Abstract
In this paper, we aim to emphasise the need for a more comprehensive and tailored approach to manage the broad nature of non-adherence, to personalise current asthma management. Although currently several methods are available to measure the extent of asthma patients’ adherence, the vast majority do not incorporate confirmation of the actual inhalation, dose and inhalation technique. Moreover, most current measures lack detailed information on the individual consequences of non-adherence and on when and how to take action if non-adherence is identified. Notably, one has to realise there are several forms of non-adherence (erratic non-adherence, intelligent non-adherence and unwitting non-adherence), each requiring a different approach. To improve asthma management, more accurate methods are needed that integrate measures of non-adherence, asthma disease control and patient preferences. Integrating information from the latest inhaler devices and patient-reported outcomes using mobile monitoring- and feedback systems (‘mHealth’) is considered a promising strategy, but requires careful implementation. Key issues to be considered before large-scale implementation include patient preferences, large heterogeneity in patient and disease characteristics, economic consequences, and long-term persistence with new digital technologies.
Similar content being viewed by others
Introduction
A key driver for asthma treatment success is the extent to which patients adhere to their prescribed pharmacological regimen.1 Good adherence encompasses multiple dimensions, including intensity and timing of use according to prescription (compliance), continuous use (persistence) and correct use (inhalation technique).2,3 Non-adherence to asthma medication is associated with poor clinical, humanistic and economic outcomes.4–6 Previous studies showed that adherence to asthma medications on average is far from optimal. Depending on methods, population and setting, estimates of non-adherence typically range between 30 and 75% in both adults and children.7,8 Current methods to measure medication adherence include direct biochemical measurement, clinician judgment, self-report, assessment of prescription refill data and the use of electronic devices.8,9 These methods all have their advantages and disadvantages. However, an important limitation that most methods share is that they do not incorporate confirmation of actual inhalation, dose and inhalation technique. Furthermore, most methods fail to provide detailed information on the individual consequences of non-adherence and on when and how to take action if non-adherence is identified. Therefore, more accurate methods are required that integrate measures of the broad nature of non-adherence and essential elements of asthma control. Combining patient-reported outcomes with the latest inhalation-, adherence monitoring- and feedback systems offers a promising new strategy.
The aim of this paper is to assess the value of current asthma adherence measures in relation to the management of diverse types of non-adherence, levels of asthma control and patient preferences and engagement. Subsequently, a more comprehensive non-adherence-managing approach is proposed and discussed.
Identification of papers
To identify relevant papers, a semi-structured search in Pubmed and Cochrane was performed with several combinations of the following search terms: adherence, asthma, inhalers, mobile phone and electronic monitoring. Papers deemed relevant were studied, and additional papers were retrieved through searching the references.
The broad nature of asthma non-adherence
In the management of asthma, good understanding of the diversity and complexity of patient adherence is required.2 As such, the World Health Organization has defined three types of non-adherence: erratic non-adherence, intelligent non-adherence and unwitting non-adherence.2
Currently, the terms intentional and unintentional non-adherence are also commonly used.10
Erratic non-adherence
Erratic non-adherence is probably the most well-known type of non-adherence. This form of unintentional non-adherence is often referred to as forgetfulness.2 Patients have the intention to be as adherent as possible, but simply cannot combine the medication regimen with their busy daily life.
