Abstract
Objective:
To characterize the risk factors for late-onset circulatory collapse (LCC) in preterm infants responsive to corticosteroid therapy and evaluate the long-term neurological prognosis.
Study Design:
A retrospective case–control study for preterm infants (⩽32 weeks’ gestation) admitted to our neonatal intensive care unit from 1994 through 2002.
Result:
Sixty-five infants (11%) were diagnosed with LCC. Infants with a shorter gestation and lower birth weight had a higher incidence of LCC. LCC infants had a significantly lower 1-min Apgar score, significantly higher incidence of severe intraventricular hemorrhage, chronic lung disease, and postnatal periventricular leukomalacia, and significantly longer duration of ventilation use, oxygen use, and hospital stay. Somatic growth at 36 weeks’ postmenstrual age was poorer in infants with LCC than without LCC (controls). LCC infants were significantly more likely than controls to have cerebral palsy at 3 years.
Conclusion:
LCC is associated with poor neurodevelopmental outcomes. Prevention of LCC can lead to improved neurological prognoses.
Similar content being viewed by others
Introduction
There have been several reports on corticosteroid-responsive hypotension among very low birth weight (VLBW) infants during the early postnatal period.1, 2, 3, 4, 5, 6 Some reports mention the presence of impaired adrenal function in preterm infants in the immediate postnatal period.7, 8, 9 However, the adrenal insufficiency in these preterm infants usually returns to normal by the end of the second week of life.10 However, according to a recent nationwide survey in Japan, a significant proportion (4%) of VLBW infants may develop corticosteroid-responsive circulatory collapse beyond the first week of life.11 This study focuses on corticosteroid-responsive hypotension among VLBW infants after the first week of life, referred to as late-onset circulatory collapse (LCC). Most infants with LCC show sudden systemic hypotension and oliguria accompanied by hyponatremia and hyperkalemia, and do not respond to conventional treatment with a volume expander or vasopressor-inotrope support. Corticosteroid administration dramatically improves LCC. Recently, the adrenal insufficiency associated with premature birth has been proposed as being involved in the pathogenesis of LCC.12, 13 The objective of this study was to describe the characteristics and neonatal complications of infants with LCC during the hospital stay, identify its adverse effects, and evaluate long-term neurodevelopmental outcomes.
Methods
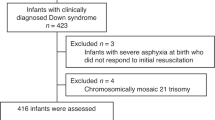
From January 1994 to December 2002, 735 premature infants (⩽32 weeks of gestation) were admitted to the neonatal intensive care unit (NICU) at Osaka City General Hospital. As no case with LCC was found beyond 32 weeks of gestation, infants over 32 weeks were excluded. Among these patients, 68 had a life-threatening congenital anomaly or chromosomal anomaly and were excluded. In addition, 84 infants who died during the first month were also excluded. Among the remaining 583 preterm infants, 65 were diagnosed with LCC and were included in this study.
Case–control study to evaluate long-term outcomes
According to our preliminary study, the gestation and birth weight of LCC infants were significantly lower than those in infants without LCC (mean±s.d.; 25.4±1.7 weeks vs 28.8±2.4 weeks, P<0.001; 776±184 g vs 1209±369 g, P<0.001, respectively). Therefore, to exclude the potential effect of prematurity on the analysis of long-term outcomes of LCC, we performed a matched 1:2 case–control study by matching LCC infants with those without LCC (control infants) whose gestational age matched within ⩽1 week. Finally, 26 and 52 infants with and without LCC, respectively, who were followed for at least 3 years underwent additional analyses to determine additional risk factors for LCC.
