Abstract
The tyrosine kinase inhibitor (TKI) imatinib has transformed the treatment and outlook of chronic myeloid leukemia (CML); however, the development of drug resistance and the persistence of TKI-resistant stem cells remain obstacles to eradicating the disease. Inhibition of proteasome activity with bortezomib has been shown to effectively induce apoptosis in TKI-resistant cells. In this study, we show that exposure to the next generation proteasome inhibitor carfilzomib is associated with a decrease in ERK signaling and increased expression of Abelson interactor proteins 1 and 2 (ABI-1/2). We also investigate the effect of carfilzomib in models of imatinib-sensitive and -resistant CML and demonstrate a potent reduction in proliferation and induction of apoptosis in a variety of models of imatinib-resistant CML, including primitive CML stem cells. Carfilzomib acts synergistically with the TKIs imatinib and nilotinib, even in imatinib-resistant cell lines. In addition, we found that the presence of immunoproteasome subunits is associated with an increased sensitivity to carfilzomib. The present findings provide a rational basis to examine the potential of carfilzomib in combination with TKIs as a potential therapy for CML, particularly in imatinib-resistant disease.
Similar content being viewed by others
Introduction
Chronic myeloid leukemia (CML) is a myeloproliferative neoplasm that arises in a hematopoietic stem cell. It is characterized by a reciprocal translocation between the long arms of chromosomes 9 and 22. The resulting fusion gene BCR-ABL, encodes a constitutively active protein tyrosine kinase Bcr-Abl, which is responsible for the pathogenesis of CML. Current first-line therapy for CML is imatinib mesylate (imatinib, Glivec; Novartis Pharmaceuticals), a small molecule tyrosine kinase inhibitor (TKI) specifically designed to inhibit the Bcr-Abl tyrosine kinase. Imatinib has dramatically improved the treatment of CML, inducing durable responses in the majority of patients with chronic phase CML. Nevertheless, two key issues remain—a number of patients develop resistance1 and primitive CML stem cells are insensitive to imatinib.2 The most common mechanisms of resistance are mutations in the kinase domain that affect imatinib binding,3 BCR-ABL amplification4 and altered drug efflux or influx.5 Second and third generation TKIs such as dasatinib, nilotinib6 and ponatinib7 demonstrate clinical efficacy in some cases of imatinib resistance; however, CML stem cells remain insensitive.8, 9 This highlights the need to find alternative therapeutic strategies to overcome resistance and eliminate the CML stem cell.
The proteasome is an enzymatic complex that has a key role in regulating cellular processes through selective degradation of intracellular proteins. There are three distinct enzymatic activities associated with the proteasome—chymotrypsin-like (CT-L), trypsin-like (T-L) and caspase-like (C-L)—mediated by subunits β5, β2 and β1, respectively. Upon exposure to interferon (IFN)-γ and tumor necrosis factor-α, an alternative form of the proteasome is formed, referred to as the immunoproteasome. The immunoproteasome expresses subunits LMP7, MECL1 and LMP2 in place of β5, β2 and β1, altering the proteasome to favor the generation of antigenic peptides.10 Over the last decade, the proteasome has emerged as a therapeutic target in hematopoietic malignancies. Bortezomib, the first-in-class proteasome inhibitor (PI) validated the proteasome as a therapeutic target and has provided significant advancement in the treatment of multiple myeloma (MM)11 and mantle cell lymphoma.12 Clinical benefit has also been seen with bortezomib-based combinations for non-Hodgkin’s lymphoma,13 myelodysplastic syndromes14 and acute myeloid leukemia.15 Following bortezomib’s success, there are a number of next generation PIs with improved pharmacological properties in clinical trials. The next generation compound carfilzomib is an epoxyketone-based inhibitor that binds irreversibly to the proteasome. Carfilzomib has recently been approved by the FDA for the treatment of relapsed/refractory MM and demonstrates greater efficacy and fewer side effects than bortezomib.16, 17
A number of studies support a potential role for the use of PIs in CML. In vitro studies demonstrated that bortezomib alone and in combination with kinase inhibitors is effective in imatinib-resistant CML cells.18, 19, 20 In addition, we have previously shown that BCR-ABL activity is associated with increased proteasome activity, and that CML cell lines are more susceptible to PIs than normal counterparts.21 In this study, we evaluate the activity of carfilzomib alone and in combination with TKIs imatinib and nilotinib, using imatinib-sensitive and -resistant CML models. We demonstrate a downregulation of phosphorylated ERK and accumulation of Abelson interactor proteins 1 and 2 (ABI 1/2), along with induction of apoptosis and inhibition of proliferation by carfilzomib in imatinib-sensitive and -resistant cell lines and CD34+38−-enriched CML stem cells. We show that the combination of carfilzomib with imatinib or nilotinib results in synergistic effects, even in imatinib-resistant cell lines. Finally, we demonstrate that the immunoproteasome is a major constituent of the total proteasome in the majority of CML cell lines and primary CML cells and that the presence of immunoproteasome subunits is associated with an increased sensitivity to carfilzomib.
Results
Effect of carfilzomib on key signaling pathways in CML
Cell lines and primary cells were pulsed with carfilzomib at IC50 doses for 1 h and returned to fresh medium for 24 h before protein lysates were prepared and immunoblot analysis was performed to determine the effect of carfilzomib on Bcr-Abl signaling pathways. Carfilzomib treatment resulted in a decrease of p-ERK by 52±11% (P<0.01), with no effect on STAT5 or PI3K signaling pathways (Figure 1a). We next looked at the effect of carfilzomib treatment on ABI 1/2 proteins, which have been reported to inhibit ERK activation that was induced by v-Abl.22 ABI 1/2 proteins have been shown to be stable in normal cells but rapidly degraded via the ubiquitin–proteasome pathway in Bcr-Abl expressing cells.23 We observed increased expression of ABI 1/2 in cells in which BCR-ABL was knocked down using siRNA and also in NBM CD34+38−-enriched cells compared with CML counterparts (Supplementary Figure 1). Treatment with carfilzomib at IC50 levels increased the expression of ABI 1/2 in cell lines and primary CD34+38−-enriched cells (range 2.2–6.8 fold, Figure 1b) and this was associated with an accumulation of polyubiquitinated ABI 1/2 (Figure 1c). ABI 2 has been reported to be tagged for degradation by the E3 ligase TRIM32 in head and neck cancer.24 Figure 1d demonstrates an association of ABI 2 with TRIM32 in the CML cell lines, which appears to be enhanced following treatment with carfilzomib, suggesting that TRIM32 also acts as an E3 ligase to target ABI proteins for degradation in Bcr-Abl expressing cells.
