Abstract
Cancer invasion is a complex process requiring, among other events, extensive remodeling of the extracellular matrix including deposition of pro-migratory and pro-proliferative moieties. In recent years, it has been described that while invading through matrices cancer cells can change shape and adapt their migration strategies depending on the microenvironmental context. Although intracellular signaling pathways governing the mesenchymal to amoeboid migration shift and vice versa have been mostly elucidated, the extracellular signals promoting these shifts are largely unknown. In this review, we summarize findings that point to matrikines that bind specifically to the EGF receptor as matricellular molecules that enable cancer cell migrational plasticity and promote invasion.
Similar content being viewed by others
Main
The major part of cancer morbidity and mortality results from both metastatic dissemination and invasion from the primary tumor. The extracellular matrix (ECM) is the first obstacle that solid tumors encounter during this spreading. Matrix remodeling during tumor invasion does not only involve proteolytic degradation of the barrier but also a concomitant synthesis of bioactive matrix molecules, in a process resembling active matrix remodeling during wound healing. This new matrix environment in turn promotes and nurtures cancer cell spreading. Both tumor and stromal cells contribute to these changes, with the matrix components secreted by the tumor cells varying significantly in conjunction with their metastatic potential.1 Many of these proteins have profound effects on cell morphology, inducing weaker states of cell adherence and thus promote migration. In this review, we will concentrate on the recent findings that point toward dysregulation of ECM components that promotes invasion of cancer cells from the primary site by enabling plasticity of migration strategies. In particular, this focused brief missive emphasizes ECM proteins that can bind to the epidermal growth factor receptor (EGFR), thus, subsuming established signaling networks that govern effective migration in various conditions. The wealth of other matricellular molecules that are implicated in carcinogenesis and metastasis, often by regulating adhesion and migration and thus invasion, have been elegantly reviewed elsewhere.2, 3
The EGFR signaling axis is the growth factor system most often implicated in tumor progression via upregulation or activation of the receptor or of its numerous ligands.4 Even though EGFR activation by its traditional soluble ligands leads to both mitogenesis and motogenesis, it is the motility that correlates to tumor progression.5, 6, 7 More recently, EGFR activation by cryptic, ultralow affinity ligands, embedded within ECM molecules, has been recognized.8, 9 These matrikines limit EGFR signaling to the perimembrane area of the cytosol, a mode that is preferential for motility10, 11 and cell survival.12, 13 As these matrix components are upregulated during cancer progression, the role of EGFR in altering tumor behaviors is being re-examined in terms of such ECM-embedded signaling.14, 15, 16 This perspective aims to provide the background for addressing such questions.
Cancer cell invasion programs
Cancer cells are known to use both protease-dependent and protease-independent invasion strategies. During the mesenchymal mode of invasion, in the presence of proteases that can degrade the surrounding ECM,17, 18 movement of cells is a multi-step process: (1) cell polarization and initial protrusion are followed by the attachment at the base of the leading edge to the ECM, (2) the cell surface-localized degradation of ECM generates space into which actomyosin contraction will move the advancing cell body deforming both the cell and the ECM; finally, (3) retraction of the cell rear and turnover of adhesions occur.19, 20 On the other hand, in the absence of significant proteolytic activity or an inability to degrade the surrounding substrate, cancer cells can still invade by using actin contractile force to generate a rounded morphology and amoeboid bleb-like protrusions that push and squeeze cells through spaces in the ECM.17, 18, 21, 22, 23 This type of migration is possible if both the cell body deformability and the porosity of the matrix match so that the cells can fit through the spaces. Cytoskeletal organization and cell adhesion are modulated by the rigidity of the ECM, density and gap size, and orientation of fibers.19 In 3D stiff matrices, mesenchymal migratory force generation is β1 integrin dependent,18 whereas soft matrices do not reinforce focal adhesion (FA) formation and fail to support cell rounding.24
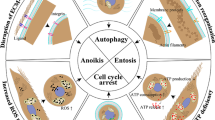
Signaling integrators that control the adoption of either the mesenchymal or the rounded mode of migration are the Rac and Rho/ROCK signaling pathways.17 In the mesenchymal mode of migration, formation of actin-rich lamellipodia is Rac1 dependent.25, 26, 27 Cdc42 and Rac regulate WASP/WAVE proteins that promote the nucleation of actin filaments and the formation of the leading edge.28, 29 Superimposed upon these is the small GTPase Cdc42, which provides for directionality.30, 31 The protruding leading edge is then stabilized by integrin interactions with the ECM and the formation of FAs. Rho and its downstream effector ROCK have been shown to be dispensable for the mesenchymal mode of migration,17 in a situation where Cdc42 can compensate the loss of Rho/ROCK signaled contractility.32 In contrast, the rounded mode of motility is dependent on Rho and ROCK activity,17 where ROCK-dependent myosin light chain (MLC) phosphorylation is crucial for the correct organization of MLC and force generation within the moving cell.22 Phosphorylated MLC increases ATPase activity to promote actin–myosin interactions and contractile force generation. The intracellular pressure results in the rupture of the actomyosin cortex and the formation of membrane blebs.33 After the formation of the bleb, the contractile cortex re-assembles.34 One major difference between mesenchymal and amoeboid movement is therefore the driving force for the formation of protrusions, which are actin polymerization and cytoplasm inflow, respectively. The silencing of ROCK pathway induces an amoeboidal to mesenchymal shift17, 35 and the silencing of Rac induces cells to attain the opposite morphology.35, 36 This mesenchymal to amoeboid transition is summarized in Figure 1.
This plasticity of migrational modes allows great adaptation during invasion and although underlying cellular machinery has been extensively studied, only recently has attention been given to the ECM signals that might induce these shifts.
Matricelular proteins as regulators of migration
The concept of matricellular proteins has been proposed in order to define protein domains from the ECM, which can signal to the surrounding cells.37 It has become appreciated that some of these signals can be provided by cryptic sites within ECM molecules, which are revealed/accessible to cells only after structural or conformational alterations in the components.38, 39 In the course of tumor invasion, matrix alterations because of ECM denaturation, enzymatic breakdown, mechanical forces or protein multimerization and adsorption provide for a plethora of matrycriptic signals. Matricellular proteins can interact with multiple other matrix proteins and cellular receptors and therefore have complex biological functions. Some of the matricellular proteins and their peptide fragments that can signal through growth factor receptors have been denoted as matrikines to emphasize their direct cell signaling capacities.
Matricellular proteins that lessen adhesion, via integrin or growth factor signaling, have a profound influence on cell motility as the intermediate state of cell adhesion favors motility.40, 41 ECM proteins that promote this intermediate state of adhesion, such are tenasicin C, thrombospondin, laminins, and secreted protein-rich in cysteine (SPARC), are increased in expression at the exact sites of remodeling that require cell migration—during embryogenesis, wound healing, inflammation, and tumor invasion. This suggests a role for the matricellular proteins in promoting migration by enabling the intermediate adhesive state.
