Abstract
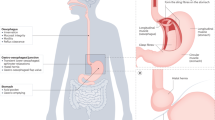
Nonerosive reflux disease (NERD) represents the more common phenotypic presentation of GERD and comprises patients who have typical symptoms without any mucosal breaks at endoscopy. However, these patients are markedly heterogeneous from a pathophysiological point of view and should be correctly classified by means of 24 h impedance–pH testing, which enables detection of both acidic and weakly acidic reflux and correlation with symptoms. This technique is able to identify two subsets of NERD (that is, patients with an excess of acid or with a hypersensitive oesophagus to both acid and weakly acidic reflux) and patients with functional heartburn (who do not have any kind of reflux underlying their symptoms and must be excluded from the realm of GERD). The mechanisms of symptom generation are not clear in patients with NERD, but the presence of microscopic oesophagitis, including the dilation of intercellular spaces, seems to have a relevant role. Patients with NERD in whom acid is the main pathogenetic factor respond successfully to PPI therapy, while those with hypersensitive oesophagus to weakly acidic reflux need to be treated with reflux inhibitors or surgery, although the experience in this field is very scant. Patients with functional heartburn should undergo therapy with pain modulators, but large placebo-controlled trials are necessary.
Key Points
-
Nonerosive reflux disease (NERD) represents the more common phenotypic presentation of GERD and includes patients who are heterogeneous from a pathophysiological and clinical point of view
-
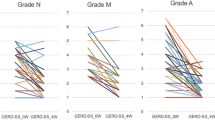
24 h impedance–pH testing has enabled subdivision of patients with NERD into several subgroups according to their oesophageal acid exposure time and symptom association analysis to acid and/or weakly acidic reflux episodes
-
This technique has identified a new subgroup of patients with NERD who have hypersensitive oesophagus to weakly acidic reflux, which contributes to narrowing down the population of patients with functional heartburn
-
The mechanisms of symptom generation are not completely understood in patients with NERD, but the presence of microscopic oesophagitis seems to have a relevant role
-
Treatment of NERD is based on the use of PPIs, which are successful in patients in whom acid has a pathogenetic role; pain modulators can be used in patients with hypersensitive oesophagus
-
Patients with functional heartburn should be treated with pain modulators, but clinical trials aimed at assessing the efficacy of these drugs in this well-defined group are lacking at this time
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Locke, G. R. 3rd, Talley, N. J., Fett, S. L., Zinsmeister, A. R. & Melton, L. J. 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 112, 1448–1456 (1997).
Dent, J., El-Serag, H. B., Wallander, M. A. & Johansson, S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 54, 710–717 (2005).
Vigneri, S. et al. A comparison of five maintenance therapies for reflux esophagitis. N. Engl. J. Med. 333, 1106–1110 (1995).
Chiba, N., De Gara, C. J., Wilkinson, J. M. & Hunt, R. H. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: ameta-analysis. Gastroenterology 112, 1798–1810 (1997).
Vakil, N., van Zanten, S. V., Kahrilas, P., Dent, J. & Jones, R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am. J. Gastroenterol. 101, 1900–1920 (2006).
Modlin, I. M. et al. Diagnosis and management of non-erosive reflux disease—The Vevey NERD Consensus Group. Digestion 80, 74–88 (2009).
Ronkainen, J. et al. High prevalence of gastro-oesophageal reflux symptoms and oesophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand. J. Gastroenterol. 40, 275–285 (2005).
Zagari, R. M. et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: the Loiano-Monghidoro study. Gut 57, 1354–1359 (2008).
Gaddam, S. et al. The impact of pre-endoscopy proton pump inhibitor use on the classification of non-erosive reflux disease and erosive esophagitis. Aliment. Pharmacol. Ther. 32, 1266–1274 (2010).
Pace, F., Santalucia, F. & Bianchi Porro, G. Natural history of gastro-oesophageal reflux disease without oesophagitis. Gut 32, 845–848 (1991).
