Abstract
Mesenchymal stem cells (MSCs) have been identified and isolated from dental tissues, including stem cells from apical papilla, which demonstrated the ability to differentiate into dentin-forming odontoblasts. The histone demethylase KDM6B (also known as JMJD3) was shown to play a key role in promoting osteogenic commitment by removing epigenetic marks H3K27me3 from the promoters of osteogenic genes. Whether KDM6B is involved in odontogenic differentiation of dental MSCs, however, is not known. Here, we explored the role of KDM6B in dental MSC fate determination into the odontogenic lineage. Using shRNA-expressing lentivirus, we performed KDM6B knockdown in dental MSCs and observed that KDM6B depletion leads to a significant reduction in alkaline phosphate (ALP) activity and in formation of mineralized nodules assessed by Alizarin Red staining. Additionally, mRNA expression of odontogenic marker gene SP7 (osterix, OSX), as well as extracellular matrix genes BGLAP (osteoclacin, OCN) and SPP1 (osteopontin, OPN), was suppressed by KDM6B depletion. When KDM6B was overexpressed in KDM6B-knockdown MSCs, odontogenic differentiation was restored, further confirming the facilitating role of KDM6B in odontogenic commitment. Mechanistically, KDM6B was recruited to bone morphogenic protein 2 (BMP2) promoters and the subsequent removal of silencing H3K27me3 marks led to the activation of this odontogenic master transcription gene. Taken together, our results demonstrated the critical role of a histone demethylase in the epigenetic regulation of odontogenic differentiation of dental MSCs. KDM6B may present as a potential therapeutic target in the regeneration of tooth structures and the repair of craniofacial defects.
Similar content being viewed by others
Introduction
Human mesenchymal stem cells (MSCs) are multipotent progenitor cells with the capability to self-renew and differentiate into a variety of cell types including osteoblasts and adipocytes.1 Additional characteristics of MSCs, including their ease of isolation and lack of immunogenicity, make them unique and indispensable tools in tissue engineering and regenerative therapy.2,3,4 MSCs were originally discovered in the stroma of adult bone marrow. Soon after their multipotency became apparent, a search for other MSC subpopulations in different tissue organs uncovered stem cells in synovium, fat, muscle and umbilical cord.5 Similarly, a number of different MSCs have been identified and isolated from the dental tissues, including dental pulpal stem cells, stem cells from human exfoliated deciduous teeth, periodontal ligament stem cells and stem cells from apical papilla.6 Moreover, the pluripotency of these dental MSCs for odontogenic, osteogenic, chondrogenic and adipogenic potentials under different culture conditions in vitro has been demonstrated, suggesting that these dental MSCs hold significant promise for clinical applications in regenerative dental and craniofacial therapies.7
Cell fate determination requires intricate orchestration between genetic and epigenetic programs. In particular, epigenetic regulation has only recently emerged as an important mechanism of stem cell differentiation, and it does so by shaping the fate of MSCs through modifications in chromatin architecture and the accessibility of genes without changing the primary nucleotide sequence.8,9,10 In particular, modifications at the N-terminal tails of histones such as acetylation, methylation, phosphorylation, ubiquitination and ADP-ribosylation establish epigenetic signatures that either mark for gene activation such as trimethylated histone 3 lysine 4 (H3K4) or mark for gene repression, such as demethylated H3K9 and trimethylated H3K27 (H3K27me3). Epigenetic phenomena are largely responsible for the elaborate balance of gene activation and inhibition at specific time points directing towards terminally differentiated phenotypes such as osteoblasts or odontoblasts. Nonetheless, the epigenetic component in the context of odontogenic differentiation has not been identified previously, and very limited information is available for the epigenetic regulation of odontogenic differentiation.
Among different epigenetic machineries, histone demethylases, enzymes responsible for removing methyl groups from the histones, have been demonstrated to influence cell fate decisions and subsequently, cell differentiation.10,11,12 The existence of these demethylases is essential to facilitate rapid removal of methyl group from gene silencing epigenetic marks. The precise functions of histone demethylases in regulating osteogenic differentiation have only begun to be unraveled recently.13
We previously identified a specific histone demethylase, KDM6B (JMJD3) as a critical epigenetic regulator in bone marrow stem cell (BMSC) fate commitment by promoting osteogenic commitment while inhibiting adipogenic differentiation in vitro and in vivo.14 KDM6B is a histone demethylase, which activates gene activation through the removal of H3K27me3, a repressive epigenetic mark.15 Previous studies using BMSCs demonstrated that KDM6B plays an important role in neuronal differentiation by regulating neurogenic lineage genes such as NES, and through its interaction with Smad3 upon transforming growth factor β (TGFβ) signaling initiation.16,17,18 During the osteogenic differentiation of BMSCs, KDM6B occupies and demethylases histones in the promoters of BMP2, BMP4 and HOXC6-1 through which the expression of RUNX2, the master gene of osteogenesis, is regulated.14 Because of the similarities between BMSCs and dental MSCs in differentiation capacity into mineralized tissues, these previous findings strongly support the notion that epigenetic regulation, histone demethylation in particular, may also play a key role in odontogenic differentiation of dental MSCs. In this paper, we investigated the role of KDM6B in odontogenic differentiation of dental MSCs.
