Abstract
High-grade endometrioid and serous carcinomas of the ovary and fallopian tube are responsible for the majority of cancer deaths and comprise a spectrum that includes early or localized (tubal intraepithelial carcinoma) and advanced (invasive or metastatic) disease. We subdivided a series of these tumors into three groups, (1) classic serous, (2) mixed serous and endometrioid and (3) endometrioid carcinomas and determined: (1) the frequencies of coexisting tubal intraepithelial carcinoma, (2) frequency of a dominant ovarian mass suggesting an ovarian origin and (3) immuno-localization of WT-1, p53, PTEN, PAX2 and p16ink4. All tumors were analyzed for p53 mutations. Thirty six, 25 and 8% of groups 1–3 were associated with tubal intraepithelial carcinoma (P=0.09) and 34, 45 and 62% predominated in one ovary (P=0.028), respectively. Differences in frequencies of diffuse p53 immunostaining (85–93%), WT-1 (70–98%) and p16ink4 positivity (69–75%) were not significant for all groups. Greater than 95% reduction in PAX2 and PTEN occurred in 67–75 and 5–12%, respectively; however, PAX2 and PTEN staining intensity, when present, was often heterogeneous, highlighting different tumor populations. PAX2 and PTEN expression were markedly reduced or absent in 12 of 12 and 4 of 12 tubal intraepithelial carcinomas. In summary, high-grade müllerian carcinomas share identical frequencies of altered or reduced expression of p53, PTEN and PAX2, all of which can be appreciated in tubal intraepithelial carcinomas. Because only a subset of these tumors appears to arise in the fallopian tube, attention to expression of these biomarkers in the ovary and other müllerian sites might facilitate the identification of other carcinogenic pathways. PAX2 and PTEN, in addition to p53 and p16ink4, comprise a potentially important gene combination in high-grade pelvic carcinogenesis.
Similar content being viewed by others
Main
Malignant pelvic (ovary, fallopian tube and peritoneal) epithelial neoplasms can display a diverse array of histological patterns, including serous, endometrioid, mucinous and clear cell differentiation. Studies interrogating the molecular profiles and clinical behavior of these different tumors have demonstrated that they can be partitioned into two general pathways of tumor development.1 The ‘type I’ pathway is exemplified by the endometrioid, clear cell, mucinous and low-grade serous carcinomas. These tumors are associated with mutations in genes encoding mismatch repair proteins and signaling proteins governing cell proliferation, such as BRAF, KRAS, β-catenin and PTEN, but not mutations in p53.2, 3, 4 Type I tumors are felt to evolve in a step-wise manner from known pre-existing conditions such as cortical inclusion cysts, endometriosis, cystadenomas and adenofibromas to borderline tumors to invasive malignancies, and appear to be the prototype for an ovarian-derived carcinogenic sequence.5 In contrast, high-grade serous carcinomas have been assigned to the ‘type II’ pathway and the lack of a clear-cut precursor condition has, until recently, prompted the theory that these tumors arise rapidly through p53 mutations, an assumption encouraged by the fact that most of these tumors are discovered at an advanced stage.6
Two observations have progressively refined our understanding of high-grade serous carcinomas. The first has been the discovery that the fallopian tube is a site of origin for many of these tumors, highlighted by protocols that extensively sampled the fallopian tube, especially the fimbriated end, for histological evaluation.7, 8, 9 These protocols have revealed that from 35 to 45% of high-grade serous carcinomas are associated with a tubal intraepithelial carcinoma, suggesting an origin from the tube.10, 11, 12, 13 The second observation has been the increasing similarity between high-grade serous and high-grade endometrioid carcinomas, including the finding of p53 mutations in the latter.14, 15, 16, 17 As a consequence, these two subsets of high-grade carcinomas have often been grouped together. However, we have previously shown that the two tumor types are not equivalent in terms of their association with either tubal intraepithelial carcinoma or tumor distribution, with the endometrioid tumors having a lower frequency of the former and a higher frequency of association with a dominant (greater than 2X length in the greatest dimension) ovarian mass.13 The differences in the frequency of these parameters suggest differences in potential tumor origins for high-grade serous (more frequently tubal) and endometrioid (more frequently ovarian) carcinomas.
