Abstract
Lincomycin derivatives that have a 5-(2-nitrophenyl)-1,3,4-thiadiazol-2-yl thio moiety at the 7-position were synthesized. 5-Substituted 2-nitrophenyl derivatives showed potent antibacterial activities against Streptococcus pneumoniae and Streptococcus pyogenes with erm gene. Antibacterial activities of the 4,5-di-substituted 2-nitrophenyl derivatives were generally comparable to those of telithromycin (TEL) against S. pneumoniae with erm gene and clearly superior to those of TEL against S. pyogenes with erm gene. Compounds 6 and 10c that have a methoxy group at the 5-position of the benzene ring exhibited activities comparable to TEL against Haemophilus influenzae. These results suggest that lincomycin derivatives modified at the 7-position would be promising compounds as a clinical candidate. We would like to dedicate this article to the special issue for late Professor Dr. Hamao Umezawa in The Journal of Antibiotics.
Similar content being viewed by others
Introduction
Macrolide antibiotics have been widely used for respiratory infections over many years. Especially, clarithromycin1 and azithromycin2 (Figure 1) are clinically important macrolides derived from a natural product, erythromycin (EM). Clarithromycin is distinct from EM in improved pharmacokinetics because of its stability in acidic condition. Azithromycin has a long plasma half-life and good tissue distribution, and shows stronger antibacterial activity than EM against Gram-negative bacteria such as Haemophilus influenzae. However, an emergence of macrolide-resistant bacteria, such as Streptococcus pneumonia, has been causing serious clinical problems.3, 4 Ketolides, such as TEL,5 cethromycin,6 solithromycin7 and nafithromycin8 (Figure 1), newly developed/derived from natural EM, show antibacterial activities against resistant pathogens. Much effort has been made to launch ketolides, which were effective against macrolide-resistant bacteria, but only TEL has been marketed so far. Its safety problems,9 however, make it difficult to be used in the clinical site. Another promising class is 16-membered azalides10 that are effective against resistant S. pneumoniae and S. pyogenes with erm gene. These compounds, however, are still under research process and have not entered clinical phase. Thus, currently there is no clinically available drug that is effective against resistant S. pneumoniae with erm and mef genes and free of safety or taste problem.
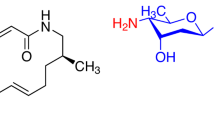
Lincomycin (LCM)11 was produced by Streptomyces lincolnensis and has been used as antibacterial agent mainly against Gram-positive bacteria. Chemical modification of LCM led to clindamycin (CLDM)12 that has an enhanced antibacterial activity against S. pneumoniae and an improved pharmacokinetic profile (Figure 2). Lincosamide antibiotics inhibit protein synthesis acting on 50S ribosome in a similar way to macrolide antibiotics. This similar mode of action led to cross-resistance against clinically problematic S. pneumoniae and S. pyogenes with erm gene.13 Thus, CLDM shows almost no antibacterial activity against these resistant pathogens as shown in Table 1. CLDM, however, is attractive because of its safety and effectiveness against resistant pathogens with efflux pump. On the other hand, macrolide antibiotics, including ketolides, are influenced by efflux pumps of resistant S. pneumoniae and S. pyogenes with mef gene. In addition, CLDM has no gastrointestinal side effect based on the mode of action of a motilin receptor known in EM.14 As a rare case, furthermore, CLDM has been reported to be effective for invasive group A streptococcal infections caused by S. pyogenes.15 A simple chemical structure of CLDM compared with that of macrolide is a positive characteristic, too. On the basis of these reasons, we initiated chemical modifications of lincosamide in order to generate a novel antibacterial agent that is effective against resistant S. pneumoniae and S. pyogenes with erm and mef genes.
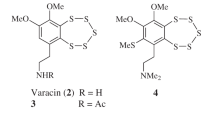
The crystal structures of bacterial 23S ribosomal RNA complexed with CLDM showed that the sugar moiety of CLDM had several hydrogen bonding and played a pivotal role in its binding mode.16 On the other hand, a hydrophobic space was observed around the C-7 position of CLDM in X-ray crystallographic analysis. It is known that modifications at the C-7 position of LCM tend to give comparable antibacterial activity to that of LCM.17, 18 We reported chemical modifications of LCM and clarified that (7S)-7-arylthio-7-deoxylincomycin derivatives19, 20, 21, 22 and (7S)-7-(azetidin-3-yl-thio)-7-deoxylincomycin derivatives23 exhibited moderate to strong antibacterial activities against S. pneumoniae and S. pyogenes with erm gene. Compound 1 that has a substituted azetidin-3-yl-thio moiety at the 7-position exhibited moderate antibacterial activities against S. pneumoniae and S. pyogenes with erm gene. Compound 2 that tethered a phenyl thiadiazol-2-yl thio moiety to the 7-position showed antibacterial activities against those resistant pathogens. The ortho nitro group of 2 played a key role for the enhancement of antibacterial activity of S. pneumoniae with erm gene.22 In this article, we report further optimization of the phenyl moiety of 2 in order to achieve potent antibacterial activity against S. pneumoniae and S. pyogenes with erm gene.
