Abstract
Abnormal autonomic nervous regulation has an important role in the development of hypertension. As to whether blood pressure (BP) or BP variability represents the proper characteristics for predisposition to hypertension in Chinese young adults remains controversial. We studied the properties of the indices extracted from beat-to-beat BP during a 13 min cold pressor test (CPT). In this study, 69 Chinese young adults including 34 offspring of hypertensive parents (OHPs; 25.6±2.5 years) and 35 offspring of normotensive parents (ONPs; 25.3±2.3 years) were analyzed. We assessed the differences between the two groups regarding mean beat-to-beat BP and variability indices. Beat-to-beat BP variability indices included time-domain indices and frequency-domain indices. Our results showed that the differences in beat-to-beat systolic BP and mean BP levels between the OHPs and the ONPs were statistically significant (P<0.05). Furthermore, more BP variability indices in the frequency domain were significantly different between the two groups. We concluded that BP variability was superior to BP as an index to evaluate the cardiovascular and sympathetic reactivity to the CPT. Moreover, compared with time-domain BP variability, we found more differences in frequency-domain BP variability between the two groups, thus indicating that frequency-domain BP variability may be a potential index of predisposition to hypertension.
Similar content being viewed by others
Introduction
The occurrence of essential hypertension is the result of genetic and metabolic disorders as well as the influence of many unhealthy lifestyle factors, which are closely related to the occurrence of cardiovascular events.1, 2 The offspring of hypertensive parents (OHPs) are more susceptible to hypertension than the offspring of normotensive parents (ONPs).3 Therefore, many studies have compared different parameters of blood pressure (BP) between the OHPs and the ONPs to identify the potential cardiovascular characteristics that are predispositions to the development of hypertension.3, 4, 5, 6, 7, 8, 9, 10, 11.
Abnormal autonomic nervous regulation has an important role in the development of hypertension.12, 13 Sympathetic nerve activity is a potential factor that predicts the occurrence of essential hypertension during mental arithmetic, independent of blood pressure.14 Lambert et al.15 found that burst amplitude increased in mean arterial pressure and muscle sympathetic nerve activity (MSNA) during arousal by observing ambulatory blood pressure monitoring. These results indicated that the morning surge in BP was associated with sympathetic reactivity.16 Some studies reported that BP was higher in healthy OHPs than in ONPs,3, 7, 8, 9, 10, 11 whereas others showed that the difference was without statistical significance.4, 6 Part of the contradiction may be explained by the fact that the conventional brachial BP used in previous studies was captured at a specified time point and that this sparse measurement may not be able to reflect the real-time dynamics of BP. Currently, compared with clinical and 24 h ambulatory BP measurement, beat-to-beat BP collected by a continuous monitoring technique can capture natural BP variability, and the significance of the beat-to-beat BP has increased in clinical practice.16, 17, 18, 19, 20, 21, 22 For example, Greaney et al.23 hypothesized that young women with family histories of hypertension have more exaggerated BP and sympathetic reactivity than young women without family histories of hypertension during acute sympathoexcitatory experiments. In their study, beat-to-beat BP measurement was used, and only the change of BP was evaluated, whereas BP variability was not mentioned. Particularly, beat-to-beat BP can provide the spectral analysis of BP variability, and these novel BP variability indices can assess autonomic cardiovascular modulation. Moreover, these indices may imply the mechanisms that increase central sympathetic drive. Therefore, beat-to-beat BP shows the potential for evaluating sympathetic reactivity in the early hypertension stage. However, to the best of our knowledge, most of the previous studies suggested that BP hyper-reactivity during the cold pressor test (CPT) was a predictor of hypertension. However, studies of BP variability, especially BP variability, in the frequency domain in this area are rare.
In our present study, we analyze beat-to-beat BP variability based on the known conclusion that OHPs have a higher risk of developing hypertension in later life compared with ONPs. The objective of our study was to compare the cardiovascular reactivity and BP variation of these two groups during cold stimulation. The main objective of our study is to collect beat-to-beat BP data during the CPT,24, 25 a standard stress test for evaluating cardiac autonomic function. In our present study, we examine the beat-to-beat BP/heart rate (HR) level and BP variability/heart rate variability (HRV) both in the time domain and the frequency domain. We aim to determine whether the BP variability/HRV in the frequency domain, which reflects sympathetic activity, can be a potential indicator for the development of hypertension as its early stage.