Intelligent non-adherence
A patient with ‘intelligent’, or intentional, non-adherence, purposely alters, discontinues, or even fails to initiate prescribed therapy. This deliberate non-adherence reflects a reasoned choice, albeit not necessarily a wise one.2 Patients who ‘feel’ better may decide that they no longer need to take their medications, i.e., their illness perception has an important role.11 A number of factors may be responsible: fear of perceived short- or long-term side effects; taste; complexity; interference with daily life; cost; disagreement with provider regarding need. All these factors may cause patients to choose to avoid daily therapy.2,11
Unwitting non-adherence
Another form of unintentional non-adherence is unwitting non-adherence. Unwitting non-adherence is the failure to understand fully either the specifics of the regimen or the necessity for adherence.2 Unwitting non-adherent patients make no intentional decision to be non-adherent. Studies have repeatedly confirmed that patients frequently forget instructions given to them during a clinic visit.12 In asthma management, it is common for patients to misunderstand the difference between ‘as needed’ medication and maintenance medication. Another example of common ‘unwitting non-adherence’ is poor inhaler technique.3,13,14
Managing non-adherence in asthma: not simply one-size fits-all
Most of the erratic non-adherent patients could be helped by straightforward interventions such as simplification of the dosing regimen, electronic reminders, or the advice to link the intake of medication to a daily habit.2 In contrast, patients that are intelligent non-adherent do not need any reminders, but may be more likely to benefit from a process of shared decision making and motivational interviewing.15 Finally, unwitting non-adherent patients are expected to benefit from extra education.9 For this purpose, self-management and written action plans have been widely recommended in international and many national guidelines.16,17 The effectiveness of these plans has been proven;18 however, uptake of written action plans is still suboptimal.19,20 In addition, there is room for improvement of the specific elements impacting effectiveness of these plans, especially regarding suitability in patients with limited literacy.21 Patients with poor inhalation technique would be helped by more information and training to enhance their skills regarding inhaler use. Thereby it should be mentioned that training and education on inhalation technique have to be provided by well-trained healthcare professionals. Notably, some studies suggest that there is ample room for improvement regarding medical personnel’s knowledge on inhalation devices.22,23
Detecting specific types of non-adherence in asthma: current limitations
To aid the healthcare provider in detecting and assessing asthma patients’ adherence, several methods are available. Most commonly used methods include direct biochemical measurement (e.g., in blood or other body fluids), judgment of healthcare providers, patient self-report, assessment of prescription refill data, and the use of electronic monitoring devices.8,9 In general, the specific value of the current measurement methods regarding detecting and managing erratic non-adherence, intelligent non-adherence and unwitting non-adherence has been under-reported, but is considered a key issue for optimal management and outcomes. For example, erratic non-adherence often remains unnoticed until exacerbations occur.5 Intelligent non-adherence may be detected during patient interviews with a healthcare provider, given that the patient is willing to share his concerns.10 However, the topic is often only covered substantially in the consultation room once it is too late (e.g., after severe exacerbations). Another possibility to detect intelligent non-adherence is by the use of validated self-report instruments such as the MARS-A questionnaire.24 Yet, asking the patient might result in a ‘socially acceptable answer’ and thereby an overestimation of actual adherence.25,26 Unwitting non-adherence, e.g., a poor inhalation technique, might be diagnosed by a healthcare provider observing the patient, but usually there would need to be another reason for consultation first. Although guidelines highlight the importance of regular inhalation technique assessment as part of every asthma review, real-life practice often falls short.17,27 Currently, patients themselves cannot rely on valid instruments to assess the quality of their inhalation.
The value of current methods regarding the three types of non-adherence and other aspects is compared and summarised in Table 1. For a more extensive comparison, we refer to previous reviews that compared adherence measurement methods in asthma.8,9,28 Table 1 was the result of thorough assessment of these previous reviews and a final consensus between the authors of this article.
Direct biochemical measurement is an unbiased method to assess actual intake, but is costly and invasive and only provides a point estimate of adherence.9,28 In-depth patient interviews by a healthcare provider can provide insight in most types of non-adherent behaviour, yet they require regular face-to-face meetings and effective patient–provider communication to obtain a continuous measure.10,29 Longitudinal measurement of adherence by prescription refills provides a continuous and remotely accessible alternative.28 However, this method of measuring adherence lacks discriminative properties regarding the three types of non-adherence and cannot detect a poor inhalation technique.
In general, most methods routinely used fail to take into account the interaction between different forms of non-adherence and variations in asthma control, thereby wasting the opportunities for tailored, proactive interventions. In conclusion, each of the current methods available has its strengths, but none of the methods are optimal for tailored asthma non-adherence management.
Optimising adherence assessment in asthma: requirements
Without disregarding the value of a good initial diagnosis and the wide availability of a basic level of asthma care, the limitations described in the previous section demonstrate the need for an integrated, personal, approach to deal with the broad nature of asthma non-adherence. This approach needs to take into account not only the type of non-adherence, but also patient preferences and asthma control (Figure 1). In our view, this requires the digital integration of the latest inhalation technology and asthma control monitoring tools in a patient-preference-based environment.