Mechanisms of action associated with carfilzomib in CML. (a, b) Cells were exposed to IC50 values of carfilzomib for 1 h, followed by growth in drug-free medium for 24 h before being harvested and whole cell lysates prepared. (a) Western blot analysis for activated (phosphorylated) ERK, Stat5 and PI3K signaling pathways following exposure to carfilzomib, total levels of ERK, Stat5 and PI3K were used as a loading control. Densitometry analysis is expressed as a percentage of untreated control, corrected to loading controls and the average results across cell lines and primary cells are given. Phosphorylated ERK was significantly decreased following carfilzomib treatment (P<0.01). (b) Western blot analysis of ABI 1/2 levels with and without exposure to carfilzomib. Densitometry analysis is expressed as a percentage of untreated control, corrected to loading controls and the average results across cell lines and primary cells are given. (c) Co-immunoprecipitation of ubiquitin and ABI 1/2 in CML cell lines with and without exposure to carfilzomib. Densitometry analysis is expressed as fold change from untreated control, corrected to input control. (d) Co-immunoprecipitation of TRIM32 and ABI-2 in CML cell lines with and without exposure to carfilzomib. Densitometry analysis is expressed as fold change from untreated control, corrected to input control.
Antiproliferative and apoptotic effects of carfilzomib in models of imatinib-sensitive and -resistant CML
CML cell lines were treated either continuously or pulsed for 1 h with increasing concentrations of carfilzomib (1–1000 nM) for up to 72 h. A time- and dose-dependent decrease in viability was observed in all cell lines with an IC50 of <15 nM at 24 h cultured continuously in the presence of carfilzomib (Figure 2a). To mimic the in vivo pharmacokinetics of carfilzomib, cell lines were pulsed for 1 h with the same concentrations of carfilzomib, followed by growth in drug-free medium for up to 72 h. This treatment also induced a time- and dose-dependent decrease in viability, although higher concentrations were required to achieve IC50 (20–79 nM, 24 h) (Figure 2b). Under both conditions, imatinib-resistant cell lines displayed equal or greater sensitivity to carfilzomib as their imatinib-sensitive counterparts.
Effects of carfilzomib on cell viability in models of imatinib-sensitive and -resistant CML. (a) Viability of CML cell lines following 24 h culture with increasing doses of carfilzomib (1–1000 nM). (b) Viability of CML cell lines following 1 h exposure to increasing doses of carfilzomib (1–1000 nM); cells were pulsed with carfilzomib followed by culture in drug-free medium for 24 h. Cell lines are grouped as parental imatinib-sensitive cell lines alongside their imatinib-resistant counterparts. (c) Viability of CML CD34+38− cells and normal CD34+38− cells exposed to 50 nM carfilzomib for 1 h followed by 24 h growth in drug-free medium. Viability of CML CD34+38− was significantly reduced compared with NBM (P=0.02). (a–c) All results are expressed as percentage of untreated control and represent mean±s.d. (n=3). (d) CML (n=3) and normal (n=2) CD34+ cells were exposed to 50 nM carfilzomib followed by long-term culture in LTC-IC assays. Results are expressed as percentage of control colony count and represent mean±s.d. There was significantly less colony growth in CML LTC-IC compared with NBM (P=0.04). (e) Western blot analysis for activated (cleaved) caspase-8 and caspase-9 following exposure to carfilzomib.
CD34+38− cells were enriched from three CML patient samples and normal bone marrow (NBM). As numbers of this enriched cell population are small, cells were exposed to a median dose of 50 nM carfilzomib for 1 h before being transferred to drug-free medium. After 24 h, the viability of CML CD34+38− cells was reduced by 39±1 % compared with 19±2 % in NBM (P=0.02; Figure 2c). To assess the effect of carfilzomib on longer-term stem cell proliferation, CD34+ cells were enriched from CML (n=3) and NBM samples (n=2), pulsed for 1 h with 50 nM carfilzomib and transferred to LTC-IC assays. Colony formation was reduced by 58±11% in CML stem cells compared with 44±7% in normal stem cells (P=0.04; Figure 2d).
The effect of 1-h exposure to carfilzomib on the induction of apoptosis in CML cell lines and primary samples was investigated. Pulse treatment with carfilzomib at IC50 doses induced an increase in caspase-3 activity along with an associated increase in the number of sub G0/G1 events, indicative of apoptosis (Supplementary Figure 2). Further analysis demonstrated induction of apoptosis through both the caspase-8 and -9 pathways, consistent with previous reports (Figure 2e).25
Synergistic activity of carfilzomib with TKIs imatinib and nilotinib
The combination of carfilzomib and imatinib or nilotinib was assessed in imatinib-sensitive and -resistant cell lines. Combinations were set up with all drugs using IC12.5, IC25, IC50 and IC75 values for imatinib-sensitive cell lines and drugs were combined in three ways: (i) carfilzomib and imatinib/nilotinib were added to cells simultaneously; (ii) cells were treated with carfilzomib at t=0 h, followed by imatinib/nilotinib at t=24 h; (iii) cells were treated with imatinib/nilotinib at t=0 h, followed by carfilzomib at t=24 h. Proliferation was assessed 48 h after first drug treatment. Calcusyn software was used to calculate a combination index (CI), whereby a value less than, equal to or greater than 1 indicates synergy, additivity or antagonism, respectively.