A mathematical model developed by DeMilla, Barbee, and Lauffenburger predicts that the maximal motility of cells is achieved when the ratio of the transcellular force, achieved through cytoskeletal contractility, and the adhesive strength, achieved through integrin–matrix interactions, is intermediate.41 Weak cell adhesion does not generate sufficient force for cell movement, and excessive adhesion prevents the releasing of the cell from the ECM.42, 43, 44 It must be noted that the assays that test effects of ECM proteins on cell motility impose certain requirements for cytoskeletal organization and adhesion for the motility to be considered successful. Mesenchymal moving cells that form strong adhesions perform better in 2D migrational assays (such as wound-healing assay or live cell tracking on 2D matrices), whereas amoeboid-moving, less adherent, cells move slowly on rigid 2D substrates, but more swiftly in 3D migration assays. Thus, seemingly discrepant findings of the role of a certain ECM protein in cell motility are partly due to different contexts used to ascertain migratory performance. Our recent findings that epidermal growth factor-like repeats (EGF-like; EGFL) of tenascin C (TNC) can promote mesenchymal to amoeboid shift in migration in melanoma cells,15 with the cells expressing the EGFL domain moving slower on 2D substrates than the control melanoma cells, but nevertheless moving faster in 3D environments; and this is without an increase in MMP activities.
This finding impels us to examine other matricellular proteins that have anti-adhesive properties. What is common for these proteins is that they bind multiple cellular receptors and they can induce multiple, sometimes even opposing cellular responses. TNC, Thrombospondin 1 (TSP1), Laminin 5, and SPRC are all anti-adhesive, all can bind multiple different integrins, and all possess EGFL domains or modules. In this review, we posit that these matricellular proteins can dictate the mode of migration, mesenchymal or amoeboid, by signaling cytoskeletal adaptation to the cell surroundings, and generally promoting tumor invasion. This view imposes a demand for targeted therapies that account for the plasticity that enables cells to switch between both modes of motility during invasion, for any hope of success in limiting cancer dissemination.
Stimulatory molecules
There are a large number of molecules that can be considered ‘onco-fetal-wound’ markers, in that they also appear or are upregulated in the matrix during tumor invasion. These molecules are present during development and re-appear during the regenerative phase of wound repair. They not only mark a period of rapid ingrowth of cells of all lineages, but also promote this exuberant expansion both by altering the density of the matrix and directing the cells to migrate. Thus, during tumor invasion, the malignant turn hijacks this physiological processes to promote dissemination. The following will discuss a number of the best-characterized and most strongly mechanistically correlated proteins.
TNC
The physiologic role of TNC lies in establishing interactions between the epithelium and the mesenchyme during embryonic development, tissue differentiation, and wound repair. Therefore, expression of TNC is transient during these periods being strictly regulated.45 Persistent high levels of TNC are present in various tumor tissues, including brain, bone, prostate, intestine, lung, skin, and breast.46
TNC is a hexameric glycoprotein composed of 180–320 kDa monomers (it is actually a homodimer of homotrimers), which are disulfide-linked at their N-termini. The different molecular weights of TNC monomers are the consequence of glycosylation and alternative splicing. Each subunit contains: the N-terminal assembly domain, a domain composed of 14.5 EGFL, a domain composed of a varied number of fibronectin type III-like (FNIII) repeats, and a fibrinogen-like sequence on the C terminus.47, 48, 49, 50, 51, 52
Cells can interact with the FNIII-like domain of TNC via integrins α2β1, α7β1, α9β1, αVβ1, αVβ3, and αVβ6, thus allowing for cell attachment, and via syndecans-1 and -4, and annexin II to signal de-adhesion (reviewed in Erickson and Bourdon51 and Prieto et al53). Therefore, the response to TNC differs depending on the receptor repertoire present on the cell surface. The EGF-like repeats of TNC also have counter-adhesive properties54, 55 and have been shown to bind and signal through the EGFR.8, 10 Interestingly, the binding of TNC EGFL to EGFR preferentially promotes cell migration by limiting receptor signaling to the perimembrane space.11
TNC has been shown to promote cancer invasion by both MMP-dependent and -independent mechanisms.56 TNC induces expression of MMPs 1, 3, 9, and 1356, 57 and the activation of MMP2, and thus there is a positive feedback loop between the induction of MMPs by TNC and its cleavage by these MMPs.58 Interestingly, cleavage sites for all MMPs tested to-date are outside the EGFL repeats domain in the TNC molecule,59 leaving the EGFL intact in the face of increased ECM remodeling. Therefore, TNC is equipped not only to modulate ECM architecture but also to dramatically influence the behavior of cells by exposing its active EGFL matrikine domain.
We found that TNC EGFL induce melanoma cell rounding and decreased adhesiveness through activation of ROCK15 and that this allows transition from the mesenchymal to amoeboid mode of invasion through the dermis. On the other hand, FNIII repeats of TNC have been shown to suppresses Rho A activation while maintaining the level of active Cdc42 thus preventing stress fiber formation.60 As TNC is being deposited at the front of invading cells,15 and amoeboid cell morphology is observed at the fronts of invasion in tumors,61 it is possible that TNC can induce cytoskeletal changes in cancer cells that lead to a shift toward amoeboid movement and allow greater plasticity of invading cells. We speculate that invadopodia that can localize MMPs in the front of migrating cells62 could cleave TNC to expose the EGFL as a mechanism to promote this invasion. It is likely that after proteolytic cleavage, TNC fragments may have distinct signaling activity compared with the full-length TNC protein.
There are other members of the tenascin family, generated by alternative splicing; some of which present multiple EGFL.63 However, these have not been examined for ability to bind and activate EGFR.
Laminin-332 (formerly laminin 5)
Another matrikine protein that can signal via its EGFL-activating EGFR is laminin-332 (Ln-332),9 a widespread constituent of the basement membrane. It is composed of α-3, β-3, and γ-2 chains, coiled together and stabilized by disulfide bonds forming the long arm from which portions of all three chains protrude forming short arms.64 In normal physiological conditions, epithelial cells adhere to Ln-332 through α3β1 and α6β4 integrins and form focal contacts and hemidesmosomes (reviewed in Koshikawa et al65). But, in cases of active remodeling, during wound healing or tumorigenesis, MT1-MMP66 and MMP-267 can cleave Ln-332 and reveal cryptic pro-migratory sites. These cryptic sites were shown to be EGF-like repeats within γ-2 chain that stimulate cancer cell migration in an EGFR-dependent manner.9 On the other hand, the laminin α-3 chain interacts with α3β1 integrin and can stimulate cell adhesion, spreading, and migration,68 which involves Src/FA kinase activation and subsequent Rac1-induced lamellipod extensions.69 β-3 Chain and its cleaved products have also been shown to promote cell migration in multiple cancers (reviewed in Pyke et al70).
Invading cancer cells preferentially express increased amounts of γ-2 chain of Ln-33271 and this is the only chain that can be secreted in the monomeric form.72 Ln-332 γ-2 chain can also be processed by uPA and MMP9,73 where uPAR signaling seems to be essential for production and secretion of Ln-332 itself.74 In cancers of epithelial origin, Ln-332, uPAR and plasminogen activator-inhibitor-type 1 (PAI-1) are upregulated at the invasive fronts,75, 76 with the uPAR and PAI-1 upregulation being promoted in a feed forward manner by EGFR signaling.77 This further supports our model that not only matrix degradation, but also cryptic domains released from matricellular proteins promote migration and possibly motility shift toward amoeboid migration at the leading edges of invasive tumors. In colon adenocarcinoma, addition of Ln-233 activates α3β1 to decrease RhoA activity, which causes α2β1 to α3β1 switch in adhesion and increases attachment to Collagen IV and differentiation of cells into enterocytes.78 A similar observation was made in squamous cell carcinoma cells, where attachment to Ln-233 through α3 integrin caused decrease in RhoA activity, whereas the attachment on collagen I through α2 integrin strongly activated RhoA.79 In this case, α2β1 attachment to collagen decreased, whereas Ln-322 α3β1 integrin activation induced FA disassembly and stimulated migration on 2D-coated surfaces through decrease in RhoA and increase in Cdc42 activity. On the other hand, it has been shown that Ln-233 activates RhoA in keratinocytes on matrices through activation of both α31 and α6β4 and this enables subsequent spreading on collagen via α2β1.80 Depending on the cell type, different integrins can elicit various RhoA levels of activation in response to Ln-332 and this also depends on the other ECM proteins present.