Chemistry
Introductions of a substituent at the 4- and 5-positions of the 2-nitrophenyl group using a nucleophilic aromatic substitution (SNAr) reaction of fluoro-benzene and a nucleophile were planned. Mono-fluoro compounds 4a and 4b, and difluoro compound 4c were prepared by our method reported previously, which was the Mitsunobu reaction of 2, 3, 4-tris-O-(trimethylsilyl)lincomycin (3)24 and the corresponding thiols followed by acidic treatment (Scheme 1). A major reason of relatively low yield of these Mitsunobu reactions was explained by generation of an N-connected byproduct in the thiadiazole moiety instead of the desired S-connected derivative. Compound 6 was synthesized by an SNAr reaction of (7S)-7-deoxy-7-mercaptolincomyicn (5)21 and 2-(4,5-dimethoxy-2-nitrophenyl)-5-(methylsulfonyl)-1,3,4-thiadiazole. The derivatization of 4a, 4b and 4c is shown in Scheme 2. Compound 7a that has a 4-dimethylamino group was obtained from 4-fluoro compound 4a. Synthesis of 2-nitro-4-methoxy derivative using sodium methoxide and 4a was unsuccessful probably because of poor reactivity of 4-fluoro atom in 4a. Treatment of 5-fluoro compound 4b with amines, such as dimethylamine and methylamine, gave 7b and 8b in good yields. Compounds 7c, 8c and 9c were obtained from 4,5-difluoro compound 4c in the similar way to 4b. Methoxy derivatives 10b and 10c were prepared by reaction of sodium methoxide with 4b and 4c, respectively.
Results and discussion
Antibacterial activities of 2,4- or 2,5-di-substituted derivatives are shown in Table 2. 4-Fluoro derivative 4a showed somehow enhanced antibacterial activities against S. pneumoniae and S. pyogenes with erm gene compared with 2, and its potency especially against S. pneumoniae with erm and mef gene (strain #6) was clearly enhanced. In contrast, dimethylamino derivative 7a exhibited enhanced antibacterial activities against susceptible strains of S. pneumoniae and S. pyogenes, but the effect of the dimethylamino group on antibacterial activity against resistant strains of S. pneumoniae (#4–8) was unclear. In the case of 5-fluoro derivative 4b, the antibacterial activity decreased against almost all of the test organisms. It should be noted that the antibacterial activities of 5-dimethylamino derivative 7b, 5-methylamino derivative 8b and 5-methoxy derivative 10b were significantly improved against all of the Gram-positive pathogens compared with 2, and showed comparable antibacterial activities against constitutive-resistant S. pneumoniae with erm gene (#4 and 5) to those of TEL. The antibacterial activities of 7b, 8b and 10b against S. pyogenes with erm gene were further improved and 32 times stronger than that of TEL. The antibacterial activity of 10b against H. influenzae was also improved compared with 2 but it is still weaker than that of TEL. On the basis of the results obtained above, we performed further optimization focusing on the 4- and 5-substituents on the benzene ring.
Antibacterial activities of 2,4,5-tri-substituted derivatives are shown in Table 3. As expected, compound 7c that has the 5-dimethylamino group and the 4-fluoro group showed stronger antibacterial activities against S. pneumoniae and S. pyogenes with erm gene as well as S. pneumoniae with erm and mef gene (#6) than 5-dimethylamino derivative 7b did. Similar antibacterial profiles were confirmed not only in methylamine derivative 8c, but also 10c that has a methoxy group at the 5-position of the phenyl group. Furthermore, 4,5-dimethoxy derivative 6 showed an antibacterial profile similar to 10c. It indicates that electronic property of the substituent at the 4-position is not important for antibacterial activity. Antibacterial activities of the 2,4,5-tri-substituted derivatives (7c, 8c, 10c and 6) against S. pneumoniae with erm gene were generally comparable to those of TEL and they were significantly superior to TEL against S. pyogenes with erm gene. As for antibacterial activity against H. influenzae, 10c and 6 exhibited generally stronger activities than 7c, 8c and 9c and their activities have been getting closer to those of TEL.
Conclusions
A series of LCM derivatives that have the 5-(2-nitrophenyl)-1,3,4-thiadiazol-2-yl thio moiety at the 7-position in S-configuration were synthesized. Introductions of a substituent at the 4- and 5-positions of the 2-nitrophenyl group were accomplished by the SNAr reaction of fluoro-benzene 4a, 4b or 4c and a nucleophile. The other method was the SNAr reaction of (7S)-7-deoxy-7-mercaptolincomyicn (5)21 and 5-(methylsulfonyl)-1,3,4-thiadiazole derivative (Scheme 1, condition (c)). From the results of antibacterial activities of 2-nitro-5-substituted phenyl derivatives, the modification led to significant improvement in antibacterial activities against S. pneumoniae and S. pyogenes with erm gene. Moreover, an additional substituent at the 4-position, such as a fluoro atom or a methoxy group, further improved the antibacterial activities of 2-nitro-5-substituted phenyl derivatives against S. pneumoniae and S. pyogenes with erm gene. Antibacterial activities of the 2-nitro-4,5-di-substituted phenyl derivatives (7c, 8c, 10c and 6) against S. pneumoniae with erm gene were generally comparable to those of TEL, and they were significantly superior to TEL against S. pyogenes with erm gene. Compounds 10c and 6 that have a methoxy group at the 5-position of the benzene ring exhibited activities comparable to TEL against H. influenzae. It is noteworthy that a single modification at the 7-position realized comparable activity to that of TEL against target-resistant pathogens. LCM analogs have a promising framework to overcome the resistant S. pneumoniae and S. pyogenes with erm gene.