Methods
Study population
The experiment received ethical approval from the Shenzhen Institutes of Advanced Technology Institutional Review Board. After a preliminary artificial selection of hypertension history, 90 Chinese young adults with no known histories of hypertension were included in this experiment. The number of OHPs reached nearly fifty percent. Finally, we excluded 21 subjects from the study during the CPT. There are several reasons for rejection, including (i) some subjects with critical hypertension (135 mm Hg< systolic BP <160 mm Hg or 90 mm Hg <diastolic BP <95 mm Hg); (ii) some subjects who had motion artifacts during the CPT; (iii) some subjects who terminated the measurement because of personal reasons. The criteria for defining the motion artifact is removal of the hand from the cold water more than three times or for more than 15 s. Hence, a total of 69 qualified subjects were used for the statistical analysis. Thirty-four subjects were OHPs in the test group, and 35 subjects were ONPs in the control group. In the test group, at least one parent (father, mother or both) was determined to have high BP (systolic BP >140 mm Hg or diastolic BP >90 mm Hg). In the control group, both parents had normal BP (90 mm Hg< systolic BP <140 mm Hg and 60 mm Hg< diastolic BP <90 mm Hg). All subjects were required to refrain from influencing their BP with exercise, alcohol, medicine or coffee during the 24 h period before conducting the experiment. A consent form was obtained from each subject. Information regarding demographics, family history of hypertension and use of medicine were first collected from each subject using a questionnaire. We note that all the qualified subjects were nonsmokers. Two subjects in the younger OHP group and one subject in the younger ONP group frequently drank alcohol. Four subjects in the OHP group and one subject in the ONP group frequently drank coffee. No subject took medications to control their BP. Twenty-one subjects from the OHP group and 21 subjects from the ONP group regularly exercised. Therefore, subject-related confounding factors were similar between the two groups.
Conventional measurements at resting state
The experiment was conducted in an air-conditioned room in which the temperature was kept at 20 °C. Conventional measurements, including HR, BP, pulse pressure, pulse wave velocity and ankle-brachial blood pressure index were measured by an Omron Atherosclerosis Detector VP-1000 (BP-203RPEII, Omron Colin, Tokyo, Japan).26 Each subject was asked to quietly lie on a bed in the supine position for 5 min.
Beat-to-beat measurements during the CPT
Beat-to-beat recordings of systolic BP (in mm Hg), diastolic BP (in mm Hg), mean BP (in mm Hg) and HR (in b.p.m.) were measured using a Finometer system Model-2(Midi, Finapres Medical Systems, Amsterdam, the Netherlands) during the CPT.27 A proper cuff was selected for each subject’s arm and was placed on the left upper arm close to the elbow during beat-to-beat recordings. ECG signals were also collected by this instrument. Three ECG electrodes were placed on the right leg, the left leg and the right arm. A washbasin containing ice bags and water was used for generating cold stimulation, and a thermometer monitored the temperature of the water during the experiment. The temperature of the ice water was kept between 2 and 6 °C. The whole procedure was divided into three phases as follows:
Phase 1 (baseline): the subject was asked to remain lying on the bed quietly in the supine position for 5 min.
Phase 2 (cold stimulus): the subject was asked to immerse the left hand into a mixture of ice and water to the wrist level for 3 min.
Phase 3 (post-baseline): after taking the hand out of the water, the subject was asked to remain lying on the bed quietly in the supine position again for 5 min.
Beat-to-beat systolic BP, diastolic BP and R-R interval (RRI) series (i.e., systolic BP-t, diastolic BP-t and RRI-t) were used for systolic BP variability, diastolic BP variability and HRV analysis, respectively. RRI was defined as the time interval between two successive R peaks of the ECG signal. Beat-to-beat BP and HR were assessed by mean level and variability indices that were quantified in both the time domain and the frequency domain. The BP variability indices in the time domain included s.d., the coefficient of variation (CV), average real variability (ARV), and successive variation (SuV).16, 18, 28 The HRV indices in the time domain included the s.d. of the RRIs (SDNN), the coefficient of variation of RRIs (CVrr), and the square root of the mean squared differences of successive RRIs (rMSSD).29 Then, the power spectrum distributions of beat-to-beat systolic BP-t and RRI-t series were analyzed for calculating the frequency-domain systolic BP variability and HRV indices. Data series were first interpolated using the cubic spline to arrive at a unified sampling rate of 4 Hz. The DC component was removed by subtracting the mean value of the series. Finally, the spectrum of the series was estimated using the Fast Fourier Transform with a window length of 256. Subsequently, the frequency-domain systolic BP variability and HRV indices were classified as very low-frequency power (VLF=0.003–0.04 Hz), low-frequency power (LF=0.04–0.15 Hz) and high-frequency power (HF=0.15–0.4 Hz),29 with VLF in normalized units (VLFn), LF in normalized units (LFn), HF in normalized units (HFn) and LF/HF ratios of the BP variability and HRV spectra.