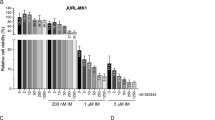
In imatinib-sensitive cell lines, all combinations of carfilzomib with the TKIs significantly reduced cell viability and proliferation compared with either drug alone (P<0.05) and were found to be synergistic (CI 0.241–0.941; IC50 values). There was no significant difference dependent on the order in which the drugs were added or the TKI used. To assess synergy in imatinib-resistant cell lines, IC50 values derived for the TKIs in imatinib-sensitive cell lines were used. Both, the simultaneous combination of carfilzomib and a TKI and the addition of either TKI before carfilzomib resulted in antagonistic effects (CI 1.053–4.553; IC50). Pretreatment with carfilzomib for 24 h followed by addition of a TKI resulted in a significant reduction in viability and proliferation compared with carfilzomib alone in 4 out of 5 imatinib-resistant cell lines (P⩽0.04; P=0.06 for Ba/F3 H396P cells) and synergy in all imatinib-resistant cell lines (CI 0.609–0.895; IC50). Using p-CRKL as a marker of Bcr-Abl kinase activity, we show that the sequential combination of carfilzomib and a TKI had no effect on p-CRKL, therefore demonstrating that the synergy observed is independent of Bcr-Abl inhibition (Figure 3c). Cell viability following combinations of carfilzomib and imatinib is represented graphically in Figures 3a and b, and CI values and cell proliferation for all combinations using IC50 values are given in Supplementary Table 1 and Supplementary Figure 3.
Carfilzomib and TKIs act synergistically in CML cell lines. (a) Viability of imatinib-sensitive cell lines following 48 h culture with carfilzomib, imatinib or a combination of both at IC12.5, IC25, IC50 or IC75 doses. Using IC50 values all combinations were significantly reduced compared to either drug alone (P<0.05). (b) Proliferation of imatinib-resistant cell lines following 48 h culture with carfilzomib, imatinib or a combination of both at IC12.5, IC25, IC50 or IC75 doses. For imatinib-resistant cell lines the IC values used for imatinib were the same as that used for imatinib-sensitive cell lines. Drugs were combined in three ways—(i) both drugs were added to cells simultaneously, (ii) cells were treated with carfilzomib first at t=0, followed by imatinib at t=24, or (iii) cells were treated with imatinib first at t=0, followed by carfilzomib at t=24. Results are expressed as a percentage of untreated control and represent mean±s.d. (n=3). Pretreatment with carfilzomib followed by addition of imatinib resulted in a significant reduction in viability in Ba/F3 T315I, Ba/F3 M351T, LAMA84R and KCL22R (P⩽0.04). (c) Western blot analysis of phosphorylated-CRKL in imatinib-sensitive and -resistant cell lines following exposure to carfilzomib, imatinib or a combination of carfilzomib at t=0, followed by imatinib at t=24; whole cell lysates were prepared 48 h after exposure to the first drug. (d) CML CD34+ cells (n=3) were cultured in the presence of carfilzomib, imatinib, nilotinib or a combination of carfilzomib plus imatinib/nilotinib either simultaneously or carfilzomib at t=0, followed by imatinib/nilotinib at t=24; after 48 h, cells were transferred to LTC-IC assays. Results are expressed as percentage of control colony count and represent mean±s.d.
We next investigated if the combination of carfilzomib and a TKI demonstrated a beneficial effect in CML cells. CD34+ cells were enriched from primary CML samples (n=3) and treated as follows: 50 nM carfilzomib, 1 μM imatinib or 30 nM nilotinib used as single agents, or carfilzomib combined simultaneously and sequentially at the prior indicated concentrations. Cells treated with single agent or combined simultaneously were exposed to inhibitors for 24 h; for sequential treatment the cells were exposed to carfilzomib for 24 h followed by either TKI for 24 h. LTC-IC assays were then performed on all cell treatments. No further decrease in colony formation was observed when carfilzomib was combined simultaneously with either TKI, compared with carfilzomib as a single agent. A reduction in colony formation from 42% with carfilzomib treatment alone, to 35%, and 40% of control following sequential treatment with imatinib and nilotinib was observed (Figure 3d); however, the difference was not significant (P=0.06 and P=0.19, respectively).
Proteasome profiles and subunit selectivity of carfilzomib in CML
Carfilzomib has been demonstrated to primarily target CT-L subunits of both the constitutive proteasome (β5) and immunoproteasome (LMP7) in MM and lymphoma cells.26, 27 To evaluate the inhibitory effect of carfilzomib in CML cells, we quantified the levels of constitutive proteasome and immunoproteasome subunits in primary CML cells, normal mononuclear cells and imatinib-sensitive and -resistant CML cell lines (Supplementary Table 2). In primary cells, the amount of active proteasome subunits per total protein concentration was significantly higher in CML cells compared with normal donors (24.05±1.38 ng/μg vs 16.69±2.86 ng/μg, P=0.001), consistent with our previous observations that Bcr-Abl activity is associated with increased proteasome activity.21 We found that immunoproteasome subunits were the major constituent of total proteasome in primary cells (59.1–65.4%) and Ba/F3 cell lines (61.1–70.2%), and comprised 16.3–30.1% of total proteasome in KCL22-S and -R and LAMA84-S and -R CML cell lines (Table 1). This is in agreement with previous reports on cells of hematopoietic origin27, 28 and confirms that the immunoproteasome is a substantive component of total proteasome in myeloid as well as lymphoid cells. The amount of CT-L subunits relative to total cellular protein was similar across all cell lines and primary CML cells (6.29±1.04 ng/μg). LMP7 was the predominant form of CT-L subunit expressed in normal mononuclear cells (83.8%), CML mononuclear cells (76.6%) and Ba/F3 cell lines (52.6–65.8%), and accounted for a significant proportion of CT-L activity in human CML cell lines (36.6–51.2%) (Figure 4a). In keeping with previous observations, we found that primary CML cells and KCL22-S and -R and LAMA84-S and -R predominantly express the immunoproteasome subunit LMP7 (12–25.3%) relative to MECL1 (2.2–15.2%) and LMP2 (1.2–18.6%).26 The contribution of individual proteasome subunits in Ba/F3 cell lines differs quite markedly from both primary cells and human CML cell lines. We have previously demonstrated that the proteasome subunit profiles are cell type dependent29 and this difference may reflect the different lineage origin and species of the cell lines.
Proteasome subunit selectivity of carfilzomib in CML. (a) Levels of CT-L proteasome subunits (β5 and LMP7) in primary CML and NBM and CML cell lines. (b–d) Proteasome active site subunit inhibition profiles of carfilzomib in KCL22S (b), LAMA84S (c) and Ba/F3 p210 (d) cell lines. Cells were treated with a 1 h pulse of carfilzomib and the ProCISE assay was performed to determine the level of inhibition. Results are expressed as a percentage of untreated control cells and represent mean±s.d. (n=3).
