Abstract
The incidence of columnar cell lesions in breast core needle biopsies since full-field digital mammography in comparison with screen-filmed mammography was analyzed. As tiny microcalcifications characterize columnar cell lesions at mammography, we hypothesized that more columnar cell lesions are diagnosed since full-field digital mammography due to its higher sensitivity for microcalcifications. In all, 3437 breast core needle biopsies performed in three hospitals and resulting from in total 55 159 mammographies were revised: 1424 taken in the screen-filmed mammography and 2013 in the full-field digital mammography period. Between the screen-filmed mammography and full-field digital mammography periods, we compared the proportion of mammographies that led to core needle biopsies, the mammographic indication for core needle biopsies (density, microcalcifications, or both) and the proportion of columnar cell lesions with or without atypia. The columnar cell lesions were graded according to Schnitt, and we included atypical ductal hyperplasia arising in the context of columnar cell lesions. Proportions were compared using χ2 tests and prevalence ratios were adjusted for age and hospital. We found that more core needle biopsies per mammogram were taken in the full-field digital mammography period (7.6%) compared with the screen-filmed mammography period (5.0%, P<0.0001). Microcalcifications were more often diagnosed with full-field digital mammography than with screen-filmed mammography (adjusted prevalence ratio: 1.14, confidence interval 95%: 1.01–1.28). Core needle biopsies from the full-field digital mammography era showed more columnar cell lesions (10.8%) than those from the screen-filmed mammography era (4.9%; adjusted prevalence ratio: 1.93, confidence interval 95%: 1.48–2.51), particularly due to more columnar cell lesions without atypia (8.2% respectively 2.8%) while the proportion of columnar cell lesions with atypia remained nearly constant (2.0 vs 2.6%). In conclusion, since the implementation of full-field digital mammography, more microcalcifications are seen at mammography, more often resulting in core needle biopsies, which especially yields more columnar cell lesions without atypia.
Similar content being viewed by others
Main
Over the decade, columnar cell lesions of the breast have gained interest as possibly premalignant lesions. However, the clinical significance of columnar cell lesions is not well known. Many alternate names have been used to describe these lesions, such as flat epithelial atypia,1 columnar cell alterations with apical snouts and secretions with atypia,2 enlarged lobular units with columnar alteration,3 atypical cystic lobules,4 ductal intraepithelial neoplasia flat type,5 atypical cystic ducts,6 and clinging carcinoma monomorphic type.7
Columnar cell lesions are enlarged terminal duct lobular units lined by columnar type epithelial cells, often with luminal secretions and tiny microcalcifications. Columnar cell lesions differ with respect to the degree of architectural and/or cytonuclear atypia, ranging from no atypia to columnar cell lesions with atypia, toward almost low-grade ductal carcinoma in situ.8
Many studies have shown that there is an association between the presence of columnar cell lesions and ductal carcinoma in situ, atypical ductal hyperplasia or lobular neoplasia, and low-grade luminal type invasive carcinomas like tubular and lobular carcinomas.2, 4, 9, 10, 11, 12, 13, 14, 15 Moreover, protein expression as detected by immunohistochemistry is quite similar between columnar cell lesions and atypical ductal hyperplasia or ductal carcinoma in situ grade I.8, 15, 16 Also, molecular studies provide evidence that atypical columnar cell lesions may be the ‘missing link’ between normal breast tissue and low-grade ductal carcinoma in situ and/or low-grade invasive carcinomas,9, 10, 15, 17, 18 thereby being true precursors.15, 17, 19
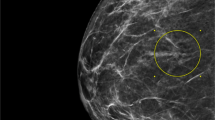
On mammography, columnar cell lesions characteristically present as microcalcifications. The calcifications are mostly small and often clustered, amorphous, or fine pleiomorphic like in ductal carcinoma in situ, and are therefore often classified as BIRADS III or IV on mammography and a reason to take a core needle biopsy to exclude atypical ductal hyperplasia, ductal carcinoma in situ, or invasive carcinoma.2, 20, 21, 22
Full-field digital mammography has increasingly been implemented in hospitals in the last years to replace conventional screen-filmed mammography. Full-field digital mammography has better image quality and the practical advantage of digital data retrieving and storage.23, 24, 25, 26 Some studies described detection of more lesions in patients under 50 years of age and in women with dense breasts, others concluded that full-field digital mammography seemed to be a valid alternative to screen-filmed mammography with regard to diagnostic accuracy.27, 28, 29, 30, 31, 32 However, some studies have reported an increased detection rate of (tiny) microcalcifications, resulting in an increased number of core needle biopsies taken for microcalcifications,23, 24, 26, 33 we hypothesized that the incidence of columnar cell lesions in core needle biopsies has increased since the implementation of full-field digital mammography.