Statistical analysis
Data analysis was performed using SPSS version 13.0 statistical software (SPSS, Chicago, IL, USA). The heterogeneity between two subgroups was assessed by the two-sample t-test and chi-square test, among which, the two-sample t-test was used to examine quantitative data, while the chi-square test was used for the analysis of qualitative data. A P-value <0.05 was statistically significant.
Results
Properties of conventional measurements at the resting state
BP variability (evaluated by s.d., CV, ARV and SuV) and HRV (evaluated by SDNN, CVrr and rMSSD) were calculated (the definitions and equations are shown in Supplementary Table 1). Supplementary Table 2 shows the baseline clinical characteristics of the subjects. The average age was 25.6±2.5 years in the OHP group, and 25.3±2.3 years in the ONP group. The age differences between the two groups were not statistically significant. OHPs had higher systolic and diastolic BP than the ONPs. However, the differences were not statistically significant (P=0.428 and P=0.423, respectively). In contrast, the HR in the OHP group was significantly higher than in the ONP group (P=0.014). Otherwise, no significant difference was found in the other characteristics.
Properties of beat-to-beat measurements during the CPT
Mean level properties
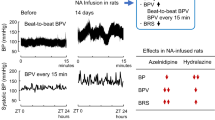
Figure 1 shows the mean level change of each beat-to-beat measurement during every minute of the CPT for both OHPs and ONPs. Squares and circles show the mean values of the BP/HR, respectively. The error bar shows the s.d. of the data set. Systolic BP, diastolic BP, mean BP and HR all increased during the cold stimulus phase and gradually returned to the baseline values during the post-baseline phase. The values reached their maximums during the second minute of the cold stimulus phase. The OHP group showed significantly higher systolic BP, mean BP and HR than the ONP group (P<0.05) during some periods of the CPT test. Only systolic BP, mean BP and HR showed significant differences between the two groups. These differences were marked in bold and with an asterisk * in the figure. Because the subjects were kept in the same state during the entire initial baseline phase, each parameter changed during the cold stimulus phase (7th minute) and gradually returned to the initial baseline during the post-baseline phase (Figure 1). Table 1 presents the detailed values of the mean level of each beat-to-beat measurement in these representative time periods for both OHPs and ONPs. The HR between the OHPs and the ONPs showed statistical significance during the baseline phase (P=0.008) and the post-baseline phase (P=0.024) of the CPT. Values were 68.0±8.3 vs. 62.5±8.5 (P=0.008) and 67.0±7.6 vs. 62.5±8.8 (P=0.024), respectively. In addition, the OHP group showed higher mean BP levels (i.e., systolic BP, diastolic BP and mean BP) during all CPT phases than the ONP group (Table 1). However, the differences had no statistical significance. Table 2 reveals the reactivity and recovery properties of OHPs and ONPs during CPT. Reactivity was calculated by the mean value in the 7th minute minus the mean value during the 1st–5th minute. Recovery was calculated by the mean value in the 13th minute minus the mean value during the 1st–5th minute. As shown in the table, although OHPs had a greater BP reactivity, this difference showed no statistical significance. In contrast, the BP parameters including systolic BP, diastolic BP and mean BP during recovery showed significant differences between the OHP and ONP groups (P<0.05).
Mean levels and s.d. of beat-to-beat measurements during every minute of the cold pressure test, stratified by parental history of hypertension, OHP vs. ONP. Squares and circles show the mean values, and the error bar shows the s.d. of the data set. Baseline (1–5th minute), Cold stimulus (6–8th minute), Post-baseline (9–13th minute); significance of the estimates, *P<0.05; +P<0.01. OHP, offspring with hypertensive parents; ONP, offspring with normotensive parents.