Labenz, J. et al. Prospective follow-up data from the ProGERD study suggest that GERD is not a categorical disease. Am. J. Gastroenterol. 101, 2457–2462 (2006).
Kuster, E. et al. Predictive factors of the long-term outcome in gastro-oesophageal reflux disease: six year follow-up of 107 patients. Gut 35, 8–14 (1994).
Fass, R. & Ofman, J. Gastroesophageal reflux disease—should we adopt a new conceptual framework? Am. J. Gastroenterol. 97, 1901–1909 (2202).
Fullard, M., Kang, J. Y., Neild, P., Poullis, A. & Maxwell, J. D. Systematic review: does gastro-oesophageal reflux disease progress? Aliment. Pharmacol. Ther. 24, 33–45 (2006).
Dent, J. et al. An evidence-based appraisal of reflux disease management—the Genval Workshop Report. Gut 44 (Suppl. 2), S1–S16 (1999).
Martinez, S. D. et al. Non-erosive reflux disease (NERD)—acid reflux and symptom patterns. Aliment. Pharmacol. Ther. 17, 537–545 (2003).
Galmiche, J. P. et al. Functional esophageal disorders. Gastroenterology 130, 1459–1465 (2006).
Calabrese, C. et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am. J. Gastroenterol. 100, 537–542 (2005).
Numans, M. E., Lau, J., de Wit, N. J. & Bonis, P. A. Short-term treatment with proton-pump inhibitors as a test for gastroesophageal reflux disease: a meta-analysis of diagnostic test characteristics. Ann. Intern. Med. 140, 518–527 (2004).
Dent, J. et al. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: the Diamond Study. Gut 59, 714–721 (2010).
Bytzer, P. et al. Limited ability of the proton-pump inhibitor test to identify patients with gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol. 10, 1360–1366 (2012).
Smout, A. J. The patient with GORD and chronically recurrent problems. Best Pract. Res. Clin. Gastroenterol. 21, 365–378 (2007).
Pandolfino, J. E. & Kwiatek, M. A. Use and utility of the Bravo pH capsule. J. Clin. Gastroenterol. 42, 571–578 (2008).
Sifrim, D. et al. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid and gas reflux. Gut 53, 1024–1031 (2004).
Zentilin, P. et al. Combined multichannel intraluminal impedance and pH-metry—a novel technique to improve detection of gastro-oesophageal reflux. Literature review. Dig. Liver Dis. 36, 565–569 (2004).
Shay, S. et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am. J. Gastroenterol. 99, 1037–1043 (2004).
Zerbib, F. et al. Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian-French cohort of healthy subjects. Aliment. Pharmacol. Ther. 22, 1011–1021 (2005).
Zentilin, P. et al. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig. Liver Dis. 38, 226–232 (2006).
Tutuian, R. Reflux monitoring: current status. Curr. Gastroenterol. Rep. 10, 263–270 (2008).
Bredenoord, A. J., Hemmink, G. J. & Smout, A. J. Relationship between gastro-oesophageal reflux pattern and severity of mucosal damage. Neurogastroenterol. Motil. 21, 807–812 (2009).
Frazzoni, M. et al. Reflux patterns in patients with short-segment Barrett's oesophagus: a study using impedance-pH monitoring off and on proton pump inhibitor therapy. Aliment. Pharmacol. Ther. 30, 508–515 (2009).
Savarino, E. et al. Characteristics of gastro-esophageal reflux episodes in Barrett's esophagus, erosive esophagitis and healthy volunteers. Neurogastroenterol. Motil. 22, 1061-e280 (2010).
Sifrim, D. et al. Acid, non-acid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology 120, 1588–1598 (2001).
Namasivayam, V., Arora, A. S. & Murray, J. A. Weakly acidic reflux. Dis. Esophagus 24, 56–62 (2011).
Savarino, E. et al. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. Am. J. Gastroenterol. 105, 1053–1061 (2010).
Zerbib, F. et al. Esophageal pH-impedance monitoring and symptom analysis in GERD: a study in patients off and on therapy. Am. J. Gastroenterol. 101, 1956–1963 (2006).
