Abstract
Objective
To compare neurodevelopmental outcomes of large and appropriate for gestational age (LGA, AGA) infants <29 weeks’ gestation at 18–24 months of corrected age.
Study design
Retrospective cohort study using the Canadian Neonatal Network and Canadian Neonatal Follow-Up Network databases. Primary outcome was a composite of death or significant neurodevelopmental impairment (NDI), defined as severe cerebral palsy, Bayley III cognitive, language and motor scores of <70, need for hearing aids or cochlear implant and bilateral visual impairment. Univariate and multivariable logistic analyses were applied for outcomes.
Results
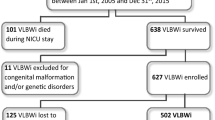
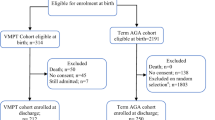
The study cohort comprised 170 LGA and 1738 AGA infants. There was no difference in significant NDI or individual components of the Bayley III between LGA and AGA groups. LGA was associated with the increased risk of death by follow-up, 44/170 (25.9%) vs. 320/1738 (18.4%) (aOR: 1.60 95% CI: 1.00–2.54).
Conclusions
Risk of NDI was similar between LGA and AGA infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data sets generated and analyzed during this study are with PSS, Director CNN, but current data transfer approval agreements do not allow for data to be made available to others.
References
Cartwright R, Anderson NH, Sadler LC, Harding JE, McCowan LME, McKinlay CJD. Neonatal morbidity and small and large size for gestation: a comparison of birthweight centiles. J Perinatol. 2020;40:10.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. Morbidity and mortality in small for gestational age infants at 22 to 29 weeks’ gestation. Pediatrics. 2018;141:e20172533.
Nobile S, Marchionni P, Carnielli VP. Neonatal outcome of small for gestational age preterm infants. Eur J Pediatr. 2017;176:6.
De Jesus LC, Pappas A, Shankaran S, Li L, Das A, Bell EF, et al. Outcomes of small for gestational age infants born at <27 weeks’ gestation. J Pediatr. 2013;163:55–60 e51-53.
ElSayed E, Daspal S, Yee W, Pelausa E, Canning R, Shah PS, et al. Outcomes of singleton small for gestational age preterm infants exposed to maternal hypertension: a retrospective cohort study. Pediatr Res. 2019;86:269–75.
Sacchi C, Marino C, Nosarti C, Vieno A, Visentin S, Simonelli A. Association of intrauterine growth restriction and small for gestational age status with childhood cognitive outcomes: a systematic review and meta-analysis. JAMA Pediatr. 2020;174:772–81.
Arcangeli T, Thilaganathan B, Hooper R, Khan KS, Bhide A. A neurodevelopmental delay in small babies at term: a systematic review. Ultrasound Obstet Gynecol. 2012;40:267–75.
Mericq V, Martinez-Aguayo A, Uauy R, Iniguez G, Van der Steen M, Hokken-Koelega A. Long-term metabolic risk among children born premature or small for gestational age. Nat Rev Endocrinol. 2017;13:50–62.
Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A. Management of the child born small for gestational age through to adulthood: a consensus statement of the international societies of pediatric endocrinology and the growth hormone research society. J Clin Endocr Metab. 2007;92:804–10.
Chiavaroli VDJ, Hofman PL, Cutfield WS. Born large for gestational age: bigger is not always better. J Pediatr. 2016;170:307–11.
Kramer MS, Morin I, Yang H, Platt RW, Usher R, McNamara H, et al. Why are babies getting bigger? Temporal trends in fetal growth and its determinants. J Pediatr. 2002;141:538–42.
Dabelea D, Crume T. Maternal environment and the transgenerational cycle of obesity and diabetes. Diabetes. 2011;60:1849–55.
Catalano PM. Obesity and pregnancy-the propagation of a viscous cycle? J Clin Endocrinol Metab. 2003;88:3505–6.
Goldstein RF, Abell SK, Ranasinha S, Misso ML, Boyle JA, Harrison CL, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018;16:153.
Chauhan SP, Rice MM, Grobman WA, Bailit J, Reddy UM, Wapner RJ, et al. Neonatal morbidity of small- and large-for-gestational-age neonates born at term in uncomplicated pregnancies. Obstet Gynecol. 2017;130:511–9.
Ibiebele I, Bowen JR, Nippita TA, Morris JM, Ford JB. Childhood health and education outcomes following early term induction for large-for-gestational age: A population-based record linkage study. Acta Obstet Gynecol Scand. 2019;98:423–32.