Variability properties
Figure 2 shows the time-domain beat-to-beat BP variability during every minute of the whole CPT for both OHPs and ONPs. In general, all characteristics significantly changed between the 6th minute and the 9th minute in response to the cold stimulus. However, all indices of systolic BP variability showed no statistical significance between OHPs and the ONPs during the cold stimulus phase. Differences in the CV, ARV and SuV of diastolic BP were significant between the OHPs and ONPs during the 11th minute during the post-baseline phase, while ARV, SuV of diastolic BP and HRV indices, including SDNN and rMSSD, also showed significant differences between the two groups during the 13th minute in the post-baseline phase. They were marked in bold and with an asterisk * in the figure. Table 3 displays the detailed values of the time-domain BP variability and HRV indices during these representative time periods. Although most of the BP variability indices increased during the cold stimulus phase, the significant difference between the two groups only showed in the post-baseline phase. The ARV and SuV of diastolic BP showed significantly (P<0.05) lower values in the OHP group than in the ONP group in the post-baseline phase. Furthermore, the SDNN and rMSSD also showed significantly (P<0.05) lower values in the OHP group than in the ONP group. Table 4 shows the detailed values of the frequency domain BP variability and HRV indices of the OHP and ONP groups during each phase of the CPT. The significant differences are shown in bold. In the baseline phase, the LF of systolic BP between the two groups showed a significant difference (P<0.05). In addition, LF, normalized LF, normalized HF and LHR of diastolic BP variability were also significantly different between the two groups. Regarding HRV indices, only the VLF of HRV was significantly different between OHPs and ONPs (P<0.05). In the cold stimulus phase, the VLF of systolic BP in OHPs was significantly higher than in ONPs (P<0.05). Notably, no indices were significantly different between the two groups in this phase. In the post-baseline phase, the LHR of the systolic BP, the normalized LF and the normalized HF of HRV between the two groups were significantly different (P<0.05).
Beat-to-beat BP variability and HRV indices during every minute of the cold pressure test, stratified by parental history of hypertension, OHP vs. ONP. Baseline (1–5th minute), cold stimulus (6–8th minute), post-baseline (9–13th minute); significance of the estimates, *P<0.05. BP variability; HRV, heart rate variability; OHP, offspring with hypertensive parents; ONP, offspring with normotensive parents.
Discussion
In our present study, we tested the hypothesis that the frequency-domain BP variability indices, which reflect autonomic nervous regulation, have a role in the development of later hypertension. The major findings were as follows. First, compared with time-domain BP variability, frequency-domain BP variability may be a better index to predict the predisposition to hypertension. Second, although the OHPs had greater BP reactivity in the CPT, BP variability was superior to BP as an index to evaluate cardiovascular and sympathetic reactivity to the CPT. Third, HRV and BP variability may have different mechanisms in the progression of hypertension.
Many previous studies have shown that essential hypertension is accompanied by sympathetic nerve activation.13, 30, 31 Smith et al.32 estimated sympathetic action using MSNA by comparing the white coat hypertension group with the normotensive group and essential hypertensive group. The study showed that the white coat hypertension group had greater MSNA compared with the normotensive group and that the essential hypertension group still had an exaggerated increase in MSNA. In another study, Greaney et al.23 concluded that systolic BP, diastolic BP, mean arterial pressure, and MSNA were excessively increased in young normotensive women with family histories of hypertension compared with those without family histories of hypertension during CPT, isometric handgrip exercise, and post-exercise ischemia. The results implied that the OHP group had greater cardiovascular reactivity than the ONP group, which indicated that the OHP group had undergone abnormal changes in neural control of the cardiovascular system. However, unlike the complicated experiments performed in the above studies, such as isometric handgrip and post-exercise ischemia, our research only used beat-to-beat BP measurement during the three phases of CPT. Compared with other experiments, CPT is useful as a predictor of future hypertension in a young study population, as claimed by Menkes.33 and Woods.34 The frequency domain of BP variability, which reflects autonomic nervous system regulation, showed significant differences between the two groups. Particularly, some differences of parameters exist at baseline. These results are beyond our expectations. These results indicate that BP variability in the frequency domain may reveal the potential preclinical significance of evaluating the predisposition to later hypertension. Moreover, if the follow-up study can validate these findings, perhaps frequency domain analysis can replace CPT as a predictor of hypertension.