Experimental procedure
General
1H NMR spectra were measured with Varian Gemini-300 (Varian Inc., Palo Alto, CA, USA) for 300 MHz, JEOL JNM-GSX 400 (JEOL Ltd, Tokyo, Japan) for 400 MHz or BRUKER Ascend 400 NMR spectrometer (BRUKER Corporation, Coventry, UK) for 400 MHz in CDCl3 or CD3OD with 0.03% TMS as an internal standard. 13C NMR spectra were measured with BRUKER Ascend 400 NMR spectrometer (BRUKER Corporation) for 100 MHz. Mass spectra were obtained on a JEOL JMS-FABmate spectrometer or JEOL JMS-700 mass spectrometer or Agilent Technologies 6530-Q-TOF LC/MS mass spectrometer (Agilent Technologies, Santa Clara, CA, USA). The optical rotations were recorded with Jasco P-2300 digital polarimeter (Jasco, Tokyo, Japan). The melting points were measured with Yanaco MP-S (Yanaco, Tokyo, Japan). The infrared spectra were measured with Jasco FT/IR-410 (Jasco). Column chromatography was performed with silica gel 60N (Kanto Chemical, Tokyo, Japan, spherical, neutral).
(7S)-7-Deoxy-7-[5-(4-fluoro-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (4a)
To a solution of 3 (240 mg, 0.39 mmol) in toluene (5 ml) at 0 °C were added triphenylphosphine (150 mg, 0.57 mmol) and diethylazodicarboxylate (0.10 ml, 0.55 mmol) and stirred at 0 °C for 30 min and 5-(4-fluoro-2-nitrophenyl)-1,3,4-thiadiazole-2-thiol (120 mg, 0.47 mmol) was added and stirred at room temperature for 3 h. The mixture was concentrated under reduced pressure. To the resulting mixture were added methanol (5 ml), 1N hydrochloric acid (0.7 ml) and stirred at room temperature for 1 h. The mixture was concentrated under reduced pressure and the resulting residue was dissolved by water and washed with ethyl acetate. To the mixture was added NaHCO3, and the mixture was extracted with ethyl acetate. The organic phase was concentrated under reduced pressure and the resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/1/0.1) to afford 4a (132 mg, 34%) as colorless solid.
[α]D22 +67° (c 0.73, CH3OH); 1H NMR (300 MHz, CDCl3) δ 9.09 (br d, J=9.1 Hz, 1H), 7.69–7.85 (m, 2H), 7.37–7.54 (m, 1H), 5.35 (d, J=5.3 Hz, 1H), 5.21–5.33 (m, 1H), 4.31–4.54 (m, 2H), 4.24 (br d, J=10.2 Hz, 1H), 4.16 (dd, J=9.9, 5.3 Hz, 1H), 3.68–3.83 (m, 1H), 3.58 (dd, J=10.2, 3.3 Hz, 1H), 3.35 (br s, 1H), 3.06–3.22 (m, 1H), 2.41 (s, 3H), 2.18 (s, 3H), 1.83–2.15 (m, 4H), 1.57 (d, J=6.6 Hz, 3H), 1.26–1.42 (m, 4H), 0.81–1.01 (m, 3H); HRMS (ESI) m/z calcd for C26H37FN5O7S3 646.1834, found 646.1841 (M+H)+.
(7S)-7-Deoxy-7-[5-(5-fluoro-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (4b)
Reaction of 3 (690 mg, 1.01 mmol) with 5-(5-fluoro-2-nitrophenyl)-1,3,4-thiadiazole-2-thiol (200 mg, 1.55 mmol) gave 4b as a colorless solid in 19% yield by a similar procedure to 4a. [α]D22 +66° (c 0.18, CH3OH); 1H NMR (300 MHz, CDCl3) δ 9.09 (d, J=9.2 Hz, 1H), 8.12 (dd, J=9.0, 4.9 Hz, 1H), 7.46 (dd, J=8.1, 2.7 Hz, 1H), 7.36–7.43 (m, 1H), 5.36 (d, J=5.6 Hz, 1H), 5.33 (br s, 1H), 4.33–4.48 (m, 2H), 4.23 (d, J=10.0 Hz, 1H), 4.15 (dd, J=10.0, 5.5 Hz, 1H), 3.71 (br s, 1H), 3.52–3.63 (m, 1H), 3.29–3.37 (m, 1H), 3.10 (dd, J=10.5, 4.6 Hz, 1H), 2.40 (s, 3H), 2.19 (s, 3H), 2.05–2.16 (m, 2H), 1.85–2.02 (m, 2H), 1.58 (d, J=7.0 Hz, 4H), 0.85–0.95 (m, 3H); HRMS (ESI) m/z calcd for C26H37FN5O7S3 646.1834, found 646.1840 (M+H)+.
