Abstract
Objective:
The critically ill, premature patients of neonatal intensive care units are susceptible to venous thrombosis, an adverse event associated with short- and long-term morbidity. Venous thrombosis is frequently treated with low-molecular-weight heparins (LMWHs) such as enoxaparin, but optimal dosing of LMWH must balance the morbidity of venous thrombosis with the potential adverse affects of anticoagulation. The optimal dosing of enoxaparin for premature infants is unclear. The objective of this study was to describe enoxaparin therapy and follow-up in critically ill neonates diagnosed with venous thrombosis.
Study Design:
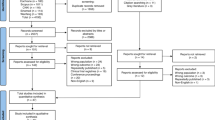
Retrospective medical record review in the neonatal intensive care unit (NICU) in a single tertiary care institution. Infants with venous thrombosis diagnosed in the NICU were identified using preexisting quality improvement lists and medical records.
Results:
Twenty-six infants with 30 venous thromboses were identified with a median gestational age of 31 weeks at birth. Eighteen (69%) infants received enoxaparin for venous thrombosis during their hospitalization, beginning with a median dose of 1.5 mg kg−1 every 12 h. This dose was increased to a median of 2.1 mg kg−1 every 12 h to achieve target anti-factor Xa levels. The target dose was significantly higher in patients with a postmenstrual age of <37 weeks. Enoxaparin treatment was documented after discharge in 12 patients, continuing for a median of 99 days. Four patients died during hospitalization and their deaths were not attributable to venous thrombosis or anticoagulation complication. Follow-up documentation between 6 and 24 months after venous thrombosis diagnosis revealed no major morbidity of venous thrombosis or enoxaparin therapy.
Conclusion:
Our data reinforce the relative safety and necessity of enoxaparin doses above 1.5 mg kg−1 per 12 h in most neonates. This was particularly true for infants at lower postmenstrual age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Stein PD, Kayali F, Olson RE . Incidence of venous thromboembolism in infants and children: data from the National Hospital Discharge Survey. J Pediatr 2004; 145 (4): 563–565.
Chalmers EA . Epidemiology of venous thromboembolism in neonates and children. Thromb Res 2006; 118 (1): 3–12.
Higgerson RA, Lawson KA, Christie LM, Brown AM, McArthur JA, Totapally BR et al. Incidence and risk factors associated with venous thrombotic events in pediatric intensive care unit patients. Pediatr Crit Care Med 2011; 12 (6): 628–634.
Amankwah EK, Atchison CM, Arlikar S, Ayala I, Barrett L, Branchford BR et al. Risk factors for hospital-sssociated venous thromboembolism in the neonatal intensive care unit. Thromb Res 2014; 134 (2): 305–309.
Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefsen DM et al. Development of the human coagulation system in the full-term infant. Blood 1987; 70 (1): 165–172.
Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefsen DM et al. Development of the human coagulation system in the healthy premature infant. Blood 1988; 72 (5): 1651–1657.
Paes BA, Nagel K, Sunak I, Rashish G, Chan AK, Thrombosis and Hemostasis in Newborns (THiN) Group. Neonatal and infant pulmonary thromboembolism: a literature review. Blood Coagul Fibrinolysis 2012; 23 (7): 653–662.
Yang JY, Chan AK . Neonatal systemic venous thrombosis. Thromb Res 2010; 126 (6): 471–476.
Nowak-Gottl U, Janssen V, Manner D, Kenet G . Venous thromboembolism in neonates and children—update 2013. Thromb Res 2013; 131 (Suppl 1): S39–S41.
Monagle P, Chan AK, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Gottl U et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141 (2 Suppl): e737S–e7801.
Bauman ME, Belletrutti MJ, Bajzar L, Black KL, Kuhle S, Bauman ML et al. Evaluation of enoxaparin dosing requirements in infants and children. Better dosing to achieve therapeutic levels. Thromb Haemost 2009; 101 (1): 86–92.
Michaels LA, Gurian M, Hegyi T, Drachtman RA . Low molecular weight heparin in the treatment of venous and arterial thromboses in the premature infant. Pediatrics 2004; 114 (3): 703–707.
