Abstract
Objective
Determine how neurodevelopmental impairment (NDI) relates to concurrent outcomes for children born extremely preterm.
Study design
Retrospective cohort study children born 22 0/7–26 6/7 weeks’ gestation at NICHD Neonatal Research Network hospitals. Outcomes were ascertained at 18–22 months’ corrected age.
Result
Of 6562 children, 2618 (40%) died and 441 (7%) had no follow-up. Among the remaining 3483 children, 825 (24%), 1576 (45%), 657 (19%), and 425 (12%) had no, potential/mild, moderate, and severe NDI, respectively. Rehospitalization, respiratory medications, surgery, and medical support services were associated with greater NDI severity but affected >10% of children without NDI. Rehospitalization occurred in 40% of children with no NDI (mean (SD): 1.7 (1.3) episodes).
Conclusion
Medical, functional, and social outcomes at 18–22 months’ corrected age were associated with NDI; however, many children without NDI were affected. These data should contribute to counseling families and the design of studies for childhood outcomes beyond NDI.
Similar content being viewed by others
Introduction
Neurodevelopmental impairment (NDI) is among the most common outcomes reported in studies of neonatal prognosis and therapy. Guidelines recommend discussing NDI in antenatal discussions about what to expect if an infant survives [1]. The outcome of NDI has also become a standard primary endpoint of neonatal clinical trials [2]. Although definitions vary among studies, NDI is commonly defined as having one or more of the following: cerebral palsy, blindness, deafness, or a low score on an assessment of cognitive, language, or motor development (e.g., the Bayley Scales of Infant and Toddler Development) [3].
Some parents, researchers, and clinicians have questioned whether NDI should be extensively used as the primary outcome of prognostic and therapeutic research and whether it adequately represents the concerns of patients, families, and society [4,5,6,7]. Diagnoses such as cerebral palsy and developmental scores may not reflect the day-to-day impact of premature birth in areas such as the need for medical care (e.g., appointments, surgeries, rehospitalizations, and medicines) and daily functioning.
The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network (NRN) collects detailed follow-up outcome data for children born extremely preterm (22–26 weeks’ gestation) at participating NRN centers and so provides a resource for describing the early lives of families of children with and without NDI. The purpose of this study was to describe concurrent outcomes of children born extremely preterm with and without diagnoses of NDI in order to guide clinical care and future research.
Methods
Population
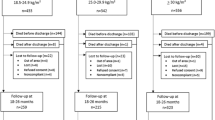
This study included children born at 22 0/7 to 26 6/7 weeks’ gestation between 5/1/2006 and 6/30/2012 in 21 US academic centers participating in the NRN. The end date for the study was defined by the last births with follow-up examinations taking place at 18–22 months’ corrected age (for infants born after 7/1/2012, the timing of NRN follow-up assessments was changed from 18–22 months to 22–26 months’ corrected age). Infants with major congenital anomalies were excluded from the analysis, as factors besides prematurity may impact their outcomes. The institutional review board at each participating site approved NRN in-hospital and follow-up protocols.
Data collection
Trained research personnel at each center obtained data for all liveborn extremely preterm infants using previously described protocols [8, 9]. Gestational age at birth was defined by the best obstetric estimate. Small for gestational age was defined as <10th percentile by gestational age at birth using sex-specific growth charts [10]. Neonatal morbidities included intraventricular hemorrhage (IVH) grade 3–4 [11], necrotizing enterocolitis (NEC) requiring surgical intervention, retinopathy of prematurity (ROP) stage ≥3 [12], and severe bronchopulmonary dysplasia (BPD) defined as supplemental oxygen ≥30% or positive pressure [13].
