Abstract
Secretory leukocyte protease inhibitor (SLPI) is an important respiratory tract host defense protein, which is proteolytically inactivated by excessive neutrophil elastase (NE) during chronic Pseudomonas infection in the cystic fibrosis (CF) lung. We generated two putative NE-resistant variants of SLPI by site-directed mutagenesis, SLPI-A16G and SLPI-S15G-A16G, with a view to improving SLPI’s proteolytic stability. Both variants showed enhanced resistance to degradation in the presence of excess NE as well as CF patient sputum compared with SLPI-wild type (SLPI-WT). The ability of both variants to bind bacterial lipopolysaccharides and interact with nuclear factor-κB DNA binding sites was also preserved. Finally, we demonstrate increased anti-inflammatory activity of the SLPI-A16G protein compared with SLPI-WT in a murine model of pulmonary Pseudomonas infection. This study demonstrates the increased stability of these SLPI variants compared with SLPI-WT and their therapeutic potential as a putative anti-inflammatory treatment for CF lung disease.
Similar content being viewed by others
Introduction
Chronic lung infection, inflammation, and gradual destruction of the lung are characteristic clinical features of cystic fibrosis (CF). This gradual loss of lung function is fatal to most CF patients as over 95% die of respiratory failure. Neutrophils have a leading role in the destruction of the lung tissue in CF.1, 2, 3 Infection by resistant pathogens such as Pseudomonas aeruginosa4 causes impairment of host immune defense mechanisms triggering a sustained pro-inflammatory environment and the recruitment of neutrophils in high numbers to the CF airways.5 As a consequence of this accumulation of neutrophils, elevated levels of proteases, such as neutrophil elastase (NE), are found in the CF airways.6, 7 NE is regarded as a key driver of lung destruction8, 9 and inflammation, especially during chronic P. aeruginosa infection in the CF lung.10, 11
Consequently, the development of NE inhibitors has been a major research focus. Small molecule inhibitors such as L-658,758 (ref. 12) as well as protein-based inhibitors of NE such as EPI-hNE4/DX-890 (ref. 13,14) have been developed for this purpose. Naturally occurring inhibitors such as α-1 antitrypsin, secretory leukocyte protease inhibitor (SLPI), elafin, and monocyte/NE inhibitor (MNEI) have also attracted a lot of interest. They have a broad protease inhibition spectrum, which is clearly beneficial in the context of CF lung disease where many different proteases are involved in the degradation of the lung tissue. In addition, some of these natural antiproteases have other properties, which could contribute to the reduction of lung tissue degradation. SLPI and elafin, for instance, have been demonstrated to possess anti-bacterial as well as anti-inflammatory properties.15, 16, 17, 18
One major limitation to the use of natural antiproteases as therapeutic drugs for the treatment of CF lung disease is their susceptibility to cleavage by proteases.19, 20 In the CF lung where protease levels are very high, many endogenous protease inhibitors are found in a cleaved, inactive form.10, 11 Engineering antiproteases to make them resistant to proteolytic degradation could be a way of enhancing their therapeutic profile to a sufficient level to turn them into marketed drugs.
SLPI, a member of the lung antiprotease screen particularly abundant in the upper airways and a potent inhibitor of NE,21 was demonstrated to be cleaved by NE in its N-terminal domain at positions Ser15-Ala16 and Ala16-Gln17 in the lungs of CF patients infected with P. aeruginosa.10 In this study, we have developed new ways to improve SLPI’s stability, which may improve its therapeutic potential for the treatment of CF lung inflammation.
Results
Design of SLPI variants resistant to cleavage by neutrophil elastase
The determination of the NE cleavage site at positions Ser15-Ala16 and Ala16-Gln17 in the amino-acid sequence of human SLPI-wild type (SLPI-WT) by Weldon et al.10 paved the way for the design of SLPI variants resistant to degradation by this protease. Taking advantage of the key role played by the amino-acid at the P1 position of a protease cleavage site in the determination of the susceptibility of the substrate to cleavage by the protease,22 variants resistant to cleavage by a given protease can be conveniently engineered by a simple change of the amino-acid at the P1 position of the cleavage site.23 The MEROPS database24 provides a list of NE substrates and their amino-acid composition at the cleavage site. This information was used to select the amino-acids best suited to replace those at the P1 positions of the NE cleavage sites in the SLPI sequence. Two amino-acids, tryptophan and histidine, were never found at the P1 position of the cleavage site in the 482 NE substrates listed in the MEROPS database. However, we selected glycine (only found to be present at the P1 position of an NE substrate in two occurrences; Figure 1a) to replace serine and alanine at the P1 position of the two NE cleavage sites in the SLPI amino-acid sequence, owing to a reduced likelihood of disruption of the overall protein conformation with this amino-acid. Two SLPI variants were engineered by site-directed mutagenesis. As illustrated in Figure 1b, the first variant (SLPI-A16G) has a glycine residue instead of an alanine residue at the P1 position of the preferred Ala16-Gln17 NE cleavage site.10 In the second variant (SLPI-S15G-A16G), the amino-acids at the P1 positions of the two NE cleavage sites were replaced by glycine residues.