Detection of non-adherence
Ideally, non-adherence detection aids will provide us with both a qualitative measure of adherence (e.g., inhaler handling and inhalation technique) and a continuous, quantitative measure to detect all types of non-adherence. The quantitative measure includes the frequency, hour of the day and time interval between inhalations. Electronic monitoring devices, attached or integrated in inhalation devices, appear the most promising to capture both aspects.30 These electronic devices have been recommended as the reference standard to assess medication adherence in both research and real-world clinical settings.31 Technically, these devices have shown their feasibility and some have been available on the healthcare market for almost 20 years, although they are still primarily used in small-scale research settings.32 Examples of monitoring devices that are able to log the date and time of actuations are the SmartMist, Doser CT, MDIlog and the Nebulizer Chronolog, of which studies demonstrated that all devices were sufficiently accurate.33,34 A more recent development is the Propeller Health sensor that not only keeps a record of time and date, but also of location of use.35 Another development is the Smartinhaler that automatically sends usage data to a mobile application or computer via Bluetooth and can provide discreet audio-visual reminders if the patient forgets to take the prescribed medication.36 Yet, all devices still do not assess the quality of inhalation. A promising new technique relies on the use of acoustic inhalation measurements. In research settings, time-stamped acoustic recordings seem to be a suitable method for monitoring inhalation technique over time.32,37 Interestingly, an association between better adherence and changes in asthma quality of life and peak expiratory flow was only found when adherence was operationalised as both time of use and inhalation technique, and not for time of use only.32 These developments illustrate that some of the technology to introduce an electronic monitoring component within asthma management is already available.
Asthma control
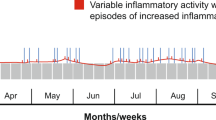
Two of the most frequently used health status tools to measure asthma control are the Asthma Control Questionnaire (ACQ-6) and the Asthma Control Test.38,39 In current clinical practice, these tools are only occasionally used, most often during regular patient consultations. Interventions following from these asthma control scores are generally reactive. In contrast, continuous digital monitoring of asthma control would enable early detection of increasing symptoms and proactive interventions. Theoretically, whenever ACQ/Asthma Control Test scores exceed a certain threshold (based on previous scores and preferences), alerts and decision support could be sent to the patient and/or healthcare provider. Subsequently, initial remote assessment of the patient (e-consultations) could be performed, only followed by active in-person consultation if deemed relevant. In stable periods, no consultations would be needed, even when non-adherence is signalled. First results from studies assessing e-consultations showed that patients were satisfied with an e-consultation process,40 but research is still very limited and no specific studies in asthma have been performed. Therefore, more studies are obviously necessary before large-scale implementation should take place.
Patient preferences
The asthma population is very heterogeneous regarding its needs, preferences and capabilities.41 For example, patients with low health literacy and self-management ability may need a different approach, especially as these aspects are associated with worsened outcomes.42,43 Also patients’ current use and preferences towards mobile phone-based management may have a role in both uptake and effectiveness of this digital strategy. In renal transplant recipients, 79% showed a positive attitude towards mobile phone-based adherence and health monitoring, but their attitude was positively influenced by smartphone ownership.44 In asthma, disease severity and comorbidities may influence patients’ preferences and abilities for more or less self-care.45 A cross-sectional study indicated that about 60% of the asthma patients preferred an active or collaborative role in treatment decisions and 40% a passive role, regardless of disease severity.46 As regards this heterogeneity, a three-point approach to enhance patients’ motivation and to optimise outcomes has been suggested.47 This approach includes counselling on the necessity of asthma medication, addressing patients’ concerns about medication, and tailoring the choice of the treatment regimen to patients’ preferences and capacities.