Definition
LCC was diagnosed according to the clinical criteria for corticosteroid treatment in our NICU. Only infants who received corticosteroid treatment for LCC were included in our study. Four symptoms were assessed: (1) sudden systemic hypotension (mean arterial pressure (MAP) <35 mm Hg sustained for at least 3 h); (2) oliguria (<1 ml kg−1h−1 during an 8-h interval); (3) electrolyte abnormality (hyponatremia <130 mEq l−1, hyperkalemia >5.5 mEq l−1); and (4) excess body weight gain per day (15 g kg−1 per day or 1.5% per day). When more than two of these symptoms were detected 7 or more days postnatally, and after all other common conditions causing systemic hypotension and oliguria, such as hypovolemia, dehydration, symptomatic patent ductus arteriosus (PDA), and sepsis were ruled out, corticosteroid treatment was started. The dose of corticosteroid was 1 to 5 mg kg−1 per dose of hydrocortisone or 0.1 to 0.2 mg kg−1 per dose of dexamethasone. Once the infant responded to corticosteroid therapy, LCC was diagnosed. Daily changes in body weight, MAP, serum sodium and potassium concentrations, and urine output before and at symptom onset were also assessed to help the attending physician make the diagnosis of LCC.
We measured the arterial blood pressure at least every 3 h by the oscillometric technique because most infants did not have an arterial catheter after the first week of life. If the infant was stable, blood pressure was measured, at minimum, once daily. If an arterial line was present, we measured arterial blood pressure using a pressure transducer through the catheter. A cutoff value of MAP of 35 mm Hg was used to define hypotension based on an earlier study.14 Electrolytes were measured daily within 1 week of birth and once weekly thereafter.
Maternal hypertension and maternal diabetes mellitus (DM) or gestational DM (GDM) were diagnosed according to the diagnostic criteria.15 Premature rupture of membranes (PROM) was defined as rupture of membranes before onset of labor. Antenatal steroid treatment was defined as administration of any corticosteroid to accelerate fetal lung maturity. Chorioamnionitis (CAM) was diagnosed histologically by pathologists in our hospital.
Respiratory distress syndrome (RDS) was diagnosed based on clinical and radiographic findings. PDA was diagnosed based on the echocardiographic findings and clinical evidence of volume overload because of a left–right shunt. Intraventricular hemorrhage (IVH) was diagnosed according to the criteria of Papile classification,16 with head ultrasound performed before 14 days of life. Necrotizing enterocolitis (NEC) was defined according to the criteria of Bell et al.17 Gastrointestinal perforation was diagnosed when free air was detected in the abdominal cavity by radiograph examination.
Chronic lung disease (CLD) was defined when an infant received supplemental oxygen on the 28th day after birth, and 36-week CLD was defined when an infant received supplemental oxygen at 36 weeks’ postmenstrual age (PMA). Retinopathy of prematurity (ROP) was defined according to the International Classification for Retinopathy of Prematurity.18
Periventricular leukomalacia (PVL) was defined as evidence of periventricular cysts (>3 mm) on a cranial ultrasound routinely performed on days 0, 1, 2, 7, 14, 21, 28 and more frequently if clinically indicated until 40 weeks’ PMA. Some PVL cases were also diagnosed with cranial computed tomography (CT) scanning and magnetic resonance imaging (MRI) scanning at hospital discharge by detecting ventricular dilatation, reduction in periventricular white matter, or irregularities of the lateral ventricular walls. To distinguish postnatal risk factors of PVL from antenatal or perinatal ones, PVL was classified into two groups: PVL diagnosed before 28 days was defined as perinatal PVL, whereas PVL diagnosed after 28 days was defined as postnatal PVL. All preterm infants with PVL had the diagnosis further confirmed with MRI and tests for neurodevelopmental abnormalities at 3 years of age.
CP was defined as abnormal muscle tone in at least one extremity and abnormal control of movement and posture at 3 years of age.