Mutation of neutrophil elastase (NE) cleavage sites in recombinant secretory leukocyte protease inhibitor (SLPI). (a) The relative amino-acid frequency at the P1 position of NE cleavage sites identified in human SLPI10 was determined using the MEROPS database.24 Gly was selected to replace the Ser 15 and Ala16 residues at the P1 position in the cleavage sites of SLPI by NE as Gly is rarely found at the P1 position of NE substrates. (b) The positions of NE cleavage sites in SLPI are indicated by the arrows between Ser15-Ala16 and between Ala16-Gln17. The cleavage sites were mutated to Gly16-Gln17 for SLPI-A16G and Gly15-Gly16 for SLPI-S15G-A16G. The mutations are indicated in underlined bold type. WT, wild type.
Expression and purification of recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants
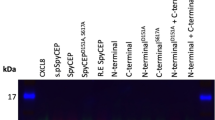
SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were expressed in a bacterial system, using M15 [pREP4] Escherichia coli cells as a host and pQE30 as an expression vector. In this system, the recombinant proteins were expressed with an N-terminal His6-tag for convenient purification by immobilized metal ion affinity chromatography. After purification, all three recombinant proteins were isolated in similar yields (1.3–1.9 mg l−1 of culture). SLPI-WT and its two variants gave bands of the expected molecular weight (ca. 13 kDa) when analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and could be detected by both anti-SLPI and anti-His antibodies by western blotting, confirming the integrity of the proteins (Figure 2). The purity of all three proteins was confirmed by SDS-PAGE analysis followed by staining with Coomassie Brilliant Blue (Figure 2a). The identity was also confirmed by western blotting with anti-SLPI and anti-His antibodies (Figure 2b, c).
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) analysis of purified secretory leukocyte protease inhibitor-wild type (SLPI-WT), SLPI-A16G and SLPI-S15G-A16G. SLPI variants were expressed as N-terminal His6-tagged recombinant proteins within the pQE30 expression vector in M15 [pREP4] Escherichia coli and purified by immobilized metal ion affinity chromatography. Purified SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were analyzed by SDS-PAGE on 15% (w v−1) SDS-PAGE gels under reducing Laemmli conditions. (a) Gels were stained with Coomassie Brilliant blue for total protein analysis. (b) Proteins were transferred onto nitrocellulose membrane and SLPI was detected with a biotinylated anti-SLPI antibody. (c) Proteins were transferred onto nitrocellulose membrane and SLPI was detected with a rabbit anti-His tag antibody.
Inhibition of NE by SLPI-A16G and SLPI-S15G-A16G variants
To determine if the mutations engineered in SLPI amino-acid sequence had any effect on its antiprotease activity, an NE activity assay was carried out where recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were incubated at 37 °C with NE in the presence of a fluorogenic peptide substrate specific for NE. All proteins were able to fully inhibit NE in similar molar ratios (data not shown).
Interaction of SLPI variants with NF-κB DNA binding sites
The ability to bind and block nuclear factor-κB (NF-κB) DNA binding sites in the promoter regions of target genes involved in the inflammatory response is an important mechanism through which SLPI exerts its anti-inflammatory properties.25 Previous work has demonstrated that this ability is abrogated following cleavage of SLPI by NE.10 To determine if the mutations engineered in SLPI amino-acid sequence had any effect on its ability to bind to NF-κB DNA binding sites, SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were incubated with an NF-κB consensus oligonucleotide and the formation of SLPI–DNA complexes was monitored by electrophoretic mobility shift assay. Bands corresponding to SLPI–DNA complexes were detected for all three recombinant proteins, suggesting that the variants retained the ability to bind to NF-κB DNA binding sites and interfere with the pro-inflammatory pathways (Figure 3).
Binding of secretory leukocyte protease inhibitor (SLPI) and the SLPI variants to DNA. SLPI-wild type (SLPI-WT), SLPI-A16G and SLPI-S15G-A16G (1 μg) were incubated with a biotinylated consensus nuclear factor-κB (NF-κB) DNA oligonucleotide, electrophoresed on a 15% polyacrylamide gel, and transferred onto nitrocellulose membrane. SLPI–NF-κB oligonucleotide complexes were detected by incubating the blot with streptavidin–horseradish peroxidase and visualized using a chemiluminescent substrate.
Binding of SLPI variants to P. aeruginosa LPS
The binding of SLPI to bacterial lipopolysaccharide (LPS) and the possible ensuing disruption of the bacterial membrane are thought to be responsible for SLPI's anti-bacterial properties.26 This ability to bind LPS is lost upon cleavage of SLPI by NE.10 To see if the mutations engineered in the SLPI amino-acid sequence could have affected its ability to bind bacterial LPS, the binding of all three recombinant proteins to P. aeruginosa LPS was tested by indirect enzyme-linked immunosorbent assay (ELISA). SLPI-A16G and SLPI-S15G-A16G variants, as well as SLPI-WT, all showed a dose-dependent binding to P. aeruginosa LPS, suggesting that the mutations in the SLPI amino-acid sequence did not alter its capacity to interact with bacterial LPS (Figure 4).