To examine the effect of carfilzomib on individual proteasome activities, cell lines were pulsed with increasing concentrations of carfilzomib (1–1000 nM) for 1 h and analyzed using the ProCISE assay. Whereas there was a dose-dependent inhibition of all proteasome activities (Figures 4b–d), carfilzomib displayed preferential inhibitory activity against CT-L subunits, with IC50 values of ⩽8.32 nM for the β5 subunit and ⩽16.55 nM for LMP7. IC50 values for T-L and C-L subunits were at least threefold higher (Supplementary Table 3).
The presence of immunoproteasome subunits increases sensitivity to carfilzomib
We, along with others, have reported that the sensitivity of tumor cells to PIs may be associated with differential expression of proteasome subunits.28, 29, 30 In this study, we found that in contrast to the proteasome profiles observed for CML cell lines and primary samples above, immunoproteasome subunits made little or no contribution to the overall proteasome activity in K562 cells (Supplementary Table 2). In this regard, the K562 cell line is more similar to a nonhematopoietic cell line. We demonstrate that although carfilzomib is a potent inhibitor of the β5 CT-L subunit in K562 cells (IC50=6.68 nM; Supplementary Table 2), the IC50 value for carfilzomib in reducing the proliferation of this cell line was >fivefold higher than the corresponding values for the other CML cell lines. We therefore sought to investigate whether the difference in sensitivity we observed with K562 cells was related to immunoproteasome expression. A549 lung carcinoma cell line, known to express low amounts of immunoproteasome,26 was included as a comparison. K562 and A549 cells were cultured in the presence of 100 U/ml IFN-γ for 72 h to induce immunoproteasome expression, before treatment with carfilzomib (1–1000 nM continuous exposure for 24 h). IFN-γ treatment resulted in an increase in the expression of LMP7 by fourfold in K562 cells and 10-fold in A549 cells (Figures 5a and b); IFN-α treatment produced similar results (Supplementary Figure 4C). The increase in LMP7 expression corresponded with a significantly increased sensitivity to carfilzomib (IC50 value reduced from 608 nM to 179 nM in K562 cells and 92 nM to 10 nM in A549 cells, P⩽0.01; Figures 5c and d). Conversely, we looked at the effect of LMP7 knockdown on the sensitivity of cells to carfilzomib. KCL22S and LAMA84S cells were treated with siRNA targeted against LMP7 before treatment with carfilzomib (1–1000 nM continuous exposure for 24 h). Downregulation of LMP7 (Supplementary Figure 4) was associated with a significant decrease in sensitivity to carfilzomib; the IC50 value for KCL22S cells increased from 5 nM to 16 nM (P=0.01) and LAMA84S cells increased from 7 nM to 20 nM (P=0.04). These results demonstrate that the presence of both the β5 and LMP7 CT-L subunits are required for optimal effect with carfilzomib and pretreatment with IFN-γ can sensitize cells to carfilzomib.
The presence of immunoproteasome subunits increases sensitivity to carfilzomib. (a) Levels of proteasome active site subunits in K562 cells before and after exposure to 100 U/ml IFN-γ (n=3). (b) Levels of proteasome active site subunits in A549 cells before and after exposure to 100 U/ml IFN-γ (n=3). (c) Proliferation of control K562 cells and K562 cells cultured in the presence of IFN-γ, following 1 h exposure to increasing doses of carfilzomib (1–1000 nM). Results are expressed as a percentage of untreated control cells and represent mean±s.d. (n=3). (d) Proliferation of control A549 cells and A549 cells cultured in the presence of IFN-γ, following 1 h exposure to increasing doses of carfilzomib (1–1000 nM). Results are expressed as a percentage of untreated control cells and represent mean±s.d. (n=3). (c, d) Exposure to INF-γ significantly increased sensitivity to carfilzomib (P<0.01). (e) Proliferation of control KCL22S cells and KCL22S cells transfected with either scrambled siRNA or siRNA targeted against LMP7 following 24 h exposure to increasing doses of carfilzomib (1–1000 nM). Results are expressed as a percentage of untreated control cells and represent mean±s.d. (n=3). Downregulation of LMP7 significantly reduces sensitivity of KCL22S to carfilzomib (P=0.01). (f) Proliferation of control LAMA84S cells and LAMA84S cells transfected with either scrambled siRNA or siRNA targeted against LMP7 following 24 h exposure to increasing doses of carfilzomib (1–1000 nM). Results are expressed as a percentage of untreated control cells and represent mean±s.d. (n=3). Downregulation of LMP7 significantly reduces sensitivity of LAMA84S to carfilzomib (P=0.04).
Discussion
Although the introduction of TKIs into the clinic has provided a major advancement in the treatment of CML, the development of drug resistance and persistence of TKI-resistant stem cells remain obstacles to eradicating the disease. The proteasome has become a validated target for cancer therapy, particularly in hematological malignancies. A number of reports demonstrate that bortezomib induces apoptosis in BCR-ABL expressing cells, including those resistant to imatinib and suggest that PIs may have significant activity in CML.18, 19, 20, 31 To date, only one study has investigated the clinical activity of bortezomib in CML. The pilot study demonstrated minimal efficacy of bortezomib as a single agent in imatinib-refractory CML and suggested that future trials should focus on alternative use of PIs in CML, such as combination-based treatments.32 In support of this, a recent report by Dewer et al.,31 demonstrates that a bortezomib-based regimen resulted in a complete hematological, cytogenetic and molecular remission in BCR-ABL+ acute lymphoblastic leukemia. Until recently, bortezomib was the only PI licensed for use in the clinic and its use can be restricted by limiting side effects such as peripheral neuropathy.17 However, the next generation PI carfilzomib has received FDA approval for the treatment of relapsed/refractory myeloma and appears to exhibit less toxicities than bortezomib. In this study, we have analyzed the effect of carfilzomib, both on its own and in combination with TKIs, in cell lines that reflect a wide spectrum of imatinib resistance and in CD34+38− populations, which represent the TKI-resistant stem cell population.
