Abstract
Objective:
To evaluate characteristics of unimpaired outcome in extremely low-birth-weight (ELBW) survivors.
Study design:
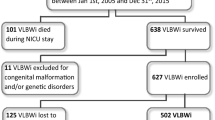
ELBW infants (n=714) with 30 months’ assessments were analyzed. Logistic regression was used to develop a model for the binary outcome of unimpaired versus impaired outcome.
Result:
Thirty-three percent of infants had an unimpaired outcome. Seventeen percent of ELBW survivors had a Bayley II Mental Developmental Index score of ⩾101 and 2% had a score of ⩾116. Female gender, use of antenatal steroids (ANS), maternal education ⩾high school and the absence of major neonatal morbidities were independent predictors of unimpaired outcome. The likelihood of an unimpaired outcome in the presence of major neonatal morbidities was higher in infants exposed to ANS.
Conclusion:
The majority of unimpaired ELBW survivors had cognitive scores shifted toward the lower end of the normal distribution. Exposure to ANS was associated with higher likelihood of an unimpaired outcome in infants with major neonatal morbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007; 196, 147 e1–e8.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsc MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126: 443–456.
Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Andreias L et al. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA 2005; 294: 318–325.
Saigal S, Pinelli J, Hoult L, Kim MM, Boyle M . Psychopathology and social competencies of adolescents who were extremely low birth weight. Pediatrics 2003; 111: 969–975.
Gargus RA, Vohr BR, Tyson JE, High P, Higgins RD, Wrage LA et al. Unimpaired outcomes for extremely low birth weight infants at 18 to 22 months. Pediatrics 2009; 124: 112–121.
Poindexter BB, Ehrenkranz RA, Stoll BJ, Wright LL, Poole WK, Oh W et al. Parenteral glutamine supplementation does not reduce the risk of mortality or late-onset sepsis in extremely low birth weight infants. Pediatrics 2004; 113: 1209–1215.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Higgins RD, Langer JC et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics 2007; 120: e953–e959.
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M . Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 2005; 115: 997–1003.
Doyle LW, Roberts G, Anderson PJ Victorian Infant Collaborative Study Group. Outcomes at age 2 years of infants<28 weeks’ gestational age born in Victoria in 2005. J Pediatr 2010; 156: 49e1–53e1.
Claas MJ, de Vries LS, Bruinse HW, van Haastert IC, Uniken Venema MMA, Peelem LM et al. Neurodevelopmental outcome over time of preterm born children ≤750 g at birth. Early Hum Dev 2011; 87: 183–191.
Latal B . Prediction of neurodevelopmental outcome after preterm birth. Pediatr Neurol 2009; 40: 413–419.
Mercier CE, Dunn MS, Ferrelli KR, Howard DB, Soll RF Vermont Oxford Network ELBW Infant Follow-Up Study Group. Neurodevelopmental outcome of extremely low birth weight infants from the Vermont Oxford network: 1998-2003. Neonatology 2010; 97: 329–338.
Reiss AL, Kesler SR, Vohr B, Duncan CC, Katz KH, Pajoy S et al. Sex differences in cerebral volumes of 8-year-olds born preterm. J Pediatr 2004; 145: 242–249.
Kesler SR, Reiss AL, Vohr B, Watson C, Schneider KC, Katz KH et al. Brain volume reductions within multiple cognitive systems in male preterm children at age twelve. J Pediatr 2008; 152: 513–520.
Sommerfelt K, Ellertsen B, Markestad T . Parental factors in cognitive outcome of non-handicapped low birthweight infants. Arch Dis Child Fetal Neonatal Ed 1995; 73: F135–F142.
Bohm B, Katz-Salamon M, Institute K, Smedler AC, Lagercrantz H, Forssberg H . Developmental risks and protective factors for influencing cognitive outcome at 5 1/2 years of age in very-low-birthweight children. Dev Med Child Neurol 2002; 44: 508–516.
Strenze T . Intelligence and socioeconomic success: a meta-analytic review of longitudinal research. Intelligence 2007; 35: 401–426.
Batty GD, Deary IJ, Gottfredson LS . Premorbid (early life) IQ and later mortality risk: systematic review. Ann Epidemiol 2007; 17: 278–288.
Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J . Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 2009; 124: 717–728.
Taylor HG, Klein N, Anselmo MG, Minich N, Espy KA, Hack M . Learning problems in kindergarten students with extremely preterm birth. Arch Pediatr Adolesc Med 2011; 165: 819–825.
EXPRESS Group. Incidence of and risk factors for neonatal morbidity after active perinatal care: extremely preterm infants study in Sweden (EXPRESS). Acta Paediatr 2010; 99: 978–992.
Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA 2003; 289: 1124–1129.
Bassler D, Stoll BJ, Schmidt B, Asztalos EV, Roberts RS, Robertson CM et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics 2009; 123: 313–318.
Foix-L'Hélias L, Marret S, Ancel PY, Marchand L, Arnaud C, Fresson J et al. Impact of the use of antenatal corticosteroids on mortality, cerebral lesions and 5-year neurodevelopmental outcomes of very preterm infants: the EPIPAGE cohort study. BJOG 2008; 115: 275–282.
Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ, Ehrenkranz RA et al. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks’ gestation. JAMA 2011; 306: 2348–2358.