SPARC
SPARC is an ECM protein with highest expression in bone tissue, but distributed throughout other tissues at the sites of remodeling, angiogenesis, and in pathological conditions such as tumorigenesis. SPARC is a 32-kDa protein with an acidic domain, a follistatin-like domain, and an extracellular calcium-binding domain.81, 82 The follistatin-like domain contains three EGFL modules, which are twisted by disulfide bonds,83 and a copper-binding region that interacts with β1 integrin.84 SPARC signaling through αvβ3 and αvβ5 integrins has also been demonstrated.85, 86 Like TNCs, effects of SPARC are context and cell type dependent with seemingly contradictory roles in tumor progression (reviewed in Chlenski and Cohn87). In ovarian, prostate, and colorectal cancers, SPARC expression is downregulated by methylation of the promoter, compared with normal tissues (reviewed in Sage et al88). In these cancers, overexpression of SPARC suppresses growth and survival of cancer cells. On the other hand, in glioma and breast cancer, SPARC expression is increased and it promotes invasion. These different effects on tumor progression can be explained by different requirements of tumor cell–matrix interactions for progression of neoplasms.
SPARC has anti-adhesive properties, inducing cell rounding and FA disassembly, which is induced by the EGFL module of SPARC;89, 90 suggesting that these might signal via the EGFR similar to TNC and laminin 322, although they have not been experimentally tested for such activity. The acidic domain of the molecule also has anti-adhesive properties.91
SPARC can bind integrin-linked kinase and augments fibronectin-induced integrin-linked kinase activation, formation of stress fibers and cell contractility.92 SPARC is also a regulator of the ECM remodeling, it interacts with collagens I, II, III, IV, V, vitronectin, and thrombospondin (reviewed in Sage et al88) and induces MMP-1, -2, -3, and -9 secretion.93, 94 SPARC also directly binds VEGF and PDGF, and interferes with their signaling.95, 96 Therefore, this plethora of effects that SPARC can impose on cancer cells has different effects on progression in different cancer types. In glioma, overexpression of SPARC promotes tumor invasion by increasing MMP production, but also by the activation of RhoA and uPA-uPAR signaling.94
As expected for anti-adhesive domains, deletion of the EGFL module decreases SPARC-induced directional 2D migration on fibronectin, which is p38 mitogen-activated kinase dependent.91 On the other hand, SPARC overexpression in medulloblastoma suppresses activity of Rho, Rac, and Cdc42 and inhibits invasion.97 In ovarian cancer, SPARC abrogates cancer cell adhesion to the peritoneal mesothelial cells and ECM, thus inhibiting implantation and cancer progression.98 These seemingly opposite effects are a consequence of a requirement for a certain level of adhesion and the adequate mode of migration that is needed for invasion through different matrices. Thus, based on environment, SPARC-induced increased de-adhesiveness could promote or ameliorate invasion. Interestingly, SPARC treatment of endothelial cells decreases production of TSP1, but induces production of plasminogen activator inhibitor 1,99 with these two ECM proteins driving mesenchymal to amoeboid migration transition by these changes in levels.
Thrombospondins
TSP1 is a 420-kDa trimer composed of three identical 145 kDa peptides linked by disulfide bonds. Like SPARC and TNC, TSP1 is expressed at the sites of tissue remodeling, associated with wound healing and tumorigenesis (reviewed in Liu et al100 and Murphy-Ullrich and Poczatek101). It contains N-terminal globular domain, inter-chain disulfide knot, segment homologous to pro-collagen I, three properdin repeats, three EGFL, seven calcium-binding repeats, and carboxy-terminal L-lectin-like domain.100 Its role in tumor progression has been controversial, as findings that support both promotion and suppression exist. This is, again, a consequence of multiple binding partners of TSP1 and especially its ability to bind and activate latent complexes of TGFβ.102 TSP 1 binds syndecans-1103 and -4104 and multiple integrins-α6β1, α4β1, α9β1, αvβ3, and α3β1.105, 106 It can also indirectly modulate integrin signaling. For example, the C-terminal domain of TSP1 binds to integrin-associated protein and modulates αvβ3 signaling.107, 108 TSP1 is also an endogenous angiogenesis inhibitor109 (reviewed in Fontana et al110), but some cancer cells can override this inhibitory effect.111, 112 Overexpression of TSP1, thus, in some cancers promotes113, 114 while in others, inhibits invasion and metastasis (reviewed in Bein and Simons115). TSP1 binds MMP2 and is believed to inhibit its activity,116 whereas it upregulates MMP-9 expression.117 The N-terminal domain of TSP1 induces disassembly of FAs,118, 119 which is stimulated by RhoA inactivation through FA kinase and activation of ERK and PI-3-kinase.120 TSP1-induced FA disassembly is signaled through calreticulin and can promote migration of endothelial cells and fibroblasts.121 EGFL repeats of TSP1 were found to activate EGFR and increase motility, but direct binding was not demonstrated, and MMP9 activity was required.122 Interestingly, TSP1 increases secretion of matrix-bound PAI-1 in breast and lung cancers,123, 124 mediated through TGFβ activation.124 PAI-1 has recently been found to promote mesenchymal to amoeboid migration transition by RhoA-ROCK-MLC pathway.125 TSP1 also increases expression of other members of plasminogen system, uPA and uPAR126 and thus increases invasion.127
Thrombospondin 2 is encoded by a different gene and has different temporal and spatial distribution compared with TSP1 (reviewed in Angelucci et al128). This isoform has been shown to be a matricellular protein that modulates both MMPs and growth factor signaling (VEGF in particular)129 to inhibit angiogenesis in wound repair and tumor progression. However, this isoform has not been shown to interact with EGFR, the subject of this review.
Osteopontin (OPN)
OPN, a matricellular protein initially found in bone and thus also named bone sialoprotein-1, binds integrin β1 and via that colocalizes with EGFR. OPN permissive and even enhancing effects on tumor cells appear to need EGFR signaling, but this is secondary to co-clustering and increased EGFR and TGFα levels.130, 131
Fibulins
Fibulins are a family of secreted glycoproteins with modular structure132 that contain calcium-binding epidermal growth factor-like (EGFL) modules133 and can also modulate cell adhesion through integrin signaling (reviewed in Obaya et al134 and Camaj et al135). As in the case of many modular matricellular proteins that can interact with various other ECM components, fibulins have been described to have both pro- and anti-tumor progression activities (reviewed in Yates et al136).