(7S)-7-Deoxy-7-[5-(4,5-difluoro-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (4c)
Reaction of 3 (240 mg, 0.39 mmol) with 5-(4,5-difluoro-2-nitrophenyl)-1,3,4-thiadiazole-2-thiol gave (140 mg, 0.51 mmol) as a colorless solid in 33% yield by a similar procedure to 4a. 1H NMR (300 MHz, CDCl3) δ 9.03 (d, J=8.2 Hz, 1H), 7.95–8.04 (m, 1H), 7.59–7.68 (m, 1H), 5.35 (d, J=5.6 Hz, 1H), 5.29 (br s, 1H), 4.29–4.51 (m, 2H), 4.09–4.27 (m, 2H), 3.67–3.78 (m, 1H), 3.57 (dd, J=10.2, 2.7 Hz, 1H), 3.28–3.38 (m, 1H), 3.10 (dd, J=10.2, 4.6 Hz, 1H), 2.40 (s, 3H), 2.17 (s, 3H), 2.03–2.15 (m, 2H), 1.86–2.02 (m, 2H), 1.57 (d, J=7.1 Hz, 3H), 1.27–1.36 (m, 4H), 0.85–0.96 (m, 3H); HRMS (ESI) m/z calcd for C26H36F2N5O7S3 664.1739, found 664.1735 (M+H)+.
(7S)-7-Deoxy-7-[5-(4,5-dimethoxy-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (6)
To a solution of 521 (74 mg, 0.18 mmol) in N,N-dimethylformamide (0.5 ml) were added 1 M sodium hexamethyldisilazane tetrahydrofuran solution (0.33 ml) and 2-(4,5-dimethoxy-2-nitrophenyl)-5-(methylsulfonyl)-1,3,4-thiadiazole (63 mg, 0.18 mmol) and the mixture was stirred at room temperature for 20 min. The mixture was diluted with ethyl acetate and washed with water. The organic phase was dried over Na2SO4, filtered and concentrated under reduced pressure. The residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=10/1/0.1) to afford 6 (75 mg, 67%) as a colorless solid; MP 222–227 °C (dec.); [α]D23 +65° (c 0.20, CH3OH); IR (KBr) 3364.21, 2922.59, 2866.67, 2866.67, 2787.60, 2360.44, 1654.62, 1614.13, 1547.59, 1508.06 cm-1; 1H NMR (400 MHz, CDCl3) δ 8.94 (br d, J=9.0 Hz, 1H), 7.66 (s, 1H), 7.14 (s, 1H), 5.36 (d, J=5.6 Hz, 1H), 5.27 (br s, 1H), 4.36–4.46 (m, 2H), 4.25 (d, J=10.0 Hz, 1H), 4.15 (dd, J=10.2, 5.6 Hz, 1H), 4.02 (s, 3H), 4.00 (s, 3H), 3.58 (dd, J=10.0, 3.7 Hz, 1H), 3.33 (dd, J=7.7, 5.2 Hz, 1H), 3.09 (dd, J=10.7, 4.4 Hz, 1H), 2.39 (s, 3H), 2.17 (s, 3H), 2.04–2.16 (m, 2H), 1.85–2.01 (m, 2H), 1.57 (d, J=6.8 Hz, 3H), 1.26–1.40 (m, 4H), 0.85–0.94 (m, 3H); 13C NMR (100 MHz, CDCl3) δ 178.94, 164.79, 164.40, 152.80, 150.67, 141.11, 118.40, 113.44, 108.11, 89.01, 71.70, 71.10, 69.37, 68.47, 68.19, 62.60, 56.73, 56.70, 53.15, 44.81, 41.81, 38.13, 38.04, 35.72, 21.59, 18.81, 14.75, 14.29; HRMS (ESI) m/z calcd for C28H42N5O9S3 688.2139, found 688.2150 (M+H)+.
(7S)-7-Deoxy-7-[5-(4-dimethylamino-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (7a)
A solution of 4a (70 mg, 0.11 mmol) in 2M dimethylamine methanol solution (1.0 ml) was stirred at 80 °C for 16 h in a sealed tube. The mixture was concentrated under reduced pressure and the resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/2/0.2) to afford 7a (59 mg, 81%) as a colorless solid. [α]D22 +69° (c 1.0, CH3OH); 1H NMR (400 MHz, CDCl3) δ 9.20 (d, J=9.0 Hz, 1H), 7.55 (d, J=8.7 Hz, 1H), 7.09 (d, J=2.7 Hz, 1H), 6.86 (dd, J=8.8, 2.7 Hz, 1H), 5.39 (br s, 1H), 5.35 (d, J=5.5 Hz, 1H), 4.37–4.45 (m, 1H), 4.23–4.31 (m, 2H), 4.14 (dd, J=10.1, 5.5 Hz, 1H), 3.71 (d, J=3.4 Hz, 1H), 3.57 (dd, J=10.0, 3.4 Hz, 1H), 3.37 (dd, J=8.2, 5.6 Hz, 1H), 3.11 (s, 6H), 3.06–3.11 (m, 1H), 2.38 (s, 3H), 2.19 (s, 3H), 2.04–2.18 (m, 2H), 1.85–2.00 (m, 2H), 1.54 (d, J=7.1 Hz, 3H), 1.29–1.37 (m, 4H), 0.85–0.95 (m, 3H); HRMS (ESI) m/z calcd for C28H43N6O7S3 671.2350, found 671.2346 (M+H)+.