The LF of BP variability and HRV represent both sympathetic and parasympathetic activity, while the HF component is solely an index of parasympathetic activity. Both the LF and HF of the systolic BP variability increased in the cold stimulus phase, indicating that both enhancements of sympathetic and parasympathetic activity are present in the cold stimulus phase. In our present study, the variability of systolic and diastolic BP in the LF between the OHP group and the ONP group in the baseline phase was significantly different, and the variability of diastolic BP in the normalized HF was also significantly different. The results indicate that there is a distinct difference in sympathetic activity between the OHP group and the ONP group. The OHP group had higher levels of the LF and HF of systolic BP than the ONP group in the baseline phase. Duprez et al.35 studied power spectral analysis of BP variability and the change of the R-R-interval between a borderline arterial hypertension group and a normotensive group. The results showed that the LF and HF of the BP were already significantly increased in borderline arterial hypertension at rest.35 Furthermore, systolic BP in the VLF was significantly higher in the OHP group than in the ONP group in the cold stimulus phase. Few studies have reported the physiological mechanism of BP variability in VLF. It may reflect myogenic vascular function, the renin-angiotensin system and endothelium-derived NO.36 As is commonly known, the LHR is a sensitive indicator of sympathovagal balance.37 The LHR of BP variability in OHPs was significantly higher than in ONPs during the base baseline phase of our study. However, OHPs had a lower LHR of BP than ONPs in the post-baseline phase. Some of these differences were statistically significant. According to the autonomic nervous system regulation mechanism, when the human body is subjected to an external stimulus, sympathetic nerve activity has an important role first; subsequently, parasympathetic nerve activity gradually dominates. However, in our study, OHPs had a greater decrease in the LHR of diastolic BP during the cold stimulus phase and a clear increase in the post-baseline phase. This finding shows that the sympathovagal balance changed in the OHP group during the CPT. In conclusion, we speculated that the sympathovagal balance might be different in the OHP group. Accordingly, the lower LHR in the post-baseline phase may increase the risk of future hypertension.
In addition to the BP variability in the frequency domain, BP variability in the time domain has been known to be a prognostic indicator of hypertension and can also predict cardiovascular disease.38, 39 The ARV and SuV of diastolic BP increased in the cold stimulus phase and returned to the baseline level gradually in the post-baseline phase (Figure 2). We also found that the ARV and SuV of diastolic BP were significantly different between the OHPs and ONPs in the post-baseline phase (13th minute; Figure 2, Table 3). The results indicate that these indices of BP variability may have a certain role in predicting later hypertension and that diastolic BP variability is superior to systolic BP variability in this predictive role. In this study, we used four indices to evaluate BP variability. The s.d. and CV are mathematically equal to the total power of spectral analysis, while ARV and SuV estimate high-frequency variations.29 ARV and SuV are two new measures proposed recently that are calculated from the difference between adjacent measurements.40 Different from the traditional indicator of s.d., these new measures represent the short-term fluctuation of BP. Therefore, ARV and SuV can provide a simple way of estimating variation while avoiding the influence of a trend and are thus more suitable for our analysis of BP variability, especially for exploring the potential factors underlying the predisposition to hypertension.
To take this discussion further, the HR and HRV indices in the CPT also deserve to be discussed. First, the difference of the conventional occasional HR (P<0.05, Table 1) and the difference between OHPs and the ONPs in HR calculated from beat-to-beat measurements in the baseline phase and the post-baseline phase (P<0.05, Table 1) were statistically significant. These differences indicate that HR may be an important marker for evaluating sympathetic reactivity in the early stage of hypertension. This conclusion is consistent with Huynh’s study, which discussed resting HR in the correlation between fitness and arterial stiffness, wherein higher cardiorespiratory fitness may reduce arterial stiffness mainly by affecting resting HR.41 We also found that rMSSD and SDNN changed little in the cold stimulus phase, but showed significantly lower values in the OHP group and higher values in the ONP group in the post-baseline phase. We presume that HRV has a certain contribution to the activation of the autonomic nervous system in the early hypertension stage. Wustmann et al.42 studied HRV and HR turbulence using 24 h ECG in a sub-study of the Device-Based Therapy in Hypertension Trial and demonstrated sustained changes in HRV and HR turbulence, which were caused by chronic baroreceptor stimulation. Note that the baroreceptor correlates to the inhibition of sympathetic nerve activity and increased parasympathetic nerve activity.42 Therefore, HR and HRV can evaluate sympathetic reactivity in the early hypertension stage, and they can be the potential cardiovascular characteristics that predispose to the development of hypertension.