Although it has not been conclusively explored whether fibulins can bind EGFR, a related molecule EFEMP1 appears to bind and activate EGFR.137 Whether this family of proteins has an impact on cancer cell migration or invasion, given that its structure implies possible integration of signals similar to the above-discussed molecules, awaits further exploration.
Suppresive molecules
The ECM of quiescent, mature tissue contains numerous molecules that suppress the proliferative and migratory properties of the resident cells, and steer them toward a differentiated state. These molecules appear late in development after the formative burst, and during the transition from regenerative to resolving phase of wound repair.138 A similar but inverted transition occurs in tumor progression.139 At this emergence of invasiveness, these suppressive ECM components are decreased. Key among these are the structural collagens, which have been reviewed extensively elsewhere,140, 141, 142 and a family of small leucine-rich proteoglycans.143 The best characterized of the latter is decorin (DCN), the only molecule we will explore in detail due to its description as an EGFR-binding molecule.
DCN
DCN is the small (40 kDa) leucine-rich proteoglycan synthesized chiefly by stromal fibroblasts, endothelial cells under stress, and smooth muscle cells.16 Unlike above-mentioned matricellular proteins, DCN has strictly anti-tumor activities. DCN consists of a protein core and a single chondroitin/dermatan sulfate glycosaminoglycan chain attached to a serine near the N terminus.144 It is mostly found in collagen-rich connective tissues,145 where it interacts with high affinity with collagen fibers (‘decorates’) and is involved in collagen fibrilogenesis.146, 147, 148
DCN can bind to and inhibit the activation of a number of growth factor receptors including EGFR,149 Met receptor,150 PDGF receptor,151 and IGF-1R.152 It can also sequester TGFβ family members into the ECM, as there are two binding sites for TGFβ in the DCN core.153 DCN can be considered an endogenous matrix-centric pan-kinase inhibitor16 and along with TGFβ sequestering function, which leads to tumor immunosupression and growth retardation, has been proposed to be ‘a guardian from the matrix’ to draw a comparison to ‘guardian of the genome’ p53.16 Notably, the cooperation between DCN and p53 has already been established.154 DCN inhibits cancer cell migration via inhibition of multiple growth factor receptors and by upregulation of E-cadherin.155
Quiescent fibroblasts are the main source of DCN, as proliferating fibroblasts produce significantly lower levels.156 The disruption of DCN leads to abnormal collagen fibril morphology and tissue fragility.147 In cancer, DCN is generally downregulated and can be found in peritumoral stroma, but not in tumor cells or dense tumor tissue (reviewed in ref. 154).
In recent years DCN has been explored as therapeutic agent, both alone and in combinational cancer therapy.154 Our group has looked at effect of DCN on melanoma cell migration and found that it drastically inhibits it both in 2D and 3D migration assays (Grahovac and Wells, unpublished observations). This opens an avenue for further exploration of effects of DCN in presence of matricellular proteins that promote cancer cell migration and possibility of normalization of the cancer ECM by induction or administration of DCN.
Summary
Matricellular proteins are important regulators of tissue organization and cell activation status, and consequently their altered expression during tumorigenesis greatly impacts cancer progression. What is common for all of the above-discussed matricellular proteins that promote migration and invasion is that, in addition to regions binding to β1 integrin, they all have EGFL domains. TNC, TSP1, and Ln-332 have EGFL that have been shown to bind and activate EGFR, whereas SPARC and fibulins have EGFL that have not been examined for growth factor receptor binding. Furthermore, they all bind syndecans and induce or activate various MMPs that may in turn clip the molecules to expose these cryptic signaling moieties. TSP1 and SPARC also activate uPA/uPAR signaling and the generation of active HGF/Scatter Factor.94, 126 All of the described matricellular proteins can lessen the adhesiveness of the cells and enable signaling that can promote both mesenchymal or amoeboid cell movement depending on the ECM surroundings (Figure 2).
TNC, SPARC, TSP1, and Ln-322 are all expressed in the sites of active tissue remodeling, some distinctly present at the invasion borders. For example, Ln-322 γ-2 chains and TNC are co-deposited and form a physical complex at the invasion fronts and carcinoma-stroma borders.155,156 We speculate that this localization is enabling shift toward amoeboid mode of migration as an adaptation to the previously un-encountered ECM.
The notion that the same matricellular protein can signal mesenchymal or amoeboid migration depending on the context imposes a requirement for inhibiting both modes of migration to limit invasion. Simultaneous inhibition of both MMPs and RhoA/ROCK signaling pathway could work toward that goal.
Another important signaling factor that sits at the crossroads of matricellular proteins is TGFβ. TGFβ induces production of SPARC and TNC, but decreases production of DCN. TSP1 binds and activates latent TGFβ complexes, whereas DCN can sequester TGFβ from the ECM, and SPARC indirectly diminishes TGFβ activity. This raises question whether TGFβ is the major regulator of the tumor stroma and whether normalization of the ECM through TGFβ manipulation holds promise as a means for better cancer treatment.
References
Naba A, Clauser KR, Hoersch S et al. The matrisome: in silico definition and in vivo characterization by proteomics of normal and tumor extracellular matrices. Mol Cell Proteomics 2012;11:M111 014647.
Wong GS, Rustgi AK . Matricellular proteins: priming the tumour microenvironment for cancer development and metastasis. Br J Cancer 2013;108:755–761.
Chong HC, Tan CK, Huang RL et al. Matricellular proteins: a sticky affair with cancers. J Oncol 2012;2012:351089.
Wells A . EGF receptor. Int J Biochem Cell Biol 1999;31:637–643.
Wells A . Tumor invasion: role of growth factor-induced cell motility. Adv Cancer Res 2000;78:31–101.
Wells A, Grahova J, Wheeler S et al. Targeting tumor cell motility as a strategy against invasion and metastasis. Trends Pharmacol Sci 2013;34:283–289.
Condeelis JS, Wyckoff JB, Bailly M et al. Lamellipodia in invasion. Semin Cancer Biol 2001;11:119–128.
Swindle CS, Tran KT, Johnson TD et al. Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. J Cell Biol 2001;154:459–468.
Schenk S, Hintermann E, Bilban M et al. Binding to EGF receptor of a laminin-5 EGF-like fragment liberated during MMP-dependent mammary gland involution. J Cell Biol 2003;161:197–209.
Iyer AK, Tran KT, Borysenko CW et al. Tenascin cytotactin epidermal growth factor-like repeat binds epidermal growth factor receptor with low affinity. J Cell Physiol 2007;211:748–758.
Iyer AK, Tran KT, Griffith L et al. Cell surface restriction of EGFR by a tenascin cytotactin-encoded EGF-like repeat is preferential for motility-related signaling. J Cell Physiol 2008;214:504–512.
Fan VH, Tamama K, Au A et al. Tethered epidermal growth factor provides a survival advantage to mesenchymal stem cells. Stem Cells 2007;25:1241–1251.
Rodrigues M, Blair H, Stockdale L et al. Surface tethered epidermal growth factor protects proliferating and differentiating multipotential stromal cells from FasL-induced apoptosis. Stem Cells 2013;31:104–116.
Anderson AR, Weaver AM, Cummings PT et al. Tumor morphology and phenotype evolution driven by selective pressure from the microenvironment. Cell 2006;127:905–915.
Grahovac J, Becker D, Wells A . Melanoma Cell Invasiveness Is Promoted at Least in Part by the Epidermal Growth Factor-Like Repeats of Tenascin-C. J Invest Dermatol 2012;133:210–220.