The purpose of this study was to determine (1) if high-grade serous and endometrioid carcinomas were equivalent in terms of p53 mutations status, (2) if they shared similarities in other biomarkers and (3) if these biomarkers were similarly altered in recognizable early phases of the diseases (tubal intraepithelial carcinoma). In addition to p53, biomarkers traditionally upregulated in serous (WT-1 and p16ink4) and downregulated in endometrioid (PTEN and PAX2) carcinomas were studied.13, 18, 19, 20 The purpose of this strategy was to gain a greater understanding of high-grade Müllerian carcinomas in terms of (1) the need to separate them in the context of diagnostic pathology, (2) their potential origins and (3) the timing of these gene alterations, ie, their role in early (tubal intraepithelial carcinoma) and more widespread disease. In this study, we show these biomarkers are equivalent in their frequencies in all high-grade müllerian carcinomas. Further we will show that alterations in the expression of these biomarkers characterize the earliest malignant phases of pelvic serous cancer.
Materials and methods
Case Selection and Analysis
The study was approved by the institutional review board at Brigham and Women's Hospital. We evaluated 89 consecutive cases of high-grade carcinoma retrieved from the pathology database between 2006 and 2008. In all, a protocol for extensively examining the fimbria and proximal tube was used (SEE-FIM protocol).8 The histological diagnoses were verified by concurrent pathologic review by two coauthors (CPC and MRN) using a variation on published criteria.21 Tumors with marked atypia, and papillary or prominent slit-forming gland-like spaces were designated as serous (Group 1). Tumors exhibiting sheet-like growth or focal endometrioid gland morphology with uniform nuclear features and lacking papillary, or slit-forming architecture were designated as high-grade endometrioid (Group 3). Tumors considered to have features intermediate between the two were designated as mixed serous and endometrioid pattern (Group 2). The presence or absence of a dominant ovarian mass, defined as greater than a twofold difference in the maximum recorded dimension between the two ovaries, and a tubal intraepithelial carcinoma were determined for each case, as described previously.13 For statistical analysis, Groups 1 and 3 were compared using Fisher's exact test.
Immunohistochemistry
Sections (5 μm) were cut from formalin-fixed, paraffin-embedded blocks containing tumor tissue onto positively charged slides and baked overnight at 37°C. After sections were de-waxed and rehydrated, antigen retrieval was performed in a pressure cooker in 10 mM citrate buffer, pH 6.0. Immunostaining was performed with the following antibodies, respectively: mouse monoclonal anti-p53 antibody (clone DO-1; ImmunoTech, Westbrook, ME, USA); mouse anti-p16ink4 antibody (clone 16P07; NeoMarkers, Fremont, CA, USA); and anti-WT-1 antibody (clone 6F-H2; DAKO, Carpinteria, CA, USA). The EnVision+ System for use with mouse primary antibodies (DAKO) was subsequently used according to manufacturer's instructions and the slides were developed using 3, 3′-diaminobenzidine as a substrate and Gill's hematoxylin as a counterstain. For p53 and WT-1 immunohistochemistry, uniformly distributed and strong nuclear staining in at least 50% of the tumor cells was considered a positive, although diffuse positivity was the norm. Similarly, immunopositivity for p16ink4 was scored positive when uniform and strong nuclear and cytoplasmic staining was seen in virtually all of the tumor cells. If the staining was weak or patchy in distribution, it was classified as negative. Statistical comparison of the immunoprofiles of the high-grade serous and endometrioid carcinomas were performed using Fisher's exact test. PAX2 immunostaining was performed using an antibody from Invitrogen (Carlsbad, CA, USA; Cat# 71–6000) at 1:300. PTEN immunostaining was performed using the DAKO Monoclonal Mouse Anti-Human PTEN (Cat# M3627) at a dilution of 1:200. In both, cases were classified as negative if staining was seen in less than 5% of the cells in the tumor, heterogeneous if two discrete populations were negative and positive, and positive if over 95% of the tumor cells stained positive. This three step scoring strategy was used because the significance of staining distribution for these two biomarkers has not been clearly determined. In contrast, heterogeneous staining for p53, WT-1 and p16ink4 was classified as negative on the basis of earlier experience.