Lipopolysaccharide (LPS) binding properties of SLPI variants. Serial dilutions of secretory leukocyte protease inhibitor-wild type (SLPI-WT) and its SLPI-A16G and SLPI-S15G-A16G variants were analyzed via enzyme-linked immunosorbent assay (ELISA) to determine the relative LPS binding properties of the purified proteins. Biotinylated Pseudomonas aeruginosa LPS bound to SLPI was calculated as the increase in absorbance at 405 nm. Data presented for each SLPI protein are corrected with the background absorbance readings obtained from wells coated with diluent only. OD, optical density.
Effects of excesses of NE and CF sputum on recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants
To determine if the SLPI variants were resistant to degradation by NE, equal amounts of active recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were incubated with a 10-fold molar excess of NE at 37 °C and samples were taken at various timepoints and analyzed by SDS-PAGE and western blotting with both anti-SLPI and anti-His antibodies. Recombinant SLPI-WT was quickly degraded in the presence of an excess of NE (Figure 5a). Both SLPI-A16G and SLPI-S15G-A16G mutants proved much more resistant to degradation by NE with only partial cleavage of SLPI-S15G-A16G evident (Figure 5a). To further demonstrate the clinical relevance of the two SLPI variants, equal amounts of active recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were incubated with CF patient sputum. As in experiments involving incubation with purified NE, recombinant SLPI-WT was quickly degraded (Figure 5b). The two SLPI variants proved again more resistant to degradation by CF patient sputum compared with recombinant SLPI-WT, and significant amounts of protein could still be detected following incubation (Figure 5b). The density of each SLPI band was evaluated using densitometry and confirmed a greater decrease of the SLPI-WT protein compared with SLPI-A16G and SLPI-S15G-A16G following incubation with NE (Figure 5c) or CF sputum (Figure 5d).
Susceptibility of purified secretory leukocyte protease inhibitor (SLPI) to cystic fibrosis (CF) sputum and neutrophil elastase (NE) proteolytic cleavage. Recombinant SLPI-wild type (SLPI-WT) and its SLPI-A16G and SLPI-S15G-A16G variants were incubated with a (a) 10-fold molar excess of NE or (b) pooled CF sputum for 8 h at 37 °C. Samples were analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and western blotting with an anti-His tag antibody. Each result for (c) NE and (d) CF sputum were analyzed by densitometry.
Effect of SLPI-WT and SLPI-A16G in an in vivo model of pulmonary infection
We have previously demonstrated significant cleavage of SLPI by NE in the lungs of CF patients infected with P. aeruginosa.10 Following on from our experiments in Figure 5 demonstrating increased resistance of SLPI-A16G to cleavage by NE and CF sputum compared with SLPI-WT, we tested the effect of both proteins in an in vivo model of pulmonary infection induced by instillation of a clinical strain of P. aeruginosa isolated from the lungs of a patient with CF. SLPI-A16G was chosen over SLPI-S15G-A16G as it appeared to be more stable in incubations with NE and pooled CF sputum. Although we did not demonstrate a reduction in bacterial counts in the mice treated with SLPI-WT and SLPI-A16G vs. untreated mice (data not shown), we did observe a significant decrease in neutrophil recruitment to the lungs of mice treated with SLPI-A16G vs. mice instilled with P. aeruginosa alone (Figure 6a). In contrast, mice treated with SLPI-WT did not exhibit a decrease in lung neutrophil recruitment (Figure 6a). To explain this decrease in neutrophil recruitment, we measured serum levels of the neutrophil chemokine keratinocyte chemoattractant (KC) (Figure 6b). KC levels were significantly decreased in the serum of mice treated with SLPI-A16G but not in the serum of mice treated with SLPI-WT. Other cytokines/chemokines were measured in lung homogenate (Supplementary Figure 1 online—tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), interleukin-6 (IL-6), KC, and macrophage inflammatory protein-2 (MIP-2)) and serum (Supplementary Figure 2 —IL-1β, IL-6, and MIP-2) but were shown not to be significantly decreased in Pseudomonas-infected SLPI-WT vs. SLPI-AG groups.
Secretory leukocyte protease inhibitor (SLPI)-A16G attenuates pulmonary neutrophil infiltration in a mouse model of Pseudomonas aeruginosa infection. C57BL/6 mice received an intranasal administration of saline or P. aeruginosa Q502 (PA), in combination with an intraperitoneal injection of saline, SLPI-wild type (WT) or SLPI-A16G (n=5 per group). After 24 h, (a) pulmonary neutrophil counts were characterized by flow cytometry as CD11b+Gr1+, and (b) serum keratinocyte chemoattractant (KC) levels were quantified by enzyme-linked immunosorbent assay (ELISA). *P<0.05; **P<0.01 vs. PA.
