were compared with control infants. A clinical health evaluation score was assigned to each infant. A prediction model was developed and validated by multivariable analysis.
Results
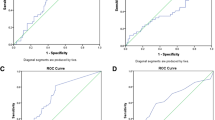
The study included 145 infants, 48 with sepsis, and 97 controls. LOS was independently associated with: sick appearance (OR: 5.7, 95% CI: 1.1–29.1), C-reactive protein > 0.75 (OR: 5.4, 95% CI: 1.1–26.3), and neutrophil-to-lymphocyte ratio > 1.5 (OR: 6.7, 95% CI: 1.2–38.5). Our model had an area under the receiver operating characteristic curve of 0.92 (95% CI: 0.86–0.97).
Conclusions
Clinical evaluation with neutrophil-to-lymphocyte ratio and C-reactive protein can rapidly identify LOS enabling decreased health costs and antibiotic use.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–80.
Dong Y, Speer CP. Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed. 2015;100:F257–63.
Qazi SA, Stoll BJ. Neonatal sepsis: a major global public health challenge. Pediatr Infect Dis J. 2009;28:S1–2.
Dillenseger L, Langlet C, Iacobelli S, Lavaux T, Ratomponirina C, Labenne M, et al. Early inflammatory markers for the diagnosis of late-onset sepsis in neonates: The Nosodiag Study. Front Pediatr. 2018;6:346.
Hornik CP, Benjamin DK, Becker KC, Benjamin DK Jr, Li J, Clark RH, et al. Use of the complete blood cell count in late-onset neonatal sepsis. Pediatr Infect Dis J. 2012;31:803–7.
Sharma D, Farahbakhsh N. Biomarkers for diagnosis of neonatal sepsis: a literature review. J Matern Fetal Neonatal Med. 2018;31:1646–59.
Verstraete EH, Blot K, Mahieu L, Vogelaers D, Blot S. Prediction models for neonatal health care-associated sepsis: a meta-analysis. Pediatrics. 2015;135:e1002–14.
Gasparrini AJ, Wang B, Sun X, Kennedy EA, Hernandez-Leyva A, Ndao IM, et al. Persistent metagenomic signatures of early-life hospitalization and antibiotic treatment in the infant gut microbiota and resistome. Nat Microbiol. 2019;4:2285–2297.
Brown JVE, Meader N, Cleminson J, McGuire W. C-reactive protein for diagnosing late-onset infection in newborn infants. Cochrane Database Syst Rev. 2019;1:CD012126. https://doi.org/10.1002/14651858.CD012126.pub2.
Rosenfeld CR, Shafer G, Scheid LM, Brown LS. Screening and serial neutrophil counts do not contribute to the recognition or diagnosis of late-onset neonatal sepsis. J Pediatr. 2019;205:105–11.e2.
Ng S, Strunk T, Jiang P, Muk T, Sangild PT, Currie A. Precision medicine for neonatal sepsis. Front Mol Biosci. 2018;5:70.
Nuntnarumit P, Yang W, Bada-Ellzey HS. Blood pressure measurements in the newborn. Clin Perinatol. 1999;26:981–96.
Klinger G, Chin CN, Beyene J, Perlman M. Predicting the outcome of neonatal bacterial meningitis. Pediatrics. 2000;106:477–82.
Walker SAN, Cormier M, Elligsen M, Choudhury J, Rolnitsky A, Findlater C, et al. Development, evaluation and validation of a screening tool for late onset bacteremia in neonates—a pilot study. BMC Pediatr. 2019;19:253.
Alkan Ozdemir S, Arun Ozer E, Ilhan O, Sutcuoglu S. Can neutrophil to lymphocyte ratio predict late-onset sepsis in preterm infants? J Clin Lab Anal. 2018;32:e22338.
Christensen RD, Baer VL, Gordon PV, Henry E, Whitaker C, Andres RI, et al. Reference ranges for lymphocyte counts of neonates: associations between abnormal counts and outcomes. Pediatrics. 2012;129:e1165–72.
Moons KGM, Altman DG, Reitsma JB, Ioannidis JPA, Macaskill P, Steyerberg EW, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162:W1–73.
Eschborn S, Weitkamp JH. Procalcitonin versus C-reactive protein: review of kinetics and performance for diagnosis of neonatal sepsis. J Perinatol. 2019;39:893–903.
Makkar M, Gupta C, Pathak R, Garg S, Mahajan NC. Performance evaluation of hematologic scoring system in early diagnosis of neonatal sepsis. J Clin Neonatol. 2013;2:25–9.
Aydemir C, Aydemir H, Kokturk F, Kulah C, Mungan AG. The cut-off levels of procalcitonin and C-reactive protein and the kinetics of mean platelet volume in preterm neonates with sepsis. BMC Pediatr. 2018;18:253.
Beltempo M, Viel-Thériault I, Thibeault R, Julien AS, Piedboeuf B. C-reactive protein for late-onset sepsis diagnosis in very low birth weight infants. BMC Pediatr. 2018;18:16.
Turner D, Hammerman C, Rudensky B, Schlesinger Y, Schimmel MS. The role of procalcitonin as a predictor of nosocomial sepsis in preterm infants. Acta Paediatr. 2006;95:1571–6.
Omran A, Maaroof A, Saleh MH, Abdelwahab A. Salivary C-reactive protein, mean platelet volume and neutrophil lymphocyte ratio as diagnostic markers for neonatal sepsis. J Pediatr. 2018;94:82–7.
Delano MJ, Ward PA. Sepsis-induced immune dysfunction: can immune therapies reduce mortality? J Clin Invest. 2016;126:23–31.
Escobar GJ, Puopolo KM, Wi S, Turk BJ, Kuzniewicz MW, Walsh EM, et al. Stratification of risk of early-onset sepsis in newborns ≥34 weeks’ gestation. Pediatrics. 2014;133:30–6.
Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr. 2017;171:365–71.
Sullivan BA, Fairchild KD. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin Fetal Neonatal Med. 2015;20:255–61.
Author information
Authors and Affiliations
Contributions
OG: leading role in study design, data acquisition, analysis and interpretation, writing and revision of paper, approved the submitted paper. NA: leading role in study conception and design. Contributed to data acquisition and revision of paper, approved the submitted paper. GC: study conception and design, data analysis and interpretation, revision of paper, approved the submitted paper. RB: study conception and design, data acquisition and interpretation, critical revision of paper, approved the submitted paper. OS: study conception and design, data interpretation, critical revision of paper, approved the submitted paper. HBZ: study conception and design, data acquisition, approved the submitted paper. GK: leading role in all study aspects including: conception and design of study, data acquisition, analysis and interpretation, writing of paper, final approval of the submitted paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Goldberg, O., Amitai, N., Chodick, G. et al. Can we improve early identification of neonatal late-onset sepsis? A validated prediction model. J Perinatol 40, 1315–1322 (2020). https://doi.org/10.1038/s41372-020-0649-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0649-6
This article is cited by
-
Comparison of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for the diagnosis of neonatal sepsis: a systematic review and meta-analysis
BMC Pediatrics (2023)
-
Meta-analysis of the role of neutrophil to lymphocyte ratio in neonatal sepsis
BMC Infectious Diseases (2023)
-
Artificial and human intelligence for early identification of neonatal sepsis
Pediatric Research (2023)
-
Prediction modelling in the early detection of neonatal sepsis
World Journal of Pediatrics (2022)