Materials and methods
Cell isolation and culture
Primary dental MSCs used in this study were described previously.6 Cells were grown in a humidified 5% CO2 incubator at 37 °C in alpha modified Eagle’s medium (Invitrogen, Carlsbad, CA, USA) supplemented with 15% fetal bovine serum (Invitrogen, Carlsbad, CA, USA), Gibco MEM non-essential amino acids (Invitrogen, Carlsbad, CA, USA), 2 mmol⋅L−1 L-glutamate, 100 units⋅mL−1 penicillin and 100 units⋅mL−1 streptomycin each.
Viral infection
Viral packaging was prepared as described previously.6,19 For viral infection, MSCs were plated overnight and then infected with retroviruses or lentiviruses in the presence of polybrene (6 µg⋅mL−1; Sigma-Aldrich, St Louis, MO, USA) for 24 h. The cells were then selected with puromycin for 3 days. Resistant clones were pooled and knockdown/overexpression was confirmed via reverse transcription-polymerase chain reaction (RT-PCR) analysis. In rescue experiments, the knockdown MSCs were transduced with retroviral constructs containing the Flag- or HA-tagged gene of interest. The target sequences for shRNA were: KDM6Bsh2, 5′-GCA GTC GGA AAC CGT TCT T-3′; KDM6Bsh3, 5′-GTG GGA ACT GAA ATG GTA T-3′. Flag-KDM6B full-length cDNA was cloned into retroviral construct by PCR.
Alkaline phosphate and Alizarin Red staining
MSCs were grown in mineralization-inducing media containing 100 µmol⋅L−1 ascorbic acid, 2 mmol⋅L−1 β-glycerophosphate and 10 nmol⋅L−1 dexamethasone. For alkaline phosphate (ALP) staining, after induction, cells were fixed with 4% paraformaldehyde and incubated with a solution of 0.25% naphthol AS-BI phosphate and 0.75% Fast Blue BB (Sigma-Aldrich, St Louis, MO, USA) dissolved in 0.1 mol⋅L−1 Tris buffer (pH 9.3). ALP activity assay was performed using an ALP kit according to the manufacturer’s protocol (Sigma-Aldrich, St Louis, MO, USA) and normalized based on protein concentrations. To detect mineralization potential, cells were induced for 2–3 weeks, fixed with 4% paraformaldehyde and stained with 2% Alizarin Red (Sigma-Aldrich, St Louis, MO, USA). To quantify the calcium mineral deposition, Alizarin Red was destained with 10% cetylpyridinium chloride in 10 mmol⋅L−1 sodium phosphate for 30 min at room temperature. The concentration was determined by absorbance measurement at 562 nm on a multiplate reader using a standard calcium curve in the same solution. The final calcium level in each group was normalized with the total protein concentrations prepared from a duplicate plate.