Discussion
SLPI has previously been used in a clinical study in CF patients leading to reduced NE activity and neutrophil levels in the lungs of these patients.27 However, we have previously shown that during Pseudomonas infection in the CF lung, elevated levels of NE are responsible for the proteolytic cleavage of SLPI.10 Two NE cleavage sites in SLPI were identified between residues Ser15-Ala16 and between Ala16-Gln17. Based on this information, we designed variants of SLPI that we hypothesized would be more resistant to degradation by NE, speculating that this could perhaps improve SLPI’s potential as a therapeutic. We introduced substitutions into the SLPI sequence at the NE cleavage sites to reduce cleavage susceptibility. The resulting proteins (SLPI-A16G and SLPI-S15G-A16G) were successfully more resistant to cleavage by NE and Pseudomonas-infected CF sputum, and, in addition, retained many of the features of native SLPI.
With the use of the Pseudomonas infection model of lung inflammation, we have demonstrated that the SLPI-A16G variant displayed enhanced anti-inflammatory properties when compared with the native SLPI-WT protein, as indicated by a significant reduction in inflammatory cells within the lungs, specifically neutrophils. Neutrophilic influx to the respiratory tract is characteristic of the initial stages of acute pulmonary infection and is associated with disruption of the alveolar–capillary barrier and lung tissue damage.28, 29 Bacterial infection is known to upregulate the expression of key neutrophil chemokines including KC and MIP-2. However, in this current investigation, we noted that only KC levels were significantly reduced in mice treated with the SLPI-A16G mutant, which was not the case in mice treated with SLPI-WT. Other key chemokines and cytokines (TNF-α, MIP-2, IL-6, IL-1β) were not reduced in mice treated with either SLPI-A16G or SLPI-WT (data not shown). We postulate that this reduction in KC levels in mice treated with SLPI-A16G may be related to the enhanced cleavage resistance and therefore sustained anti-inflammatory effect of this variant compared with the native SLPI-WT protein.
We have previously demonstrated that native recombinant SLPI can inhibit LPS-induced IL-8 production by macrophages, but in our in vivo infection model this anti-inflammatory effect of native SLPI is not evident, most likely because of the proteolytic degradation of SLPI by increased levels of NE. We have observed similar effects when we mutated the SLPI-related WFDC protein, elafin, to enhance its stability. In that study, we found that a more NE-resistant variant of elafin (GG-elafin) could also significantly reduce neutrophil recruitment in a mouse model of LPS-induced lung inflammation compared with WT elafin.30 However, in contrast to the current SLPI study, we found that GG-elafin did not reduce KC levels. This may be related to the fact that SLPI and elafin have different anti-inflammatory effects. However, it may also be because of the use of different models of inflammation in the two studies—Pseudomonas- vs. LPS-induced inflammation.
One of the limitations of this study is the use of an acute lung infection model to replicate what happens in a chronic lung infection-based disease such as CF. Future studies may involve evaluation of SLPI-A16G and SLPI-WT in a relevant chronic inflammation model such as the βENaC-transgenic model, which reproduces many of the features of CF-like lung disease.31 Another unexpected effect of SLPI-WT and SLPI-A16G in this study was the absence of any reduction in colony-forming units in the in vivo model of infection. SLPI has previously been shown to display anti-bacterial activity against Gram-negative bacteria such as P. aeruginosa.32 However, to our knowledge, SLPI’s anti-bacterial activity in in vivo models of lung infection has not been evaluated and there may be no effect of SLPI against bacteria in vivo.
Overall, our findings indicate that the SLPI-A16G and SLPI-S15G-A16G variants we have engineered are more resistant to protease degradation, while retaining antiprotease and anti-inflammatory properties similar to the SLPI-WT protein. These SLPI variants may hold enhanced therapeutic potential. In particular, we have shown that SLPI-A16G may be of therapeutic benefit in reducing the potentially damaging inflammatory response to infection in the lung, as demonstrated by its increased effectiveness in a murine model of pulmonary infection compared with the proteolytically sensitive SLPI-WT protein.
Methods
Cloning of SLPI variants. pET32c-SLPI was a kind gift from Dr Cantin (University of Sherbrook, Sherbrooke, QC, Canada). The DNA sequence encoding for human SLPI-WT was cloned into the KpnI and HindIII restriction sites of the pQE30 expression vector (Qiagen, Manchester, UK) and this plasmid is referred to as pQE30-SLPI-WT. For each SLPI variant, the synthesis of the mutant strand was performed by PCR using 25 ng of pQE30-SLPI-WT plasmid, 125 ng of the relevant forward and reverse primers (Table 1), 2.5 U of PfuTurbo DNA polymerase and 1 μl of dNTP mix, and 5 μl of 10 × reaction buffer as required in a final volume of 50 μl as per the Quik-Site Directed Mutagenesis Kit (Agilent Technologies LDA UK, Stockport, UK). This mix was then subjected to PCR under the conditions of 30 s at 95 °C, 16 cycles of 30 s at 95 °C, 1 min at 55 °C, and 4 min 30 s at 68 °C. After cooling down the reaction to 37 °C, 10 U of DpnI (New England Biolabs, Hitchin, UK) were added to the PCR mix and the parental strands were digested at 37 °C for 1 h. The digestion products were then used to transform E. coli XL1-Blue supercompetent cells (Agilent Technologies LDA UK). The success of the site-directed mutagenesis was verified by DNA sequencing, and, for each SLPI variant, a single clone was used for all subsequent experiments. The plasmids encoding for the SLPI variants SLPI-A16G and SLPI-S15G-A16G are referred to as pQE30-SLPI-A16G and pQE30-SLPI-S15G-A16G, respectively.