Bcr-Abl activates multiple downstream signaling pathways, including ERK, PI3K and STAT5 pathways, which contribute to leukemic cell proliferation and survival. We analyzed the effect of carfilzomib on these signaling pathways and found that exposure to carfilzomib resulted in a downregulation of phosphorylated ERK; this effect was replicated across all cell line models and primary CD34+38− cells. A previous study by Orlowski et al.,33 has also suggested inhibition of ERK signaling as a key factor in proteasome inhibitor-mediated apoptosis. Following on from this, we investigated the effect of carfilzomib on ABI proteins that have been reported to negatively regulate cell growth and transformation by specifically targeting the ERK pathway.22 ABI proteins were originally identified as binding partners of the Abl tyrosine kinase and two highly homologous members of this family, ABI-1 and ABI-2, were shown to be rapidly degraded through the ubiquitin–proteasome system in Bcr-Abl-expressing cells.23 In keeping with the findings by Dai et al.,23 we found that ABI 1/2 levels were higher in normal compared with CML CD34+38− cells and also that ABI 1/2 expression increased in CML cell lines in which BCR-ABL was knocked down. Treatment with carfilzomib resulted in a similar increase in ABI 1/2 protein expression by preventing the degradation of these proteins through the proteasome, as proved by the accumulation of polyubiquitinated ABI 1/2. ABI-2 in particular, has been documented to act as a tumor suppressor and an inhibitor of cell migration.24, 34, 35 Kano et al.,24 demonstrated that the E3 ligase TRIM32 is responsible for mediating the degradation of ABI-2 in head and neck squamous cell carcinoma, thereby promoting tumor cell growth, metastasis and drug resistance.34 In this study, we have demonstrated a protein–protein interaction between ABI-2 and TRIM32 and observed an accumulation of this protein interaction following treatment with carfilzomib, suggesting that TRIM32 may also act as an E3 ligase for ABI-2 in Bcr-Abl expressing cells. The role of Bcr-Abl in promoting the degradation of ABI-2 through TRIM32 is yet to be fully delineated. Collectively, these results demonstrate a novel mechanism of action for PIs in CML.
The effect of carfilzomib on the proliferation of imatinib-sensitive and -resistant cell populations was evaluated using either continuous treatment, or 1-h pulse treatment, which is more reflective of the in vivo pharmacokinetics of carfilzomib. Both methods induced a time- and dose-dependent decrease in proliferation, with equal or greater sensitivity to carfilzomib exhibited by imatinib-resistant cell lines compared with their imatinib-sensitive counterparts. This is in agreement with earlier studies demonstrating that imatinib resistance does not affect sensitivity to PIs.20, 21 The IC50 values obtained for carfilzomib in CML cell lines are comparable to those reported for MM cell lines,22 suggesting that these doses may be clinically relevant. Heaney et al.,20 previously demonstrated that primitive CML stem cells are sensitive to the apoptotic effects of bortezomib. Here we also demonstrate an antiproliferative and apoptotic effect of carfilzomib on the imatinib-resistant stem cell population. Furthermore, we found that the stem cells enriched from CML samples displayed greater sensitivity to carfilzomib than those enriched from nonmalignant samples.
Having established an effect for carfilzomib as a single agent in cell line models of imatinib-sensitive and -resistant CML, we also looked at the effect of carfilzomib in combination with the TKIs imatinib and nilotinib. In imatinib-sensitive cell lines, all combinations of carfilzomib with either TKI resulted in synergistic effects. Notably, we also observed that pretreatment with carfilzomib sensitizes imatinib-resistant cells to TKIs. The mechanism behind this synergistic effect is unclear; however, we demonstrate that it is independent of Bcr-Abl activity. Similar effects have been documented in a number of other studies using inhibitors of signaling pathways downstream of Bcr-Abl. For example, the combination of imatinib with chemotherapeutic agents,36 a Hsp90 inhibitor,37 PDK-1 inhibitor38 and leptomycin B39 have all been shown to produce synergistic activity in imatinib-resistant cell lines. The synergism between carfilzomib and TKIs was not replicated in the CML-quiescent stem cell population, nonetheless carfilzomib has a significant effect as a single agent in these cells.
Total levels of proteasome activity were found to be significantly higher in primary CML cells compared with normal, supporting previous observations by our group and others that demonstrate an increase in proteasome activity in BCR-ABL+ cells.21, 32, 40 Primary cells and cell lines exhibited both constitutive proteasome and immunoproteasome subunits. Primary cells were found to express a higher percentage of the LMP7 subunit than CML cell lines. This pattern of higher immunoproteasome activity in primary cells has also been observed in MM.26 Carfilzomib has been reported to selectively inhibit the CT-L subunits (β5 and LMP7) of the proteasome in MM and lymphoma cells.26, 27 In keeping with this, we show that carfilzomib inhibits CT-L subunits with at least threefold selectivity compared with T-L and C-L subunits.
Finally, we investigated whether the presence of immunoproteasome subunits in CML cells influences the sensitivity of the cells to carfilzomib. Our group, along with others, have reported that sensitivity of tumor cells to PIs is associated with proteasome activity levels and subunit composition.28, 29, 30 In addition, Parlati et al.,26 demonstrated that inhibition of either the β5 or LMP7 subunit alone was insufficient to produce an antitumor response in hematopoietic cells. In this study, we found that the CML cell line K562 exhibited little to no immunoproteasome activity and, although carfilzomib was a potent inhibitor of the β5 subunit in these cells, the IC50 for carfilzomib in K562 cells was >fivefold higher than that for the immunoproteasome-expressing cell lines. Induction of immunoproteasome expression in K562 cells by IFN-γ resulted in an increase in sensitivity to carfilzomib, and this effect was also replicated in the lung carcinoma cell line A549. Conversely, knockdown of LMP7 expression reduced sensitivity to carfilzomib in KCL22S and LAMA84S cells. These results suggest that both CT-L subunits are required for optimal effect and that proteasome composition may predict the response to carfilzomib.
In summary, this work shows that carfilzomib effectively reduces proliferation and induces apoptosis in CML cell lines and primary cells, regardless of their sensitivity to imatinib. We have shown for the first time that proteasome inhibition in CML cells is associated with a decrease in ERK signaling and increased expression of the tumor suppressor ABI-2. Combination of carfilzomib with TKIs has been demonstrated to generate synergistic effects, even in imatinib-resistant cells, and the presence of immunoproteasome subunits influences sensitivity to carfilzomib. Taken together, these findings suggest that carfilzomib could be a useful therapeutic agent in CML, and its role in resensitizing imatinib-resistant cells to TKIs warrants further investigation.