Follow-up assessments at 18–22 months’ corrected age consisted of standardized neurological examination and administration of the Bayley Scales of Infant and Toddler Development, third edition (Bayley-III) by annually certified examiners [14]. Additional information was obtained through questionnaires, structured interviews, and review of children’s medical records. This information included: post-discharge hospitalizations, medical subspecialty care, medications, and surgeries; home medical equipment use; medical support service utilization; child care arrangements; and information on feeding. Data on hospitalizations, subspecialist visits, and surgeries reflected the duration between initial neonatal intensive care discharge and follow-up evaluation. Medication data reflected use during the 3 months prior to follow-up. Medication data were collected using categories defined by indication without specifying medication names or dosages. Anti-reflux medications included proton-pump inhibitors, H2 antagonists, and prokinetics. Medications for asthma or BPD included inhaled bronchodilators and corticosteroids. Anti-seizure medications included anticonvulsants; thyroid medications included levothyroxine; and anti-spasticity medications included baclofen. Information on medical equipment was recorded if the child used the equipment at follow-up or if it had been ordered for use at that time. Information on medical support service use at the time of follow-up, child care during the month prior to follow-up, and feeding habits at the time of follow-up were reported by the primary caretaker.
NDI classification
NDI was described using the definitions in Table 1. Components of NDI included the Bayley-III cognitive composite score, diagnosis of cerebral palsy, modified Gross Motor Function Classification System (GMFCS) score [15, 16], blindness and deafness. The Bayley-III cognitive composite score has a standardized mean of 100 with standard deviations (SDs) of 15 points, which have been used to define NDI cutoffs (“moderate NDI” being defined as >1 SD below the standardized mean [score <85], “severe NDI” as >2 SD below the standardized mean [score <70]) [17, 18]. Because of controversy about the appropriateness of normative reference cutoffs for Bayley-III scores in our population [19], a “potential/mild NDI” category was defined as a cognitive composite score ≤1 SD below the mean to avoid potential inclusion of children with cognitive composite scores near those used to define NDI in the “no NDI” group. All Bayley-III norms were based on the child’s adjusted age. Per NRN protocols, a modified GMFCS score was determined for all children and ranged from 0 (no abnormalities) to 5 (most severe), with the category of “possible level 1” being reserved for children with toe walking or asymmetric walking, suggesting the potential for mild diplegia or hemiplegia but not diagnostic of cerebral palsy at 18–22 months’ corrected age [20]. The latter was also used to characterize the “potential/mild NDI” group in order to avoid including children with non-diagnostic examiner concerns about motor function in the “no NDI” group. Functional blindness was defined by caretaker report with an exam consistent with bilateral visual acuity <20/200 despite correction. Functional deafness was defined as severe, bilateral hearing loss with or without amplification per caretaker report and consistent with the exam.
Statistical analysis
Differences in the prevalence of outcomes among children in the four NDI groups (none, potential/mild, moderate, and severe NDI) were compared using Cochran-Mantel-Haenszel tests (for categorical variables) and ANCOVA (for continuous variables), as appropriate. The analyses were adjusted for gestational age at birth (in completed weeks), known to be correlated with NDI classification and expected to correlate with several outcomes. A p value <0.05 was considered statistically significant. Corrections for multiple comparisons were not conducted. All analyses were conducted using SAS version 9.4.
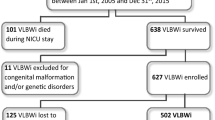
Results
There were 6542 children born at 22–26 weeks’ gestation who were eligible for inclusion. Of these, 2618 (40%) died and 441 (7%) had incomplete follow-up information. Of the remaining 3483 children, 825 (24%), 1576 (45%), 657 (19%), and 425 (12%) had no, potential/mild, moderate, and severe NDI, respectively.
Components of NDI among the children in this cohort are described in Table 2. In all categories, the most prevalent determinant of NDI classification was the Bayley-III cognitive composite score. Cerebral palsy was diagnosed in 6%, 18%, and 49% of children with potential/mild, moderate, and severe NDI, respectively. Blindness and deafness were present among 12% and 24% of children, respectively, with severe NDI.
Among infants surviving to follow-up, 17/27 (63%), 106/253 (42%), 293/786 (37%), 348/1122 (31%), and 318/1295 (25%) of children born at 22, 23, 24, 25, and 26 weeks’ gestation had moderate or severe NDI. As shown in Table 3, severity of NDI was associated with lower birth weight, male sex, 1-minute Apgar score ≤3, no exposure to antenatal corticosteroids, small for gestational age, maternal self-identification as non-white race, and lack of private insurance (p < 0.001). Severity of NDI was also associated with increased rates of grade 3–4 IVH, surgical NEC, stage ≥3 ROP, and severe BPD.