Hemmink, G. J. et al. Esophageal pH-impedance monitoring in patients with therapy-resistant reflux symptoms: on or off proton pump inhibitor? Am. J. Gastroenterol. 103, 2446–2453 (2008).
Savarino, E. et al. The role of non-acid reflux in NERD: lessons learned from impedance pH monitoring in 150 patients off therapy. Am. J. Gastroenterol. 103, 2685–2693 (2008).
Kahrilas, P. J. & Smout, A. J. Esophageal disorders. Am. J. Gastroenterol. 105, 747–756 (2010).
Frazzoni, M., De Micheli, E. & Savarino, V. Different patterns of esophageal acid exposure distinguish complicated reflux disease from either reflux esophagitis or non-erosive reflux disease. Aliment. Pharmacol. Ther. 18, 1091–1098 (2003).
Hershcovici, T. & Fass, R. Nonerosive reflux disease (NERD)—An update. J. Neurogastroenterol. Motil. 16, 8–21 (2010).
Hirschowitz, B. I. A critical analysis, with appropriate controls, of gastric acid and pepsin secretion in clinical esophagitis. Gastroenterology 101, 1149–1158 (1991).
Zentilin, P. et al. Circadian pattern of intragastric acidity in patients with non-erosive reflux disease (NERD). Aliment. Pharmacol. Ther. 17, 353–359 (2003).
Adachi, K. et al. Predominant nocturnal acid reflux in patients with Los Angeles grade C and D reflux esophagitis. J. Gastroenterol. Hepatol. 16, 1191–1196 (2001).
Shapiro, M., Green, C., Faybush, E. M., Esquivel, R. F. & Fass, R. The extent of oesophageal acid exposure overlap among the different gastro-oesophageal reflux disease groups. Aliment. Pharmacol. Ther. 23, 321–329 (2006).
Dickman, R. et al. Comparison of esophageal acid exposure distribution along the esophagus among the different gastro-esophageal reflux disease (GERD) groups. Am. J. Gastroenterol. 101, 2463–2469 (2006).
Fass, R. Erosive esophagitis and nonerosive reflux disease (NERD). Comparison of epidemiologic, physiologic, and therapeutic characteristics. J. Clin. Gastroenterol. 41, 131–137 (2007).
Frazzoni, M., Manno, M., De Micheli, E. & Savarino, V. Pathophysiological characteristics of the various forms of gastro-oesophageal reflux disease. Spectrum disease or distinct phenotypic presentations? Dig. Liver Dis. 38, 643–648 (2006).
Savarino, E. & Tutuian, R. Combined multichannel intraluminal impedance and manometry testing. Dig. Liver Dis. 40, 167–173 (2008).
Savarino, E. et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment. Pharmacol. Ther. 34, 476–486 (2011).
Cameron, A. J. Barrett's esophagus: prevalence and size of hiatal hernia. Am. J. Gastroenterol. 94, 2054–2059 (1999).
Savarino, V., Savarino, E., Parodi, A. & Dulbecco, P. Functional heartburn and non-erosive reflux disease. Dig. Dis. 25, 172–174 (2007).
Zerbib, F., Bruley des Varannes, S., Simon, M. & Galmiche, J. P. Functional heartburn: definition and management strategies. Curr. Gastroenterol. Rep. 14, 181–188 (2012).
Savarino, E. et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J. Gastroenterol. 47, 159–168 (2012).
Savarino, E. et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut 58, 1185–1191 (2009).
Hershcovici, T. & Fass, R. Are functional heartburn and functional dyspepsia one disorder? Nat. Rev. Gastroenterol. Hepatol. 7, 71–72 (2010).
Lee, S. Y. et al. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion 79, 196–201 (2009).
Jung, H. K. et al. Overlap of gastrooesophageal reflux disease and irritable bowel syndrome: prevalence and risk factors in the general population. Aliment. Pharmacol. Ther. 26, 453–461 (2007).