Therefore, the aim of this study was to investigate the incidence of columnar cell lesions in core needle biopsy specimens since the implementation of the full-field digital mammography in comparison with the screen-filmed mammography era, in relation to the presence of atypia in columnar cell lesions.
Materials and methods
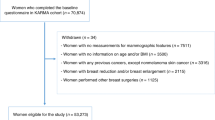
Using the Dutch national pathology archiving system (PALGA), all breast core needle biopsy specimens from women were identified from the University Medical Center of Utrecht from January 2001 until May 2008; the St Antonius Hospital Nieuwegein and the Mesos Medical Center Utrecht from 2002 until 2006, in the Netherlands. Anonymous use of redundant tissue for research purposes is part of the standard treatment agreement with patients in our hospitals.34 During these years, there was a switch from screen-filmed mammography to the full-field digital mammography (August 2003, December 2004, and November 2004, respectively). The mammographic technique (screen-filmed mammography or full-field digital mammography) preceding the core needle biopsy was recorded.
Mammography
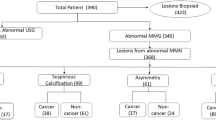
For the screen-filmed technique, Philips Mammo Diagnost MD3000 was used in University Medical Center Utrecht and St Antonius Hospital Nieuwegein, and General Electric Senographe DMR Mammo unit in Mesos Medical Center Utrecht. In all three hospitals, the Selenia™ LORAD/Hologic system was used for the digital mammography. The core needle biopsies were performed under ultrasound (in case of a solid mass) or stereotactic guidance (in case of a solid mass not visible with ultrasound, or for biopsy of microcalcifications), using 14-gauge needles in the University Medical Center Utrecht, and St Antonius Hospital Nieuwegein. In the Mesos Medical Center Utrecht, 16–18-gauge was used and sporadically 11-gauge (with Mammotome). In case of a breast lesion consisting out of microcalcifications, a specimen X-ray of the core needle biopsies was performed in all hospitals to confirm the presence of microcalcifications.
The mammography records were reviewed to ascertain the reason for taking the core needle biopsies and were divided into three categories: density, microcalcifications, or both. In the group of densities, also palpable masses, architectural distortions and asymmetries were included.
Pathology
The original hematoxylin-and-eosin-stained slides from all 3437 female breast core needle biopsies were reviewed by two experienced observers (AVM and PJvD), blinded to the radiological findings. The biopsies were scored for the presence of invasive carcinoma, ductal carcinoma in situ, columnar cell lesions, and other lesions (including usual ductal hyperplasia, atypical ductal hyperplasia, fibroepithelial lesions, and lobular neoplasia) as most advanced lesion. These core needle biopsies were taken in 2959 women; some women underwent more core needle biopsies at different sites of the breast or at different time points. When women were biopsied more than once in the same session and had infiltrative carcinoma or ductal carcinoma in situ, the core needle biopsies were calculated as only one.