Risk factors
Patient data were retrospectively collected from the hospital record. LCC infants were compared with control patients with regard to several variables. We assessed birth weight, gestational age, birth weight s.d. score, male gender, patients born at other hospitals and then transferred to our hospital, multiple births, 1- and 5-min Apgar scores, surfactant therapy, MAP, ventilatory index, and A-aDO2 on admission to NICU. Perinatal characteristics consisted of maternal hypertension, maternal DM/GDM, PROM, antenatal steroid treatment, CAM, and vaginal delivery. Neonatal complications consisted of RDS, pulmonary hemorrhage, PDA, IVH, and NEC/gastrointestinal perforation. Short-term prognosis consisted of supplemental oxygen at 28 days after birth and 36 weeks’ PMA, body weight at 28 days after birth and 36 weeks’ PMA, and total length of mechanical ventilation, O2 supplement and hospital stay, ROP, and PVL. Long-term prognosis was evaluated by the presence or absence of CP at 3 years.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (version 17.0 SPSS, Chicago, IL, USA). Data were summarized as mean±s.d. or median and ranges. χ2-test or Fisher's exact test was used with odds ratio (OR) and 95% confidence intervals (95% CI) for categorical variables to test differences between infants with or without LCC. A Mann–Whitney U test or an unpaired t-test was used to compare continuous variables. A P-value <0.05 was considered significant.
Study approval
This study was approved by the internal review board of the hospital. The study was a retrospective anonymous clinical analysis; thus, permission from parents was waived.
Results
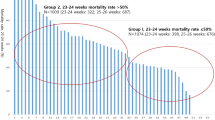
Overall, a total of 65 infants (11.1%) were diagnosed with LCC. The incidence of LCC increased in accordance with lower gestational age, occurring in 8 of 13 (61.5%) at 23 weeks’ gestation, 14 of 35 (40.0%) at 24 weeks’ gestation, 13 of 46 (28.3%) at 25 weeks’ gestation, 11 of 53 (20.8%) at 26 weeks’ gestation, 13 of 77 (16.9%) at 27 weeks’ gestation, 5 of 57 (8.8%) at 28 weeks’ gestation, 0 of 237 (0.0%) at 29, 30, and 32 weeks’ gestation, and 1 of 65 (1.5%) at 31 weeks’ gestation. The median number of days after birth for LCC occurrence was 19 (range, 7 to 48 days), which corresponds to around 29 weeks’ gestation.
Of the 65 infants with LCC, only 26 were followed over 3 years and were included in the rest of the analyses.
Changes in body weight, MAP, serum Na and K concentrations, and urine output
Changes in body weight, MAP, serum Na and K concentrations, and urine output around the onset of LCC are shown in Table 1. Each parameter significantly changed at the onset of LCC compared with before onset of LCC. These changes were important factors that helped the attending physician make a diagnosis of LCC. After corticosteroid treatment, all values returned to findings seen before LCC onset. The median time intervals from before, onset, and after LCC were 2 days (range, 2 to 4 days).
Basic and perinatal characteristics and incidence of neonatal complications among LCC infants
Gestation and birth weight did not differ between LCC and control infants (mean±s.d., 25.7±1.5 weeks vs 26.2±1.1 weeks; 741±166 g vs 811±144 g, respectively). Apgar score at 1 min was significantly lower in LCC infants (median 3, range 1 to 8) than in controls (median 5, range 1 to 8; P<0.05) (Table 2).
There were no significant differences between perinatal characteristics among LCC infants and controls. In terms of neonatal complications, infants with LCC had a significantly higher incidence of grade ⩾3 IVH (P<0.01).
Short- and long-term prognosis of LCC infants
LCC infants had a significantly higher incidence of 36-week CLD than controls (P<0.05). The length of mechanical ventilation (P<0.05), O2 supplementation (P<0.05), and hospital stay (P<0.01) were significantly longer in LCC infants. In addition, body weight at 36 weeks’ PMA was significantly lower in LCC infants than controls (P<0.05) (Table 3).
LCC infants had a significantly greater incidence of postnatal PVL than controls (P<0.01). In addition, they had a significantly higher incidence of CP at 3 years of age compared with controls (P<0.001). Among LCC infants, eight were treated with dexamethasone, but this was not a significant factor for the high incidence of CP (P=0.64; OR, 1.15; 95% CI, 0.17 to 7.7).