Analysis of p53 Mutations
Sections (5 μm) were cut onto membrane slides (Leica Microsystems, Bannockburn, IL, USA). Tumor and control tissues were dissected manually using sterile scalpels or laser-capture microdissection (LCM). LCM was performed using the PALM microbeam instrument (P.A.L.M. Microlaser Technologies, Bernried, Germany). Genomic DNA was isolated, as described previously and amplified by polymerase chain reaction (PCR), using tailed primers designed to amplify p53 exons 1 through 11.22 Secondary amplification was performed using T3 and T7 primers specific to the tail sequences used in the original amplification. T3 and T7 primers were subsequently used to sequence the PCR products. DNA sequences were analyzed using the Mutation Surveyor program (Soft Genetics, State College, PA, USA). To exclude spurious mutations introduced into somatic DNA as a consequence of formalin-fixation, all p53 mutation-positive exons were re-sequenced from a replicate amplified products.23
Results
Fimbrial Involvement and Dominant Ovarian Mass are Inversely Related in High-Grade Müllerian Carcinomas and are More Common in Serous and Endometrioid Carcinomas Respectively
Previously, we reported two parameters that correlated with assigning tumor origin for pelvic serous and endometrioid carcinomas, dominant ovarian mass and tubal intraepithelial carcinoma.13 In this report, we subdivided the spectrum of tumors into three categories, including classic serous, one composed of tumors resembling serous and endometrioid and a third consisting of features characteristic of high-grade endometrioid tumors. The results are summarized in Table 1. Overall, 20 of 56, 5 of 20 of category 1 and 2 tumors were associated with a tubal intraepithelial carcinoma, compared with 1 of 13 category 3 (endometrioid) tumors, a difference (between catetories 1 and 3) that bordered on significant (P=0.09). In contrast, a significantly higher frequency of category 3 tumors were associated with a dominant ovarian mass (P=0.028).
High-Grade Müllerian Carcinomas have Equivalent Frequencies of (Positive) p53, WT-1, p16ink4 and (Negative) PTEN and PAX2 Expression
Table 1 and Figures 1 and 2 summarize the immunostaining for the above biomarkers in the three groups of tumors. No significant differences in staining frequency were seen for any of the biomarkers including WT-1, which has been previously associated with serous carcinomas. Staining frequencies for p53 (85–93%, not shown in table), p16ink4 (69–75%), WT-1 (70–98%) and PAX2 (negative; 67–75%) were high in all categories, with P-values ranging from 0.58 to 1.0. Similarly, the rate of negative staining for PTEN (5–12%) was comparable and did not distinguish high-grade endometrioid carcinomas from the other two categories. However, when the numbers demonstrating either negative or focally negative (heterogeneous) were combined, the difference between groups 1 and 3 were significant at P=0.048 (Table 1), suggesting a higher frequency of heterogeneous or negative staining in high-grade endometrioid carcinomas. However, high frequencies of heterogeneous PTEN staining were also seen in Groups 1 and 2. In contrast, staining pattern frequencies for PAX2 staining were equivalent in all groups (P=1.0).
Immunohistochemical analysis of high-grade serous and endometrioid carcinomas. Hematoxylin and eosin-stained sections of high-grade serous, mixed serous and endometrioid and endometrioid carcinomas (a, e, i) along with immunohistochemical stains for p53 (b, f, j), p16ink4 (c, g, k) and PAX2 (d, h, l) are illustrated. The staining pattern for PAX2 in normal fallopian tube is shown in Figure 3b.
Paired hematoxylin and eosin (a, c, e) and PTEN immunostains (b, d, f) of high-grade Müllerian carcinomas, demonstrating diffusely positive (b), negative (d) and heterogeneous (f) staining. The latter typically designates discrete units of epithelium with juxtaposed positive (right) and negative (left) staining (f). The staining pattern for PTEN in normal fallopian tube is shown in Figure 3c.