Expression of recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants in M15 [pREP4] E. coli. M15 [pREP4] E. coli cells (Qiagen) were transformed with the pQE30-SLPI-WT, pQE30-SLPI-A16G, and pQE30-SLPI-S15G-A16G plasmids and grown overnight with shaking at 37 °C in Luria-Bertani medium (5 ml) supplemented with 100 μg ml−1 ampicillin and 25 μg ml−1 kanamycin (Sigma-Aldrich, Dorset, UK). These overnight cultures (2.5 ml) were used to inoculate Luria-Bertani (500 ml) supplemented with 100 μg ml−1 ampicillin and 25 μg ml−1 kanamycin and prewarmed to 37 °C. The cultures were grown with shaking at 37 °C until OD600 (optical density at 600 nm) reached 0.6. Expression of the recombinant proteins was then induced with IPTG (isopropylthio-β-galactoside; 1 mM final concentration). The cultures were incubated at 37 °C with shaking for another 4 h before the cells were harvested by centrifugation (4,000 r.p.m. for 30 min at 4 °C). Cells pellets awaiting purification were stored at −80 °C.
Purification of SLPI-WT, SLPI-A16G, and SLPI-S15G-A16G. Cell pellets were thawed on ice and then resuspended in lysis buffer (40 ml) containing 8 M urea, 1 mM β-mercaptoethanol, 500 mM NaCl, 5 mM imidazole, and 20 mM sodium phosphate, pH 8.0. The cells were lysed for 2 h at room temperature with shaking. The cell lysates were clarified by centrifugation at 4,500 g for 1 h, followed by filtration of the supernatants through 0.2 μm filter disks. HiTrap Chelating HP columns (1 ml) (GE Healthcare Life Sciences, Little Chalfont, UK) were mounted on AKTAprime™ chromatography systems (GE Healthcare Life Sciences), charged with Ni2+ ions, and equilibrated with a buffer containing 8 M urea, 1 mM β-mercaptoethanol, 500 mM NaCl, 5 mM imidazole, and 20 mM sodium phosphate, pH 8.0. The clarified cell lysates were loaded onto the columns at 1 ml min−1. Nonspecifically bound material was washed off the column at 1 ml min−1 with 10 column volumes of buffer containing 8 M urea, 1 mM β-mercaptoethanol, 500 mM NaCl, 5 mM imidazole, and 20 mM sodium phosphate, pH 8.0. The denatured recombinant proteins bound onto the column were refolded on the column at a flow rate of 0.5 ml min−1 by gradually removing the urea from the buffer over 15 column volumes. The refolded recombinant proteins bound to the column were then washed at 1 ml min−1 with 10 column volumes of buffer containing 500 mM NaCl, 5 mM imidazole, 20 mM sodium phosphate, pH 8.0, and 1 mM β-mercaptoethanol. Refolded recombinant proteins were eluted off the column at 1 ml min−1 by increasing the concentration of imidazole from 5 to 500 mM in 20 column volumes. Elution fractions (1 ml) were collected and analyzed by SDS-PAGE followed by Coomassie staining. Fractions containing SLPI-WT or its SLPI-A16G and SLPI-S15G-A16G variants were pooled and dialyzed at 4 °C with gentle agitation against 10 volumes of phosphate-buffered saline (PBS), pH 7.4, with two changes of dialysis buffer. The concentrations of the purified recombinant proteins were determined by BCA assay according to the manufacturer’s instructions (Pierce BCA Assay; Fisher Scientific UK, Leicestershire, UK).
Characterization of purified SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants by SDS-PAGE. Purified dialyzed SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants were analyzed by SDS-PAGE on 15% (w v−1) polyacrylamide gels under reducing Laemmli conditions. Gels were stained with Coomassie Brilliant blue for total protein analysis. For western blotting, gels were transferred onto nitrocellulose membrane and the membranes blocked with 3% (w v−1) bovine serum albumin in PBS containing 0.1% (v v−1) Tween-20 for 1 h at room temperature. Probing was carried out with a biotinylated anti-SLPI antibody (1:500 dilution; R&D Systems, Abingdon, UK), followed by incubation with streptavidin-conjugated horseradish peroxidase (1:2,500 dilution; BioLegend, London, UK) in 3% bovine serum albumin (w v−1) in PBS containing 0.1% Tween-20 or with rabbit anti-His antibody (1:1,000 dilution; Insight Biotechnology, Wembley, UK), followed by incubation with horseradish peroxidase-conjugated goat anti-rabbit antibody (1:10,000 dilution; Insight Biotechnology, Wembley, UK). Peroxidase activity was detected using a chemiluminescent substrate (GE Healthcare, Buckinghamshire, UK) and analyzed using the Syngene G:Box and GeneSnap software (SynGene UK, Cambridge, UK).