Neill T, Schaefer L, Iozzo RV . Decorin: a guardian from the matrix. Am J Pathol 2012;181:380–387.
Sahai E, Marshall CJ . Differing modes of tumour cell invasion have distinct requirements for Rho/ROCK signalling and extracellular proteolysis. Nat Cell Biol 2003;5:711–719.
Wolf K, Mazo I, Leung H et al. Compensation mechanism in tumor cell migration: mesenchymal-amoeboid transition after blocking of pericellular proteolysis. J Cell Biol 2003;160:267–277.
Friedl P, Wolf K . Plasticity of cell migration: a multiscale tuning model. J Cell Biol 2010;188:11–19.
Wolf K, Friedl P . Extracellular matrix determinants of proteolytic and non-proteolytic cell migration. Trends Cell Biol 2011;21:736–744.
Friedl P . Prespecification and plasticity: shifting mechanisms of cell migration. Curr Opin Cell Biol 2004;16:14–23.
Wyckoff JB, Pinner SE, Gschmeissner S et al. ROCK- and myosin-dependent matrix deformation enables protease-independent tumor-cell invasion in vivo. Curr Biol 2006;16:1515–1523.
Zaman MH, Trapani LM, Sieminski AL et al. Migration of tumor cells in 3D matrices is governed by matrix stiffness along with cell-matrix adhesion and proteolysis. Proc Natl Acad Sci USA 2006;103:10889–10894.
Ulrich TA, de Juan Pardo EM, Kumar S . The mechanical rigidity of the extracellular matrix regulates the structure, motility, and proliferation of glioma cells. Cancer Res 2009;69:4167–4174.
Ridley AJ, Paterson HF, Johnston CL et al. The small GTP-binding protein rac regulates growth factor-induced membrane ruffling. Cell 1992;70:401–410.
Ridley AJ, Hall A . The small GTP-binding protein rho regulates the assembly of focal adhesions and actin stress fibers in response to growth factors. Cell 1992;70:389–399.
Nobes CD, Hall A . Rho, rac, and cdc42 GTPases regulate the assembly of multimolecular focal complexes associated with actin stress fibers, lamellipodia, and filopodia. Cell 1995;81:53–62.
Miki H, Suetsugu S, Takenawa T . WAVE, a novel WASP-family protein involved in actin reorganization induced by Rac. EMBO J 1998;17:6932–6941.
Rohatgi R, Ma L, Miki H et al. The interaction between N-WASP and the Arp2/3 complex links Cdc42-dependent signals to actin assembly. Cell 1999;97:221–231.
Ridley AJ . Rho GTPases and cell migration. J Cell Sci 2001;114 (Pt 15):2713–2722.
Chou J, Burke NA, Iwabu A et al. Directional motility induced by epidermal growth factor requires Cdc42. Exp Cell Res 2003;287:47–56.
Wilkinson S, Paterson HF, Marshall CJ . Cdc42-MRCK and Rho-ROCK signalling cooperate in myosin phosphorylation and cell invasion. Nat Cell Biol 2005;7:255–261.
Keller H, Eggli P . Protrusive activity, cytoplasmic compartmentalization, and restriction rings in locomoting blebbing Walker carcinosarcoma cells are related to detachment of cortical actin from the plasma membrane. Cell Motil Cytoskeleton 1998;41:181–193.
Charras GT, Hu CK, Coughlin M et al. Reassembly of contractile actin cortex in cell blebs. J Cell Biol 2006;175:477–490.
Sanz-Moreno V, Gadea G, Ahn J et al. Rac activation and inactivation control plasticity of tumor cell movement. Cell 2008;135:510–523.
Yamazaki D, Kurisu S, Takenawa T . Involvement of Rac and Rho signaling in cancer cell motility in 3D substrates. Oncogene 2009;28:1570–1583.
Bornstein P, Sage EH . Matricellular proteins: extracellular modulators of cell function. Curr Opin Cell Biol 2002;14:608–616.
Maquart FX, Simeon A, Pasco S et al. Regulation of cell activity by the extracellular matrix: the concept of matrikines. J Soc Biol 1999;193:423–428.
Davis GE, Bayless KJ, Davis MJ et al. Regulation of tissue injury responses by the exposure of matricryptic sites within extracellular matrix molecules. Am J Pathol 2000;156:1489–1498.
DiMilla PA, Stone JA, Quinn JA et al. Maximal migration of human smooth muscle cells on fibronectin and type IV collagen occurs at an intermediate attachment strength. J Cell Biol 1993;122:729–737.
DiMilla PA, Barbee K, Lauffenburger DA . Mathematical model for the effects of adhesion and mechanics on cell migration speed. Biophys J 1991;60:15–37.
Palecek SP, Loftus JC, Ginsberg MH et al. Integrin-ligand binding properties govern cell migration speed through cell-substratum adhesiveness. Nature 1997;385:537–540.
Ware MF, Wells A, Lauffenburger DA . Epidermal growth factor alters fibroblast migration speed and directional persistence reciprocally and in a matrix-dependent manner. J Cell Sci 1998;111 (Pt 16):2423–2432.
Xie H, Pallero MA, Gupta K et al. EGF receptor regulation of cell motility: EGF induces disassembly of focal adhesions independently of the motility-associated PLCgamma signaling pathway. J Cell Sci 1998;111 (Pt 5):615–624.
Jones FS, Jones PL . The tenascin family of ECM glycoproteins: structure, function, and regulation during embryonic development and tissue remodeling. Dev Dyn 2000;218:235–259.
Pas J, Wyszko E, Rolle K et al. Analysis of structure and function of tenascin-C. Int J Biochem Cell Biol 2006;38:1594–1602.
Aukhil I, Joshi P, Yan Y et al. Cell- and heparin-binding domains of the hexabrachion arm identified by tenascin expression proteins. J Biol Chem 1993;268:2542–2553.
Chiquet-Ehrismann R, Chiquet M . Tenascins: regulation and putative functions during pathological stress. J Pathol 2003;200:488–499.
Orend G . Potential oncogenic action of tenascin-C in tumorigenesis. Int J Biochem Cell Biol 2005;37:1066–1083.
Orend G, Chiquet-Ehrismann R . Tenascin-C induced signaling in cancer. Cancer Lett 2006;244:143–163.
Erickson HP, Bourdon MA . Tenascin: an extracellular matrix protein prominent in specialized embryonic tissues and tumors. Annu Rev Cell Biol 1989;5:71–92.
Midwood KS, Orend G . The role of tenascin-C in tissue injury and tumorigenesis. J Cell Commun Signal 2009;3:287–310.
Prieto AL, Andersson-Fisone C, Crossin KL . Characterization of multiple adhesive and counteradhesive domains in the extracellular matrix protein cytotactin. J Cell Biol 1992;119:663–678.
Spring J, Beck K, Chiquet-Ehrismann R . Two contrary functions of tenascin: dissection of the active sites by recombinant tenascin fragments. Cell 1989;59:325–334.
Hancox RA, Allen MD, Holliday DL et al. Tumour-associated tenascin-C isoforms promote breast cancer cell invasion and growth by matrix metalloproteinase-dependent and independent mechanisms. Breast Cancer Res 2009;11:R24.