Real-time RT-PCR
Total RNA was isolated from MSCs using Trizol reagents (Invitrogen, Carlsbad, CA, USA). Two microgram aliquots of RNAs were synthesized using random hexamers and reverse transcriptase according to the manufacturer’s protocol (Invitrogen, Carlsbad, CA, USA). The real-time PCR reactions were performed using the QuantiTect SYBR Green PCR kit (Qiagen, Valenica, CA, USA) and the Icycler iQ Multi-color Real-time PCR Detection System. The primers for 18S rRNA were: forward, 5′-CGG CTA CCA CAT CCA AGG AA-3′; reverse, 5′-GCT GGA ATT ACC GCG GCT-3′. The primers for OSX were: forward, 5′-CGC TTT GTG CCT TTG AAA T-3′; reverse, 5′- CCG TCA ACG ACG TTA TGC-3′. The primers for OCN were: forward, 5′-CAG ACA CCA TGA GGA CCA TC-3′; reverse, 5′-GGA CTG AGG CTC TGT GAG T-3′. The primers for OPN were: forward, 5′-ATG ATG GCC GAG GTG ATA GT-3′; reverse, 5'-ACC ATT CAA CTC CTC GCT TT-3′. The primers for ALP were: forward, 5′-GAC CTC CTC GGA AGA CAC TC-3′; reverse: 5′-TGA AGG GCT TCT TGT CTG TG-3′. The primers for BMP2 were: forward, 5′-GTC AAC TCG ATG CTG TAC CTT GAC G-3′; reverse, 5′-CAA CCC TCC ACA ACC ATG TCC-3′. The primers for BMP4 were: forward, 5′-CGG CGA AGA AGA ATA AGA ACT GCC G-3′; reverse, 5′- CCA GTC ATT CCA GCC CAC ATC-3′. The primers for DLX2 were: forward, 5′-ACT CAA TAC TTG GCC TTG CC-3′; reverse, 5′-TTG ACC TGA GTC TGG GTG AG-3′. The primers for KDM6B were: forward, 5′-GCA CTA CTG GGA GAC CAT CA-3′; reverse, 5′-ACC AGG AAC CCG TCA AGT AG-3′.
Chromatin immunoprecipitation assays
The assay was performed using a chromatin immunoprecipitation (ChIP) assay kit (Upstate/Milliopore, Billerica, MA, USA) according to the manufacturer’s protocol as described previously.6 Cells were incubated with a dimethyl 3,3′-dithiobispropionimidate-HCl (Pierce/Thermo Scientific, Rockford, IL, USA) solution (5 mmol) for 10 min at room temperature, and then by formaldehyde treated for 15 min in 37 °C water bath. For each ChIP reaction, 2×106 cells were used. All resulting precipitated DNA samples were quantified with real-time PCR. Data are expressed as the percentage of input DNA. Antibodies for ChIP assays were purchased from the following commercial sources: rabbit polyclonal anti-KDM6B (Abgent, San Diego, CA, USA), rabbit monoclonal anti-H3K27me3 (Millipore, Billerica, MA, USA). The primers for BMP2 were: forward, 5′-CGT CTA GTA TTT TGG CAT AGC ATA GAC G-3′; reverse, 5′- ACT CAA TTT CCA GCC TGC TGT TT-3′. The primers for BMP2-4 kb-down were: forward, 5′-CAA TCA TAA GAA TTA CCT GTT GGG-3′; reverse, 5′- TGG TCG CAT TAT ACT CAT ATT GG-3′.
Results
KDM6B promotes odontogenic potential of dental MSCs
Our previous study showed that osteogenic differentiation of BMSCs is epigenetically regulated by the histone demethylase, KDM6B.14 Because certain dental MSCs are capable of differentiating into the odontoblast lineage through similar mechanisms as BMSCs,20 we explored whether KDM6B plays a role in the fate determination of dental MSCs. To do so, we knocked down KDM6B in dental MSCs by transducing lentiviruses expressing KDM6B shRNAs. The knockdown of KDM6B by two different shRNAs was confirmed using real-time RT-PCR (Figure 1a). When these cells were induced to undergo odontogenic differentiation, MSC/KDM6Bsh2 and MSC/KDM6Bsh3 cells lost their capacity to differentiate as demonstrated by ALP staining and activity on the eighth day (Figure 1b). Furthermore, KDM6B knockdown suppressed the formation of mineralized nodules after prolonged treatment with odontogenic media for 3 weeks as demonstrated by Alizarin Red staining (Figure 1c). Of note, there was a dose-dependent reduction of odontogenic differentiation potential that reflected the efficiency of KDM6B knockdown in MSCs. Using MSC/KDM6Bsh3 cells, which exhibited more significant suppression of KDM6B, we further confirmed that KDM6B deficiency inhibited odontogenic potential by examining mRNA expression of several odontogenic marker genes at different time points after induction. In particular, KDM6B depletion significantly suppressed the expression of marker genes for early (OSX, Figure 1d), middle (ALP, Figure 1e) and late (OCN and OPN, Figure 1f and 1g) stages of odontogenic differentiation, indicating that KDM6B is required for the odontogenic differentiation of MSCs.