Andrade-Campos MM, Montes-Limon AE, Fernandez-Mosteirin N, Salvador-Osuna C, Torres M, Lucia-Cuesta JF et al. Dosing and monitoring of enoxaparin therapy in children: experience in a tertiary care hospital. Blood Coagul Fibrinolysis 2013; 24 (2): 194–198.
Malowany JI, Monagle P, Knoppert DC, Lee DS, Wu J, McCusker P et al. Enoxaparin for neonatal thrombosis: a call for a higher dose for neonates. Thromb Res 2008; 122 (6): 826–830.
Schloemer NJ, Abu-Sultaneh S, Hanson SJ, Yan K, Hoffmann RG, Punzalan RC et al. Higher doses of low-molecular-weight heparin (enoxaparin) are needed to achieve target anti-Xa concentrations in critically ill children*. Pediatr Crit Care Med 2014; 15 (7): e294–e299.
Mateos MK, Wright FA, Cohn RJ . Pharmacokinetic analysis of enoxaparin in a term neonate and review of literature. Thromb Res 2013; 132 (4): 487–489.
Chan AK, Monagle P . Updates in thrombosis in pediatrics: where are we after 20 years? Hematology Am Soc Hematol Educ Program 2012; 2012: 439–443.
Bhat R, Monagle P . The preterm infant with thrombosis. Arch Dis Child Fetal Neonatal Ed 2012; 97 (6): F423–F428.
Sanchez de Toledo J, Gunawardena S, Munoz R, Orr R, Berry D, Sonderman S et al. Do neonates, infants and young children need a higher dose of enoxaparin in the cardiac intensive care unit? Cardiol Young 2010; 20 (2): 138–143.
Engle WA, American Academy of Pediatrics Committee on Fetus and Newborn. Age terminology during the perinatal period. Pediatrics 2004; 114 (5): 1362–1364.
Streif W, Goebel G, Chan AK, Massicotte MP . Use of low molecular mass heparin (enoxaparin) in newborn infants: a prospective cohort study of 62 patients. Arch Dis Child Fetal Neonatal Ed 2003; 88 (5): F365–F370.
Malowany JI, Knoppert DC, Chan AK, Pepelassis D, Lee DS . Enoxaparin use in the neonatal intensive care unit: experience over 8 years. Pharmacotherapy 2007; 27 (9): 1263–1271.
Demirel G, Oguz SS, Celik IH, Altug N, Uras N, Erdeve O et al. Evaluation and treatment of neonatal thrombus formation in 17 patients. Clin Appl Thromb Hemost 2011; 17 (6): E46–E51.
Takemoto CM, Sohi S, Desai K, Bharaj R, Khanna A, McFarland S et al. Hospital-associated venous thromboembolism in children: incidence and clinical characteristics. J Pediatr 2014; 164 (2): 332–338.
Salonvaara M, Riikonen P, Kekomaki R, Heinonen K . Clinically symptomatic central venous catheter-related deep venous thrombosis in newborns. Acta Paediatr 1999; 88 (6): 642–646.
Acknowledgements
We acknowledge the CHP Data Warehouse and the UPMC and University of Pittsburgh’s CARe who provided data for this project. We thank the Clinical and Translational Science Institute of the University of Pittsburgh for their assistance with statistical analysis. JCB is supported by the University of Pittsburgh Dean’s Summer Research Scholarship. RKA is supported by R01GM098474 from the National Institutes of Health. MG is supported by K08DK101608 from the National Institutes of Health and the Children’s Hospital of Pittsburgh of the UPMC Health System. Data analysis was performed by the Clinical and Translational Science Institute and was supported by the National Institutes of Health through Grant Number UL1TR001857.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bohnhoff, J., DiSilvio, S., Aneja, R. et al. Treatment and follow-up of venous thrombosis in the neonatal intensive care unit: a retrospective study. J Perinatol 37, 306–310 (2017). https://doi.org/10.1038/jp.2016.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.218