Barlow, W. J. & Orlando, R. C. The pathogenesis of heartburn in non-erosive reflux disease: a unifying hypothesis. Gastroenterology 128, 771–778 (2005).
Caviglia, R. et al. Dilated intercellular spaces of esophageal epithelium in non erosive reflux disease patients with physiological esophageal acid exposure. Am. J. Gastroenterol. 100, 543–548 (2005).
Van Malenstein, H., Farrè, R. & Sifrim, D. Esophageal dilated intercellular spaces (DIS) and non erosive reflux disease. Am. J. Gastroenterol. 103, 1021–1028 (2008).
Zentilin, P. et al. Reassessment of the diagnostic value of histology in patients with GERD, using multiple biopsy sites and an appropriate control group. Am. J. Gastroenterol. 100, 2299–2306 (2005).
Mastracci, L. et al. Cell proliferation of squamous epithelium in gastro-oesophageal reflux disease: correlation with clinical, endoscopic and morphological data. Aliment. Pharmacol. Ther. 25, 637–645 (2007).
Ribolsi, M. et al. Intercellular space diameters of the oesophageal epithelium in NERD patients: head to head comparison between light and electron microscopy analysis. Dig. Liver Dis. 41, 9–14 (2009).
Savarino, E. et al. Microscopic esophagitis distinguishes patients with non-erosive reflux disease from those with functional heartburn. J. Gastroenterol. http://dx.doi.org/10.1007/s00535-012-0672–2.
Vela, M. F., Craft, B. M., Sharma, N. & Hazen-Martin, D. Refractory heartburn: comparison of intercellular space diameter in documented GERD vs functional heartburn. Am. J. Gastroenterol. 106, 844–850 (2011).
Savarino, E. et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig. Liver Dis. 43, 542–547 (2011).
Venables, T. L. et al. Omeprazole 10 milligrams once daily, omeprazole 20 milligrams once daily, or ranitidine 150 milligrams twice daily, evaluated as initial therapy for the relief of symptoms of gastro-oesophageal reflux disease in general practice. Scand. J. Gastroenterol. 32, 965–973 (1997).
Dent, J. Microscopic esophageal mucosal injury in nonerosive reflux disease. Clin. Gastroenterol. Hepatol. 64, 1–8 (2007.
Farrè, R. et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut 59, 164–169 (2010).
Bredenoord, A. J. Mechanisms of reflux perception in gastroesophageal reflux disease: a review. Am. J. Gastroenterol. 107, 8–15 (2012).
Farrè, R. et al. Short exposure of oesophageal mucosa to bile acids, both in acidic and weakly acidic conditions, can impair mucosal integrity and provoke dilated intercellular spaces. Gut 57, 1366–1374 (2008).
Mastracci, L. et al. Microscopic esophagitis in gastro-esophageal reflux disease: individual lesions, biopsy sampling, and clinical correlations. Virchows Arch. 454, 31–39 (2009).
Vela, M. et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology 120, 1599–1606 (2001).
Fiocca, R. et al. Long-term outcome of microscopic esophagitis in chronic GERD patients treated with esomeprazole or laparoscopic antireflux surgery in the LOTUS trial. Am. J. Gastroenterol. 105, 1015–1023 (2010).
Galmiche, J. P. et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA 305, 1969–1977 (2011).
Fass, R. & Tougas, G. Functional heartburn: the stimulus, the pain, and the brain. Gut 51, 885–892 (2002).
Ang, D., Sifrim, D. & Tack, J. Mechanisms of heartburn. Nat. Clin. Pract. Gastroenterol. Hepatol. 5, 383–392 (2008).
Fass, R. et al. The effect of auditory stress on perception of intraesophageal acid in patients with gastroesophageal reflux disease. Gastroenterology 134, 696–705 (2008).
Thoua, N. M., Khoo, D., Kalantzis, C. & Emmanuel, A. V. Acid-related oesophageal sensitivity, not dismotility, differentiates subgroups of patients with non-erosive reflux disease. Aliment. Pharmacol. Ther. 27, 396–403 (2008).