KDM6B promotes odontogenic potential of dental MSCs. (a) Knockdown of KDM6B by shRNA. MSC/Scrsh, MSCs expressing scramble shRNA; MSC/KDM6Bsh2, MSCs expressing KDM6B shRNA2; MSC/KDM6Bsh3, MSCs expressing KDM6B shRNA3. (b) Knockdown of KDM6B inhibited ALP activities in MSCs. (c) Knockdown of KDM6B inhibited mineralization in MSCs. (d) Knockdown of KDM6B inhibited OSX expression in MSCs as determined by real-time RT-PCR. (e) Knockdown of KDM6B inhibited ALP expression in MSCs. (f) Knockdown of KDM6B inhibited OCN expression in MSCs. (g) Knockdown of KDM6B inhibited OPN expression in MSCs. ALP, alkaline phosphate; MSC, mesenchymal stem cell; RT-PCR, reverse transcription-polymerase chain reaction.
KDM6B activates genes regulating odontogenic differentiation
BMP2 and BMP4 play significant roles in odontogenic differentiation21,22 and DLX family genes are suggested to be involved in dentin matrix mineralization.23 To further explore whether KDM6B mediates odontogenic differentiation through these genes, we induced MSC/Scrsh and MSC/KDM6Bsh3 cells to undergo odontogenic differentiation and assessed mRNA expression of BMP2, BMP4 and DLX2. Although KDM6B was strongly upregulated upon odontogenic differentiation in MSC/Scrsh cells, MSC/KDM6Bsh3 cells exhibited suppressed induction of KDM6B due to the presence of KDM6B shRNA (Figure 2a). Similarly, mRNA levels of BMP2, BMP4 and DLX2 were induced upon odontogenic differentiation in both MSC/Scrsh and MSC/KDM6Bsh3 cells. However, the degree of induction was significantly suppressed in MSC/KDM6Bsh3 cells when compared to MSC/Scrsh cells, indicating that KDM6B activates genes that regulate odontogenic differentiation.
KDM6B activates genes regulating odontogenic differentiation. (a) Knockdown of KDM6B by shRNA suppresses KDM6B expression in MSC differentiation. MSC/Scrsh, MSCs expressing scramble shRNA; MSC/KDM6Bsh3, MSCs expressing KDM6B shRNA. (b) Knockdown of KDM6B inhibited BMP2 expression in MSCs as determined by real-time RT-PCR. (c) Knockdown of KDM6B inhibited BMP4 expression in MSCs. (d) Knockdown of KDM6B inhibited DLX2 expression in MSCs. BMP, bone morphogenic protein; MSC, mesenchymal stem cell; RT-PCR, reverse transcription-polymerase chain reaction.
Rescue of KDM6B restores odontogenic potential of dental MSCs
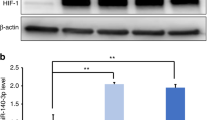
In order to mechanistically delineate whether KDM6B histone demethylase activity is required for odontogenic differentiation of MSCs, we strategically restored KDM6B expression in MSCs that already express KDM6B shRNA. We introduced Flag-tagged KDM6B in MSCs that harbor KDM6B shRNA targeting the 5′ UTR region of KDM6B mRNA. By doing so, shRNA targets only the endogenous KDM6B but not ectopically introduced KDM6B. As expected, the control MSCs (Scrsh/V) exhibited significant amounts of KDM6B, which was suppressed upon introducing KDM6B shRNA (KDM6Bsh/V) (Figure 3a). When Flag-tagged KDM6B was ectopically introduced in these KDM6Bsh cells, KDM6B was re-expressed to the level similar to Scrsh/V (Figure 3a). When KDM6Bsh/Flag-KDM6B cells were induced to undergo odontogenic differentiation, the inhibited odontogenic potential of MSCs due to KDM6B depletion was restored with the retrieval of functional KDM6B in KDM6B knockdown cells was demonstrated by ALP staining (Figure 3b) and Alizarin Red staining (Figure 3c). Similarly, the suppressed expression of BMP2, BMP4 and DLX2 as a result of KDM6B depletion was rescued as well when KDM6B was re-introduced, indicating that KDM6B specifically regulates odontogenic differentiation.
Rescue of KDM6B restores odontogenic potential of dental MSCs. (a) Overexpression of KDM6B in MSCs that express KDM6B shRNA. Scrsh/V, MSCs expressing scramble shRNA and empty vector; KDM6Bsh/V, MSCs expressing KDM6B shRNA and empty vector; KDM6Bsh/Flag-KDM6B, MSCs expressing KDM6B shRNA and Flag-tagged KDM6B. (b) Overexpression of Flag-KDM6B rescued ALP activities in MSC differentiation. (c) Overexpression of Flag-KDM6B rescued mineralization in MSC differentiation. (d) Overexpression of Flag-KDM6B rescued BMP2 expression in MSC differentiation as determined by real-time RT-PCR. (e) Overexpression of Flag-KDM6B rescued BMP4 expression in MSC differentiation. (f) Overexpression of Flag-KDM6B rescued DLX2 expression in MSC differentiation. ALP, alkaline phosphate; BMP, bone morphogenic protein; MSC, mesenchymal stem cell; RT-PCR, reverse transcription-polymerase chain reaction.