Lei X, Zhao D, Huang L, Luo Z, Zhang J, Yu X, et al. Childhood health outcomes in term, large-for-gestational-age babies with different postnatal growth patterns. Am J Epidemiol. 2018;187:507–14.
Moore GS, Kneitel AW, Walker CK, Gilbert WM, Xing G. Autism risk in small- and large-for-gestational-age infants. Am J Obstet Gynecol. 2012;206:314 e311–319.
Khambalia AZ, Algert CS, Bowen JR, Collie R, Roberts CL. Long-term outcomes for large for gestational age infants born at term. Paediatrics Child Health Div. 2017;53:876–81.
Baer RJ, Rogers EE, Partridge JC, Anderson JG, Morris M, Kuppermann M, et al. Population-based risks of mortality and preterm morbidity by gestational age and birth weight. J Perinatol. 2016;36:1008–13.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. In-hospital outcomes in large for gestational age infants at 22-29 weeks of gestation. J Pediatr. 2018;198:174–80 e113.
Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A, Whyte R, et al. Variations in practice and outcomes in the Canadian NICU network: 1996–7. Pediatrics. 2000;106:1070–9.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal audit of the Canadian Neonatal Network Data Collection System. Am J Perinatol. 2017;34:1241–9.
Canadian Neonatal Follow-Up Network. 18-month corrected age assessment manual. Neonatal folow-up network. Toronto, Canada: Canadian Neonatal Follow-Up Network; 2012. http://www.cnfun.ca/LinkClick.aspx?fileticket=d4p7mZoXWDU%3d&tabid=68Canadian. Accessed 14 July 2020.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
The Canadian Neonatal Network. Abstractor’s manual v.3.3.0. Toronto, Canada: The Canadian Neonatal Network; 2018. http://wwwcanadianneonatalnetworkorg/portal/CNNHome/Publicationaspx.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Hand IL, Shellhaas RA, Milla SS, Committee On Fetus, Newborn SONSOR. Routine neuroimaging of the preterm brain. Pediatrics 2020;146:e2020029082.
Bass WT. Periventricular leukomalacia. NeoReviews. 2011;12:e76.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis - therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Gole G, Ells A, Katz X, Holmstrom G, Fielder A, Capone A, et al. The international classification of retinopathy of prematurity revisited. Arch Ophathlmology. 2005;123:991–9.
Kluckow M, Lemmers P. Hemodynamic assessment of the patent ductus arteriosus: beyond ultrasound. Semin Fetal Neonatal Med. 2018;23:239–44.
Academic Press. Bayley-III clinical use and interpretation. 1st ed. Academic Press: Massachussets, USA: Academic Press; 2016.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–F243.
Ounsted M, Moar VA, Scott A. Factors affecting development: similarities and differences among children who were small, average, and large for gestational age at birth. Acta Paediatr Scand. 1986;75:261–6.
Shenkin SD, Starr JM, Deary IJ. Birth weight and cognitive ability in childhood: a systematic review. Psychol Bull. 2004;130:989–1013.
Shah PS, Shah V, Qiu Z, Ohlsson A, Lee SK. Improved outcomes of outborn preterm infants if admitted to perinatal centers versus freestanding pediatric hospitals. J Pediatr. 2005;146:626–31.
Pulver LS, Guest-Warnick G, Stoddard GJ, Byington CL, Young PC. Weight for gestational age affects the mortality of late preterm infants. Pediatrics. 2009;123:e1072–1077.
Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Weisz B, Achiron R, et al. Maternal and neonatal outcomes of large for gestational age pregnancies. Acta Obstet Gynecol Scand. 2012;91:844–9.
Berger H, Gagnon R, Sermer M, Basso M, Bos H, Brown RN, et al. Diabetes in pregnancy. J Obstet Gynaecol Can. 2016;38:667–79 e661.
Boghossian NS, Hansen NI, Bell EF, Brumbaugh JE, Stoll BJ, Laptook AR, et al. Outcomes of extremely preterm infants born to insulin-dependent diabetic mothers. Pediatrics. 2016;137:e201523424.
Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. 2015;66:14–20.
Chiossi G, Pedroza C, Costantine MM, Truong VTT, Gargano G, Saade GR. Customized vs population-based growth charts to identify neonates at risk of adverse outcome: systematic review and Bayesian meta-analysis of observational studies. Ultrasound Obstet Gynecol. 2017;50:156–66.
Romero R, Tarca AL. Fetal size standards to diagnose a small- or a large-for-gestational-age fetus. Am J Obstet Gynecol. 2018;218:S605–S607.