NE inhibition assays. NE (100 ng; Elastin Products Company, Owensville, MO) was incubated for 10 min at 37 °C alone or with different amounts of recombinant SLPI-WT and its SLPI-A16G or SLPI-S15G-A16G variant in 80 μl (final volume) of 0.5 M NaCl, 100 mM HEPES, pH 7.5, and 0.1% (v v−1) Brij 97. After the addition of 20 μl of N-(methoxysuccinyl)-Ala-Ala-Pro-Val-7-amino-4-methylcoumarin (AAPV-AMC; 100 μM final concentration; Enzo Life Sciences, Exeter, UK), NE activity was monitored by detecting the release of the fluorescent AMC cleavage product (excitation at 360 nm; emission at 465 nm) for 12 min at 37 °C using a 96-well microplate reader (Synergy HT using Gen5 Software; BioTek, Bedfordshire, UK). The change in relative fluorescence units over a 12-min period were calculated for all samples and the results expressed as the percentage of non-inhibited NE.
Electrophoretic Mobility Shift Assay. The binding of SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants to an NF-κB consensus DNA binding site was assessed by electrophoretic mobility shift assay as described previously.10, 25 Recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants (1 μg) were incubated with double-stranded biotinylated NF-κB consensus oligonucleotide 5′-AGTTGAGGGGACTTTCCCAGGC-3′ (100 pmol; Life Technologies, Paisley, UK) and poly(dI–dC).poly(dI–dC) (2 μg; Sigma-Aldrich) for 30 min at room temperature in binding buffer containing 4% (v v−1) glycerol, 0.1 mg ml−1 nuclease-free bovine serum albumin, 1 mM EDTA, 5 mM DTT, 100 mM NaCl, and 10 mM Tris-HCl, pH 7.5 (20 μl). After incubation, the mixtures were electrophoresed on native 15% polyacrylamide gels. The gels were transferred onto 1 μm pore size nitrocellulose membranes in 1 × TBE for 30 min at 380 mA, 100 V, and then crosslinked under UV light for 10 min. A Chemiluminescent Nucleic Acid Detection Kit (Pierce, Fisher Scientific UK) was used to detect the SLPI–DNA complexes, which were analyzed using the Syngene G:Box and GeneSnap software.
LPS-binding assay. Binding of recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants to P. aeruginosa LPS was assessed by indirect ELISA as previously described with some minor modifications.10, 33 Briefly, Greiner high-binding 96-well plates (Greiner Bio-One Ltd., Gloucestershire, UK) were coated with serial dilutions (in serum-free medium) of recombinant SLPI-WT and its SLPI-A16G and SLPI-S15G-A16G variants. Blank wells were coated with diluent alone. The plate was incubated at 37 °C for 2 h and then washed three times with PBS containing 0.05% (v v−1) Tween-20. The plate was blocked for 1 h at room temperature with 200 μl of 1% (w v−1) bovine serum albuminin PBS containing 0.05% (v v−1) Tween-20 per well. Biotinylated P. aeruginosa LPS (100 ng) was then added to each well and the plate was incubated at 37 °C for 3 h. The plate was washed three times before the addition of 100 μl per well of streptavidin-conjugated horseradish peroxidase (1:2,500 dilution). After incubation at room temperature for 20 min, the plate was washed and ABTS single solution substrate (Life Technologies, Paisley, UK) was added. The absorbance at 405 nm of the wells was measured on a Synergy HT plate reader and data presented for each SLPI protein are corrected with the background absorbance readings obtained from wells coated with diluent only.
CF sputum and study approval. Sputum from Pseudomonas-infected CF patients was obtained anonymously from the adult CF Centre at Belfast City Hospital. Sputum samples were in excess to requirements for diagnostic purposes. Permission to use sputum samples, which would have been disposed of, for validation purposes was given by the Director of R&D, Belfast Health and Social Care Trust. Sputum was frozen immediately at −80 °C and used the next day after thawing at room temperature.
Western blot analysis of recombinant SLPI incubated with CF sputum and NE. Each purified SLPI protein (100 ng) was incubated with 10 μl of pooled Pseudomonas-positive CF sputum or 2,500 ng of NE in Tris-buffered saline (total volume of 20 μl) for 8 h at 37 °C as described previously.10 Samples were separated by denaturing SDS-PAGE using 15% polyacrylamide gels and blotted onto nitrocellulose membrane. Membranes were probed using biotinylated anti-SLPI antibody as described above, visualized, and individual SLPI bands were analyzed by densitometry using the Syngene G:Box and GeneSnap software.