KDM6B epigenetically regulates BMP expression in dental MSCs by removing the H3K27me3 mark
KDM6B is a histone demethylase that activates the targeting gene expressions by removing the methyl groups in H3K27me3.24 Previously, it was shown that KDM6B regulates BMP expression in human BMSCs.14 To examine whether KDM6B is directly involved in the epigenetic regulation of genes associated with odontogenic differentiation by demethylating H3K27me3, we performed the ChIP assay to assess the physical occupancy of KDM6B and the changes in the histone methylation status at the BMP2 promoter region. We confirmed the direct binding of KDM6B to the promoter region of BMP2 as shown previously.14 KDM6B knockdown diminished the binding pattern of KDM6B in the BMP2 promoter regions (Figure 4a), and the loss of KDM6B occupancy was mirrored by an increase in the amount of H3K27me3 (Figure 4b). Therefore, our data suggest that the recruitment of KDM6B to BMP promoters and removal of H3K27me3 is an important mechanism by which KDM6B epigenetically regulates expression of odontogenic-mediating genes such as BMP2.
KDM6B epigenetically regulates BMP2 expression. (a) Knockdown of KDM6B reduced KDM6B binding to the promoter of BMP2 in MSCs. The promoter of BMP2 was ChIPed with anti-KDM6B antibody or IgG control. The 9 kb downstream of the transcriptional start site was also ChIPed with anti-KDM6B antibody. (b) Knockdown of KDM6B increased the level of H3K27me3 at the BMP2 promoter. BMP, bone morphogenic protein; ChIP, chromatin immunoprecipitation; MSC, mesenchymal stem cell.
Discussion
One of the most important goals of dental tissue engineering utilizing dental MSCs is to regenerate forms and functions of a tooth. Understanding the underlying mechanisms of odontogenic differentiation potential in these cells is therefore of significant interest in regenerative dental medicine. While dental MSCs resemble BMSCs in their potent ability to differentiate into mineralized tissues in vitro and in vivo, MSCs of different origins exhibit tissue-specific mechanisms of osteogenic differentiation at the transcriptional level.25,26 Developmentally, dental MSCs are derived from neuroectoderm while BMSCs are derived from mesoderm. Indeed, direct comparisons between dental MSCs and BMSCs from the same donor revealed increased mineralization potential, a faster proliferation rate and a higher number of stem/progenitor cells in dental MSCs.27 These disparities in stem cell properties suggest possibly similar but nuanced molecular mechanisms underlying cell fate decision depending on the sources of the cell origins.
KDM6B is a histone demethylase that has been shown to epigenetically regulate osteogenic differentiation of MSCs by removing H3K27me3 and subsequently activating genes associated with osteogenesis.14 However, the role of KDM6B in the epigenetic regulation of dental MSCs has not been studied. Our present study showed that depletion of KDM6B inhibited odontogenic differentiation of dental MSCs and restoration of KDM6B in the knockdown cells abrogated the suppression of odontogenic potential. Mechanistically, upon induction, KDM6B removes H3K27me3 silencing marks at BMP2 promoters, thus activating this odontogenic gene. Our findings confirmed that in dental MSCs, KDM6B is also an important epigenetic link in their differentiation towards odontoblasts.