Emerenziani, S., Ribolsi, M., Sifrim, D., Blondeau, K. & Cicala, M. Regional oesophageal sensitivity to acid and weakly acidic reflux in patients with non-erosive reflux disease. Neurogastroentrol. Motil. 21, 253–258 (2009).
Knowles, C. H. & Aziz, Q. Visceral hypersensitivity in non-erosive reflux disease. Gut 57, 674–683 (2008).
Bhat, Y. M. & Bielefeldt, K. Capsaicin receptor (TRPV1) and non-erosive reflux disease. Eur. J. Gastroenterol. Hepatol 18, 263–270 (2006).
Guarino, M. P. L. et al. Increased TRPV1 gene expression in esophageal mucosa of patients with non-erosive and erosive reflux disease. Neurogastroenterol. Motil. 22, 746–751, e219 (2010).
Waldmann, R. Proton-gated cation channels/neuronal acid sensors in the central and peripheral nervous system. Adv. Exp. Med. Biol. 502, 293–304 (2001).
Page, A. J. et al. Different contributions of ASIC channels 1a, 2 and 3 in gastrointestinal mechanosensory function. Gut 54, 1408–1415 (2005).
Cao, W. et al. Proinflammatory cytokines alter/reduce esophageal circular muscle contraction in experimental cat esophagitis. Am. J. Physiol. Gastrointest. Liver Physiol. 287, G1131–G1139 (2004).
Harnett, K. M., Rieder, F., Behar, J. & Biancani, P. Viewpoints on acid-induced inflammatory mediators in esophageal mucosa. J. Neurogastroenterol. Motil. 16, 374–388 (2010).
Schey, R. et al. Comparison of the different characteristics of sensed reflux events among different heartburn subgroups. J. Clin. Gastroenterol. 43, 699–704 (2009).
Chua, Y. C. & Aziz, Q. Perception of gastro-oesophageal reflux. Best Pract. Res. Clin. Gastroenterol. 24, 883–891 (2010).
Bredenoord, A. J., Weusten, B. L., Timmer, R. & Smout, A. J. Characteristics of gastro-esophageal reflux in symptomatic patients with and without excessive esophageal acid exposure. Am. J. Gastroenterol. 101, 2470–2475 (2006).
Tutuian, R. et al. Characteristics of symptomatic reflux episodes on acid suppressive therapy. Am. J. Gastroenterol. 103, 1090–1096 (2008).
Emerenziani, S. et al. Presence of gas in the refluxate enhances reflux perception in non-erosive patients with physiological acid exposure of the oesophagus. Gut 57, 443–447 (2008).
Sifrim, D. et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut 54, 449–454 (2005).
Tutuian, R., Mainie, I., Agrawal, A., Adams, D. & Castell, D. O. Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest 130, 386–391 (2006).
de Bortoli, N. et al. How many cases of laryngopharyngeal reflux suspected by laryngoscopy are gastroesophageal reflux disease-related? World J. Gastroenterol. 18, 4363–4370 (2012).
Malhotra, A., Freston, J. W. & Aziz, K. Use of pH-impedance testing to evaluate patients with suspected extraesophageal manifestations of gastroesophageal reflux disease. J. Clin. Gastroenterol. 42, 271–278 (2008).
Blondeau, K. et al. Gastro-oesophageal reflux and aspiration of gastric contents in adult patients with cystic fibrosis. Gut 57, 1049–1055 (2008).
Savarino, E. et al. Gastroesophageal reflux and pulmonary fibrosis in scleroderma: a study using pH-impedance monitoring. Am. J. Respir. Crit. Care Med. 179, 408–413 (2009).
Trimble, K. C., Pryde, A. & Heading, R. C. Lowered oesophageal sensory thresholds in patients with symptomatic but not excess gastro-oesophageal reflux: evidence for a spectrum of visceral sensitivity in GORD. Gut 37, 7–12 (1995).
Yang, M. et al. Quantitative assessment and characterization of visceral hyperalgesia evoked by esophageal balloon distension and acid perfusion in patients with functional heartburn, nonerosive reflux disease, and erosive esophagitis. Clin. J. Pain 26, 326–331 (2010).