We used the scheme described by Schnitt and Vincent-Salomon8 for classifying columnar cell lesions into the four following categories. Columnar cell change is characterized by dilated terminal duct lobular units, lined by one or two layers of columnar type epithelium. The cells contain elongated nuclei with inconspicuous or absent nucleoli. Apical snouts are often present, and often intraluminal secretions and microcalcifications are seen. Columnar cell hyperplasia has a similar appearance as columnar cell change, but the terminal duct lobular units are now lined by more than two stratified cell layers. In columnar cell change with atypia and columnar cell hyperplasia with atypia, cytonuclear atypia is superimposed, showing relatively round or ovoid (instead of elongated) nuclei that are not regularly oriented along the basement membrane. The nuclei are irregular, often with prominent nucleoli and show an increase in the nuclear/cytoplasmic ratio. Mitotic figures may be present. Complex architectural patterns as seen in atypical ductal hyperplasia and low-grade ductal carcinoma in situ are lacking. Columnar cell change with atypia and columnar cell hyperplasia with atypia were grouped for further analysis (as columnar cell lesions with atypia), as we often saw the two appearing together.
According to the usual criteria,1 lesions with enlarged ducts with complex architectural patterns with arcades, bridging, or micropapillae were considered as atypical ductal hyperplasia or low-grade ductal carcinoma in situ, depending on the size of the lesion and the extensiveness of the architectural complexity and regularity. Atypical ductal hyperplasia lesions arising in the context of a columnar cell lesion were noted, as these lesions might represent a further step in the progression of columnar cell lesions to atypical ductal hyperplasia and low-grade ductal carcinoma in situ.
Moreover, the presence of microcalcifications in the columnar cell lesions was noted in each specimen. Since the extent of sampling is a potential confounder, we noted the number of cores taken and the number of histological slides produced from the core needle biopsies. The number of cores ranged between 1 and 8 and the number of histological slides ranged from 1 to 14. There were no significant differences between the number of cores and histological slides in the screen-filmed mammography and full-field digital mammography periods.
Statistical Analysis
Numbers of mammographies in the screen-filmed mammography and full-field digital mammography periods were described, as well as the proportions of core needle biopsies after mammography. Characteristics of the women biopsied were also described using descriptive statistics. The proportions of core needle biopsies that were done for microcalcifications only were compared between the screen-filmed mammography and full-field digital mammography periods, as well as the numbers of invasive carcinomas, ductal carcinoma in situ, columnar cell lesions, and benign lesions. Among the biopsies resulting in a columnar cell lesion, we compared the proportions of columnar cell lesions with and without atypia between the screen-filmed mammography and the full-field digital mammography groups, considering columnar cell change and columnar cell hyperplasia as columnar cell lesions without atypia, and columnar cell lesions with atypia and atypical ductal hyperplasia-columnar cell lesions as columnar cell lesions with atypia. Also, we compared the proportions of mammographies with ‘microcalcifications only’ that led to the diagnosis of columnar cell lesions between the two periods.
Additionally, the core needle biopsy rate and the detection rate of malignant breast tumors were calculated as the number of core needle biopsies and the number of malignant breast tumors, respectively, divided by the total number of mammograms taken in the screen-filmed mammography or full-field digital mammography periods. Then, the relative risks of obtaining a core needle biopsy and of detecting a malignant tumor for full-field digital mammography mammograms compared with screen-filmed mammography mammograms were calculated, adjusted for the hospital where the mammography was performed using a Mantel–Haenszel procedure.
Statistical differences in proportions were tested using χ2 test. The relationships between mammography technique (screen-filmed mammography vs full-field digital mammography) and the results of mammography and core needle biopsies were also estimated with prevalence ratios and accompanying 95% confidence intervals. Modified Poisson regression models were used to adjust the prevalence ratios for age of the woman at examination and the hospital where she was diagnosed.35
All analysis were performed using SPSS version 15 (SPSS, Chicago, IL, USA) except for the modified Poisson regression analyses that were performed using the PROC GENMOD procedure in SAS version 9.1 (SAS Institute, Cary, NC, USA). The two-tailed significance level was set at 0.05.