Effect of SLPI-WT and SLPI-A16G in an in vivo model of pulmonary infection. Housing and experimentation was carried out in accordance with the Animal (Scientific Procedures) Act 1986 and current guidelines approved by the Queen’s University Ethical Review Committee. A log-phase culture of clinical strain of P. aeruginosa (PA Q502) isolated from the lungs of a CF patient was washed and suspended in sterile endotoxin-free PBS (Sigma-Aldrich) at an OD (600 nm) of 0.5, equating to 3 × 108 CFU. C57BL/6 mice purchased from Charles River Laboratories (Kent, UK) were anesthetized and intranasally inoculated with 20 μl of PA Q502 or saline control. Concurrently, 100 μg of SLPI-WT and SLPI-A16G (or saline control) was administered intraperitoneally. Animals were killed 24 h after infection. The animals were exsanguinated by cardiac puncture; the blood was coagulated at room temperature and then centrifuged at 13,000 g for 10 min. Sera were stored at −20 °C until required for analysis. KC was quantified by ELISA (R&D Systems) following the manufacturer’s instructions.
Perfused, minced lungs were incubated in Iscove’s modified Dulbecco’s medium containing 1 mg ml−1 of collagenase D and 200 μg ml−1 of DNase at 37 °C by centrifugation at 200 g for 1 h. The tissue was then passed through a 70 μm cell strainer, resulting in a single-cell suspension. The cells were washed with sterile PBS and red blood cells were lysed with 3 ml of ACK lysis buffer (8.3 g l−1 NH4Cl, 1 g l−1 KHCO3, 3.72 g l−1 EDTA in distilled water). The cells were counted and incubated with Fc block (1:1,000 in PBS; eBioscience, Hatfield, UK) for 15 min. The cells were stained for flow cytometry with CD45 FITC (1:1,000 in PBS; BioLegend), CD11b APC (1:1,000 in PBS; eBioscience), Gr1 PE (1:1,000 in PBS; eBioscience), and F4/80 PeCy7 (1:500 in PBS; eBioscience) for 20 min in the dark at room temperature. Cells were then washed and acquired using a FACSCanto II (BD Biosciences, Oxford, UK). The data were analyzed using the FlowJo software (Tree Star, Ashland, OR).
Statistical analysis. All data were analyzed using GraphPad Prism 5.0 (GraphPad Software, San Diego, CA) and are reported as mean±s.e.m. or median (interquartile range) where appropriate. Results are representative of n=3, unless otherwise indicated. Means were compared by unpaired t-test, Mann–Whitney test, one-way analysis of variance, or Kruskal–Wallis test as appropriate. P<0.05 was accepted to indicate statistical significance.
References
Chmiel, J.F., Berger, M. & Konstan, M.W. The role of inflammation in the pathophysiology of CF lung disease. Clin. Rev. Allergy Immunol. 23, 5–27 (2002).
Downey, D.G., Bell, S.C. & Elborn, J.S. Neutrophils in cystic fibrosis. Thorax 64, 81–88 (2009).
Mayer-Hamblett, N. et al. Association between pulmonary function and sputum biomarkers in cystic fibrosis. Am. J. Respir. Crit. Care Med. 175, 822–828 (2007).
Murray, T.S., Egan, M. & Kazmierczak, B.I. Pseudomonas aeruginosa chronic colonization in cystic fibrosis patients. Curr. Opin. Pediatr. 19, 83–88 (2007).
Courtney, J.M., Ennis, M. & Elborn, J.S. Cytokines and inflammatory mediators in cystic fibrosis. J. Cyst. Fibros. 3, 223–231 (2004).
Van Der Vliet, A. et al. Myeloperoxidase and protein oxidation in cystic fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 279, L537–L546 (2000).
Voynow, J.A., Fischer, B.M. & Zheng, S. Proteases and cystic fibrosis. Int. J. Biochem. Cell Biol. 40, 1238–1245 (2008).
Sly, P.D. et al. Risk factors for bronchiectasis in children with cystic fibrosis. N. Engl. J. Med. 368, 1963–1970 (2013).
Sagel, S.D., Wagner, B.D., Anthony, M.M., Emmett, P. & Zemanick, E.T. Sputum biomarkers of inflammation and lung function decline in children with cystic fibrosis. Am. J. Respir. Crit. Care Med. 186, 857–865 (2012).
Weldon, S. et al. Decreased levels of secretory leucoprotease inhibitor in the Pseudomonas-infected cystic fibrosis lung are due to neutrophil elastase degradation. J. Immunol. 183, 8148–8156 (2009).
Guyot, N. et al. Elafin, an elastase-specific inhibitor, is cleaved by its cognate enzyme neutrophil elastase in sputum from individuals with cystic fibrosis. J. Biol. Chem. 283, 32377–32385 (2008).
Rees, D.D., Brain, J.D., Wohl, M.E., Humes, J.L. & Mumford, R.A. Inhibition of neutrophil elastase in CF sputum by L-658,758. J. Pharmacol. Exp. Ther. 283, 1201–1206 (1997).
Attucci, S. et al. EPI-hNE4, a proteolysis-resistant inhibitor of human neutrophil elastase and potential anti-inflammatory drug for treating cystic fibrosis. J. Pharmacol. Exp. Ther. 318, 803–809 (2006).
Dunlevy, F.K., Martin, S.L., de Courcey, F., Elborn, J.S. & Ennis, M. Anti-inflammatory effects of DX-890, a human neutrophil elastase inhibitor. J. Cyst. Fibros. 11, 300–304 (2012).