In addition, the possibility for asthma patients to interact with their peer patients may be beneficial. Peer-to-peer contact has been shown to improve self-efficacy and asthma control with favourable cost-effectiveness; however, studies are limited.48–50 Finally, acceptance of digital asthma health care, in particular, depends on age, duration of disease, education and use of computers/Internet.51
The concept of integrating adherence measurement, asthma control and patient preferences
Developments in inhalation technology and digital asthma control measurement are promising. These technologies offer the potential to enhance adherence and tailor asthma management, that could result in improved quality of life and reduced healthcare utilisation.3,4,52,53 However, to achieve optimal intervention uptake and effect size, careful conceptualisation of the design is essential. Ideally, adherence measurements of electronic inhalation devices are directly transferred to an mHealth platform on a mobile phone. First, this will provide patients with real-time insight in their own medication-taking behaviour, but second, these data can be extracted during regular consultations with their healthcare providers. It is unlikely that the healthcare provider will be monitoring these signals on a daily basis, but the server could be set up to issue alarms, should control fall outside of certain preset levels. The information gathered would help in the performance of the next structured asthma review. In this context, such a system could fall under M for Monitoring in SIMPLES or under S for Support.54 Integrating information regarding the timing and quality of inhalations with patient-reported outcomes has the potential to provide the full picture; that is, it may be able to signal patterns regarding forms of non-adherence and subsequent poor asthma control. On the basis of these observations, personalised treatment and recommendations can be provided, depending on patients’ needs. For some patients, automatically generated, but tailored, feedback by decision-aid systems may be sufficient. For other patients, however, direct in-person and digital consultations are required for optimal patient-centred care, education and outcomes. In addition, the digital platform will allow patients to interact with their peers. It may also serve as a place where healthcare providers can provide general treatment and lifestyle recommendations, given that patient confidentiality is always taken into account.
A global outline of this approach is visualised in Figure 2. It includes the use of a smartinhaler combined with a mobile phone application to measure adherence and asthma control, tailored decision support and motivational feedback, and optional digital or direct face-to-face contacts with healthcare providers and/or peer patients. As depicted, several opportunities for tailored asthma management are offered, depending on patients’ and healthcare providers’ needs and preferences (more self-management or more guidance by healthcare providers) and feasibility studies.
Optimising adherence assessment in asthma: considerations
This integrated approach seems promising and fits well with the current movement towards personalised, predictive, preventive and participatory respiratory medicine (‘P4 medicine’).55 Yet, an important barrier to innovation is that technologies such as these are often considered to be too costly.56 Regarding the innovative technology itself, it is expected that product costs will rapidly decrease over time.30 Less predictable, however, are the economic consequences of this potential shift from primarily ‘scheduled’ chronic care to future ‘on-demand’ care. It is likely that face-to-face consultations would reduce as the patients learnt better how to control their disease.57 It is, however, unclear whether this would also lead to fewer hospitalisations. Therefore, careful analysis of current chronic digital asthma care is necessary. A review by Huckvale et al.58 systematically assessed the content of 103 asthma apps and compared the contents to international guidelines and best practices. The authors concluded that none of the different apps combined reliable information about asthma with supportive tools for self-management. A recent Cochrane review reported on the effectiveness and cost-effectiveness of digital apps for asthma self-management and found that the current evidence is not sufficient to advise large-scale implementation.59
Long-term adherence to these technologies is one of the other issues that should be taken into account. A study from 2004 suggested that patients used an asthma-monitoring website only for a limited amount of time.60 Note that this study was performed in times before the smartphone era. A more recent study, by van Gaalen et al.,61 did indeed show persistence of effect in the intervention group. Evidence of the economic dimension of more comprehensive digital asthma management tools suggest neutral to unfavourable cost-effectiveness, but evidence is limited and highly dependent on implementation and current technology costs.57,62
The question rises whether this technology should be restricted to selected populations. Should we for instance focus on the mild asthma population, in whom fewer in-person contacts may be safe, or should we focus on the persistent asthma population, where disease burden and costs are highest? Another possibility is that these technologies become an integrated part of the medication, just as is currently the case with existing inhaler devices. Manufacturers would not only provide the pharmacological component, but also the technology to assist patients and healthcare providers in optimising asthma disease management. Especially in the current era of limited major pharmacological breakthroughs but a wealth of new inhalers available, the provision of these kinds of services may significantly increase the added value of manufacturers and make them stand out from the rest. Other issues that need to be addressed include privacy issues, data ownership, and digital competences of patients and healthcare providers.
In general, the most successful telemonitoring implementations have occurred when all of the basics (including sample size, intervention, duration of follow-up and definition of outcomes) have been done properly and monitoring is integrated into a system that is ready to receive it.63 However, these systems are much less likely to have a positive impact unless all the other prerequisites are in place, which is why so many telemonitoring trials fail to demonstrate benefit. When used as part of an integrated pathway,64 mHealth support has the opportunity to improve asthma outcomes, but more research regarding optimal implementation is highly required.