Furthermore, the mean level properties should also be discussed in this session. First, the OHPs had higher BP values than the ONPs. However, this difference was without significance. These results are in accordance with two previous studies.4, 6 However, several studies reported differences in BP between the OHP and ONP groups, which were statistically significant.3, 43 These controversial results may depend on the number, age, and race of the subjects used for the analysis. Kaess et al.44 showed that aortic stiffness was associated with hypertension in a longitudinal cohort study. Treiber et al.11 indicated that children with family histories of essential hypertension showed increases in systemic vascular resistance and systolic and diastolic BP and decreases in HR in response to a cold stressor. These findings demonstrated our assumption that OHPs had more risk and likelihood of developing hypertension in later life.
Although we found that beat-to-beat BP variability, especially frequency domain BP variability, may have a certain role in increasing the risk for future hypertension in Chinese young adults, the present study still had some limitations. First, it was a cross-sectional comparative study. Therefore, we could not conclude the cause-and-effect characteristics to predict later hypertension. These potential factors that increase the likelihood of future hypertension need to be verified in our follow-up study. Second, further analysis is required to study the influence of age and gender in greater detail. Finally, this was only a single center study, and the sample size was relatively small in comparison with other well-established existing studies.
Conclusions
In summary, to find the potential characteristics that increase the likelihood of hypertension, we analyzed the properties of beat-to-beat BP of OHPs compared with ONPs during a CPT, a standard stress test for evaluating cardiac autonomic function. Changes in beat-to-beat BP have existed during the early lives of Chinese young adults with hypertensive parents. Moreover, beat-to-beat BP level and variability, especially frequency domain BP variability, can potentially predict hypertension at an early stage. Hypertension is a chronic disease caused by long-term cumulative damage due to various factors. Evaluating the predisposition to develop hypertension in later life can help prevent hypertension and provide an early warning for treatment before major clinical events occur. Current knowledge of the mechanisms of beat-to-beat BP is limited. More studies are needed to improve the understanding of the potential mechanisms and their potential prognostic implications. If our findings can be verified in prospective studies with hypertension outcomes, a method using beat-to-beat BP variability as a risk factor to identify the early occurrence of hypertension may be provided as the most promising indicator.
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J . Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365: 217–223.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ . Global and regional burden of disease and risk factors 2001 systematic analysis of population health data. Lancet 2006; 36: 1747–1757.
Kucerova J, Filipovsky J, Staessen JA, Cwynar M, Wojciechowska W, Stolarz K, Kuznetsova T, Gasowski E, Dolesjova M, Grodzicki T, Kawecka-Jaszcz K, Fagard R . Arterial characteristics in normotensive offspring of parents with or without a history of hypertension. Am J Hypertens 2006; 19: 264–269.
Albarwani S, Jaju DS, Al-Yahyaee S, Bayoumi RA, Alvaranga JCL, Commuzie AG, Hassan MO . Cardiovascular reactivity to mental and physical stress in offspring of hypertensive parents from large Omani Arab families. FASEB J 2011; 25: 1099–1094.
Farah K, Keshav G, Pawan S . Autonomic reactivity to cold pressor test in prehypertensive and hypertensive medical students. Indian J Physiol Pharmacol 2011; 55: 246–252.
Garg S, Kumar A, Singh K . Blood pressure response to cold pressor test in the children of hypertensives. Online J Health Allied Sci 2010; 9: 1–3.
Maver J, Strucl M, Accetto R . Autonomic nervous system activity in normotensive subjects with a family history of hypertension. Clin Auton Res 2004; 14: 369–375.
Maver J, Strucl M, Accetto R . Autonomic nervous system and microvascular alterations in normotensives with a family history of hypertension. Blood Press 2004; 13: 95–100.
Othman AS, Othman NI, Rosman A, Nudin SSH, Rahman ARA . Central and peripheral blood pressure profile of young offspring with hypertensive and normotensive parents. J Hypertens 2012; 30: 1552–1555.