Tremble P, Chiquet-Ehrismann R, Werb Z . The extracellular matrix ligands fibronectin and tenascin collaborate in regulating collagenase gene expression in fibroblasts. Mol Biol Cell 1994;5:439–453.
Dang D, Yang Y, Li X et al. Matrix metalloproteinases and TGFbeta1 modulate oral tumor cell matrix. Biochem Biophys Res Commun 2004;316:937–942.
Siri A, Knauper V, Veirana N et al. Different susceptibility of small and large human tenascin-C isoforms to degradation by matrix metalloproteinases. J Biol Chem 1995;270:8650–8654.
Wenk MB, Midwood KS, Schwarzbauer JE . Tenascin-C suppresses Rho activation. J Cell Biol 2000;150:913–920.
Sanz-Moreno V, Gaggioli C, Yeo M et al. ROCK and JAK1 signaling cooperate to control actomyosin contractility in tumor cells and stroma. Cancer Cell 2011;20:229–245.
Yamaguchi H . Pathological roles of invadopodia in cancer invasion and metastasis. Eur J Cell Biol 2012;91:902–907.
Beck K, Hunter I, Engel J . Structure and function of laminin: anatomy of a multidomain glycoprotein. FASEB J 1990;4:148–160.
Jones PL, Jones FS . Tenascin-C in development and disease: gene regulation and cell function. Matrix Biol 2000;19:581–596.
Tsuruta D, Kobayashi H, Imanishi H et al. Laminin-332-integrin interaction: a target for cancer therapy? Curr Med Chem 2008;15:1968–1975.
Koshikawa N, Giannelli G, Cirulli V et al. Role of cell surface metalloprotease MT1-MMP in epithelial cell migration over laminin-5. J Cell Biol 2000;148:615–624.
Giannelli G, Falk-Marzillier J, Schiraldi O et al. Induction of cell migration by matrix metalloprotease-2 cleavage of laminin-5. Science 1997;277:225–228.
Shang M, Koshikawa N, Schenk S et al. The LG3 module of laminin-5 harbors a binding site for integrin alpha3beta1 that promotes cell adhesion, spreading, and migration. J Biol Chem 2001;276:33045–33053.
Choma DP, Milano V, Pumiglia KM et al. Integrin alpha3beta1-dependent activation of FAK/Src regulates Rac1-mediated keratinocyte polarization on laminin-5. J Invest Dermatol 2007;127:31–40.
Guess CM, Quaranta V . Defining the role of laminin-332 in carcinoma. Matrix Biol 2009;28:445–455.
Pyke C, Romer J, Kallunki P et al. The gamma 2 chain of kalinin/laminin 5 is preferentially expressed in invading malignant cells in human cancers. Am J Pathol 1994;145:782–791.
Gagnoux-Palacios L, Allegra M, Spirito F et al. The short arm of the laminin gamma2 chain plays a pivotal role in the incorporation of laminin 5 into the extracellular matrix and in cell adhesion. J Cell Biol 2001;153:835–850.
Cheng CY, Sun CC, Yu WH et al. Novel laminin 5 gamma 2-chain fragments potentiating the limbal epithelial cell outgrowth on amniotic membrane. Invest Ophthalmol Vis Sci 2009;50:4631–4639.
D'Alessio S, Gerasi L, Blasi F . uPAR-deficient mouse keratinocytes fail to produce EGFR-dependent laminin-5, affecting migration in vivo and in vitro. J Cell Sci 2008;121 (Pt 23):3922–3932.
Pyke C, Salo S, Ralfkiaer E et al. Laminin-5 is a marker of invading cancer cells in some human carcinomas and is coexpressed with the receptor for urokinase plasminogen activator in budding cancer cells in colon adenocarcinomas. Cancer Res 1995;55:4132–4139.
Lindberg P, Larsson A, Nielsen BS . Expression of plasminogen activator inhibitor-1, urokinase receptor and laminin gamma-2 chain is an early coordinated event in incipient oral squamous cell carcinoma. Int J Cancer 2006;118:2948–2956.
Mamoune A, Kassis J, Kharait S et al. DU145 human prostate carcinoma invasiveness is modulated by urokinase receptor (uPAR) downstream of epidermal growth factor receptor (EGFR) signaling. Exp Cell Res 2004;299:91–100.
Gout SP, Jacquier-Sarlin MR, Rouard-Talbot L et al. RhoA-dependent switch between alpha2beta1 and alpha3beta1 integrins is induced by laminin-5 during early stage of HT-29 cell differentiation. Mol Biol Cell 2001;12:3268–3281.
Zhou H, Kramer RH . Integrin engagement differentially modulates epithelial cell motility by RhoA/ROCK and PAK1. J Biol Chem 2005;280:10624–10635.
Nguyen BP, Ren XD, Schwartz MA et al. Ligation of integrin alpha 3beta 1 by laminin 5 at the wound edge activates Rho-dependent adhesion of leading keratinocytes on collagen. J Biol Chem 2001;276:43860–43870.
Maurer P, Mayer U, Bruch M et al. High-affinity and low-affinity calcium binding and stability of the multidomain extracellular 40-kDa basement membrane glycoprotein (BM-40/SPARC/osteonectin). Eur J Biochem 1992;205:233–240.
Lane TF, Sage EH . The biology of SPARC, a protein that modulates cell-matrix interactions. FASEB J 1994;8:163–173.
Hohenester E, Maurer P, Timpl R . Crystal structure of a pair of follistatin-like and EF-hand calcium-binding domains in BM-40. EMBO J 1997;16:3778–3786.
Weaver MS, Workman G, Sage EH . The copper binding domain of SPARC mediates cell survival in vitro via interaction with integrin beta1 and activation of integrin-linked kinase. J Biol Chem 2008;283:22826–22837.
Pavasant P, Yongchaitrakul T . Secreted protein acidic, rich in cysteine induces pulp cell migration via alphavbeta3 integrin and extracellular signal-regulated kinase. Oral Dis 2008;14:335–340.
De S, Chen J, Narizhneva NV et al. Molecular pathway for cancer metastasis to bone. J Biol Chem 2003;278:39044–39050.
Arnold SA, Brekken RA . SPARC: a matricellular regulator of tumorigenesis. J Cell Commun Signal 2009;3:255–273.
Chlenski A, Cohn SL . Modulation of matrix remodeling by SPARC in neoplastic progression. Semin Cell Dev Biol 2010;21:55–65.
Sage H, Vernon RB, Funk SE et al. SPARC, a secreted protein associated with cellular proliferation, inhibits cell spreading in vitro and exhibits Ca+2-dependent binding to the extracellular matrix. J Cell Biol 1989;109:341–356.
Murphy-Ullrich JE, Lane TF, Pallero MA et al. SPARC mediates focal adhesion disassembly in endothelial cells through a follistatin-like region and the Ca(2+)-binding EF-hand. J Cell Biochem 1995;57:341–350.
McClung HM, Golembieski WA, Schultz CR et al. Deletion of the SPARC acidic domain or EGF-like module reduces SPARC-induced migration and signaling through p38 MAPK/HSP27 in glioma. Carcinogenesis 2012;33:275–284.
Barker TH, Baneyx G, Cardo-Vila M et al. SPARC regulates extracellular matrix organization through its modulation of integrin-linked kinase activity. J Biol Chem 2005;280:36483–36493.