Conclusion
Current measures to assess asthma non-adherence do not provide sufficient information. More targeted and personalised methods, combining measures of non-adherence, asthma control and patient preferences are needed. Mobile monitoring systems offer a promising integrated approach to assess (non)-adherence and optimise asthma management, but require careful implementation.
References
Heaney LG, Horne R . Non-adherence in difficult asthma: time to take it seriously. Thorax 2012; 67: 268–270.
World Health Organization Adherence to long-term therapies—evidence for action 2003. http://apps.who.int/medicinedocs/pdf/s4883e/s4883e.pdf (Accessed 20 November 2014).
Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011; 105: 930–938.
Murphy AC, Proeschal A, Brightling CE, Wardlaw AJ, Pavord I, Bradding P et al. The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax 2012; 67: 751–753.
Williams LK, Pladevall M, Xi H, Peterson EL, Joseph C, Lafata JE et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol 2004; 114: 1288–1293.
Bender BG, Rand C . Medication non-adherence and asthma treatment cost. Curr Opin Allergy Clin Immunol 2004; 4: 191–195.
Morton RW, Everard ML, Elphick HE . Adherence in childhood asthma: the elephant in the room. Arch Dis Child 2014; 99: 949–953.
Rand CS, Wise RA . Measuring adherence to asthma medication regimens. Am J Respir Crit Care Med 1994; 149: S69–S76, discussion S77-S78.
Sumino K, Cabana MD . Medication adherence in asthma patients. Curr Opin Pulm Med 2013; 19: 49–53.
Horne R . Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130: 65S–72S.
Charles C, Ninot G, Sultan S . Patients' illness perceptions and adherence to treatment with inhaled corticosteroids in asthma. Rev Mal Respir 2011; 28: 626–635.
DiMatteo MR . Enhancing patient adherence to medical recommendations. JAMA 1994; 271: 79.
Levy ML, Hardwell A, McKnight E, Holmes J . Asthma patients' inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the global initiative for asthma (GINA) strategy: a retrospective analysis. Prim Care Respir J 2013; 22: 406–411.
Hardwell A, Barber V, Hargadon T, McKnight E, Holmes J, Levy ML . Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J 2011; 20: 92–96.
Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med 2010; 181: 566–577.
British Thoracic Society/Scottish Intercollegiate Guideline Network. British guideline on the management of asthma. http://www.sign.ac.uk (Accessed 10 February 2015).
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. http://www.ginasthma.org (Accessed 30 October 2014).
Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2003; (1): CD001117.
Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011; 85: e131–e143.
Wiener-Ogilvie S, Pinnock H, Huby G, Sheikh A, Partridge MR, Gillies J . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16: 369–377.
Yin HS, Gupta RS, Tomopoulos S, Wolf MS, Mendelsohn AL, Antler L et al. Readability, suitability, and characteristics of asthma action plans: examination of factors that may impair understanding. Pediatrics 2013; 131: e116–e126.
Hanania NA, Wittman R, Kesten S, Chapman KR . Medical personnel's knowledge of and ability to use inhaling devices. Metered-dose inhalers, spacing chambers, and breath-actuated dry powder inhalers. Chest 1994; 105: 111–116.
Fink JB, Rubin BK . Problems with inhaler use: a call for improved clinician and patient education. Respir Care 2005; 50: 1360–1374, discussion 1374–1375.
Cohen JL, Mann DM, Wisnivesky JP, Home R, Leventhal H, Musumeci-Szabo TJ et al. Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: the Medication Adherence Report Scale for Asthma. Ann Allergy Asthma Immunol 2009; 103: 325–331.
Patel M, Perrin K, Pritchard A, Williams M, Wijesinghe M, Weatherall M et al. Accuracy of patient self-report as a measure of inhaled asthma medication use. Respirology 2013; 18: 546–552.
Osterberg L, Blaschke T . Adherence to medication. N Engl J Med 2005; 353: 487–497.
Corrigan CJ . Asthma therapy: there are guidelines, and then there is real life. Prim Care Respir J 2011; 20: 13–14.
Jentzsch NS, Camargos PA . Methods of assessing adherence to inhaled corticosteroid therapy in children and adolescents: adherence rates and their implications for clinical practice. J Bras Pneumol 2008; 34: 614–621.