Schneider GM, Jacobs DW, Gevirtz RN, O’Connor DT . Cardiovascular haemodynamic response to repeated mental stress in normotensive subjects at genetic risk of hypertension evidence of enhanced reactivity blunted adaptation and delayed recovery. J Hum Hypertens 2003; 17: 829–840.
Treiber FA, Mccaffrey F, Musante L, Rhodes T, Davis H, Strong WB, Levy M . Ethnicity family history of hypertension and patterns of hemodynamic reactivity in boys. Psychosom Med 1993; 55: 70–77.
Grassi G . Role of the sympathetic nervous system in human hypertension. J Hypertens 1998; 16: 1979–1987.
Mancia G, Grassi G . The autonomic nervous system and hypertension. Circ Res 2014; 114: 1804–1814.
Flaa A, Eide IK, Kjeldsen SE, Rostrup M . Sympathoadrenal stress reactivity is a predictor of future blood pressure an 18-year follow-up study. Hypertension 2008; 52: 336–341.
Lambert EA, Chatzivlastou K, Schlaich M, Lambert G, Head GA . Morning surge in blood pressure is associated with reactivity of the sympathetic nervous system. Am J Hypertens 2014; 27: 783–792.
Parati G, Ochoa JE, Lombardi C, Bilo G . Assessment and management of blood-pressure variability. Nat Rev Cardiol 2013; 10: 143–155.
Dawson SL, Manktelow BN, Robinson TG, Panerai RB, Potter JF . Which parameters of beat-to-beat blood pressure and variability best predict early outcome after acute ischemic stroke? Stroke 2000; 31: 463–468.
Dolan E, O’Brien E . Blood pressure variability clarity for clinical practice. Hypertension 2010; 56: 179–181.
Wei FF, Li Y, Zhang L, Xu TY, Ding FH, Wang JG, Staessen JA . Beat-to-beat reading-to-reading and day-to-day blood pressure variability in relation to organ damage in untreated Chinese. Hypertension 2014; 63: 790–796.
Asayama K, Wei FF, Liu YP, Hara A, Gu YM, Schutte R, Li Y, Thijs L, Staessen JA . Does blood pressure variability contribute to risk stratification? Methodological issues and a review of outcome studies based on home blood pressure. Hypertens Res 2015; 38: 97–101.
Yildirim A, Kosger P, Ozdemir G, Sahin FM, Ucar B, Kilic Z . Carotid intima-media thickness and elastic properties of aortas in normotensive children of hypertensive parents. Hypertens Res 2015; 38: 621–626.
Madden JM, O’Flynn AM, Fitzgerald AP, Kearney PM . Correlation between short-term blood pressure variability and left-ventricular mass index: a meta-analysis. Hypertens Res 2016; 39: 171–177.
Greaney JL, Matthews EL, Wenner MM . Sympathetic reactivity in young women with a family history of hypertension. Am J Physiol Heart Circ Physiol 2015; 308: H816–H822.
Silverthorn DU, Michael J . Cold stress and the cold pressor test. Adv Physiol Educ 2013; 37: 93–96.
Wirch JL, Wolfe LA, Weissgerber TL, Davies GA . Cold pressor test protocol to evaluate cardiac autonomic function. Appl Physiol Nutr Metab 2006; 31: 235–243.
Meyer ML, Tanaka H, Gouskova N, Aguilar D, Agarwal SK, Heiss G . Differential distributions of carotid-femoral and brachial-ankle pulse wave velocity with age and race: the ARIC study. Circulation 2013; 127: AP382.
Maestri R, Pinna GD, Robbi E, Capomolla S, La Rovere MT . Noninvasive measurement of blood pressure variability accuracy of the Finometer monitor and comparison with the Finapres device. Physiol Meas 2005; 26: 1125–1136.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlof B, Sever PS, Poulter NR . Prognostic significance of visit-to-visit variability maximum systolic blood pressure and episodic hypertension. Lancet 2010; 375: 895–905.
Camm AJ, Malik M, Bigger JT, Breithardt G, Cerutti S, Cohen RJ, Coumel P, Fallen EL, Kennedy HL, Kleiger RE, Lombardi F, Malliani A, Moss AJ, Rottman JN, Schmidt G, Schwartz PJ, Singer D . Heart rate variability standards of measurement physiological interpretation and clinical use. Circulation 1996; 93: 1043–1065.