In both BMSCs and dental MSCs, the osteogenic/odontogenic commitment was mediated by KDM6B activating BMP2 which is primarily known to regulate cartilage and bone formation.28,29 We also discovered distinct molecular mechanisms that reflect tissue specificity of the impact from KDM6B. While Hox family genes were activated by KDM6B in BMSCs, they were not expressed in dental MSCs (data not shown). Previously, we reported that in BMSCs, KDM6B knockdown did not affect DLX genes,14 transcription factors that are well known to play especially important roles in craniofacial development.30,31 Instead, DLX2 expression was significantly altered in dental MSCs, an observation that is consistent with other reports that DLX2 is essential for initial patterning of dentition as well as for biomineralization by regulating expression of ECM proteins including OCN.32,33 DLX2 is necessary in tooth development and odontogenic differentiation such that its inactivation resulted in dental defects and failure of normal dental development.34,35 Recent study showed that odontoblast-specific terminal differentiation genes, dentin sialophosphoprotein and dentin matrix protein are induced by BMP signaling by stimulating the activity of several transcription factors including DLX gene.23 We did not observe as significant induction of DLX5 as in DLX2 and this finding is consistent with greater expression of DLX2 than DLX5 in dental pulp clonal cell lines.36 Therefore, it may be possible that, unlike in BMSCs, DLX2 is the downstream target gene of KDM6B and plays a critical role in odontogenic differentiation of dental MSCs. Other DLX family members such as DLX3 and DLX5 found to be involved in osteogenic commitment of BMSCs were epigenetically regulated by KDM4B to mediate BMP2 signaling, activate RUNX2 and regulate OCN expression.37,38 However, in dental MSCs, neither DLX3 nor DLX5 genes were suppressed by KDM6B depletion (data not shown), thus implicating that finer regulatory mechanisms exist to ensure that varied sets of genes are switched on in different tissue microenvironments.
The histone demethylase KDM6B has also been reported to play critical roles in controlling cell fate of stem cells. Recent reports have linked KDM6B to the key epigenetic factor facilitating differentiation of progenitor cells into epidermal,39 endodermal,40,41 as well as mesodermal lineages.14,17,18 In human embryonic stem cells, KDM6B is temporally associated with activation of WNT3 and DKK1 to drive differentiation from pluripotent cells to mesendoderm, then to definitive endoderm.40 In addition, KDM6B associates with Tbx-3 at the enhancer of EOMES gene to allow chromatin reconfiguration, which further stimulates EOMES expression to drive the stem cells towards definitive endoderm.41 Similarly, during neuronal and epidermal differentiation, KDM6B occupancy at the promoters of lineage-specific transcription factors increases when stem cells exit the poised state, and the accompanying removal of H3K27me3 repressing marks leads to transcriptional activation of related genes. This mechanism holds true for osteogenic/odontogenic differentiation of MSCs as well. Of note, KDM6B could also achieve chromatin reconfiguration independent of its demethylase activity in Th1 differentiation.42 However, in our case, we find the demethylase activity to be essential,14 consistent with KDM6B activity in other lineage programs of stem cell differentiation.
The therapeutic function of MSCs relies on the intricate mechanisms that control the fate and delineation of these multipotent cells.43,44,45,46 MSC commitment to different lineages is controlled by transcriptional and epigenetic regulatory factors; thus, understanding the pathways that MSCs undergo when differentiating into odontoblasts may guide MSCs to make lineage-specific decisions for therapeutic applications. Here, we provide evidence that differentiation of dental MSCs to odontogenic lineages is epigenetically regulated by the histone demethylase, KDM6B. Our finding of this novel epigenetic approach to direct dental MSC fate into odontoblasts can have potentially innovative clinical implications in regenerative dentistry. With a better understanding of factors influencing differentiation potential of dental MSCs, dental MSCs may be the key to the repair of craniofacial defects and therapeutic regeneration of a living and functioning tooth to replace a damaged or decayed one.47
References
Dominici M, Le Blanc K, Mueller I et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy 2006; 8( 4): 315–317.
Kolf CM, Cho E, Tuan RS . Mesenchymal stromal cells. Biology of adult mesenchymal stem cells: regulation of niche, self-renewal and differentiation. Arthritis Res Ther 2007; 9( 1): 204.
Phinney DG, Prockop DJ . Concise review: mesenchymal stem/multipotent stromal cells: the state of transdifferentiation and modes of tissue repair—current views. Stem Cells 2007; 25( 11): 2896–2902.
Undale AH, Westendorf JJ, Yaszemski MJ et al. Mesenchymal stem cells for bone repair and metabolic bone diseases. Mayo Clin Proc 2009; 84( 10): 893–902.
Kuhn NZ, Tuan RS . Regulation of stemness and stem cell niche of mesenchymal stem cells: implications in tumorigenesis and metastasis. J Cell Physiol 2010; 222( 2): 268–277.
Fan Z, Yamaza T, Lee JS et al. BCOR regulates mesenchymal stem cell function by epigenetic mechanisms. Nat Cell Biol 2009; 11( 8): 1002–1009.
Chang J, Sonoyama W, Wang Z et al. Noncanonical Wnt-4 signaling enhances bone regeneration of mesenchymal stem cells in craniofacial defects through activation of p38 MAPK. J Biol Chem 2007; 282( 42): 30938–30948.