Heiner MM . Key barriers to optimal management of adult asthma in Australia: physician and patient perspectives. Curr Med Res Opin 2007; 23: 1799–1807.
Chan AH, Reddel HK, Apter A, Eakin M, Riekert K, Foster JM . Adherence monitoring and e-health: how clinicians and researchers can use technology to promote inhaler adherence for asthma. J Allergy Clin Immunol Pract 2013; 1: 446–454.
Patel M, Pilcher J, Travers J, Perrin K, Shaw D, Black P et al. Use of metered-dose inhaler electronic monitoring in a real-world asthma randomized controlled trial. J Allergy Clin Immunol Pract 2013; 1: 83–91.
D'Arcy S, MacHale E, Seheult J, Holmes MS, Hughes C, Sulaiman I et al. A method to assess adherence in inhaler use through analysis of acoustic recordings of inhaler events. PLoS One 2014; 9: e98701.
Julius SM, Sherman JM, Hendeles L . Accuracy of three electronic monitors for metered-dose inhalers. Chest 2002; 121: 871–876.
Gong H Jr, Simmons MS, Clark VA, Tashkin DP . Metered-dose inhaler usage in subjects with asthma: comparison of Nebulizer Chronolog and daily diary recordings. J Allergy Clin Immunol 1988; 82: 5–10.
Propeller Health. http://www.propellerhealth.com (Accessed 8 December 2014).
Smartinhaler. http://www.smartinhaler.com (Accessed 8 December 2014).
Seheult JN, O'Connell P, Tee KC, Bholah T, Al Bannai H, Sulaiman I et al. The acoustic features of inhalation can be used to quantify aerosol delivery from a Diskus dry powder inhaler. Pharm Res 2014; 31: 2735–2747.
Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR . Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999; 14: 902–907.
Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004; 113: 59–65.
Rodriguez KL, Burkitt KH, Bayliss NK, Skoko JE, Switzer GE, Zickmund SL et al. Veteran, primary care provider, and specialist satisfaction with electronic consultation. JMIR Med Inform 2015; 3: e5.
Thomas M . Why aren't we doing better in asthma: time for personalised medicine? NPJ Prim Care Respir Med 2015; 25: 15004.
Wisnivesky JP, Krauskopf K, Wolf MS, Wilson EA, Sofianou A, Martynenko M et al. The association between language proficiency and outcomes of elderly patients with asthma. Ann Allergy Asthma Immunol 2012; 109: 179–184.
Talreja N, Soubani AO, Sherwin RL, Baptist AP . Modifiable factors associated with severe asthma exacerbations in urban patients. Ann Allergy Asthma Immunol 2012; 109: 128–132.
McGillicuddy JW, Weiland AK, Frenzel RM, Mueller M, Brunner-Jackson BM, Taber DJ et al. Patient attitudes toward mobile phone-based health monitoring: questionnaire study among kidney transplant recipients. J Med Internet Res 2013; 15: e6.
Joubert A, Kidd-Taylor A, Christopher G, Nanda J, Warren R, Lindong I et al. Complementary and alternative medical practice: self-care preferred vs. practitioner-based care among patients with asthma. J Natl Med Assoc 2010; 102: 562–569.
Caress AL, Beaver K, Luker K, Campbell M, Woodcock A . Involvement in treatment decisions: what do adults with asthma want and what do they get? Results of a cross sectional survey. Thorax 2005; 60: 199–205.
Ostrem A, Horne R . Reducing asthma attacks: consider patients' beliefs. NPJ Prim Care Respir Med 2015; 25: 15021.
Shah S, Peat JK, Mazurski EJ, Wang H, Sindhusake D, Bruce C et al. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. BMJ 2001; 322: 583–585.
Rhee H, McQuillan BE, Belyea MJ . Evaluation of a peer-led asthma self-management program and benefits of the program for adolescent peer leaders. Respir Care 2012; 57: 2082–2089.
Rhee H, Pesis-Katz I, Xing J . Cost benefits of a peer-led asthma self-management program for adolescents. J Asthma 2012; 49: 606–613.
Duplaga M . The acceptance of e-health solutions among patients with chronic respiratory conditions. Telemed J E Health 2013; 19: 683–691.