Results
The numbers of mammographies in the screen-filmed mammography and full-field digital mammography period are presented in Table 1. The proportion of core needle biopsies was higher in the full-field digital mammography (7.6%) than in the screen-filmed mammography period (5.0%) (P<0.0001). The proportions of screen-filmed and full-field digital mammographies were not equally distributed among the hospitals. However, the increased risk of a core needle biopsy procedure after mammography in the full-field digital mammography period compared with the screen-filmed mammography period remained increased after adjustment for hospital (relative risk crude: 1.25, 95% confidence interval: 1.19–1.31; relative risk adjusted: 1.24, 95% confidence interval: 1.18–1.30).
Table 2 refers to core needle biopsies only. The age of the patients biopsied was slightly, but statistically significantly higher in the full-field digital mammography than in the screen-filmed mammography period. Again, the proportions of screen-filmed mammography and full-field digital mammography core needle biopsies were not equally distributed among the hospitals.
The proportion of core needle biopsies taken for only microcalcifications as abnormality at mammography was significantly higher in the full-field digital mammography (28%) than in the screen-filmed mammography (21%) period (Table 2), also after adjustment for age at examination and hospital (adjusted prevalence ratio of ‘microcalcifications only’ for full-field digital mammography vs screen-filmed mammography=1.14, 95% confidence interval: 1.01–1.28) (Table 3).
Columnar cell lesions were significantly more present in the full-field digital mammography period compared with the screen-filmed mammography period (10.8 vs 4.9%, P<0.0001) (Table 2), also after adjustment for age at examination and hospital (adjusted prevalence ratio of columnar cell lesions vs other diagnoses, for full-field digital mammography vs screen-filmed mammography=1.93, 95% confidence interval: 1.48–2.51) (Table 3). As shown in Tables 2 and 3, the proportion of columnar cell lesions without atypia increased significantly from 2.8% in the screen-filmed mammography to 8.2% in the full-field digital mammography period, whereas the proportion of columnar cell lesions with atypia remained nearly constant (2.0 vs 2.6%) (adjusted prevalence ratio of columnar cell lesions with atypia vs columnar cell lesions without atypia for full-field digital mammography vs screen-filmed mammography=0.59, 95% confidence interval: 0.41–0.84).
In both the screen-filmed mammography and full-field digital mammography periods, columnar cell lesions were significantly more often diagnosed in biopsies taken on the basis of only microcalcifications than in biopsies taken on the basis of density with or without microcalcifications (42/303=14% vs 28/1121=2.5%, P<0.0001 in the screen-filmed mammography period and 158/557=28% vs 60/1256=4.1%, P<0.0001 in the full-field digital mammography period). This relationship appeared to be stronger in the full-field digital mammography period than in the screen-filmed mammography period, but the P-value for interaction was not statistically significant (P for interaction=0.20).
More columnar cell lesions were diagnosed with digital mammography compared with screen-filmed mammography and relatively slightly fewer invasive carcinoma, ductal carcinoma in situ, and benign tumors as shown in Table 2. Per mammography, however, the detection rate of malignant tumors (invasive carcinoma and ductal carcinoma in situ in core needle biopsies) was higher in the full-field digital mammography period (771/26 513=2.91%) than in the screen-filmed mammography period (596/28 646=2.08%, P<0.0001). This result remained unchanged after adjustment for hospital with relative risk for detection of malignant tumor being 1.39 (95% confidence interval: 1.24–1.56).
Discussion
This is the first study that systematically investigated the incidence of columnar cell lesions in breast core needle biopsy specimens since the implementation of full-field digital mammography in comparison with screen-filmed mammography. We found significantly more columnar cell lesions in the full-field digital mammography era compared with the screen-filmed mammography era (10.8 vs 4.9%), which was also related to a higher number of core needle biopsies taken for microcalcifications.