(7S)-7-Deoxy-7-[5-(5-dimethylamino-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (7b)
A solution of 4b (27 mg, 0.042 mmol) in 2M dimethylamine methanol solution (1.0 ml) was stirred at room temperature for 1 h. The mixture was concentrated under reduced pressure and the resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/2/0.2) to afford 7b (24 mg, 87%) as a colorless solid. [α]D22 +73° (c 0.70, CH3OH); 1H NMR (300 MHz, CDCl3) δ 8.94 (d, J=8.5, 1H), 8.18 (d, J=9.1 Hz, 1H), 6.69–6.79 (m, 2H), 5.36 (d, J=5.4 Hz, 1H), 5.19–5.34 (m, 1H), 4.34–4.48 (m, 2H), 4.27 (br d, J=10.2 Hz, 1H), 4.15 (dd, J=9.9, 5.4 Hz, 1H), 3.72 (br d, J=3.4 Hz, 1H), 3.59 (dd, J=10.2, 3.4 Hz, 1H), 3.30–3.39 (m, 1H), 3.16 (s, 6H), 3.05–3.13 (m, 1H), 2.40 (s, 3H), 2.18 (s, 3H), 1.86–2.15 (m, 4H), 1.57 (d, J=6.9 Hz, 3H), 1.21–1.42 (m, 4H), 0.85–0.95 (m, 3H); HRMS (ESI) m/z calcd for C28H43N6O7S3 671.2350, found 671.2346 (M+H)+.
(7S)-7-Deoxy-7-[5-(5-dimethylamino-4-fluoro-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (7c)
A solution of 4c (10 mg, 0.015 mmol) in 2M dimethylamine methanol solution (1.0 ml) was stirred at 50 °C for 3.5 h in a sealed tube. The mixture was concentrated under reduced pressure and the resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/2/0.2) to afford 7c (9.0 mg, 87%) as a colorless solid. [α]D23 +91° (c 0.35, CH3OH); 1H NMR (400 MHz, CDCl3) δ 8.94 (br d, J=9.0 Hz, 1H), 7.94 (d, J=14.1 Hz, 1H), 6.86 (d, J=8.8 Hz, 1H), 5.36 (d, J=5.6 Hz, 1H), 5.28 (br d, 1H), 4.36–4.47 (m, 2H), 4.26 (d, J=10.0 Hz, 1H), 4.18–4.23 (m, 1H), 4.15 (dd, J=10.0, 5.6 Hz, 1H), 3.68–3.75 (m, 1H), 3.58 (dd, J=10.1, 3.5 Hz, 1H), 3.33 (dd, J=7.9, 5.5 Hz, 1H), 3.16–3.19 (m, 1H), 3.15 (s, 3H), 3.15 (s, 3H), 3.07–3.13 (m, 1H), 2.40 (s, 3H), 2.03–2.16 (m, 3H), 1.85–2.02 (m, 3H), 1.57 (d, J=7.1 Hz, 3H), 1.26–1.35 (m, 4H), 0.85–0.94 (m, 3H); HRMS (ESI) m/z calcd for C28H42FN6O7S3 689.2256, found 689.2258 (M+H)+.
(7S)-7-Deoxy-7-[5-(5-methylamino-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (8b)
Reaction of 4b (30 mg, 0.046 mmol) with 40% methylamine methanol solution (1.0 ml) gave 8b (23 mg, 75%) as a colorless solid by a similar procedure to 7b. [α]D22 +73° (c 0.69, CH3OH); 1H NMR (300 MHz, CDCl3) δ 8.89 (br d, J=8.5 Hz, 1H), 8.10–8.18 (m, 1H), 6.63–6.72 (m, 2H), 5.36 (d, J=5.2 Hz, 1H), 5.17–5.34 (m, 1H), 4.92–5.04 (m, 1H), 4.34–4.48 (m, 2H), 4.27 (d, J=9.9 Hz, 1H), 4.15 (dd, J=10.1, 5.2 Hz, 1H), 3.71–3.78 (m, 1H), 3.60 (dd, J=9.9, 3.3 Hz, 1H), 3.29–3.38 (m, 1H), 3.11 (dd, J=10.2, 4.7 Hz, 1H), 2.95 (d, J=4.9 Hz, 3H), 2.40 (s, 3H), 2.16 (s, 3H), 1.81–2.14 (m, 4H), 1.56 (d, J=6.6 Hz, 3H), 1.24–1.38 (m, 4H), 0.85–0.96 (m, 3H); HRMS (FAB) m/z calcd for C27H41N6O7S3 657.2193, found 657.2192 (M+H)+.
