Abstract
Objective:
To calculate the prevalence of vocal fold paralysis (VFP) in preterm (<37 weeks of gestation) infants at a single neonatal intensive care unit (NICU) and identify risk factors for the development of VFP.
Study Design:
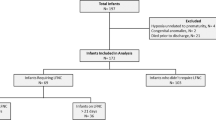
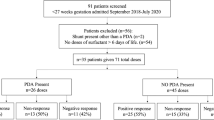
This is a case control study of all surviving preterm infants admitted to the NICU at Children’s Hospital of Wisconsin from 2006 to 2012, comparing those with and without VFP. Multivariate analysis was performed to identify significant risk factors for VFP.
Results:
Of the 2083 patients included, 73 (3.5%) had VFP, including 18% of those at <26 weeks of gestation. On multivariate analyses, VFP was associated with patent ductus arteriosus (PDA) ligation (P<0.001, odds ratio (OR) 15.9, 95% confidence interval (CI) 8.9 to 28.1), history of invasive ventilation (P=0.008, OR 4.5, 95% CI 1.5 to 13.6) and black vs non-black race (P=0.001, OR 2.5, 95% CI 1.5 to 4.3).
Conclusion:
Given the prevalence of VFP and its associated morbidity, efforts to decrease PDA ligation and invasive ventilation in preterm infants are warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Holinger PH, Brown WT . Congenital webs, cysts, laryngoceles, and other anomalies of the larynx. Ann Otol Rhinol Laryngol 1967; 76 (4): 744–752.
Fan LL, Campbell DN, Clarke DR, Washington RL, Fix EJ, White CW . Paralyzed left vocal cord associated with ligation of patent ductus arteriosus. J Thorac Cardiovasc Surg 1989; 98 (4): 611–613.
Zbar RI, Chen AH, Behrendt DM, Bell EF, Smith RJ . Incidence of vocal fold paralysis in infants undergoing ligation of patent ductus arteriosus. Ann Thorac Surg 1996; 61 (3): 814–816.
Spanos WC, Brookes JT, Smith MC, Burkhart HM, Bell EF, Smith RJ . Unilateral vocal fold paralysis in premature infants after ligation of patent ductus arteriosus: vascular clip versus suture ligature. Ann Otol Rhinol Laryngol 2009; 118 (10): 750–753.
Jabbour J, Martin T, Beste D, Robey T . Pediatric vocal fold immobility: natural history and the need for long-term follow-up. JAMA Otolaryngol Head Neck Surg 2014; 140 (5): 428–433.
Clement WA, El-Hakim H, Phillipos EZ, Cote JJ . Unilateral vocal cord paralysis following patent ductus arteriosus ligation in extremely low-birth-weight infants. Arch Otolaryngol Head Neck Surg 2008; 134 (1): 28–33.
Benjamin JR, Smith PB, Cotten CM, Jaggers J, Goldstein RF, Malcolm WF . Long-term morbidities associated with vocal cord paralysis after surgical closure of a patent ductus arteriosus in extremely low birth weight infants. J Perinatol 2010; 30 (6): 408–413.
Nichols BG, Jabbour J, Hehir DA, Ghanayem NS, Beste D, Martin T et al. Recovery of vocal fold immobility following isolated patent ductus arteriosus ligation. Int J Pediatr Otorhinolaryngol 2014; 78 (8): 1316–1319.
Roksund OD, Clemm H, Heimdal JH, Auklan SM, Sandvik L, Markestad T et al. Left vocal cord paralysis after extreme preterm birth, a new clinical scenario in adults. Pediatrics 2010; 126 (6): e1569–e1577.
Strychowsky JE, Rukholm G, Gupta MK, Reid D . Unilateral vocal fold paralysis after congenital cardiothoracic surgery: a meta-analysis. Pediatrics 2014; 133 (6): e1708–e1723.
Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy K et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med 2011; 183 (12): 1715–1722.
Fisher JG, Bairdain S, Sparks EA, Khan FA, Archer JM, Kenny M et al. Serious congenital heart disease and necrotizing enterocolitis in very low birth weight neonates. J Am Coll Surg 2015; 220 (6): 1018–1026.
de Guademar I, Roudaire M, Francois M, Narcy P . Outcome of laryngeal paralysis in neonates: a long term retrospective study of 113 cases. Int J Pediatr Otorhinolaryngol 1996; 34 (1-2): 101–110.
Daya H, Hosni A, Bejar-Solar I, Evans JN, Bailey CM . Pediatric vocal fold paralysis: a long-term retrospective study. Arch Otolaryngol Head Neck Surg 2000; 126 (1): 21–25.
Truong MT, Messner AH, Kerschner JE, Scholes M, Wong-Dominguez J, Milczuk HA et al. Pediatric vocal fold paralysis after cardiac surgery: rate of recovery and sequelae. Otolaryngol Head Neck Surg 2007; 137 (5): 780–784.
Reynolds V, Meldrum S, Simmer K, Vijayasekaran S, French N . Dysphonia in very preterm children: a review of the evidence. Neonatology 2014; 106: 69–73.
Walz PC, Hubbell MP, Elmaraghy CA . Voice related quality of life in pediatric patients with a history of prematurity. Int J Pediatr Otorhinolaryngol 2014; 78 (7): 1010–1014.
French N, Kelly R, Vijayasekaran S, Reynolds V, Lipscombe J, Buckland A et al. Voice abnormalities at school age in children born extremely preterm. Pediatrics 2013; 131 (3): e733–e739.
Himpens E, Van den Broeck C, Oostra A, Calders P, VAnhaesebrouck P . Prevalence, type, distribution, and severity of cerebral palsy in relation to gestational age: a meta-analytic review. Dev Med Child Neurol 2008; 50 (5): 334–340.
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK . Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics 2012; 129 (2): e298–e304.
Gaylord MS, Thieme RE, Woodall DL, Quissell BJ . Predicting mortality in low-birth-weight infants with pulmonary interstitial emphysema. Pediatrics 1985; 76 (2): 219–224.
Smith ME, King JD, Elsherif A, Muntz HR, Park AH, Kouretas PC . Should all newborns who undergo patent ductus arteriosus ligation be examined for vocal fold mobility? Laryngoscope 2009; 119 (8): 1606–1609.
Brandwein M, Abramson AL, Shikowitz MJ . Bilateral vocal cord paralysis following endoctracheal intubation. Arch Otolaryngol Head Neck Surg 1986; 112: 866–882.
Yin SS, Qui WW, Stucker FJ . Value of electromyopgraphy in differential diagnosis of laryngeal joint injuries after intubation. Ann Otol Rhinol Laryngol 1996; 105: 446–451.
Carpes LF, Kozak FK, Leblanc JG, Campbell AI, Human DG, Fandino M et al. Assessment of vocal fold mobility before and after cardiothoracic surgery in children. Arch Otolaryngol Head Neck Surg 2011; 137 (6): 571–575.
Acknowledgements
We thank Natalie Hasbani for her assistance with study design and data analysis. We also thank David Bramlett for his assistance with data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jabbour, J., Uhing, M. & Robey, T. Vocal fold paralysis in preterm infants: prevalence and analysis of risk factors. J Perinatol 37, 585–590 (2017). https://doi.org/10.1038/jp.2016.263
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.263