NDI severity was associated with several concurrent outcomes at 18–22 months’ corrected age overall (Table 4) and at each gestational age (Supplemental Tables A1–A4). Rehospitalization following discharge from the neonatal intensive care unit was common for all children born extremely preterm, regardless of NDI severity, with 331/825 (40%) of children with no NDI and 300/425 (70%) of children with severe NDI rehospitalized by 18–22 months’ corrected age. Children without NDI were rehospitalized, on average, 1.7 times (SD 1.3) before 18–22 months’ corrected age and children with severe NDI 3.2 (SD 3.1) times. The most common reason for rehospitalization was respiratory disease. Regardless of NDI status, large proportions of children in each NDI category (17–31%) used medications at 18–22 months’ corrected age to treat asthma or BPD. Similarly, tympanostomy tube placement (rates of 9–16% across NDI categories) and hernia repair (rates of 11–17% across NDI categories) were common among all children born extremely preterm, regardless of NDI status.
While nearly one quarter (82/361) of children with severe NDI had gastrostomy tube placement by 18–22 months’ corrected age, there was evidence of functional feeding difficulties in all NDI categories and 2% (15/725) of children with no NDI had a gastrostomy tube placed. With no NDI, 96% of children could feed themselves at 18–22 months’ corrected age, whereas 44% of children with severe NDI were able to feed themselves.
Use of medical equipment and medical support services was more common among children with severe NDI. Among children without NDI, 17% utilized physical and occupational therapy at 18–22 months and 21% utilized speech therapy services. These compare to 75% and 53%, respectively, among children with severe NDI. The utilization of traditional home-based or center-based daycare was much more common among children with no NDI (33%) than those with severe NDI (11%).
Discussion
In a cohort of children born extremely preterm, NDI severity was associated with increased rates of rehospitalization, medical subspecialty visits, surgeries, medication and equipment use, specialty medical child care, and functional feeding difficulties at 18–22 months’ corrected age. However, children born extremely preterm with no diagnosis of NDI also had high rates of rehospitalization, surgery, and medical utilization.
Childhood outcomes of extremely preterm infants have been extensively studied [21]. However, few others have described non-NDI outcomes in relation to NDI diagnosis [22, 23]. Our study raises important questions about how to best design and report studies of the outcomes of extremely premature birth. At a workshop held jointly by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Society for Maternal–Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists, participants recommended that “Physicians should recognize that the parents’ views on what is a ‘severe’ disability may be different from those of the researchers or clinicians…” [24] Others, including the Core Outcomes in Neonatology group, have worked with key stakeholders, including families, healthcare providers, and members of society, to evaluate which outcomes of prematurity are of importance to these stakeholders to collect and report in neonatal studies [25,26,27]. These outcomes include respiratory illnesses, readmissions, multiple operations, and the effects of a child’s illness on the family [26].
Strengths of this study include the large number of infants and high rates of follow-up in the NICHD Neonatal Research Network, as well as the availability of standardized data obtained by annually certified research personnel to diagnose NDI. The data included outcomes from academic medical centers across the United States representing various geographies and populations. NDI data from the NRN have been widely used in prognostic studies and clinical trials to help guide care of extremely preterm infants in the United States and around the world [28,29,30,31].
Limitations of this study include the post-hoc design of the analysis, which used only available data and precluded the ability to obtain additional information on family and parental quality of life, employment, education, relationships, health, and other outcomes. Moreover, this study was intended to be descriptive and was not designed to determine which factors affected both NDI and other outcomes at follow-up, such as neonatal morbidities or socioeconomic hardships. Importantly, follow-up data were limited to those collected at 18–22 months’ corrected age and provide only a snapshot from that time. NDI diagnoses may vary over children’s lives and assessments at later ages may have resulted in some children changing NDI categories [32, 33]. However, although 18–22 month outcomes may not adequately reflect long-term function or needs, data collected at 2 years’ corrected age are frequently used for perinatal decision-making [1].