(7S)-7-Deoxy-7-[5-(4-fluoro-5-methylamino-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (8c)
Reaction of 4c (7.0 mg, 0.011 mmol) with 40% methylamine methanol solution (1.0 ml) gave 8c (7.0 mg, 98%) as a colorless solid by a similar procedure to 7b. MP 220–225 °C (dec.); [α]D22 +64° (c 0.47, CH3OH); IR (KBr) 3397.96, 2922.59, 2782.78, 2369.12, 1654.62, 1577.49 and 1527.35 cm−1; 1H NMR (400 MHz, CD3OD) δ 7.98 (d, J=11.9 Hz, 1H), 6.78 (d, J=8.1 Hz, 1H), 5.28 (d, J=5.6 Hz, 1H), 4.61 (dd, J=9.8, 3.0 Hz, 1H), 4.41–4.49 (m, 2H), 4.11 (dd, J=10.4, 5.6 Hz, 1H), 3.82 (d, J=3.1 Hz, 1H), 3.55–3.63 (m, 2H), 3.00–3.05 (m, 1H), 2.92 (s, 3H), 2.40 (s, 3H), 2.04–2.10 (m, 1H), 2.03 (s, 3H), 1.82–1.89 (m, 1H), 1.58 (d, J=7.1 Hz, 3H), 1.28–1.36 (m, 4H), 0.88–0.94 (m, 3H); 13C NMR (100 MHz, CDCl3) δ 178.93, 165.07, 164.77, 151.06, 148.59, 142.50, 142.38, 135.50, 135.42, 123.96, 123.93, 112.79, 112.72, 112.67, 112.56, 88.99, 71.67, 71.11, 69.38, 68.47, 68.20, 62.61, 53.19, 44.76, 41.82, 38.11, 38.04, 35.72, 29.74, 21.59, 18.86, 14.72, 14.29; HRMS (ESI) m/z calcd for C27H40FN6O7S3 675.2099, found 675.2103 (M+H)+.
(7S)-7-Deoxy-7-{5-[4-fluoro-5-(2-hydroxyethylamino)-2-nitrophenyl]-1,3,4-thiadiazol-2-ylthio}lincomycin (9c)
A solution of 4c (12 mg, 0.018 mmol) in 2-ethanolamine (0.5 ml) was stirred at 50 °C for 2 h. The mixture was diluted with ethyl acetate and washed with water. The organic phase was dried over Na2SO4, filtered and concentrated under reduced pressure. The resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/2/0.2) to afford 9c (11 mg, 86%) as a colorless solid. [α]D23 +63° (c 0.42, CH3OH); 1H NMR (400 MHz, CD3OD) δ 8.00 (d, J=11.9 Hz, 1H), 6.93 (d, J=8.3 Hz, 1H), 5.28 (d, J=5.6 Hz, 1H), 4.62 (dd, J=9.9, 3.0 Hz, 1H), 4.41–4.49 (m, 2H), 4.12 (dd, J=10.3, 5.6 Hz, 1H), 3.80–3.84 (m, 1H), 3.73 (t, J=5.6 Hz, 2H), 3.58 (dd, J=10.3, 3.2 Hz, 1H), 3.42 (t, J=5.6 Hz, 2H), 3.25–3.29 (m, 1H), 3.03 (dd, J=10.5, 5.1 Hz, 1H), 2.40 (s, 3H), 2.16–2.27 (m, 1H), 2.04–2.10 (m, 1H), 2.04 (s, 3H), 1.99–2.03 (m, 1H), 1.81–1.91 (m, 1H), 1.58 (d, J=7.1 Hz, 3H), 1.29–1.38 (m, 4H), 0.89–0.95 (m, 3H); HRMS (ESI) m/z calcd for C28H42FN6O8S3 705.2205, found 705.2209 (M+H)+.
(7S)-7-Deoxy-7-[5-(5-methoxy-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (10b)
A solution of 4b (17 mg, 0.026 mmol) in methanol (0.50 ml) was added 28% methanol solution of sodium methoxide (0.10 ml) stirred at room temperature for 1 h. The mixture was diluted with ethyl acetate and washed with water. The organic phase was dried over Na2SO4, filtered and concentrated under reduced pressure. The resulting residue was purified by preparative TLC (CHCl3/CH3OH/28% aq NH4OH=20/2/0.2) to afford 10b (11 mg, 64%) as a colorless solid. [α]D23 +56° (c 0.36, CH3OH); 1H NMR (300 MHz, CDCl3) δ 8.91–9.14 (m, 1H), 8.16 (d, J=8.4 Hz, 1H), 7.05–7.20 (m, 2H), 5.36 (d, J=5.4 Hz, 1H), 5.09–5.34 (m, 1H), 4.56–4.73 (m, 1H), 4.34–4.50 (m, 1H), 4.08–4.29 (m, 1H), 3.94 (s, 3H), 3.58–3.83 (m, 2H), 2.69–3.00 (m, 2H), 2.46–2.64 (m, 1H), 1.99–2.40 (m, 7H), 1.87–1.95 (m, 1H), 1.51–1.65 (m, 3H), 1.17–1.48 (m, 3H), 0.82–0.99 (m, 1H); HRMS (ESI) m/z calcd for C27H40N5O8S3 658.2034, found 658.2040 (M+H)+.