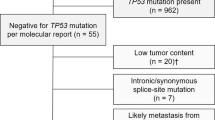
Frequency of p53 Mutations is Similar in High-Grade Serous and Endometrioid Carcinomas
As a high proportion of high-grade serous and endometrioid carcinomas were immunopositive for p53, we next sought to determine the frequency of p53 mutations (Tables 1 and 2). We detected p53 mutations in 89% of the entire group including 93, 75 and 92% of groups 1, 2 and 3.
The majority of the p53 mutations were missense mutations (Table 2). Missense mutations were detected in from 67 to 83% of tumors and were not significantly associated with any one group. The presence of missense mutations correlated highly with p53 overexpression on immunohistochemistry as 85% of these mutations were associated with strong staining. The remaining mutations were nonsense, insertion, deletion and splice donor/acceptor-site mutations. The majority of the p53 mutations were present in exons 5–8, which encode for the DNA-binding domain of p53, accounting for 83% of all p53 mutations detected.
Alterations in Expression of p53, Pax2 and PTEN Characterized Earlier forms of Serous Carcinoma (Tubal Intraepithelial Carcinoma)
Analysis of serous tubal intraepithelial carcinomas for the above biomarkers was performed to determine if they shared the same immunophenotype as the concomitant advanced malignancies (Figure 3). Fifteen blocks from 12 cases were analyzed. Eleven cases demonstrated strong staining for p53. Seven cases contained invasive carcinoma elsewhere in the same section as the intraepithelial carcinoma. In all 12 cases, PAX2 staining was negative in the intraepithelial carcinoma, although in two cases heterogeneous staining was seen in another block. In four blocks from four cases, PTEN staining was absent (negative). In four other cases, PTEN staining of tubal intraepithelial carcinoma was heterogeneous. In 9 of 10 cases, the coexisting invasive carcinomas were PAX2 negative; in another, PAX2 staining was heterogeneous. The correlation between PTEN staining in the intraepithelial and invasive carcinomas varied, with some tumors losing PTEN expression, whereas others demonstrated heterogeneous staining (Table 3, Figure 3).
Discussion
This study has confirmed earlier observations that the origin of high-grade Müllerian carcinomas is diverse, including the ovary, distal fallopian tube and possibly, other sites. The serous or mixed serous and endometrioid carcinoma phenotype correlates with the presence of a tubal intraepithelial carcinoma with involvement of both ovaries in an equal distribution, whereas high-grade endometrioid carcinoma tumors are uncommonly associated with tubal intraepithelial carcinoma and predominate in one ovary over the other (Table 1). However, as shown in Table 1, there is considerable ‘leakage’ of these two variables across all three histological groups. Thus, a diagnostic pathologist cannot expect histological criteria to segregate high-grade müllerian carcinomas to specific organs (tube vs ovary). Nevertheless, the biomarker expression patterns, seen in these tumors and in early tubal malignancies, combined with the coexisting conditions such as tubal intraepithelial carcinoma and dominant ovarian mass, raise new and compelling questions about the classification and pathogenesis of high-grade müllerian carcinomas. The immunohistochemical studies draw high-grade endometrioid and serous carcinomas closer together by shared disturbances in gene expression. However, there is reason to assume that shared pathogenetic mechanisms operate in both the ovary and tube and possibly, other sites.
As illustrated in Table 1, none of the three tumor groups, including those with classic features of high-grade endometrioid carcinoma, could be distinguished on the basis of the expression of three biomarkers that have been recently studied in ovarian cancer. p53, WT-1 and p16ink4, which are generally heterogeneous in low-grade endometrioid and typically diffusely positive in serous carcinomas, were strongly positive in a high frequency of each tumor category, an observation that has been appreciated previously.13, 15, 17, 19 Nearly 90% of all tumors exhibited mutations in p53, a gene typically assigned to the high-grade serous carcinomas. Recent studies have identified a subset of high-grade endometrioid carcinomas that contain p53 mutations, separating this group from other endometrioid carcinomas.19 Although p53 mutation-positive tumors were classified initially as an uncommon subset of ovarian endometrioid carcinomas, the relative frequency of this group may be a function of differences in tumor classification.19 Most of the high-grade endometrioid carcinomas in this study contained mutations in p53.