Unlike many other neonatal morbidities, such as IVH [11] and retinopathy of prematurity [12], NDI does not have a consensus definition. Published definitions vary widely across studies [34]. Small variations in the definition of NDI can have a substantial influence on its rate in a population and on its association with specific variables [35, 36]. Despite this, studies of NDI in children born extremely preterm are used as the basis for recommendations to make treatment decisions, including whether to direct care toward survival or palliation [1, 24], and are frequently used as a component of the primary outcome of major clinical trials [2]. For the purposes of our study, we presented results separately for “no NDI” and “potential/mild NDI.” While the clinical significance of the “potential/mild NDI” category is debatable, at least one group has suggested using cutoffs as high as 95 for the Bayley-III cognitive composite score to indicate problems with cognitive development [37]. In our study, the designation was used to avoid misclassification of marginal cases in the “no NDI” group, which was important to study adverse outcomes among children without NDI. The definitions of NDI used in this study are similar to those used elsewhere [15] but cannot be compared with studies using different NDI definitions or criteria.
In conclusion, we found that severity of NDI was associated with several other important medical, functional, and social outcomes at 18–22 months’ corrected age. However, children born extremely preterm without an NDI diagnosis had substantial medical needs following discharge that may significantly impact families and the healthcare system. These data should be useful to support counseling families and the design of studies for early childhood outcomes beyond NDI.
References
Periviable birth. Obstetric Care Consensus No. 6. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2017;130:e187–99.
Marlow N. Is survival and neurodevelopmental impairment at 2 years of age the gold standard outcome for neonatal studies? Arch Dis Child Fetal Neonatal Ed. 2015;100:F82–4.
Torchin H, Morgan AS, Ancel P-Y. International comparisons of neurodevelopmental outcomes in infants born very preterm. Semin Fetal Neonatal Med. 2020;25:101109.
Kilbride HW, Aylward GP, Doyle LW, Singer LT, Lantos J. Prognostic neurodevelopmental testing of preterm infants: do we need to change the paradigm? J Perinatol. 2017;37:475–9.
McCormick MC, Litt JS. The outcomes of very preterm infants: is it time to ask different questions? Pediatrics. 2017;139:e20161694.
Jaworski M, Janvier A, Lefebvre F, Luu TM. Parental perspectives regarding outcomes of very preterm infants: toward a balanced approach. J Pediatr. 2018;200:58–63.e1.
Daly M. Parental perspective on neonatal outcomes. BMJ Paediatr Open. 2019;3:e000404.
Generic Database of Very Low Birth Weight Infants (GDB). NIH U.S. National Library of Medicine. Clinicaltrials.gov. https://www.clinicaltrials.gov/ct2/show/NCT00063063. Accessed 8 June 2020.
Follow-up Visit of High Risk Infants (FU). NIH U.S. National Library of Medicine. Clinicaltrials.gov. https://www.clinicaltrials.gov/ct2/show/NCT00063063. Accessed 8 June 2020.
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163–8.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Newman JE, Bann CM, Vohr BR, Dusick AM, Higgins RD. Improving the Neonatal Research Network annual certification for neurologic examination of the 18–22 month child. J Pediatr. 2012;161:1041–6.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000;80:974–85.
Johnson S, Moore T, Marlow N. Using the Bayley-III to assess neurodevelopmental delay: which cut-off should be used? Pediatr Res. 2014;75:670–4.
Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017;376:617–28.
Anderson PJ, De Luca CR, Hutchinson E, Roberts G, Doyle LW. Underestimation of developmental delay by the new Bayley-III Scale. Arch Pediatr Adolesc Med. 2010;164:352–6.
Vohr BR, Msall ME, Wilson D, Wright LL, McDonald S, Poole WK. Spectrum of gross motor function in extremely low birth weight children with cerebral palsy at 18 months of age. Pediatrics. 2005;116:123–9.
Kilbride HW, Aylward GP, Carter B. What are we measuring as outcome? Looking beyond neurodevelopmental impairment. Clin Perinatol. 2018;45:467–84.