Materials and methods
Compounds
Imatinib and nilotinib were provided by Novartis Pharmaceuticals (Surrey, UK) and reconstituted in sterile water or DMSO, respectively. Carfilzomib was provided by Onyx Pharmaceuticals, Inc (South San Francisco, CA, USA) and was reconstituted in DMSO.
Cells and culture conditions
A number of cell lines were used to reflect a spectrum of imatinib-sensitive and -resistant disease. Ba/F3 cells transfected with p210 and mutated (T315I, M351T, H396P) BCR-ABL were kindly provided by Dr. Brian Druker, (Oregon Health and Science University, Portland, OR, USA). K562 cells were purchased from the European Collection of Cell Cultures (Salisbury, UK). LAMA84 imatinib-sensitive and -resistant clones (LAMA84S and LAMA84R) and KCL22 imatinib-sensitive and -resistant clones (KCL22S and KCL22R) were provided by Professor Junia Melo. LAMA84R cells have increased copy numbers of BCR-ABL and express the multidrug resistance p-glycoprotein4 and the mechanism of resistance in KCL22R cells is independent of BCR-ABL.41 Cells were cultured in a humidified incubator at 37 °C and 5% CO2 in RPMI-1640 supplemented with 100 U/ml penicillin, 100 μg/ml streptomycin and 10% fetal calf serum (Gibco BRL, Paisley, UK). LAMA84R and KCL22R cell lines were cultured continuously in the presence of 1 μM imatinib. A549 lung carcinoma cells (European Collection of Cell Cultures) were cultured in DMEM supplemented with 100 U/ml penicillin, 100 μg/ml streptomycin and 10% fetal calf serum. Authentication was conducted by LGC Standards Cell Line Authentication Service.
Primary CML samples and normal controls
Leukapheresis products were obtained from CML patients at the time of diagnosis and bone marrow from healthy donors was collected as a normal control. All samples were obtained with ethical approval from the Research Ethics Committee, Northern Ireland, and the National Health Service Greater Glasgow Institutional Review Board and those involved gave their informed consent in accordance with the Declaration of Helsinki. CD34+ cells were enriched from the samples using an AutoMACS system according to the manufacturer’s instructions (Miltenyi Biotech, Surrey, UK). CD34+ cells were stained with CD34-APC and CD38− FITC (BD Biosciences, Oxford, UK) and sorted using a FACSAria (BD Biosciences) to obtain an enriched CD34+38− population. CD34+ and CD34+38− cells were cultured in IMDM medium (Gibco BRL) supplemented with serum substitute (bovine serum albumin, insulin, transferrin; StemCell Technologies, Grenoble, France), 2 mM L-glutamine, 100 U/ml penicillin, 100 μg/ml streptomycin, 0.1 mM 2-mercaptoethanol and 0.8 μg/ml low-density lipoprotein (all from Sigma-Aldrich, Dorset, UK) and a growth factor cocktail of 20 ng/ml recombinant human (rh) IL-3, 20 ng/ml rhIL-6, 100 ng/ml rh Flt-3 ligand and 100 ng/ml rh stem cell factor (all from StemCell Technologies).
Long-term culture initiating cell assay
CD34+ cells were overlaid on a pre-established irradiated (80 Gy) stromal layer of M2–10B4 cells (ATCC, Middlesex, UK) in Myelocult myeloid long-term culture medium (StemCell Technologies). Cultures were maintained for 5 weeks with weekly half-medium changes. Cells were then harvested, counted and transferred to Methocult media (StemCell Technologies). After 2 weeks, colonies were counted using a light microscope.
Cell viability
CellTiter-Glo luminescent assay (Promega, Southampton, UK) was used to analyze cell viability by measuring ATP levels according to the manufacturer’s instructions. Luminescence was measured using a Tecan Genios microplate reader (Tecan Genios, Reading, UK).
Cell proliferation
CyQUANT proliferation assay (Life Technologies, Paisley, UK) was used to analyze cell proliferation by measuring cellular DNA content using a fluorescent dye, according to the manufacturer’s instructions. Fluorescence was measured using a Cytofluor Series 400 multiwell plate reader at an excitation wavelength of 480 nM and emission wavelength of 520 nM.
Cell cycle analysis
Cells were harvested, washed in phosphate-buffered saline and fixed in 70% ethanol. Fixed cells were stained with 50 μg/ml propidium iodide (Sigma) for 30 min. DNA content was subsequently measured using an LSR II flow cytometer.
Caspase-3 activity
The Caspase-Glo 3 Assay (Promega) was used to determine caspase-3 activity by measuring cleavage of DEVD, according to the manufacturer’s instructions. Luminescence was measured using a Tecan Genios microplate reader.
Western blotting
Cells were harvested and lysed in radioimmunoprecipitation assay buffer containing protease and phosphatase inhibitors. Immunoprecipitation experiments were carried out using a crosslink immunoprecipitation kit (Pierce, Thermo Scientific, Loughborough, UK), according to the manufacturer’s instructions. Equal amounts of protein were denatured in LDS sample buffer (Invitrogen Ltd, Paisley, UK) at 95 °C for 5 min, resolved by SDS–PAGE on 10% Bis-Tris gels (Invitrogen Ltd) and subsequently transferred to a polyvinylidene fluoride membrane. Immunoblotting was carried out using antibodies against ubiquitin, phosphorylated (p)-ERK, ERK, p-PI3K, PI3K, p-STAT5, STAT5, p-CRKL, cleaved caspase-3, cleaved caspase-8, cleaved caspase-9 (all from Cell Signaling Technology, Hertfordshire, UK), TRIM32 and GAPDH (both from Abcam, Cambridge, UK) and ABI 1/2 (kindly provided by Dr. Karim Dib, Queen’s University Belfast) or ABI-2 (Abcam) and secondary antibodies anti-mouse and anti-rabbit (DAKO, Stockport, UK). Blots were scanned into the AutoChemi System (UVP, Cambridge, UK) and densitometry analysis was performed using LabWorks 4.5 image acquisition and analysis software. Values obtained were corrected to loading controls and are expressed as a percentage of untreated controls. The average values for three replicate experiments are shown for each cell line.