We obtained MRI findings of six LCC infants with CP and two controls with CP at 3 years of age. The primary findings among these infants were four cases of reduction in periventricular white matter, three cases of enlargement of the lateral ventricles, three cases of thinning of the corpus callosum, three cases of cerebellum atrophy, and two cases of irregularities of the lateral ventricular walls.
Discussion
In the past several years, patients with sudden cardiac dysfunction after the first week of life, such as systemic hypotension and oliguria accompanied by hyponatremia and hyperkalemia, have been shown to dramatically improve with corticosteroid administration. These pathological conditions, which are clearly different from the unstable circulatory status observed in the acute phase of premature babies soon after birth, have been recently defined as LCC in Japan.
With the independent diagnostic criteria of LCC in our hospital, we found that about 11% of preterm infants at ⩽32 weeks’ gestation were diagnosed with LCC. Birth weight and gestational ages of LCC infants were significantly lower than those without LCC. The occurrence of LCC was higher with smaller gestational ages, and in addition to hypotension and oliguria, LCC infants showed abnormal serum electrolyte changes. These results indicate that prematurity is one of the most important characteristics of LCC, and we speculate that adrenal insufficiency may explain this presentation.12, 13
In this analysis, we performed a 1:2 case–control study by matching LCC infants with controls whose gestational age differed by ⩽1 week to help eliminate the role of prematurity in LCC. This study is unique because for the first time we determined the long-term prognosis of LCC infants, who experienced a significantly greater incidence of CP at 3 years of age compared with control infants. In addition, according to our results, LCC infants had a higher incidence of severe IVH and CLD at 36 weeks’ PMA, and poorer neurological prognosis such as postnatal PVL.
As previously reported, premature infants have a decreased capacity to synthesize cortisol, which may lead to a relative adrenal insufficiency and significant illness.19, 20, 21 It is conceivable that the pathogenesis of LCC correlates with the adrenal function of preterm infants,12 and the high incidence of CLD in LCC infants in this study is consistent with these reports.
Both prenatal and postnatal pathophysiologic mechanisms can induce PVL.22, 23, 24, 25, 26 A postnatal form of cystic PVL has been previously reported among eight cases detected by ultrasound between 16 days and 10 weeks after birth.27 Another report described a postnatal form of cystic PVL appearing beyond the first 5 weeks of life in a large population of preterm infants born before 33 weeks.28 Recently, Kobayashi et al.29 performed a small case–case control study of preterm infants (⩽32 weeks’ gestation) and demonstrated a significant association between late-onset PVL and late-onset circulatory dysfunction among these infants. As there is no treatment for PVL, it is important to stabilize the cerebral circulation, especially between the 28th and 32nd weeks of gestation, during which LCC was most prevalent in this study. In addition, LCC should be treated immediately to prevent postnatal PVL.
This study showed that LCC infants had a significantly greater chance of developing CP at 3 years of age. As the dose of steroid therapy used to treat LCC was within the physiological range, it is unlikely that poor neurological outcome occurred from excess use of steroid therapy.30, 31 Moreover, contrary to the use of dexamethasone, hydrocortisone administration (early or late) may not be associated with an increased incidence of CP. The high incidence of severe IVH (19%) and postnatal PVL (27%) in LCC infants might be correlated with the high incidence of CP. However, considering that 73% of LCC infants developed CP, it is possible that LCC may independently contribute to CP. On the other hand, in this study, diffuse PVL might have been missed by the routine ultrasonography because early MRI or CT was not done. In addition, MRI at discharge was not routinely performed, and MRI at 3 years of age was only performed on study group patients with CP. Thus, more LCC infants might have developed PVL, and that might be the reason for the high rate of CP in LCC infants.