Tremble PM, Lane TF, Sage EH et al. SPARC, a secreted protein associated with morphogenesis and tissue remodeling, induces expression of metalloproteinases in fibroblasts through a novel extracellular matrix-dependent pathway. J Cell Biol 1993;121:1433–1444.
Kunigal S, Gondi CS, Gujrati M et al. SPARC-induced migration of glioblastoma cell lines via uPA-uPAR signaling and activation of small GTPase RhoA. Int J Oncol 2006;29:1349–1357.
Kupprion C, Motamed K, Sage EH . SPARC (BM-40, osteonectin) inhibits the mitogenic effect of vascular endothelial growth factor on microvascular endothelial cells. J Biol Chem 1998;273:29635–29640.
Raines EW, Lane TF, Iruela-Arispe ML et al. The extracellular glycoprotein SPARC interacts with platelet-derived growth factor (PDGF)-AB and -BB and inhibits the binding of PDGF to its receptors. Proc Natl Acad Sci USA 1992;89:1281–1285.
Bhoopathi P, Gondi CS, Gujrati M et al. SPARC mediates Src-induced disruption of actin cytoskeleton via inactivation of small GTPases Rho-Rac-Cdc42. Cell Signal 2011;23:1978–1987.
Said N, Najwer I, Motamed K . Secreted protein acidic and rich in cysteine (SPARC) inhibits integrin-mediated adhesion and growth factor-dependent survival signaling in ovarian cancer. Am J Pathol 2007;170:1054–1063.
Lane TF, Iruela-Arispe ML, Sage EH . Regulation of gene expression by SPARC during angiogenesis in vitro. Changes in fibronectin, thrombospondin-1, and plasminogen activator inhibitor-1. J Biol Chem 1992;267:16736–16745.
Bornstein P . Thrombospondins: structure and regulation of expression. FASEB J 1992;6:3290–3299.
Liu A, Mosher DF, Murphy-Ullrich JE et al. The counteradhesive proteins, thrombospondin 1 and SPARC/osteonectin, open the tyrosine phosphorylation-responsive paracellular pathway in pulmonary vascular endothelia. Microvasc Res 2009;77:13–20.
Murphy-Ullrich JE, Poczatek M . Activation of latent TGF-beta by thrombospondin-1: mechanisms and physiology. Cytokine Growth Factor Rev 2000;11:59–69.
Adams JC, Kureishy N, Taylor AL . A role for syndecan-1 in coupling fascin spike formation by thrombospondin-1. J Cell Biol 2001;152:1169–1182.
Nunes SS, Outeiro-Bernstein MA, Juliano L et al. Syndecan-4 contributes to endothelial tubulogenesis through interactions with two motifs inside the pro-angiogenic N-terminal domain of thrombospondin-1. J Cell Physiol 2008;214:828–837.
Calzada MJ, Annis DS, Zeng B et al. Identification of novel beta1 integrin binding sites in the type 1 and type 2 repeats of thrombospondin-1. J Biol Chem 2004;279:41734–41743.
Staniszewska I, Zaveri S, Del Valle L et al. Interaction of alpha9beta1 integrin with thrombospondin-1 promotes angiogenesis. Circ Res 2007;100:1308–1316.
Gao AG, Lindberg FP, Dimitry JM et al. Thrombospondin modulates alpha v beta 3 function through integrin-associated protein. J Cell Biol 1996;135:533–544.
Gao AG, Lindberg FP, Finn MB et al. Integrin-associated protein is a receptor for the C-terminal domain of thrombospondin. J Biol Chem 1996;271:21–24.
Good DJ, Polverini PJ, Rastinejad F et al. A tumor suppressor-dependent inhibitor of angiogenesis is immunologically and functionally indistinguishable from a fragment of thrombospondin. Proc Natl Acad Sci USA 1990;87:6624–6628.
Isenberg JS, Martin-Manso G, Maxhimer JB et al. Regulation of nitric oxide signalling by thrombospondin 1: implications for anti-angiogenic therapies. Nat Rev Cancer 2009;9:182–194.
Fontana A, Filleur S, Guglielmi J et al. Human breast tumors override the antiangiogenic effect of stromal thrombospondin-1 in vivo. Int J Cancer 2005;116:686–691.
Filleur S, Volpert OV, Degeorges A et al. In vivo mechanisms by which tumors producing thrombospondin 1 bypass its inhibitory effects. Genes Dev 2001;15:1373–1382.
Lin XD, Chen SQ, Qi YL et al. Overexpression of thrombospondin-1 in stromal myofibroblasts is associated with tumor growth and nodal metastasis in gastric carcinoma. J Surg Oncol 2012;106:94–100.
Nucera C, Porrello A, Antonello ZA et al. B-Raf(V600E) and thrombospondin-1 promote thyroid cancer progression. Proc Natl Acad Sci USA 2010;107:10649–10654.
Roberts DD . Regulation of tumor growth and metastasis by thrombospondin-1. FASEB J 1996;10:1183–1191.
Bein K, Simons M . Thrombospondin type 1 repeats interact with matrix metalloproteinase 2. Regulation of metalloproteinase activity. J Biol Chem 2000;275:32167–32173.
Albo D, Shinohara T, Tuszynski GP . Up-regulation of matrix metalloproteinase 9 by thrombospondin 1 in gastric cancer. J Surg Res 2002;108:51–60.
Murphy-Ullrich JE, Hook M . Thrombospondin modulates focal adhesions in endothelial cells. J Cell Biol 1989;109:1309–1319.
Murphy-Ullrich JE, Gurusiddappa S, Frazier WA et al. Heparin-binding peptides from thrombospondins 1 and 2 contain focal adhesion-labilizing activity. J Biol Chem 1993;268:26784–26789.
Orr AW, Pallero MA, Xiong WC et al. Thrombospondin induces RhoA inactivation through FAK-dependent signaling to stimulate focal adhesion disassembly. J Biol Chem 2004;279:48983–48992.
Orr AW, Elzie CA, Kucik DF et al. Thrombospondin signaling through the calreticulin/LDL receptor-related protein co-complex stimulates random and directed cell migration. J Cell Sci 2003;116 (Pt 14):2917–2927.
Arnoletti JP, Albo D, Granick MS et al. Thrombospondin and transforming growth factor-beta 1 increase expression of urokinase-type plasminogen activator and plasminogen activator inhibitor-1 in human MDA-MB-231 breast cancer cells. Cancer 1995;76:998–1005.
Albo D, Arnoletti JP, Castiglioni A et al. Thrombospondin (TSP) and transforming growth factor beta 1 (TGF-beta) promote human A549 lung carcinoma cell plasminogen activator inhibitor type 1 (PAI-1) production and stimulate tumor cell attachment in vitro. Biochem Biophys Res Commun 1994;203:857–865.
Cartier-Michaud A, Malo M, Charriere-Bertrand C et al. Matrix-bound PAI-1 supports cell blebbing via RhoA/ROCK1 signaling. PLoS One 2012;7:e32204.
Albo D, Berger DH, Wang TN et al. Thrombospondin-1 and transforming growth factor-beta l promote breast tumor cell invasion through up-regulation of the plasminogen/plasmin system. Surgery 1997;122:493–499 discussion 9–500.
Albo D, Rothman VL, Roberts DD et al. Tumour cell thrombospondin-1 regulates tumour cell adhesion and invasion through the urokinase plasminogen activator receptor. Br J Cancer 2000;83:298–306.