First, more diagnostic procedures per mammography were performed in the full-field digital mammography era, due to an increase of core needle biopsies (from 5.0 to 7.6%). Other studies described an increased number of core needle biopsies taken for abnormalities with full-field digital mammography as well, since more abnormalities are recognized due to the higher resolution of full-field digital mammography and also because the accessibility of lesions is facilitated by (particular stereotactic guided) equipment.23, 26, 32
Second, in the full-field digital mammography period, more core needle biopsies were taken for microcalcifications found at mammography, confirmed by the adjusted prevalence ratio of 1.14. Detecting more and smaller microcalcifications by full-field digital mammography due to the increased resolution resulting in more core needle biopsies (due to only microcalcifications) has also been described by other authors.23, 24, 26, 33, 36 Moreover, columnar cell lesions were significantly more often diagnosed in the full-field digital mammography period than in the screen-filmed mammography period, with a prevalence ratio of 1.93. Consistent with our hypothesis was the increase of columnar cell lesions related to the significant increase of core needle biopsies performed for microcalcifications.
As described before, columnar cell lesions usually present as indistinct/amorphous, round, or pleiomorphic microcalcifications that are non-branching on mammography.21, 37, 38 These calcifications represent the psammomatous appearance in the terminal duct lobular units on histology, developed from the calcium deposits in the secretory material.8 The fact that more columnar cell lesions were diagnosed in core needle biopsies on the basis of only microcalcifications during full-field digital mammography suggests that a different type of calcifications is biopsied, for instance smaller microcalcifications, as described by some other authors as well.25, 33
Percentagewise, we found the same amount of columnar cell lesions with atypia during the full-field digital mammography period as the screen-filmed mammography period (1.8%) and significantly more columnar cell lesions without atypia (8.2% respectively 2.8%). The question is whether it is relevant to find more columnar cell lesions without atypia in core needle biopsies, since for columnar cell lesions without atypia a wait-and-see approach is usually followed and these columnar cell lesions are therefore regarded as clinically insignificant.8, 16, 39 For columnar cell lesions with atypia, most advice a surgical excision biopsy because several large studies showed more significant lesions in up to 33% in the subsequent resections.16, 38, 40, 41, 42, 43, 44
Next to the finding of more columnar cell lesions without atypia, also more tumors (including ductal carcinoma in situ and invasive carcinoma) in core needle biopsies were diagnosed per mammogram with full-field digital mammography, showing that not only more irrelevant lesions were biopsied.
So, the increased frequency of tissue sampling instigated by seeing more microcalcifications since the use of digital mammography particularly resulted in more benign lesions. This must have led to higher costs since digital mammography and more women encountering anxiety about the outcome of their biopsy. Therefore, more research is needed to study the patterns of microcalcifications in relation to the diagnosis in order to better identify harmless microcalcification clusters and minimize the number of unnecessary tissue sampling.
In conclusion, this study showed that more columnar cell lesions in core needle biopsies are found since the implementation of the full-field digital mammography in comparison with screen-filmed mammography, in particular relatively insignificant columnar cell lesions without atypia. This seemed to be correlated with the increase of core needle biopsies taken for only microcalcifications with digital mammography.
References
Tavassoli FA, Devilee P . WHO Classification Tumours of the Breast and Female Genital Organs. IARC: Lyon, 2003.
Fraser JL, Raza S, Chorny K, et al. Columnar alteration with prominent apical snouts and secretions: a spectrum of changes frequently present in breast biopsies performed for microcalcifications. Am J Surg Pathol 1998;22:1521–1527.
McLaren BK, Gobbi H, Schuyler PA, et al. Immunohistochemical expression of estrogen receptor in enlarged lobular units with columnar alteration in benign breast biopsies: a nested case-control study. Am J Surg Pathol 2005;29:105–108.
Oyama T, Maluf H, Koerner F, et al. Atypical cystic lobules: an early stage in the formation of low-grade ductal carcinoma in situ. Virchows Arch 1999;435:413–421.