Of considerable interest were the expression patterns of PAX2 and PTEN, both in intraepithelial and invasive carcinomas. PAX2 is a relatively new biomarker to be studied in ovarian cancer and its relationship to these tumors is evolving. PAX2 has been most intensively studied in the kidney. It is designated a homeogene that is critical to renal development and is expressed in approximately 60% of renal cell carcinomas.22 Its role in müllerian neoplasms is less clear. PAX2 is strongly expressed in tubal secretory cells and in similar cells in ovarian cortical inclusion cysts. Some reports have described PAX2 staining in ovarian serous carcinomas; however, more recent studies have noted a stronger likelihood of staining in low-grade versus high-grade serous carcinomas.20, 24 Our interest in this gene stemmed from a recent report by one of us (GLM) that expression of both PAX2 and PTEN are absent in the early phases of endometrial carcinogenesis, including endometrial intraepithelial neoplasia.25 On the basis of this information, we examined the expression of both in the tumors reported in this study.
We used a three stage system for both PAX2 and PTEN scoring because we had relatively little experience with these antibodies but have observed staining in both to be heterogeneous. PAX2 expression was either completely lost or stained less than 5% of tumor cells in over 70% of tumors. In contrast, diffuse expression of this biomarker was uncommon, seen in only 17% of all cases. The remaining 12% exhibited various indices of staining, more in keeping with variable regulation of gene expression. Expression of PTEN also varied but less so. Only 17% scored as completely negative, but only 34% were diffusely positive and nearly one-half exhibited heterogeneous staining. Thus, the varied staining patterns of both PTEN and PAX2 suggest more than one mechanism may be operative, including loss of function by the loss of all or part of the encoding gene, and differential regulation of gene expression, either genetic or epigenetic, as observed previously (Mutter GL, unpublished). This is in contrast to the common observation that the loss of p53 function is attributed to both mutation and loss of heterozygosity.26 The biological significance of either loss or partial loss of PAX2 and PTEN staining in invasive or advanced carcinomas remains uncertain, in the context of the extensive and widespread disturbances in gene expression that characterizes these tumors.27
A compelling finding in this study was the nearly consistent loss or marked reduction in PAX2 staining in a high percentage of not only advanced malignancies but tubal intraepithelial carcinomas (Table 3, Figure 3). In the face of the overall high frequency of PAX2 loss shown in Table 1, this is not unexpected. Moreover, a causal relationship between tubal intraepithelial carcinomas and concurrent remote tumors has been previously established by the sharing of identical mutations in p53.11, 12 However, not withstanding the fact that intraepithelial carcinomas are considered to have malignant potential (proven further by the advanced tumors with which they associate) staining of PAX2 and PTEN support the concept that the reduction in expression of these genes occurs in the earlier time points of the malignant process. Moreover, it links PAX2—a gene whose perturbations are associated with endometrioid carcinoma—to serous carcinogenesis.26
The frequency of PTEN-negative staining in intraepithelial carcinomas was lower (33%, Table 3, Figure 3); however, it was heterogeneous in four additional cases and the adjacent invasive carcinomas were often heterogeneous in their PTEN staining (Table 1, Figure 2). Thus, there is evidence to suggest that alterations in the expression of both PTEN and PAX2 could be involved in the early stages of serous carcinogenesis, similar to endometrioid carcinomas of the uterus.26 In this context, the immunostaining results raise two other important questions. The first is whether PTEN and PAX2 are lost before malignancy, as seen in the endometrial model, or are coincident with the emergence of malignancy. We have recently identified discrete benign appearing secretory cell outgrowths in the fallopian tube, many of which are associated with loss of PAX2 (and sometime PTEN) expression, presenting a compelling corollary to the observations in the endometrium.28 Thus, there is the real possibility that some of the genes downregulated in serous cancer become altered before the onset of the malignant phenotype. The second is whether a similar pathway that includes downregulation of these genes can be elucidated in a site other than the fallopian tube. Efforts to identify p53-positive ovarian cortical inclusion cysts have largely been unsuccessful. However, an alternative model of ovarian serous carcinogenesis could include the initial downregulation of PTEN, PAX2 or other genes in endometriosis, ovarian surface epithelium or cortical müllerian inclusions, setting the stage for malignancy with subsequent loss of p53 function. A variation of this theme has been proposed for ovarian surface epithelium, although based on limited cases.29 Whether such a scenario exists awaits a more exhaustive study of the benign ovarian cortex in women at risk for ovarian cancer and the general population. If the above studies are fruitful and confirm this report, PTEN and PAX2 dysregulation may join p53 as important early events in the genesis of the most common and lethal ovarian cancers in women.