Jenuwein T, Allis CD . Translating the histone code. Science 2001; 293( 5532): 1074–1080.
Stein GS, van Wijnen AJ, Imbalzano AN et al. Architectural genetic and epigenetic control of regulatory networks: compartmentalizing machinery for transcription and chromatin remodeling in nuclear microenvironments. Crit Rev Eukaryot Gene Expr 2010; 20( 2): 149–155.
Agger K, Christensen J, Cloos PA et al. The emerging functions of histone demethylases. Curr Opin Genet Dev 2008; 18( 2): 159–168.
Klose RJ, Kallin EM, Zhang Y . JmjC-domain-containing proteins and histone demethylation. Nat Rev Genet 2006; 7( 9): 715–727.
Shi Y . Histone lysine demethylases: emerging roles in development, physiology and disease. Nat Rev Genet 2007; 8( 11): 829–833.
Sinha KM, Yasuda H, Coombes MM et al. Regulation of the osteoblast-specific transcription factor Osterix by NO66, a Jumonji family histone demethylase. EMBO J 2010; 29( 1): 68–79.
Ye L, Fan Z, Yu B et al. Histone demethylases KDM4B and KDM6B promotes osteogenic differentiation of human MSCs. Cell Stem Cell 2012; 11( 1): 50–61.
Lan F, Bayliss PE, Rinn JL et al. A histone H3 lysine 27 demethylase regulates animal posterior development. Nature 2007; 449( 7163): 689–694.
Akizu N, Estaras C, Guerrero L et al. H3K27me3 regulates BMP activity in developing spinal cord. Development 2010; 137( 17): 2915–2925.
Burgold T, Spreafico F, de Santa F et al. The histone H3 lysine 27-specific demethylase Jmjd3 is required for neural commitment. PloS ONE 2008; 3( 8): e3034.
Estaras C, Akizu N, Garcia A et al. Genome-wide analysis reveals that Smad3 and JMJD3 HDM co-activate the neural developmental program. Development 2012; 139( 15): 2681–2691.
Park BK, Zhang H, Zeng Q et al. NF-κB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat Med 2007; 13( 1): 62–69.
Huang GT, Gronthos S, Shi S . Mesenchymal stem cells derived from dental tissues vs. those from other sources: their biology and role in regenerative medicine. J Dent Res 2009; 88( 9): 792–806.
Vainio S, Karavanova I, Jowett A et al. Identification of BMP-4 as a signal mediating secondary induction between epithelial and mesenchymal tissues during early tooth development. Cell 1993; 75( 1): 45–58.
Nakashima M, Reddi AH . The application of bone morphogenetic proteins to dental tissue engineering. Nat Biotechnol 2003; 21( 9): 1025–1032.
Oh SH, Hwang YC, Yang H et al. SHP is involved in BMP2-induced odontoblast differentiation. J Dent Res 2012; 91( 12): 1124–1129.
De Santa F, Totaro MG, Prosperini E et al. The histone H3 lysine-27 demethylase Jmjd3 links inflammation to inhibition of polycomb-mediated gene silencing. Cell 2007; 130( 6): 1083–1094.
Noel D, Caton D, Roche S et al. Cell specific differences between human adipose-derived and mesenchymal-stromal cells despite similar differentiation potentials. Exp Cell Res 2008; 314( 7): 1575–1584.
Peng L, Dong G, Xu P et al. Expression of Wnt5a in tooth germs and the related signal transduction analysis. Arch Oral Biol 2010; 55( 2): 108–114.
Alge DL, Zhou D, Adams LL et al. Donor-matched comparison of dental pulp stem cells and bone marrow-derived mesenchymal stem cells in a rat model. J Tissue Eng Regen Med 2010; 4( 1): 73–81.
Six N, Lasfargues JJ, Goldberg M . Differential repair responses in the coronal and radicular areas of the exposed rat molar pulp induced by recombinant human bone morphogenetic protein 7 (osteogenic protein 1). Arch Oral Biol 2002; 47( 3): 177–187.
Yamashiro T, Tummers M, Thesleff I . Expression of bone morphogenetic proteins and Msx genes during root formation. J Dent Res 2003; 82( 3): 172–176.
Robinson GW, Mahon KA . Differential and overlapping expression domains of Dlx-2 and Dlx-3 suggest distinct roles for Distal-less homeobox genes in craniofacial development. Mech Dev 1994; 48( 3): 199–215.
Gordon CT, Brinas IM, Rodda FA et al. Role of Dlx genes in craniofacial morphogenesis: Dlx2 influences skeletal patterning by inducing ectomesenchymal aggregation in ovo. Evol Dev 2010; 12( 5): 459–473.