Tavassoli FA . Ductal carcinoma in situ. Introduction of the concept of ductal intraepithelial neoplasia. Mod Pathol 1998;11:140–154.
Kusama R, Fujimori M, Matsuyama I, et al. Clinicopathological characteristics of atypical cystic duct (ACD) of the breast: assessment of ACD as a precancerous lesion. Pathol Int 2000;50:793–800.
Azzopardi JG, Ahmed A, Millis RR . Problems in breast pathology. Major Probl Pathol 1979;11:i-466.
Schnitt SJ, Vincent-Salomon A . Columnar cell lesions of the breast. Adv Anat Pathol 2003;10:113–124.
Aulmann S, Elsawaf Z, Penzel R, et al. Invasive tubular carcinoma of the breast frequently is clonally related to flat epithelial atypia and low-grade ductal carcinoma in situ. Am J Surg Pathol 2009;33:1646–1653.
Dabbs DJ, Carter G, Fudge M, et al. Molecular alterations in columnar cell lesions of the breast. Mod Pathol 2006;19:344–349.
Goldstein NS, O’Malley BA, Goldstein NS, et al. Cancerization of small ectatic ducts of the breast by ductal carcinoma in situ cells with apocrine snouts: a lesion associated with tubular carcinoma. Am J Clin Pathol 1997;107:561–566.
Page DL . Cancer risk assessment in benign breast biopsies. Hum Pathol 1986;17:871–874.
Page DL, Simpson JF . Pathology of preinvasive and excellent-prognosis breast cancer. Curr Opin Oncol 1996;8:462–467.
Rosen PP . Columnar cell hyperplasia is associated with lobular carcinoma in situ and tubular carcinoma. Am J Surg Pathol 1999;23:1561.
Simpson PT, Gale T, Reis-Filho JS, et al. Columnar cell lesions of the breast: the missing link in breast cancer progression? A morphological and molecular analysis. Am J Surg Pathol 2005;29:734–746.
Feeley L, Quinn CM . Columnar cell lesions of the breast. Histopathology 2008;52:11–19.
Lee S, Medina D, Tsimelzon A, et al. Alterations of gene expression in the development of early hyperplastic precursors of breast cancer. Am J Pathol 2007;171:252–262.
Moinfar F, Man YG, Bratthauer GL, et al. Genetic abnormalities in mammary ductal intraepithelial neoplasia-flat type (‘clinging ductal carcinoma in situ’): a simulator of normal mammary epithelium. Cancer 2000;88:2072–2081.
Sinn HP . Breast cancer precursors: lessons learned from molecular genetics. J Mol Med 2009;87:113–115.
Jara-Lazaro AR, Tse GM, Tan PH . Columnar cell lesions of the breast: an update and significance on core biopsy. Pathology (Phila) 2009;41:18–27.
Kim MJ, Kim EK, Oh KK, et al. Columnar cell lesions of the breast: mammographic and US features. Eur J Radiol 2006;60:264–269.
Schnitt SJ . Columnar cell lesions of the breast: pathological features and clinical significance. Curr Diagn Pathol 2004;10:193–203.
del Turco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR Am J Roentgenol 2007;189:860–866.
Fischer U, Baum F, Obenauer S, et al. Comparative study in patients with microcalcifications: full-field digital mammography vs screen-film mammography. Eur Radiol 2002;12:2679–2683.
Fischmann A, Siegmann KC, Wersebe A, et al. Comparison of full-field digital mammography and film-screen mammography: image quality and lesion detection. Br J Radiol 2005;78:312–315.
Karssemeijer N, Bluekens AM, Beijerinck D, et al. Breast cancer screening results 5 years after introduction of digital mammography in a population-based screening program. Radiology 2009;253:353–358.
Berman CG . Recent advances in breast-specific imaging. Cancer Control 2007;14:338–349.
D’Orsi CJ, Newell MS . Digital mammography: clinical implementation and clinical trials. Semin Roentgenol 2007;42:236–242.