(7S)-7-Deoxy-7-[5-(4-fluoro-5-methoxy-2-nitrophenyl)-1,3,4-thiadiazol-2-ylthio]lincomycin (10c)
Reaction of 4c (14 mg, 0.021 mmol) gave 10c (10 mg, 70%) as a colorless solid by a similar procedure to 10b. [α]D23 +84° (c 0.30, CH3OH); 1H NMR (400 MHz, CDCl3) δ 8.94 (br d, J=8.8 Hz, 1H), 7.96 (d, J=10.2 Hz, 1H), 7.26 (d, J=7.8 Hz, 1H), 5.36 (d, J=5.6 Hz, 1H), 5.23–5.31 (m, 1H), 4.38–4.48 (m, 2H), 4.24 (d, J=10.0 Hz, 1H), 4.14–4.17 (m, 1H), 4.03 (s, 3H), 3.71 (d, J=3.2 Hz, 1H), 3.58 (dd, J=10.0, 3.4 Hz, 1H), 3.30–3.34 (m, 1H), 3.09 (dd, J=10.5, 4.4 Hz, 1H), 2.40 (s, 3H), 2.17 (s, 3H), 2.06–2.15 (m, 2H), 1.85–2.01 (m, 3H), 1.58 (d, J=6.8 Hz, 3H), 1.28–1.37 (m, 4H), 0.87–0.93 (m, 3H); HRMS (ESI) m/z calcd for C27H39N5O8S3 676.1939, found 676.1947 (M+H)+.
In vitro antibacterial activity
Minimum inhibitory concentration (MIC) was determined by the agar dilution method. Test strains were subjected to seed culture using sensitivity test broth (STB, Nissui Pharmaceutical, Tokyo, Japan) cultured on blood agar plate for S. pneumoniae, S. pyogenes and H. influenzae. A 5 μl portion of cell suspension of the test strains having about 106 CFU per ml was inoculated into sensitivity disk agar (SDA, Nissui Pharmaceutical) supplemented with 5% horse blood and incubated at 37 °C for 20 h. Then, MIC was defined as the lowest drug concentration that prevented visible growth.

Synthesis of (7S)-7-(5-phenyl-1,3,4-thiadiazol-2-yl-thio)-7-deoxylincomycin derivatives. Reagents: (a) ArSH, DEAD, PPh3, toluene, 0 °C, 30 min, then rt, 3 h; (b) 1 N HCl, MeOH, rt, 30 min, two steps 34% from 3 to 4a, two steps 19% from 3 to 4b, two steps 33% from 3 to 4c; (c) 2-(4,5-dimethoxy-2-nitrophenyl)-5-(methylsulfonyl)-1,3,4-thiadiazole, NaHMDS, DMF, rt, 20 min, 67%.

Synthesis of (7S)-7-(5-phenyl-1,3,4-thiadiazol-2-yl-thio)-7-deoxylincomycin derivatives. Reagents: (a) 2M dimethylamine in methanol, 80 °C, 16 h, 81%; (b) 2M dimethylamine in methanol, rt, 1 h, 87%; (c) 2M dimethylamine in methanol, 50 °C, 3.5 h, 87%; (d) 40% methylamine in methanol, rt, 1 h, 75% from 4b to 8b, 98% from 4c to 8c; (e) 2-aminoethanol, 50 °C, 2 h, 86%; (f) 28% sodium methoxide methanol solution, rt, 64% from 4b to 10b, 70% from 4c to 10c.
References
Morimoto, S., Takahashi, Y., Watanabe, Y. & Omura, S. Chemical modification of erythromycins. I. Synthesis and antibacterial activity of 6-O-methylerythromycins A. J. Antibiot. 37, 187–189 (1984).
Slobodan, D. et al. Erythromycin series. Part 13. Synthesis and structure elucidation of 10-dihydro-10-deoxo-11-methyl-11-azaerythromycin A. J. Chem. Res. Synop. 1988, 152–153 (1988).
Ajito, K., Miura, T., Furuuchi, T. & Tamura, A. Sixteen-membered macrolides: chemical modifications and future applications. Heterocycles 89, 281–352 (2014).
Sato, T. et al. In vitro antibacterial activity of modithromycin, a novel 6,11-bridged bicyclolide, against respiratory pathogens, including macrolide-resistant Gram-positive cocci. Antimicrob. Agents Chemother. 55, 1588–1593 (2011).
Denis, A. et al. Synthesis and antibacterial activity of HMR 3647 a new ketolide highly potent against erythromycin-resistant and susceptible pathogens. Bioorg. Med. Chem. Lett. 9, 3075–3080 (1999).
Brueggemann, A. B. et al. In vitro activity of ABT-773, a new ketolide, against recent clinical isolates of Streptococcus pneumoniae Haemophilus influenzae, and Moraxella catarrhalis. Antimicrob. Agents Chemother. 44, 447–449 (2000).