ProCISE assay
A proteasome active site ELISA by name of ProCISE (Proteasome Constitutive/Immunoproteasome Subunit ELISA) was used to measure each proteasome subunit activity of the constitutive and immunoproteasome in homogenates of cell samples. This assay was performed as previously described in.26
Analysis of drug combinations
The median effect of Chou–Talalay was employed to analyze the effect of carfilzomib in combination with imatinib or nilotinib using Calcusyn software (Biosoft, Cambridge, UK).42 The values used for the analysis were derived from cell viability as measured by CellTiter-Glo.
Inhibition of gene expression by siRNA
K562, KCL22S or LAMA84S cells were nucleofected following the manufacturer’s instructions using the Cell Line Nucleofector Kit V, program T-03 (Amaxa, Lonza, Castleford, UK) and either siRNA directed against BCR-ABL (5′-GCA GAG AGU UCA AAA GCC CUU-3′), LMP7 (Silencer Select siRNA ID s11360, Life Technologies) or a scrambled siRNA sequence (5′-UUG UAC GGC AUC AGC GUU ATT-3′).
References
de Lavallade H, Apperley JF, Khorashad JS, Milojkovis D, Reid AG, Bua M et al. Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol 2008; 26: 3358–3363.
Graham SM, Jorgensen HG, Allan E, Pearson C, Alcorn MJ, Richmond L et al. Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood 2002; 99: 319–325.
Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J et al. Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood 2003; 102: 276–283.
Mahon FX, Deininger MW, Schultheis B, Chabrol J, Reiffers J, Goldman JM et al. Selection and characterization of BCR-ABL positive cell lines with differential sensitivity to the tyrosine kinase inhibitor STI571: diverse mechanisms of resistance. Blood 2000; 96: 1070–1079.
Ni LN, Li JY, Miao KR, Qiao C, Zhang SJ, Qiu HR et al. Multidrug resistance gene (MDR1) polymorphisms correlate with imatinib response in chronic myeloid leukemia. Med Oncol 2011; 28: 265–269.
Ibrahim AR, Clark RE, Holyoake TL, Byrne J, Sheperd P, Apperly JF et al. Second-generation tyrosine kinase inhibitors improve the survival of patients with chronic myeloid leukemia in whom imatinib therapy has failed. Haematologica 2011; 96: 1779–1782.
O'Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F et al. AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell 2009; 16: 401–412.
Jorgensen HG, Allan EK, Jordanides NE, Mountford JC, Holyoake TL . Nilotinib exerts equipotent antiproliferative effects to imatinib and does not induce apoptosis in CD34+ CML cells. Blood 2007; 109: 4016–4019.
Konig H, Copland M, Chu S, Jove R, Holyoake TL, Bhatia R . Effects of dasatinib on SRC kinase activity and downstream intracellular signaling in primitive chronic myelogenous leukemia hematopoietic cells. Cancer Res 2008; 68: 9624–9633.
Noda C, Tanahashi N, Shimbara N, Hendil KB, Tanaka K . Tissue distribution of constitutive proteasomes, immunoproteasomes, and PA28 in rats. Biochem Biophys Res Commun 2000; 277: 348–354.
Crawford LJ, Irvine AE . Proteasome inhibitors in the treatment of multiple myeloma. In: Gupta A (ed.). Multiple Myeloma—An Overview. InTech, 2012, pp 3–32.
Kane RC, Dagher R, Farrell A, Ko CW, Sridhara R, Justice R et al. Bortezomib for the treatment of mantle cell lymphoma. Clin Cancer Res 2007; 13: 5291–5294.
Mato AR, Feldman T, Goy A . Proteasome inhibition and combination therapy for non-Hodgkin's lymphoma: from bench to bedside. Oncologist 2012; 17: 694–707.
Natarajan-Ame S, Park S, Ades L, Vey N, Guerci-Beesler A, Cahn JY et al. Bortezomib combined with low-dose cytarabine in intermediate-2 and high risk myelodysplastic syndromes. A phase I/II study by the GFM. Br J Haematol 2012; 158: 232–237.
Blum W, Schwind S, Tarighat SS, Gever S, Eisfeld AK, Whitman S et al. Clinical and pharmacodynamic activity of bortezomib and decitabine in acute myeloid leukemia. Blood 2012; 119: 6025–6031.
Vij R, Wang M, Kaufman JL, Lonial S, Jakubowiak AJ, Stewart AK et al. An open-label, single-arm, phase 2 (PX-171-004) study of single-agent carfilzomib in bortezomib-naive patients with relapsed and/or refractory multiple myeloma. Blood 2012; 119: 5661–5670.
Katsnelson A . Next-generation proteasome inhibitor approved in multiple myeloma. Nat Biotechnol 2012; 30: 1011–1012.
Li QF, Yan J, Zhang K, Yang YF, Xiao FJ, Wu CT et al. Bortezomib and sphingosine kinase inhibitor interact synergistically to induces apoptosis in BCR/ABl+ cells sensitive and resistant to STI571 through downregulation Mcl-1. Biochem Biophys Res Commun 2011; 405: 31–36.
Albero MP, Vaquer JM, Andreu EJ, Villanueva JJ, Franch L, Ivorra SM et al. Bortezomib decreases Rb phosphorylation and induces caspase-dependent apoptosis in Imatinib-sensitive and -resistant Bcr-Abl1-expressing cells. Oncogene 2010; 29: 3276–3286.
Heaney NB, Pellicano F, Zhang B, Crawford L, Chu S, Kazmi SM et al. Bortezomib induces apoptosis in primitive chronic myeloid leukemia cells including LTC-IC and NOD/SCID repopulating cells. Blood 2010; 115: 2241–2250.
Crawford LJ, Windrum P, Magill L, Melo JV, McCallum L, McMullin MF et al. Proteasome proteolytic profile is linked to Bcr-Abl expression. Exp Hematol 2009; 37: 357–366.
Fan PD, Goff SP . Abl interactor 1 binds to sos and inhibits epidermal growth factor- and v-Abl-induced activation of extracellular signal-regulated kinases. Mol Cell Biol 2000; 20: 7591–7601.
Dai Z, Quackenbush RC, Courtney KD, Grove M, Cortez D, Reuther GW et al. Oncogenic Abl and Src tyrosine kinases elicit the ubiquitin-dependent degradation of target proteins through a Ras-independent pathway. Genes Dev 1998; 12: 1415–1424.