Pehlivanov, N., Liu, J. & Mittal, R. K. Sustained esophageal contraction: a motor correlate of heartburn symptom. Am. J. Physiol. Gastrointest. Liver Physiol. 281, G743–G751 (2001).
Miner, P., Orr, W., Filippone, J., Jokubaitis, L. & Sloan, S. Rabeprazole in nonerosive gastroesophageal reflux disease: a randomized placebo-controlled trial. Am. J. Gastroenterol. 97, 1332–1339 (2002).
Van Pinxteren, B., Numans, M. E., Bonis, P. A. & Lau, J. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux-like symptoms and endoscopy-negative reflux disease. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD002095 http://dx/doi.org/10.1002/14651858.CD002095.pub2.
Savarino, V., Di Mario, F. & Scarpignato, C. Proton pump inhibitors in GORD. An overview of their pharmacology, efficacy and safety. Pharmacol. Res. 59, 135–153 (2009).
Dean, B. B., Gano, A. D., Knight, K. & Ofman, J. J., Fass, R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin. Gastroenterol. Hepatol. 2, 656–664 (2004).
Scarpignato, C. Poor effectiveness of proton pump inhibitors in non-erosive reflux disease: the truth in the end! Neurogastroenterol. Motil. 24, 697–704 (2012).
Weijenborg, P. W., Cremonini, F., Smout, A. J. & Bredenoord, A. J. PPI therapy is equally effective in well-defined non-erosive reflux disease and in reflux oesophagitis: a meta-analysis. Neurogastroenterol. Motil. 24, 747–757 (2012).
Savarino, E., Zentilin, P. & Savarino, V. It is time to plan clinical trials on true NERD patients. Neurogastroenterol. Motil. 24, 885–886 (2012).
Mandel, K. G., Daggy, B. P., Brodie, D. A. & Jacoby, H. I. Review article: alginate-raft formulations in the treatment of heartburn and acid reflux. Aliment. Pharmacol. Ther. 14, 669–690 (2000).
Giannini, E. G. et al. A comparison between sodium alginate and magaldrate anhydrous in the treatment of patients with gastroesophageal reflux symptoms. Dig. Dis. Sci. 51, 1904–1909 (2006).
Savarino, E. et al. Alginate controls heartburn in patients with erosive and nonerosive reflux disease. World J. Gastroenterol. 18, 4371–4378 (2012).
Ekenved, G. & Walan, A. In vivo studies on the neutralizing effect of antacids using the Heidelberg capsule. Scand. J. Gastroenterol. 10, 267–272 (1975).
Taylor, G., Warren, S. J., Kelleway, I. W., Patel, B. & Little, S. L. Gastric residence of Gaviscon Advance and Liquid Gaviscon in healthy volunteers. J. Pharm. Pharmacol. 49 (Suppl. 4), 73–79 (1997).
Zentilin, P. et al. An evaluation of the antireflux properties of sodium alginate by means of combined multichannel intraluminal impedance and pH-metry. Aliment. Pharmacol. Ther. 21, 29–34 (2005).
Carlsson, R. et al. Gastro-oesophageal reflux disease in primary care: an international study of different treatment strategies with omeprazole—International GORD Study Group. Eur. J. Gastroenterol. Hepatol. 10, 119–124 (1998).
Talley, N. J. et al. Esomeprazole 20 mg maintains symptom control in endoscopy-negative gastro-oesophageal reflux disease: a controlled trial of “on demand” therapy for 6 months. Aliment. Pharmacol. Ther. 15, 347–354 (2001).
Tsai, H. H. et al. Esomeprazole 20 mg on-demand is more acceptable to patients than continuous lansoprazole 15 mg in the long-term maintenance of endoscopy-negative gastro-oesophageal reflux patients: the COMMAND study. Aliment. Pharmacol. Ther. 20, 657–665 (2004).