Stephens BE, Bann CM, Poole WK, Vohr BR. Neurodevelopmental impairment: predictors of its impact on the families of extremely low birth weight infants at 18 months. Infant Ment Health J. 2008;29:570–87.
Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins RD. Community supports after surviving extremely low-birth-weight, extremely preterm birth. Arch Pediatr Adolesc Med. 2008;162:748–55.
Raju TNK, Mercer BM, Burchfield DJ, Joseph GF Jr. Periviable birth: executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Obstet Gynecol. 2014;123:1083–96.
Webbe J, Brunton G, Ali S, Duffy JM, Modi N, Gale C, et al. Developing, implementing and disseminating a core outcome set for neonatal medicine. BMJ Paediatr Open. 2017;1:e000048.
Webbe J, Brunton G, Ali S, Longford N, Modi N, Gale C, et al. Parent, patient and clinician perceptions of outcomes during and following neonatal care: a systematic review of qualitative research. BMJ Paediatr Open. 2018;2:e000343.
Mitra S, Reid M, McDougall B, Johnston BC. Are neonatal clinical practice guidelines truly evidence‐based? A case for incorporating family values and preferences. Acta Paediatr. 2019;108:1564–6.
Morris BH, Oh W, Tyson JE, Stevenson DK, Phelps DL, O’Shea TM, et al. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N Engl J Med. 2008;359:1885–96.
Laparotomy vs. drainage for infants with necrotizing enterocolitis (NEST). Clinicaltrials.gov. https://www.clinicaltrials.gov/ct2/show/NCT01029353. Accessed 8 June 2020.
Transfusion of prematures trial (TOP). Clinicaltrials.gov. https://www.clinicaltrials.gov/ct2/show/NCT01702805. Accessed 8 June 2020.
Rysavy MA, Horbar JD, Bell EF, Li L, Greenberg LT, Tyson JE, et al. Assessment of an updated Neonatal Research Network Extremely Preterm Birth Outcome Model in the Vermont Oxford Network. JAMA Pediatr. 2020;174:e196294.
Ment LR, Vohr B, Allan W, Katz KH, Schneider KC, Westerveld M, et al. Change in cognitive function over time in very low-birth-weight infants. JAMA. 2003;289:705–11.
Marlow N, Wolke D, Bracewell MA, Samara M. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352:9–19.
Shah PS. Neonatal intensive care—the only constant is change. N Engl J Med. 2017;376:694–6.
Haslam MD, Lisonkova S, Creighton D, Church P, Yang J, Shah PS, et al. Severe neurodevelopmental impairment in neonates born preterm: impact of varying definitions in a Canadian cohort. J Pediatr. 2018;197:75–81.e4.
DeMauro SB, Schmidt B. Comparing like with like when reporting neurodevelopmental outcomes after preterm birth. J Pediatr. 2018;197:10–2.
Spencer-Smith MM, Spittle AJ, Lee KJ, Doyle LW, Anderson PJ. Bayley-III cognitive and language scales in preterm children. Pediatrics. 2015;135:e1258.
Acknowledgements
See Supplementary Information for additional acknowledgements.
Funding
This research was supported by the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
MAR conceptualized and designed the study, interpreted and directed statistical analyses, drafted the initial manuscript, and made revisions to subsequent drafts. TTC assisted with conceptualization and design of the study, coordinated and supervised data collection, and reviewed manuscript drafts. CMB provided statistical input on the analysis plan, conducted statistical analyses, and reviewed manuscript drafts. KJJ and SBD, AFD, JEB, MPC, HMH, SRH, BRV, and EFB coordinated and supervised data collection and reviewed manuscript drafts. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The names and affiliations for the members of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network can be found in Supplementary information.
Supplementary information
Rights and permissions
About this article
Cite this article
Rysavy, M.A., Colaizy, T.T., Bann, C.M. et al. The relationship of neurodevelopmental impairment to concurrent early childhood outcomes of extremely preterm infants. J Perinatol 41, 2270–2278 (2021). https://doi.org/10.1038/s41372-021-00999-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00999-7
This article is cited by
-
Prenatal risk factors and neonatal DNA methylation in very preterm infants
Clinical Epigenetics (2021)