This study has several limitations. Among the 735 infants admitted to our NICU, only 212 patients (26 LCC infants and 186 controls) were followed until 3 years of age because of lack of clinical records. This large attrition of records makes it difficult to set up a population-based study to determine the risk factors for long-term prognosis of LCC. In addition, this was a single-center analysis, and we cannot generalize the association between LCC and the other causative risk factors to other populations. Another weakness of this study was that because serum cortisol levels and stimulation tests were not performed, we could not directly determine the correlation between LCC and adrenal insufficiency.
LCC, which occurs at the most vulnerable time for white matter injury, may be an important risk factor for PVL and CP, and its development may identify a more vulnerable patient population. As there are no curative therapies for PVL and CP, LCC should be rapidly diagnosed and treated. A multicenter, large-scale study is warranted to elucidate the pathogenesis of LCC and its correlation with poor neurological development.
References
Helbock HJ, Insoft RM, Conte FA . Glucocorticoid-responsive hypotension in extremely low birth weight newborns. Pediatrics 1993; 92 (5): 715–717.
Fauser A, Pohlandt F, Bartmann P, Gortner L . Rapid increase of blood pressure in extremely low birth weight infants after a single dose of dexamethasone. Eur J Pediatr 1993; 152 (4): 354–356.
Sasidharan P . Role of corticosteroids in neonatal blood pressure homeostasis. Clin Perinatol 1998; 25 (3): 723–740, xi.
Gaissmaier RE, Pohlandt F . Single-dose dexamethasone treatment of hypotension in preterm infants. J Pediatr 1999; 134 (6): 701–705.
Ng PC, Lam CW, Fok TF, Lee CH, Ma KC, Chan IH et al. Refractory hypotension in preterm infants with adrenocortical insufficiency. Arch Dis Child Fetal Neonatal Ed 2001; 84 (2): F122–F124.
Seri I, Tan R, Evans J . Cardiovascular effects of hydrocortisone in preterm infants with pressor-resistant hypotension. Pediatrics 2001; 107 (5): 1070–1074.
Heckmann M, Wudy SA, Haack D, Pohlandt F . Serum cortisol concentrations in ill preterm infants less than 30 weeks gestational age. Acta Paediatr 2000; 89 (9): 1098–1103.
Watterberg KL, Gerdes JS, Cook KL . Impaired glucocorticoid synthesis in premature infants developing chronic lung disease. Pediatr Res 2001; 50 (2): 190–195.
Fernandez E, Schrader R, Watterberg K . Prevalence of low cortisol values in term and near-term infants with vasopressor-resistant hypotension. J Perinatol 2005; 25 (2): 114–118.
Ng PC, Lee CH, Lam CW, Ma KC, Fok TF, Chan IH et al. Transient adrenocortical insufficiency of prematurity and systemic hypotension in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2004; 89 (2): F119–F126.
Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y et al. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics 2006; 118 (4): e1130–e1138.
Masumoto K, Kusuda S, Aoyagi H, Tamura Y, Obonai T, Yamasaki C et al. Comparison of serum cortisol concentrations in preterm infants with or without late-onset circulatory collapse due to adrenal insufficiency of prematurity. Pediatr Res 2008; 63 (6): 686–690.
Miwa M, Kusuda S, Ikeda K . International perspectives: late-onset circulatory collapse in very low-birthweight infants: a Japanese perspective. Neoreviews 2009; 10 (8): e381–e386.
Hegyi T, Anwar M, Carbone MT, Ostfeld B, Hiatt M, Koons A et al. Blood pressure ranges in premature infants: II. The first week of life. Pediatrics 1996; 97 (3): 336–342.
Sugaya A, Sugiyama T, Nagata M, Toyoda N . Comparison of the validity of the criteria for gestational diabetes mellitus by WHO and by the Japan Society of Obstetrics and Gynecology by the outcomes of pregnancy. Diabetes Res Clin Pract 2000; 50 (1): 57–63.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92 (4): 529–534.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187 (1): 1–7.