Harnett CM, Hunt EB, Bowen BR, O'Connell OJ, Edgeworth DM, Mitchell P et al. A study to assess inhaler technique and its potential impact on asthma control in patients attending an asthma clinic. J Asthma 2014; 51: 440–445.
Horner SD, Brown A . Evaluating the effect of an asthma self-management intervention for rural families. J Asthma 2014; 51: 168–177.
Ryan D, Murphy A, Stallberg B, Baxter N, Heaney LG . 'SIMPLES': a structured primary care approach to adults with difficult asthma. Prim Care Respir J 2013; 22: 365–373.
Agusti A, Anto JM, Auffray C, Barbe F, Barreiro E, Dorca J et al. Personalized respiratory medicine: exploring the horizon, addressing the issues. Summary of a BRN-AJRCCM workshop held in Barcelona on June 12, 2014. Am J Respir Crit Care Med 2015; 191: 391–401.
Bender BG . Advancing the science of adherence measurement: implications for the clinician. J Allergy Clin Immunol Pract 2013; 1: 92–93.
Ryan D, Price D, Musgrave SD, Malhotra S, Lee AJ, Ayansina D et al. Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: multicentre randomised controlled trial. BMJ 2012; 344: e1756.
Huckvale K, Car M, Morrison C, Car J . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10: 144.
Marcano Belisario JS, Huckvale K, Greenfield G, Car J, Gunn LH . Smartphone and tablet self management apps for asthma. Cochrane Database Syst Rev 2013; 11: CD010013.
Anhoj J, Nielsen L . Quantitative and qualitative usage data of an Internet-based asthma monitoring tool. J Med Internet Res 2004; 6: e23.
van Gaalen JL, Beerthuizen T, van der Meer V, van Reisen P, Redelijkheid GW, Snoeck-Stroband JB et al. Long-term outcomes of internet-based self-management support in adults with asthma: randomized controlled trial. J Med Internet Res 2013; 15: e188.
van der Meer V, van den Hout WB, Bakker MJ, Rabe KF, Sterk PJ, Assendelft WJ et al. Cost-effectiveness of Internet-based self-management compared with usual care in asthma. PLoS One 2011; 6: e27108.
Rice KL, Dewan N, Bloomfield HE, Grill J, Schult TM, Nelson DB et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med 2010; 182: 890–896.
European Innovation Partnership on Active and Healthy Ageing, Action Plan B3 Mechanisms of the Development of Allergy, WP 10 Global Alliance against Chronic Respiratory Diseases, Bousquet J, Addis A, Adcock I et al. Integrated care pathways for airway diseases (AIRWAYS-ICPs). Eur Respir J 2014; 44: 304–323.
Acknowledgements
Funding
The authors declare that no funding was received.
Author information
Authors and Affiliations
Contributions
NHC and JFMvB designed the study. JFMvB drafted the first version of the manuscript. JFMvB and JCAT drafted the figures. JCAT, TvdM and NHC commented on the first draft and provided input for the final manuscript. NHC and TvdM supervised the overall progress and provided final revision, comments and review.
Corresponding author
Ethics declarations
Competing interests
NHC is an Associate Editor of npj Primary Care Respiratory Medicine, but was not involved in the editorial review of, nor the decision to publish, this article. The other authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
van Boven, J., Trappenburg, J., van der Molen, T. et al. Towards tailored and targeted adherence assessment to optimise asthma management. npj Prim Care Resp Med 25, 15046 (2015). https://doi.org/10.1038/npjpcrm.2015.46
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2015.46
This article is cited by
-
Electronic Monitoring Devices to Support Inhalation Technique in Patients with Asthma: a Narrative Review
Current Treatment Options in Allergy (2023)
-
Understanding relationships between asthma medication use and outcomes in a SABINA primary care database study
npj Primary Care Respiratory Medicine (2022)
-
Digital Inhalers for Asthma or Chronic Obstructive Pulmonary Disease: A Scientific Perspective
Pulmonary Therapy (2021)
-
Primary non-adherence to inhaled medications measured with e-prescription data from Poland
Clinical and Translational Allergy (2020)
-
Effectiveness and success factors of educational inhaler technique interventions in asthma & COPD patients: a systematic review
npj Primary Care Respiratory Medicine (2017)