Metz, D. C., Inadomi, J. M., Howden CW, van Zanten, S. J. & Bytzer, P. On-demand therapy for gastro-esophageal reflux disease. Am. J. Gastroenterol. 102, 642–653 (2007).
Viazis, N. et al. Selective serotonin reuptake inhibitors for the treatment of hypersensitive esophagus: a randomized, double-blind, placebo-controlled study. Am. J. Gastroenterol. 107, 1662–1667 (2012).
Fenton, P. et al. Is there a role for laparoscopic fundoplication in patients with non-erosive reflux disease (NERD) [Abstract]? Gastroenterology 118 (Suppl. 2), A481 (2000).
Mainie, I., Tutuian, R., Agrawal, A., Adams, D. & Castell, D. O. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br. J. Surg. 93, 1483–1487 (2006).
Broeders, J. A. et al. Oesophageal acid hypersensitivity is not a contraindication to Nissen fundoplication. Br. J. Surg. 96, 1023–1030 (2009).
Frazzoni, M., Conigliaro, R. & Melotti, G. Reflux parameters as modified by laparoscopic fundoplication in 40 patients with heartburn/regurgitation persisting despite PPI therapy. A study using impedance pH monitoring. Dig. Dis. Sci. 56, 1099–1106 (2011).
Broeders, J. A. et al. Effects of anti-reflux surgery on weakly acidic reflux and belching. Gut 60, 435–41 (2011).
Bredenoord, A. J., Draaisma, W. A., Weusten, B. L., Gooszen, H. G. & Smout, A. J. Mechanisms of acid, weakly acidic and gas reflux after anti-reflux surgery. Gut 57, 161–166 (2008).
Koch, O. O. et al. Subjective and objective data on esophageal manometry and impedance pH monitoring 1 year after endoscopic full-thickness plication for the treatment of GERD by using multiple Plicator implants. Gastrointest. Endosc. 77, 7–14 (2013).
Vela, M. F. et al. Baclofen decreases acid and non-acid post-prandial gastro-oesophageal reflux measured by combined multichannel intraluminal impedance and pH. Aliment. Pharmacol. Ther. 17, 243–251 (2003).
Grover, M. & Drossmann, D. A. Psychopharmacologic and behavorial treatments for functional gastrointestinal disorders. Gastrointest. Endosc. Clin. N. Am. 19, 151–170 (2009).
Blaga, T. S., Dumitrascu, D., Galmiche, J. P. & Bruley des Varannes, S. Functional heartburn: clinical characteristics and outcome. Eur. J. Gastroenterol. Hepatol. http://dx.doi.org/10.10977/MEG.0b013e32835b108f.
Lee, H. et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am. J. Gastroenterol. 105, 1504–1512 (2010).
Prakash, C. & Clouse, R. E. Long-term outcome from tricyclic antidepressant treatment of functional chest pain. Dig. Dis. Sci. 44, 2373–2379 (1999).
Varia, I. & Logue, E., O'Connor, C. et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am. Heart J. 140, 367–372 (2000).
Author information
Authors and Affiliations
Contributions
All authors equally contributed to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Savarino, E., Zentilin, P. & Savarino, V. NERD: an umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol 10, 371–380 (2013). https://doi.org/10.1038/nrgastro.2013.50
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2013.50
This article is cited by
-
Update: Benigne Erkrankungen der Speiseröhre
MMW - Fortschritte der Medizin (2022)
-
Clinical use of mean nocturnal baseline impedance and post-reflux swallow-induced peristaltic wave index for the diagnosis of gastro-esophageal reflux disease
Esophagus (2022)
-
Efficacy of different endoscopic treatments in patients with gastroesophageal reflux disease: a systematic review and network meta-analysis
Surgical Endoscopy (2021)
-
Gastroösophageale Refluxerkrankung
Der Gastroenterologe (2020)
-
Erosive Esophagitis and Symptoms of Gastroesophageal Reflux Disease in Patients with Morbid Obesity with and without Type 2 Diabetes: a Cross-sectional Study
Obesity Surgery (2020)