Ben-Sira I . An international classification of retinopathy of prematurity. Pediatrics 1984; 74 (1): 127–133.
Watterberg KL, Scott SM . Evidence of early adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics 1995; 95 (1): 120–125.
Huysman MW, Hokken-Koelega AC, De Ridder MA, Sauer PJ . Adrenal function in sick very preterm infants. Pediatr Res 2000; 48 (5): 629–633.
Yoder B, Martin H, McCurnin DC, Coalson JJ . Impaired urinary cortisol excretion and early cardiopulmonary dysfunction in immature baboons. Pediatr Res 2002; 51 (4): 426–432.
Leviton A, Paneth N, Reuss ML, Susser M, Allred EN, Dammann O et al. Maternal infection, fetal inflammatory response, and brain damage in very low birth weight infants. Developmental Epidemiology Network Investigators. Pediatr Res 1999; 46 (5): 566–575.
Perlman JM, Risser R, Broyles RS . Bilateral cystic periventricular leukomalacia in the premature infant: associated risk factors. Pediatrics 1996; 97 (6 Part 1): 822–827.
Murphy DJ, Sellers S, MacKenzie IZ, Yudkin PL, Johnson AM . Case-control study of antenatal and intrapartum risk factors for cerebral palsy in very preterm singleton babies. Lancet 1995; 346 (8988): 1449–1454.
De Felice C, Toti P, Laurini RN, Stumpo M, Picciolini E, Todros T et al. Early neonatal brain injury in histologic chorioamnionitis. J Pediatr 2001; 138 (1): 101–104.
Okumura A, Hayakawa F, Kato T, Itomi K, Maruyama K, Ishihara N et al. Hypocarbia in preterm infants with periventricular leukomalacia: the relation between hypocarbia and mechanical ventilation. Pediatrics 2001; 107 (3): 469–475.
de Vries LS, Regev R, Dubowitz LM . Late onset cystic leucomalacia. Arch Dis Child 1986; 61 (3): 298–299.
Andre P, Thebaud B, Delavaucoupet J, Zupan V, Blanc N, d’Allest AM et al. Late-onset cystic periventricular leukomalacia in premature infants: a threat until term. Am J Perinatol 2001; 18 (2): 79–86.
Kobayashi S, Fujimoto S, Koyama N, Fukuda S, Iwaki T, Tanaka T et al. Late-onset circulatory dysfunction of premature infants and late-onset periventricular leukomalacia. Pediatr Int 2008; 50 (2): 225–231.
Lodygensky GA, Rademaker K, Zimine S, Gex-Fabry M, Lieftink AF, Lazeyras F et al. Structural and functional brain development after hydrocortisone treatment for neonatal chronic lung disease. Pediatrics 2005; 116 (1): 1–7.
Watterberg KL, Shaffer ML, Mishefske MJ, Leach CL, Mammel MC, Couser RJ et al. Growth and neurodevelopmental outcomes after early low-dose hydrocortisone treatment in extremely low birth weight infants. Pediatrics 2007; 120 (1): 40–48.
Acknowledgements
We thank Hiroyuki Ichiba for helping us to collect medical records at Osaka City General Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Nakanishi, H., Yamanaka, S., Koriyama, T. et al. Clinical characterization and long-term prognosis of neurological development in preterm infants with late-onset circulatory collapse. J Perinatol 30, 751–756 (2010). https://doi.org/10.1038/jp.2010.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.41
Keywords
This article is cited by
-
Clinical risk factors for the development of late-onset circulatory collapse in premature infants
Pediatric Research (2021)
-
Late-onset Circulatory Collapse and Continuous Positive Airway Pressure are Useful Predictors of Treatment-requiring Retinopathy of Prematurity: A 9-year Retrospective Analysis
Scientific Reports (2017)
-
Trends in morbidity and mortality among very-low-birth-weight infants from 2003 to 2008 in Japan
Pediatric Research (2012)