Kano S, Miyajima N, Fukuda S, Hatakeyama S . Tripartite motif protein 32 facilitates cell growth and migration via degradation of Abl-interactor 2. Cancer Res 2008; 68: 5572–5580.
Kuhn DJ, Chen Q, Voorhees PM, Strader JS, Shenk KD, Sun CM et al. Potent activity of carfilzomib, a novel, irreversible inhibitor of the ubiquitin-proteasome pathway, against preclinical models of multiple myeloma. Blood 2007; 110: 3281–3290.
Parlati F, Lee SJ, Aujay M, Suzuki E, Levitsky K, Lorens JB et al. Carfilzomib can induce tumor cell death through selective inhibition of the chymotrypsin-like activity of the proteasome. Blood 2009; 114: 3439–3447.
Demo SD, Kirk CJ, Aujay MA, Buchholz T, Dajer M, Ho MN et al. Antitumor activity of PR-171, a novel irreversible inhibitor of the proteasome. Cancer Res 2007; 67: 6383–6391.
Busse A, Kraus M, Na IK, Rietz A, Scheibenbogen C, Driessen C et al. Sensitivity of tumor cells to proteasome inhibitors is associated with expression levels and composition of proteasome subunits. Cancer 2008; 112: 659–670.
Crawford LJ, Walker B, Ovaa H, Chauhan D, Anderson KC, Morris TC et al. Comparative selectivity and specificity of the proteasome inhibitors BzLLLCOCHO, PS-341, and MG-132. Cancer Res 2006; 66: 6379–6386.
Kraus M, Ruckrich T, Reich M, Gogel J, Beck A, Kammer W et al. Activity patterns of proteasome subunits reflect bortezomib sensitivity of hematologic malignancies and are variable in primary human leukemia cells. Leukemia 2007; 21: 84–92.
Dewar R, Chen ST, Yeckes-Rodin H, Miller K, Khosravi-Far R . Bortezomib treatment causes remission in a Ph+ALL patient and reveals FoxO as a theranostic marker. Cancer Biol Ther 2011; 11: 552–558.
Santos FP, Kantarjian H, McConkey D, O’Brien S, Faderl S, Borthakur G et al. Pilot study of bortezomib for patients with imatinib-refractory chronic myeloid leukemia in chronic or accelerated phase. Clin Lymphoma Myeloma Leuk 2011; 11: 355–360.
Orlowski RZ, Small GW, Shi YY . Evidence that inhibition of p44/42 mitogen-activated protein kinase signaling is a factor in proteasome inhibitor-mediated apoptosis. J Biol Chem 2002; 277: 27864–27871.
Dai Z, Pendergast AM . Abi-2, a novel SH3-containing protein interacts with the c-Abl tyrosine kinase and modulates c-Abl transforming activity. Genes Dev 1995; 9: 2569–2582.
Lin TY, Huang CH, Chou WG, Juang JL . Abi enhances Abl-mediated CDC2 phosphorylation and inactivation. J Biomed Sci 2004; 11: 902–910.
Tipping AJ, Mahon FX, Zafirides G, Lagarde V, Goldman JM, Melo JV . Drug responses of imatinib mesylate-resistant cells: synergism of imatinib with other chemotherapeutic drugs. Leukemia 2002; 16: 2349–2357.
Radujkovic A, Schad M, Topaly J, Veldwijk MR, Laufs S, Schultheis BS et al. Synergistic activity of imatinib and 17-AAG in imatinib-resistant CML cells overexpressing BCR-ABL-inhibition of P-glycoprotein function by 17-AAG. Leukemia 2005; 19: 1198–1206.
Tseng PH, Lin HP, Zhu J, Chen KF, Hade EM, Young DC et al. Synergistic interactions between imatinib mesylate and the novel phosphoinositide-dependent kinase-1 inhibitor OSU-03012 in overcoming imatinib mesylate resistance. Blood 2005; 105: 4021–4027.
Kancha RK, von Bubnoff N, Miething C, Peschel C, Gotze KS, Duyster J . Imatinib and leptomycin B are effective in overcoming imatinib-resistance due to bcr-abl amplification and clonal evolution but not due to bcr-abl kinase domain mutation. Haematologica 2008; 93: 1718–1722.
Magill L, Lynas J, Morris TC, Walker B, Irvine AE . Proteasome proteolytic activity in hematopoietic cells from patients with chronic myeloid leukemia and multiple myeloma. Haematologica 2004; 89: 1428–1433.
Colavita I, Esposito N, Martinelli R, Catanzano F, Melo JV, Pane F et al. Gaining insights into the Bcr-Abl activity-independent mechanisms of resistance to imatinib mesylate in KCL22 cells: a comparative proteomic approach. Biochim Biophys Acta 2010; 1804: 1974–1987.
Chou TC, Talalay P . Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul 1984; 22: 27–55.
Acknowledgements
This work was supported by the Leukaemia Lymphoma Research UK (LJC, AEI and BW), Northern Ireland Leukaemia Research Fund (LJC and AEI), Cancer Research UK (TLH and SS), the Glasgow Experimental Cancer Medicine Centre (TLH) and the NIHR Biomedical Research Centre Funding Scheme, UK (JVM). We also wish to thank Jennifer Murphy for technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
ETC and Monette Aujay are employees of Onyx Pharmaceuticals Inc.The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Oncogenesis website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Crawford, L., Chan, E., Aujay, M. et al. Synergistic effects of proteasome inhibitor carfilzomib in combination with tyrosine kinase inhibitors in imatinib-sensitive and -resistant chronic myeloid leukemia models. Oncogenesis 3, e90 (2014). https://doi.org/10.1038/oncsis.2014.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/oncsis.2014.3
Keywords
This article is cited by
-
Effect of asciminib and vitamin K2 on Abelson tyrosine-kinase-inhibitor-resistant chronic myelogenous leukemia cells
BMC Cancer (2023)
-
RUNX1-Evi-1 fusion gene inhibited differentiation and apoptosis in myelopoiesis: an in vivo study
BMC Cancer (2015)
-
Regulation rewiring analysis reveals mutual regulation between STAT1 and miR-155-5p in tumor immunosurveillance in seven major cancers
Scientific Reports (2015)
-
Combination therapy with nilotinib for drug-sensitive and drug-resistant BCR-ABL-positive leukemia and other malignancies
Archives of Toxicology (2014)