Sjaarda LA, Albert PS, Mumford SL, Hinkle SN, Mendola P, Laughon SK. Customized large-for-gestational-age birthweight at term and the association with adverse perinatal outcomes. 2014;210:63.e1–63e.11.
Hutcheon JA, Zhang X, Platt RW, Cnattingius S, Kramer MS. The case against customised birthweight standards. Paediatr Perinat Epidemiol. 2011;25:11–16.
Acknowledgements
The authors thank all site investigators and data abstractors of the Canadian Neonatal Network (CNN) and the Canadian Neonatal Follow-Up Network (CNFUN). Full lists of Network member investigators and their affiliations appear in Supplementary Information. We thank Heather McDonald-Kinkaid, PhD, of the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada, for editorial support in preparing this manuscript; and other MiCare staff, for organizational support. MiCare is supported by the Canadian Institutes of Health Research, the Ontario Ministry of Health and Long-Term Care, and the participating hospitals.
Canadian Neonatal Network and the Canadian Neonatal Follow-Up Program
Prakesh S. Shah6, Marc Beltempo7, Jaideep Kanungo8, Joseph Ting9, Ayman Abou Mehrem10, Jennifer Toye11, Khalid Aziz11, Jaya Bodani12, Lannae Strueby13, Mary Seshia14, Deepak Louis14, Ruben Alvaro15, Amit Mukerji16, Orlando Da Silva17, Sajit Augustine18, Kyong-Soon Lee19, Eugene Ng20, Brigitte Lemyre21, Thierry Daboval22, Faiza Khurshid23, Victoria Bizgu24, Keith Barrington25, Christine Drolet26, Bruno Piedboeuf26, Martine Claveau7, Valerie Bertelle27, Edith Masse27, Roderick Canning28, Hala Makary29, Cecil Ojah30, Luis Monterrosa30, Julie Emberley31, Jehier Afifi32, Andrzej Kajetanowicz33, Shoo K. Lee6, Thevanisha Pillay8, Anne Synnes9, Leonora Hendson34, Amber Reichert35, Matthew Hicks35, Jaya Bodani12, Cecilia de Cabo36, Chukwuma Nwaesei18, Thierry Daboval22, Linh Ly19, Edmond Kelly6, Karen Thomas16, Paige Church20, Ermelinda Pelausa24, Kim-Anh Nguyen24, May Khairy37, Marc Beltempo37, Veronique Dorval38, Thuy Mai Luu38, Charlotte Demers28, Alyssa Morin28, Sylvie Bélanger26, Roderick Canning29, Luis Monterrosa31, Hala Makary30, Phil Murphy39.
Funding
Although no specific funding was received for this study, organizational support for the Canadian Neonatal Network and the Canadian Neonatal Follow-Up Network was provided by the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. MiCare is supported by a Canadian Institutes of Health Research (CIHR) Team Grant (CTP 87518), the Ontario Ministry of Health and Long-Term Care, and the participating hospitals. PSS holds a CIHR Applied Research Chair in Reproductive and Child Health Services and Policy Research (APR-126340).
Role of the fundersThe funding bodies played no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
KY: Concept and design, supervised and revised the proposal, drafting of the manuscript, revision of the manuscript. DR: Wrote the proposal, interpreted data, drafting of manuscript, and revision of the manuscript. AS: Reviewed proposal, revision, and critical appraisal of the manuscript, acquisition of data. BA: Reviewed proposal, interpreted data, revision, and critical appraisal of the manuscript. SH: Reviewed proposal, interpreted data, revision, and critical appraisal of the manuscript. CD: Interpreted data, revision, and critical appraisal of the manuscript. EM: Interpreted data, revision, and critical appraisal of the manuscript. PM: Interpreted data, revision, and critical appraisal of the manuscript. PSS: Revision and critical appraisal of the manuscript, acquisition, and analysis of data. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Canadian Neonatal Network and the Canadian Neonatal Follow-Up Program are listed below Acknowledgements.
Supplementary information
Rights and permissions
About this article
Cite this article
Rustogi, D., Synnes, A., Alshaikh, B. et al. Neurodevelopmental outcomes of singleton large for gestational age infants <29 weeks’ gestation: a retrospective cohort study. J Perinatol 41, 1313–1321 (2021). https://doi.org/10.1038/s41372-021-01080-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01080-z
This article is cited by
-
Measuring intrauterine growth in healthy pregnancies using quantitative magnetic resonance imaging
Journal of Perinatology (2022)