References
Shih IM, Kurman RJ . Ovarian tumorigenesis—A proposed model based on morphological and molecular genetic analysis. Am J Pathol 2004;164:1511–1518.
Gamallo C, Palacios J, Moreno G, et al. beta-catenin expression pattern in stage I and II ovarian carcinomas—Relationship with beta-catenin gene mutations, clinicopathological features, and clinical outcome. Am J Pathol 1999;155:527–536.
Geyer JT, Lopez-Garcia MA, Sanchez-Estevez C, et al. Pathogenetic pathways in ovarian endometrioid adenocarcinoma a molecular study of 29 cases. Am J Surg Pathol 2009;33:1157–1163.
Gras E, Catasus L, Arguelles R, et al. Microsatellite instability, MLH-1 promoter hypermethylation, and frameshift mutations at coding mononucleotide repeat microsatellites in ovarian tumors. Cancer 2001;92:2829–2836.
Jarboe EA, Folkins AK, Drapkin R, et al. Tubal and ovarian pathways to pelvic epithelial cancer: a pathological perspective. Histopathology 2009;55:619.
Folkins AK, Jarboe EA, Roh MH, et al. Precursors to pelvic serous carcinoma and their clinical implications. Gynecol Oncol 2009;113:391–396.
Cass I, Holschneider C, Datta N, et al. BRCA-mutation-associated fallopian tube carcinoma: a distinct clinical phenotype? Obstet Gynecol 2005;106:1327–1334.
Medeiros F, Muto MG, Lee Y, et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am J Surg Pathol 2006;30:230–236.
Rabban JT, Krasik E, Chen LM, et al. Multistep level sections to detect occult fallopian tube carcinoma in risk-reducing salpingo-oophorectomies from women with BRCA mutations: implications for defining an optimal specimen dissection protocol. Am J Surg Pathol 2009;33:1878–1885.
Callahan MJ, Crum CP, Medeiros F, et al. Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J Clin Oncol 2007;25:3985–3990.
Carlson JW, Miron A, Jarboe EA, et al. Serous tubal intraepithelial carcinoma: its potential role in primary peritoneal serous carcinoma and serous cancer prevention. J Clin Oncol 2008;26:4160–4165.
Kindelberger DW, Lee Y, Miron A, et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: evidence for a causal relationship. Am J Surg Pathol 2007;31:161–169.
Roh MH, Kindelberger D, Crum CP . Serous tubal intraepithelial carcinoma and the dominant ovarian mass: clues to serous tumor origin? Am J Surg Pathol 2009;33:376–383.
Leng J, Lang J, Shen K, et al. Overexpression of p53, EGFR, c-erbB2 and c-erbB3 in endometrioid carcinoma of the ovary. Chin Med Sci J 1997;12:67–70.
Madore J, Ren F, Filali-Mouhim A, et al. Characterization of the molecular differences between ovarian endometrioid carcinoma and ovarian serous carcinoma. J Pathol 2010;220:392–400.
McCluggage G . My approach to and thoughts on the typing of ovarian carcinomas. J Clin Pathol 2008;61:152–163.
Geyer JT, López-García MA, Sánchez-Estevez C, et al. Pathogenetic pathways in ovarian endometrioid adenocarcinoma: a molecular study of 29 cases. Am J Surg Pathol 2009;33:1157–1163.
Phillips V, Kelly P, McCluggage WG . Increased p16 expression in high-grade serous and undifferentiated carcinoma compared with other morphologic types of ovarian carcinoma. Int J Gynecol Pathol 2009;28:179–186.
Köbel M, Kalloger SE, Boyd N, et al. Ovarian carcinoma subtypes are different diseases: implications for biomarker studies. PLoS Med 2008;5:e232.