Heddson B, Ronnow K, Olsson M, et al. Digital versus screen-film mammography: a retrospective comparison in a population-based screening program. Eur J Radiol 2007;64:419–425.
Lewin JM, Hendrick RE, D’Orsi CJ, et al. Comparison of full-field digital mammography with screen-film mammography for cancer detection: results of 4,945 paired examinations. Radiology 2001;218:873–880.
Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med 2005;353:1773–1783.
Skaane P, Hofvind S, Skjennald A . Randomized trial of screen-film versus full-field digital mammography with soft-copy reading in population-based screening program: follow-up and final results of Oslo II study. Radiology 2007;244:708–717.
Becker L, Taves D, McCurdy L, et al. Stereotactic core biopsy of breast microcalcifications: comparison of film versus digital mammography, both using an add-on unit. AJR Am J Roentgenol 2001;177:1451–1457.
van Diest PJ . No consent should be needed for using leftover body material for scientific purposes. BMJ 2002;325:648–651.
Zou G . A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706.
Pun E, Lau WF, Cassumbhoy R, et al. Clinical experience of the first digital mammographic unit in Australia in its first year of use. Med J Aust 2007;187:576–579.
Kunju LP, Kleer CG . Significance of flat epithelial atypia on mammotome core needle biopsy: should it be excised? Human Pathol 2007;38:35–41.
Senetta R, Campanino PP, Mariscotti G, et al. Columnar cell lesions associated with breast calcifications on vacuum-assisted core biopsies: clinical, radiographic, and histological correlations. Mod Pathol 2009;22:762–769.
Jacobs TW, Connolly JL, Schnitt SJ . Nonmalignant lesions in breast core needle biopsies: to excise or not to excise? Am J Surg Pathol 2002;26:1095–1110.
Chivukula M, Bhargava R, Tseng G, et al. Clinicopathologic implications of ‘flat epithelial atypia’ in core needle biopsy specimens of the breast. Am J Clin Pathol 2009;131:802–808.
David N, Labbe-Devilliers C, Moreau D, et al. Diagnosis of flat epithelial atypia (FEA) after stereotactic vacuum-assisted biopsy (VAB) of the breast: what is the best management: systematic surgery for all or follow-up? J Radiol 2006;87:1671–1677.
Guerra-Wallace MM, Christensen WN, White Jr RL . A retrospective study of columnar alteration with prominent apical snouts and secretions and the association with cancer. Am J Surg 2004;188:395–398.
Noske A, Pahl S, Fallenberg E, et al. Flat epithelial atypia is a common subtype of B3 breast lesions and associated with noninvasive cancer but not with invasive cancer in final excision histology. Hum Pathol 2009;41:522–527.
Tomasino RM, Morello V, Gullo A, et al. Assessment of ‘grading’ with Ki-67 and c-kit immunohistochemical expressions may be a helpful tool in management of patients with flat epithelial atypia (FEA) and columnar cell lesions (CCLs) on core breast biopsy. J Cell Physiol 2009;221:343–349.
Acknowledgements
This work was supported by The Oncology Center of St Antonius Hospital Nieuwegein.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Verschuur-Maes, A., van Gils, C., van den Bosch, M. et al. Digital mammography: more microcalcifications, more columnar cell lesions without atypia. Mod Pathol 24, 1191–1197 (2011). https://doi.org/10.1038/modpathol.2011.81
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.81
Keywords
This article is cited by
-
Risk factors for breast cancer development by tumor characteristics among women with benign breast disease
Breast Cancer Research (2021)
-
3-T breast magnetic resonance imaging in patients with suspicious microcalcifications on mammography
European Radiology (2014)
-
Analysis of gene copy number alterations by multiplex ligation-dependent probe amplification in columnar cell lesions of the breast
Cellular Oncology (2014)
-
Impact of full-field digital mammography on pre-operative diagnosis and surgical treatment of mammographic microcalcification
Breast Cancer Research and Treatment (2014)