McGhee, P. et al. In vitro activity of CEM-101 against Streptococcus pneumoniae and Streptococcus pyogenes with defined macrolide resistance mechanisms. Antimicrob. Agents Chemother. 54, 230–238 (2010).
Farrell, J. D. et al. In vitro activity of WCK 4873 (Nafithromycin) against resistant subsets of Streptococcus pneumoniae from a global surveillance program (2014). ASM Microbe 2016, Poster Saturday-455 (Boston, USA, (2016).
Clay, K. D. et al. Severe hepatotoxicity of telithromycin: three case reports and literature review. Ann. Intern. Med. 144, 415–420 (2006).
Miura, T. et al. Novel azalides derived from 16-membered macrolides. III. Azalides modified at the C-15 and 4” positions: Improved antibacterial activities. Bioorg. Med. Chem. 18, 2735–2747 (2010).
Mason, D. J., Dietz, A. & Deboer, C. Lincomycin, a new antibiotic I. Discovery and biological properties. Antimicrob. Agents Chemother. 554–559 (1962).
Birkenmeyer, R. D. & Kagan, F. Lincomycin. XI. Synthesis and structure of clindamycin. A potent antibacterial agent. J. Med. Chem. 13, 616–619 (1970).
Weisblum, B. Erythromycin resistance by ribosome modification. Antimicrob. Agents Chemother. 39, 577–585 (1995).
Tsuzuki, K. et al. Motilides, macrolides with gastrointestinal motor stimulating activity. I. O-substituted and tertiary N-substituted derivatives of 8,9-anhydroerythromycin A 6,9-hemiacetal. Chem. Pharm. Bull. 37, 2687–2700 (1989).
Shah, P. J., Vakil, N. & Kabakov, A. Role of intravenous immune globulin in streptococcal toxic shock syndrome and Clostridium difficile infection. Am. J. Health Syst. Pharm. 72, 1013–1019 (2015).
Schlünzen, F. et al. Structural basis for the interaction of antibiotics with the peptidyl transferase centre in eubacteria. Nature 413, 814–821 (2001).
Sztaricskai, F. et al. Semisynthetic modification of antibiotic lincomycin. J. Antibiot. 49, 941–943 (1996).
Goffic, L. F. Structure activity relationships in lincosamide and streptogramin antibiotics. J. Antimicrob. Chemother. 16 (Suppl A), 13–21 (1985).
Umemura, E. et al. Synthesis of novel lincomycin derivatives and their in vitro antibacterial activities. J. Antibiot. 66, 195–198 (2013).
Wakiyama, Y. et al. Synthesis and structure–activity relationships of novel lincomycin derivatives. Part 1. Newly generated antibacterial activities against Gram-positive bacteria with erm gene by C-7 modification. J. Antibiot. 69, 368–380 (2016).
Wakiyama, Y. et al. Synthesis and structure-activity relationships of novel lincomycin derivatives. Part 2. Synthesis of 7(S-7-deoxy-7-(4-morpholinocarbonylphenylthio)lincomycin and its 3-dimensional analysis with rRNA. J. Antibiot. 69, 428–439 (2016).
Kumura, K. et al. Synthesis and antibacterial Activity of novel lincomycin derivatives. II. Synthesis and antibacterial activity of novel lincomycin derivatives. II. Exploring (7 S -7-(5-aryl-1,3,4-thiadiazol-2-yl-thio)-7-deoxylincomycin derivatives. J. Antibiot. 70, 655–663 (2017).
Kumura, K. et al. Synthesis and antibacterial activity of novel lincomycin derivatives. I. Enhancement of antibacterial activities by introduction of substituted azetidines. J. Antibiot. 69, 440–445 (2016).
Houtman, R. L. & Mich, P. (The Upjohn Company), Trimethylsilyl ethers of lincomycin and its compounds. US3418414 (1966).
Acknowledgements
We thank Dr E Shitara, Mr A Tamura, Dr T Okutomi for valuable scientific discussion. We are grateful to Professor Emeritus Dr M Konno for supervision through our in-house drug discovery program in LCM field. We are also grateful to Ms T Miyara, Ms S Miki, Ms K Kaneda, Dr T Murata and Mr S Sato for contribution toward analytical chemistry, Ms K Yamada for biological studies, and Ms M Takagi for manuscript. We also thank Ms M Ishii for direction in intellectual properties.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kumura, K., Wakiyama, Y., Ueda, K. et al. Synthesis and antibacterial activity of novel lincomycin derivatives. III. Optimization of a phenyl thiadiazole moiety. J Antibiot 71, 104–112 (2018). https://doi.org/10.1038/ja.2017.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2017.59
This article is cited by
-
Synthesis and SARs of novel lincomycin derivatives Part 5: optimization of lincomycin analogs exhibiting potent antibacterial activities by chemical modification at the 6- and 7-positions
The Journal of Antibiotics (2018)
-
Synthesis of new chiral 1,3,4-thiadiazole-based di- and tri-arylsulfonamide residues and evaluation of in vitro anti-HIV activity and cytotoxicity
Molecular Diversity (2018)