Bornstein P, Armstrong LC, Hankenson KD et al. Thrombospondin 2, a matricellular protein with diverse functions. Matrix Biol 2000;19:557–568.
Krady MM, Zeng J, Yu J et al. Thrombospondin-2 modulates extracellular matrix remodeling during physiological angiogenesis. Am J Pathol 2008;173:879–891.
Angelucci A, Festuccia C, Gravina GL et al. Osteopontin enhances the cell proliferation induced by the epidermal growth factor in human prostate cancer cells. Prostate 2004;59:157–166.
Tuck AB, Hota C, Wilson SM et al. Osteopontin-induced migration of human mammary epithelial cells involves activation of EGF receptor and multiple signal transduction pathways. Oncogene 2003;22:1198–1205.
Timpl R, Sasaki T, Kostka G et al. Fibulins: a versatile family of extracellular matrix proteins. Nat Rev Mol Cell Biol 2003;4:479–489.
Giltay R, Timpl R, Kostka G . Sequence, recombinant expression and tissue localization of two novel extracellular matrix proteins, fibulin-3 and fibulin-4. Matrix Biol 1999;18:469–480.
Gallagher WM, Currid CA, Whelan LC . Fibulins and cancer: friend or foe? Trends Mol Med 2005;11:336–340.
de Vega S, Iwamoto T, Yamada Y . Fibulins: multiple roles in matrix structures and tissue functions. Cell Mol Life Sci 2009;66:;1890–1902.
Obaya AJ, Rua S, Moncada-Pazos A et al. The dual role of fibulins in tumorigenesis. Cancer Lett 2012;325:132–138.
Camaj P, Seeliger H, Ischenko I et al. EFEMP1 binds the EGF receptor and activates MAPK and Akt pathways in pancreatic carcinoma cells. Biol Chem 2009;390:1293–1302.
Yates CC, Bodnar R, Wells A . Matrix control of scarring. Cell Mol Life Sci 2011;68:1871–1881.
Wells A, Chao YL, Grahovac J et al. Epithelial and mesenchymal phenotypic switchings modulate cell motility in metastasis. Front Biosci 2011;16:815–837.
Wolf K, Alexander S, Schacht V et al. Collagen-based cell migration models in vitro and in vivo. Semin Cell Dev Biol 2009;20:931–941.
Ilina O, Bakker GJ, Vasaturo A et al. Two-photon laser-generated microtracks in 3D collagen lattices: principles of MMP-dependent and -independent collective cancer cell invasion. Phys Biol 2011;8:015010.
Gritsenko PG, Ilina O, Friedl P . Interstitial guidance of cancer invasion. J Pathol 2012;226:185–199.
Merline R, Schaefer RM, Schaefer L . The matricellular functions of small leucine-rich proteoglycans (SLRPs). J Cell Commun Signal 2009;3:323–335.
Chopra RK, Pearson CH, Pringle GA et al. Dermatan sulphate is located on serine-4 of bovine skin proteodermatan sulphate. Demonstration that most molecules possess only one glycosaminoglycan chain and comparison of amino acid sequences around glycosylation sites in different proteoglycans. Biochem J 1985;232:277–279.
Bianco P, Fisher LW, Young MF et al. Expression and localization of the two small proteoglycans biglycan and decorin in developing human skeletal and non-skeletal tissues. J Histochem Cytochem 1990;38:1549–1563.
Keene DR, San Antonio JD, Mayne R et al. Decorin binds near the C terminus of type I collagen. J Biol Chem 2000;275:21801–21804.
Danielson KG, Baribault H, Holmes DF et al. Targeted disruption of decorin leads to abnormal collagen fibril morphology and skin fragility. J Cell Biol 1997;136:729–743.
Zhang G, Ezura Y, Chervoneva I et al. Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development. J Cell Biochem 2006;98:1436–1449.
Iozzo RV, Moscatello DK, McQuillan DJ et al. Decorin is a biological ligand for the epidermal growth factor receptor. J Biol Chem 1999;274:4489–4492.
Goldoni S, Humphries A, Nystrom A et al. Decorin is a novel antagonistic ligand of the Met receptor. J Cell Biol 2009;185:743–754.
Merline R, Moreth K, Beckmann J et al. Signaling by the matrix proteoglycan decorin controls inflammation and cancer through PDCD4 and MicroRNA-21. Sci Signal 2011;4:ra75.
Iozzo RV, Buraschi S, Genua M et al. Decorin antagonizes IGF receptor I (IGF-IR) function by interfering with IGF-IR activity and attenuating downstream signaling. J Biol Chem 2011;286:34712–34721.
Hildebrand A, Romaris M, Rasmussen LM et al. Interaction of the small interstitial proteoglycans biglycan, decorin and fibromodulin with transforming growth factor beta. Biochem J 1994;302 (Pt 2):527–534.
Bi X, Pohl NM, Qian Z et al. Decorin-mediated inhibition of colorectal cancer growth and migration is associated with E-cadherin in vitro and in mice. Carcinogenesis 2012;33:326–330.
Mauviel A, Santra M, Chen YQ et al. Transcriptional regulation of decorin gene expression. Induction by quiescence and repression by tumor necrosis factor-alpha. J Biol Chem 1995;270:11692–11700.
Sofeu Feugaing DD, Gotte M, Viola M . More than matrix: The multifaceted role of decorin in cancer. Eur J Cell Biol 2013;92:1–11.
Franz M, Hansen T, Richter P et al. Complex formation of the laminin-5 gamma2 chain and large unspliced tenascin-C in oral squamous cell carcinoma in vitro and in situ: implications for sequential modulation of extracellular matrix in the invasive tumor front. Histochem Cell Biol 2006;126:125–131.
Berndt A, Borsi L, Hyckel P et al. Fibrillary co-deposition of laminin-5 and large unspliced tenascin-C in the invasive front of oral squamous cell carcinoma in vivo and in vitro. J Cancer Res Clin Oncol 2001;127:286–292.
Acknowledgements
We thank members of the Wells laboratory for discussions and feedback on these concepts. This work was supported in part by grants from the DoD, NIH, and VA Merit Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Cancer invasion is a complex process requiring, among other events, extensive remodeling of the extracellular matrix including deposition of pro-migratory and pro-proliferative moieties. This review summarizes findings which indicate that matricellular proteins that can induce both integrin and growth factor signaling and are being deposited at the invasive tumor fronts, enabling cancer cell migrational plasticity and promoting invasion.
Rights and permissions
About this article
Cite this article
Grahovac, J., Wells, A. Matrikine and matricellular regulators of EGF receptor signaling on cancer cell migration and invasion. Lab Invest 94, 31–40 (2014). https://doi.org/10.1038/labinvest.2013.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2013.132
Keywords
This article is cited by
-
Tumor-associated macrophages promote ovarian cancer cell migration by secreting transforming growth factor beta induced (TGFBI) and tenascin C
Cell Death & Disease (2020)
-
The extracellular matrix in tumor progression and metastasis
Clinical & Experimental Metastasis (2019)
-
Transmissible gastroenteritis virus infection decreases arginine uptake by downregulating CAT-1 expression
Veterinary Research (2018)
-
Evaluation of epidermal growth factor receptor signaling effects in gastric cancer cell lines by detailed motility-focused phenotypic characterization linked with molecular analysis
BMC Cancer (2017)