Lezot F, Thomas B, Hotton D et al. Biomineralization, life-time of odontogenic cells and differential expression of the two homeobox genes MSX-1 and DLX-2 in transgenic mice. J Bone Miner Res 2000; 15( 3): 430–441.
Peng L, Jia Z, Yin X et al. Comparative analysis of mesenchymal stem cells from bone marrow, cartilage, and adipose tissue. Stem Cells Dev 2008; 17( 4): 761–773.
McCollum M, Sharpe PT . Evolution and development of teeth. J Anat 2001; 199( Pt 1/2): 153–159.
Thomas BL, Tucker AS, Qui M et al. Role of Dlx-1 and Dlx-2 genes in patterning of the murine dentition. Development 1997; 124( 23): 4811–4818.
Priam F, Ronco V, Locker M et al. New cellular models for tracking the odontoblast phenotype. Arch Oral Biol 2005; 50( 2): 271–277.
Hassan MQ, Javed A, Morasso MI et al. Dlx3 transcriptional regulation of osteoblast differentiation: temporal recruitment of Msx2, Dlx3, and Dlx5 homeodomain proteins to chromatin of the osteocalcin gene. Mol Cell Biol 2004; 24( 20): 9248–9261.
Hassan MQ, Tare RS, Lee SH et al. BMP2 commitment to the osteogenic lineage involves activation of Runx2 by DLX3 and a homeodomain transcriptional network. J Biol Chem 2006; 281( 52): 40515–40526.
Sen GL, Webster DE, Barragan DI et al. Control of differentiation in a self-renewing mammalian tissue by the histone demethylase JMJD3. Genes Dev 2008; 22( 14): 1865–1870.
Jiang W, Wang J, Zhang Y . Histone H3K27me3 demethylases KDM6A and KDM6B modulate definitive endoderm differentiation from human ESCs by regulating WNT signaling pathway. Cell Res 2013; 23( 1): 122–130.
Kartikasari AE, Zhou JX, Kanji MS et al. The histone demethylase Jmjd3 sequentially associates with the transcription factors Tbx3 and Eomes to drive endoderm differentiation. EMBO J 2013; 32( 10): 1393–1408.
Miller SA, Mohn SE, Weinmann AS . Jmjd3 and UTX play a demethylase-independent role in chromatin remodeling to regulate T-box family member-dependent gene expression. Mol Cell 2010; 40( 4): 594–605.
Tang Y, Wu X, Lei W et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat Med 2009; 15( 7): 757–765.
Medici D, Shore EM, Lounev VY et al. Conversion of vascular endothelial cells into multipotent stem-like cells. Nat Med 2010; 16( 12): 1400–1406.
Kronenberg HM . Gs signaling in osteoblasts and hematopoietic stem cells. Ann NY Acad Sci 2010; 1192: 327–329.
Huebsch N, Arany PR, Mao AS et al. Harnessing traction-mediated manipulation of the cell/matrix interface to control stem-cell fate. Nat Mater 2010; 9( 6): 518–526.
Yen AH, Sharpe PT . Regeneration of teeth using stem cell-based tissue engineering. Expert Opin Biol Ther 2006; 6( 1): 9–16.
Acknowledgements
This study was supported by the National Institute of Dental and Craniofacial Research grants DE019412 and DE016513 (to Cun-Yu Wang). Publication of this manuscript is supported by Open Fund of State Key Laboratory of Oral Diseases, Sichuan University.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Xu, J., Yu, B., Hong, C. et al. KDM6B epigenetically regulates odontogenic differentiation of dental mesenchymal stem cells. Int J Oral Sci 5, 200–205 (2013). https://doi.org/10.1038/ijos.2013.77
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijos.2013.77
Keywords
This article is cited by
-
MicroRNA-93-5p regulates odontogenic differentiation and dentin formation via KDM6B
Journal of Translational Medicine (2024)
-
The ERα/KDM6B regulatory axis modulates osteogenic differentiation in human mesenchymal stem cells
Bone Research (2022)
-
DNA Methylation and Histone Modification in Dental-derived Mesenchymal Stem Cells
Stem Cell Reviews and Reports (2022)
-
JMJD3: a critical epigenetic regulator in stem cell fate
Cell Communication and Signaling (2021)
-
Exosomal microRNA-22-3p alleviates cerebral ischemic injury by modulating KDM6B/BMP2/BMF axis
Stem Cell Research & Therapy (2021)