Carthy ER . Autonomic dysfunction in essential hypertension: a systematic review. Ann Med Surg 2014; 3: 2–7.
Esler M . The sympathetic nervous system in hypertension back to the future? Curr Hypertens Rep 2015; 17: 1–7.
Smith PA, Graham LN, Mackintosh AF, Stoker JB, Mary DA . Sympathetic neural mechanisms in white-coat hypertension. J Am Coll Cardiol 2002; 40: 126–132.
Menkes MS, Matthews KA, Krantz DS, Lundberg U, Mead LA, Qaqish B, Liang KY, Thomas CB, Pearson TA . Cardiovascular reactivity to the cold pressor test as a predictor of hypertension. Hypertension 1989; 14: 524–530.
Wood DL, Sheps SG, Elveback LR, Schirger A . Cold pressor test as a predictor of hypertension. Hypertension 1984; 6: 301–306.
Duprez DA, Desutter JH, Debuyzere ML, Rietzschel ER, Rimbaut S, Kaufman JM, Vanhoecke MJ, Clement DL . Renin-angiotensin-aldosterone system RR interval and blood pressure variability during postural changes in borderline arterial hypertension. Am J Hypertens 1995; 8: 683–688.
Höcht C . Blood pressure variability prognostic value and therapeutic implications. Int Sch Res Notices 2013; 2013: 1–16.
Pal GK, Adithan C, Amudharaj D, Dutta TK, Pal P, Nandan PG, Nanda N . Assessment of sympathovagal imbalance by spectral analysis of heart rate variability in prehypertensive and hypertensive patients in Indian population. Clin Exp Hypertens 2011; 33: 478–483.
Eguchi K, Hoshide S, Schwartz JE, Shimada K, Kario K . Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am J Hypertens 2012; 25: 962–968.
Parati G, Ochoa JE, Lombardi C, Bilo G . Blood pressure variability assessment predictive value and potential as a therapeutic target. Curr Hypertens Rep 2015; 17: 537.
Mena LJ, Maestre GE, Hansen TW, Thijs L, Liu YP, Boggia J, Li Y, Kikuya M, Bjorklund-Bodegard K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang JG, O’Brien E, Staessen JA, Pres IDAB . How many measurements are needed to estimate blood pressure variability without loss of prognostic information? Am J Hypertens 2014; 27: 46–55.
Quan HL, Blizzard CL, Sharman JE, Magnussen CG, Dwyer T, Raitakari O, Cheung M, Venn AJ . Resting heart rate and the association of physical fitness with carotid artery stiffness. Am J Hypertens 2014; 27: 65–71.
Wustmann K, Kucera JP, Scheffers I, Mohaupt M, Kroon AA, de Leeuw PW, Schmidli J, Allemann Y, Delacretaz E . Effects of chronic baroreceptor stimulation on the autonomic cardiovascular regulation in patients with drug-resistant arterial hypertension. Hypertension 2009; 54: 530–536.
Jenie IM, Noor NM . Family history of hypertension is associated with exaggerated cardiovascular reactivity to mental but not to physical test. Med J Indones 2010; 19: 118–123.
Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF . Aortic stiffness blood pressure progression and incident hypertension. JAMA 2012; 308: 875–881.
Acknowledgements
We gratefully acknowledge the volunteers who participated in our study. This work was supported in part by the Guangdong Image-guided Therapy Innovation Team (2011S013), the STS Project of the Chinese Academy of Sciences (KFJ-EW-STS-097), Shenzhen Innovation Funding (SGLH20150213143207911, SGLH 20150216172854731, JCYJ20140901003939025, JCYJ20151030151431727) and the National Key Research and Development Program of China (2016YFC1300300).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Wu, D., Xu, L., Abbott, D. et al. Analysis of beat-to-beat blood pressure variability response to the cold pressor test in the offspring of hypertensive and normotensive parents. Hypertens Res 40, 581–589 (2017). https://doi.org/10.1038/hr.2017.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.4
Keywords
This article is cited by
-
Association between mental illness and blood pressure variability: a systematic review
BioMedical Engineering OnLine (2022)
-
Novel blood pressure and pulse pressure estimation based on pulse transit time and stroke volume approximation
BioMedical Engineering OnLine (2018)