Scott, A., Weldon, S. & Taggart, C.C. SLPI and elafin: multifunctional antiproteases of the WFDC family. Biochem. Soc. Trans. 39, 1437–1440 (2011).
Sallenave, J.-M. Secretory leukocyte protease inhibitor and elafin/trappin-2: versatile mucosal antimicrobials and regulators of immunity. Am. J. Respir. Cell Mol. Biol. 42, 635–643 (2010).
Bingle, C.D. & Vyakarnam, A. Novel innate immune functions of the whey acidic protein family. Trends Immunol. 29, 444–453 (2008).
Moreau, T. et al. Multifaceted roles of human elafin and secretory leukocyte proteinase inhibitor (SLPI), two serine protease inhibitors of the chelonianin family. Biochimie 90, 284–295 (2008).
Taggart, C.C., Greene, C.M., Carroll, T.P., O’Neill, S.J. & McElvaney, N.G. Elastolytic proteases: inflammation resolution and dysregulation in chronic infective lung disease. Am. J. Respir. Crit. Care Med. 171, 1070–1076 (2005).
Greene, C.M. & McElvaney, N.G. Proteases and antiproteases in chronic neutrophilic lung disease—relevance to drug discovery. Br. J. Pharmacol. 158, 1048–1058 (2009).
Thompson, R.C. & Ohlsson, K. Isolation, properties, and complete amino acid sequence of human secretory leukocyte protease inhibitor, a potent inhibitor of leukocyte elastase. Proc. Natl. Acad. Sci. US. 83, 6692–6696 (1986).
Krowarsch, D., Cierpicki, T., Jelen, F. & Otlewski, J. Canonical protein inhibitors of serine proteases. Cell. Mol. Life Sci. 60, 2427–2444 (2003).
Markert, Y., Köditz, J., Mansfeld, J., Arnold, U. & Ulbrich-Hofmann, R. Increased proteolytic resistance of ribonuclease A by protein engineering. Protein Eng. 14, 791–796 (2001).
Rawlings, N.D., Barrett, A.J. & Bateman, A. MEROPS: the database of proteolytic enzymes, their substrates and inhibitors. Nucleic Acids Res. 40, D343–D350 (2012).
Taggart, C.C. et al. Secretory leucoprotease inhibitor binds to NF-kappaB binding sites in monocytes and inhibits p65 binding. J. Exp. Med. 202, 1659–1668 (2005).
Hiemstra, P.S. et al. Antibacterial activity of antileukoprotease. Infect. Immun. 64, 4520–4524 (1996).
McElvaney, N.G. et al. Modulation of airway inflammation in cystic fibrosis. In vivo suppression of interleukin-8 levels on the respiratory epithelial surface by aerosolization of recombinant secretory leukoprotease inhibitor. J. Clin. Invest. 90, 1296–1301 (1992).
Maus, U. et al. The role of CC chemokine receptor 2 in alveolar monocyte and neutrophil immigration in intact mice. Am. J. Respir. Crit. Care Med. 166, 268–273 (2002).
Maus, U., Huwe, J., Maus, R., Seeger, W. & Lohmeyer, J. Alveolar JE/MCP-1 and endotoxin synergize to provoke lung cytokine upregulation, sequential neutrophil and monocyte influx, and vascular leakage in mice. Am. J. Respir. Crit. Care Med. 164, 406–411 (2001).
Small, D.M. et al. A functional variant of elafin with improved anti-inflammatory activity for pulmonary inflammation. Mol. Ther. 23, 24–31 (2014).
Mall, M., Grubb, B.R., Harkema, J.R., O’Neal, W.K. & Boucher, R.C. Increased airway epithelial Na+ absorption produces cystic fibrosis-like lung disease in mice. Nat. Med. 10, 487–493 (2004).
Wiedow, O., Harder, J., Bartels, J., Streit, V. & Christophers, E. Antileukoprotease in human skin: an antibiotic peptide constitutively produced by keratinocytes. Biochem. Biophys. Res. Commun. 248, 904–909 (1998).
McLean, D.T.F., Lundy, F.T. & Timson, D.J. IQ-motif peptides as novel anti-microbial agents. Biochimie 95, 875–880 (2013).
Acknowledgements
This work was supported by the Engineering and Physical Sciences Research Council (EP/H031065/1), Department of Employment and Learning (Northern Ireland) and InvestNI Proof of Concept funding (PoC 117), and the European Respiratory Society/GSK Romain Pauwels Award. In addition, the research leading to these results has received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013) under CFMATTERS grant agreement no. 603038. pET32c-SLPI was a kind gift from Dr André Cantin (University of Sherbrooke, Canada). We thank all patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
SUPPLEMENTARY MATERIAL is linked to the online version of the paper
Supplementary information
Rights and permissions
About this article
Cite this article
Camper, N., Glasgow, A., Osbourn, M. et al. A secretory leukocyte protease inhibitor variant with improved activity against lung infection. Mucosal Immunol 9, 669–676 (2016). https://doi.org/10.1038/mi.2015.90
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2015.90