Tung CS, Mok SC, Tsang YT, et al. PAX2 expression in low malignant potential ovarian tumors and low-grade ovarian serous carcinomas. Mod Pathol 2009;22:1243–1250.
Lee KR, Tavassoli FA, Prat J, et al. Surface epithelial-stromal tumors. In: Tavassoli FA, Devilee P (eds). Tumours of the Breast and Female Genital Organs. IARC Press: Lyon, France, 2003, pp 119–120.
Lee Y, Miron A, Drapkin R, et al. A candidate precursor to serous carcinoma that originates in the distal fallopian tube. J Pathol 2007;213:116.
Williams C, Ponten F, Moberg C, et al. A high frequency of sequence alterations is due to formalin fixation of archival specimens. Am J Pathol 1999;155:1467–1471.
Chivukula M, Dabbs DJ, O’Connor S, et al. PAX 2: a novel Müllerian marker for serous papillary carcinomas to differentiate from micropapillary breast carcinoma. Int J Gynecol Pathol 2009;28:570–578.
Monte NM, Webster KA, Neuberg D, et al. Joint loss of PAX2 and PTEN expression in endometrial precancers and cancer. Cancer Res (in press).
Chivukula M, Edwards R, Nikiforova M, et al. Loss of heterozygosity (LOH) and immunohistochemical analysis (IHC) of a subset of primary fallopian tube carcinomas (PFTC) arising in the background of tubal intraepithelial carcinoma ‘TIC’ from primary peritoneal serous carcinomas with/without associated tubal intraepithelial carcinoma ‘TIC’. Mod Pathol 2010;23:237A.
Hirshfield KM, Rebbeck TR, Levine AJ . Germline mutations and polymorphisms in the origins of cancers in women. J Oncol 2010;2010:297671.
Chen EY, Mehra KK, Mehrad M, et al. Secretory cell outgrowth, PAX2 and early serous carcinogenesis. J of Pathol (in press).
Cai KQ, Wu H, Klein-Szanto AJ, et al. Acquisition of a second mutation of the Tp53 alleles immediately precedes epithelial morphological transformation in ovarian tumorigenicity. Gynecol Oncol 2009;114:18–25.
Acknowledgements
We thank Mei Zheng, Tatiana Zolotarev and Terri Woo for technical assistance in immunohistochemistry. This work was supported by grants from the NCI (P50CA10500 [SPORE]: D. Cramer, PI), NCI 1R21CA124688-01A1 (CP Crum, PI), The Columbia Hospital For Women Research Foundation (CP Crum, PI), the Charlotte Geyer Foundation (CPC), the Francis Ward Paine and TSA Pemberton Funds from the Division of Women's and Perinatal Pathology, Brigham and Women's Hospital, the Women's Cancer Program at the Dana Farber Cancer Institute, and a gift in memory of Elizabeth Ford Smith.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented, in part, at the 98th Annual Meeting of the United States and Canadian Academy of Pathology in Boston, MA, April 2009.
Rights and permissions
About this article
Cite this article
Roh, M., Yassin, Y., Miron, A. et al. High-grade fimbrial-ovarian carcinomas are unified by altered p53, PTEN and PAX2 expression. Mod Pathol 23, 1316–1324 (2010). https://doi.org/10.1038/modpathol.2010.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.119
Keywords
This article is cited by
-
Silencing PTEN in the fallopian tube promotes enrichment of cancer stem cell-like function through loss of PAX2
Cell Death & Disease (2021)
-
PTEN Lipid Phosphatase Activity Enhances Dengue Virus Production through Akt/FoxO1/Maf1 Signaling
Virologica Sinica (2021)
-
Clinical and pathological associations of PTEN expression in ovarian cancer: a multicentre study from the Ovarian Tumour Tissue Analysis Consortium
British Journal of Cancer (2020)
-
PTEN loss in the fallopian tube induces hyperplasia and ovarian tumor formation
Oncogene (2018)
-
PAX2 function, regulation and targeting in fallopian tube-derived high-grade serous ovarian cancer
Oncogene (2017)