Acknowledgements
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study: NRN Chair; Alan H Jobe, MD, PhD, University of Cincinnati. Brown University, Women & Infants Hospital of Rhode Island: William Oh, MD; Betty R Vohr, MD; Angelita Hensman, BSN RNC; Lucy Noel, RN; Barbara Alksninis, PNP; Martha R Leonard, BA; Rachel A Vogt, MD; Teresa M Leach, MEd CAES; Victoria E Watson, MS CAS. Case Western Reserve University, Rainbow Babies & Children’s Hospital: Avroy A Fanaroff, MD; Deanne Wilson-Costello, MD; Nancy S Newman, BA RN; Bonnie S Siner, RN; Harriet G Friedman, MA. Cincinnati Children’s Hospital Medical Center, University Hospital, and Good Samaritan Hospital: Edward F Donovan, MD; Jean Steichen, MD; Barb Alexander, RN; Cathy Grisby, BSN CCRC; Marcia Mersmann, RN; Holly Mincey, RN; Jody Shively, RN; Teresa L Gratton, PA. Emory University, Children’s Healthcare of Atlanta, Grady Memorial Hospital, and Emory Crawford Long Hospital: Barbara J Stoll, MD; Ira Adams-Chapman, MD; Ellen Hale, RN BS; Maureen Mulligan LaRossa, RN; Sheena Carter, PhD. Eunice Kennedy Shriver National Institute of Child Health and Human Development: Linda L Wright, MD; Elizabeth M McClure, MEd. Indiana University, University Hospital, Methodist Hospital, Riley Hospital for Children, and Wishard Health Services: Brenda B Poindexter, MD MS; James A Lemons, MD; Anna M Dusick, MD; Carolyn Lytle, MD; Darlene Kardatzke, MD; Marilyn Bull, MD; Greg Eaken, PhD; Lon G Bohnke, MS; Leslie Richard, RN; Diana D Appel, RN BSN; Dianne Herron, RN; Lucy Miller, RN BSN CCRC; Leslie Dawn Wilson, RN BSN. RTI International: W Kenneth Poole, PhD; Betty Hastings; Carolyn Petrie Huitema, MS; Scott E Schaefer, MS. Stanford University, Lucile Packard Children’s Hospital: David K Stevenson, MD; Susan R Hintz, MD MS; Barry E Fleisher, MD; M Bethany Ball, BS CCRC; Carol G Kuelper, PhD; Julie C Lee, PhD; Joan M Baran, PhD; Lori E Bond, PhD; Nicholas St. John, PhD; Renee P Pyle, PhD. University of Alabama at Birmingham Health System and Children’s Hospital of Alabama: Waldemar A Carlo, MD; Myriam Peralta-Carcelen, MD; Monica V Collins, RN BSN MaEd; Shirley S Cosby, RN BSN; Vivien A Phillips, RN BSN; Fred J Biasini, PhD; Kirstin J Bailey, PhD; Richard V Rector, PhD; Stephanie A Chopko, PhD. University of California – San Diego Medical Center and Sharp Mary Birch Hospital for Women: Neil N Finer, MD; Yvonne E Vaucher, MD MPH; Maynard R Rasmussen MD; Kathy Arnell, RN; Martha G Fuller, RN MSN; Donna Posin, OTR/L MPA. University of Miami Holtz Children’s Hospital: Shahnaz Duara, MD; Charles R Bauer, MD; Ruth Everett, RN MSN; Alexis N Diaz, BA; Elaine O Mathews, RN; Kasey Hamlin-Smith, PhD; Lisa Jean-Gilles, BA; Maria Calejo, MS; Silvia M Frade, BA; Silvia Hiriart-Fajardo, MD; Yamiley Gideon, BA. University of Texas Southwestern Medical Center at Dallas, Parkland Health & Hospital System, and Children’s Medical Center Dallas: Abbot R Laptook, MD; R Sue Broyles, MD; Walid A Salhab, MD; Roy J Heyne, MD; Sally Adams, PNP; Cathy Boatman, MS CIMI; Cristin Dooley, MS; Alicia Guzman; Elizabeth Heyne, PA; Jackie F Hickman, RN; Linda Madden, PNP; Susie Madison, RN. Wayne State University, Hutzel Women’s Hospital, and Children’s Hospital of Michigan: Seetha Shankaran, MD; Yvette Johnson, MD; Rebecca Bara, RN BSN; Geraldine Muran, RN BSN; Deborah Kennedy, RN BSN; Laura Goldston, MA. Yale University and Yale-New Haven Children’s Hospital: Richard A Ehrenkranz, MD; Patricia Gettner, RN; Monica Konstantino, RN; Elaine Romano, RN BSN; Nancy Close, PhD; Walter Gilliam, PhD. The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; Grants U10 HD21364, U10 HD21385, U10 HD21397, U10 HD27851, U10 HD27853, U10 HD27856, U10 HD27871, U10 HD27880U10 HD27904, U10 HD34216, U10 HD36790, U10 HD40461, U10 HD40689) and The National Institutes of Health (General Clinical Research Center Grants M01 RR32, M01 RR39, M01 RR70, M01 RR80, M01 RR633, M01 RR750, M01 RR6022, M01 RR8084 and M01 RR16587) provided grant support for the Neonatal Research Network’s Glutamine Study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kumar, P., Shankaran, S., Ambalavanan, N. et al. Characteristics of extremely low-birth-weight infant survivors with unimpaired outcomes at 30 months of age. J Perinatol 33, 800–805 (2013). https://doi.org/10.1038/jp.2013.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.71
Keywords
This article is cited by
-
Neurodevelopmental outcome of Italian preterm ELBW infants: an eleven years single center cohort
Italian Journal of Pediatrics (2022)
-
Postnatal Microstructural Developmental Trajectory of Corpus Callosum Subregions and Relationship to Clinical Factors in Very Preterm Infants
Scientific Reports (2018)
-
Factors affecting neurodevelopmental outcome at 2 years in very preterm infants below 1250 grams: a prospective study
Journal of Perinatology (2018)