Abstract
Hypertensive disorders of pregnancy are known to be a risk factor for future cardiovascular diseases. In contrast, there is a paucity of data on the not so distant future prognosis of hypertensive disorders of pregnancy. In the present study, we evaluated the incidence of the diseases causing cardiovascular problems (hypertension, diabetes mellitus, dyslipidemia and metabolic syndrome) 5 years after delivery in Japanese women with hypertensive disorders of pregnancy. We performed a double-cohort study and compared medical conditions between women with and without a history of hypertensive disorders of pregnancy. A total of 1513 women who participated in the cohort study were invited to undergo a medical checkup 5 years after the index delivery, of whom 829 responded. After excluding pregnant and lactating women at the time of examination, 25 women with hypertensive disorders of pregnancy and 746 control subjects were analyzed. The incidence of hypertension was significantly higher among women with hypertensive disorders of pregnancy than women who were normotensive during pregnancy (24.0 vs. 2.5%, P<0.001). They were also at an increased risk of subsequent hypertension 5 years after the index delivery, after adjusting for confounding factors such as age, body mass index, family history of hypertension and salt intake (odds ratio 7.1, 95% CI, 2.0–25.6, P<0.003). These is no significant difference in the incidence of diabetes mellitus, dyslipidemia and metabolic syndrome. In conclusion, hypertensive disorders of pregnancy are strong risk factors for subsequent hypertension only 5 years after delivery.
Similar content being viewed by others
Introduction
Hypertensive disorders of pregnancy (HDP) occur in 5–10% of all pregnancies.1, 2 Women with a history of pre-eclampsia3, 4, 5, 6 or gestational hypertension5, 7, 8 are at an increased risk of cardiovascular disease (CVD) later in life. Several studies have found that women who have had pregnancies complicated by HDP are at higher risk of developing hypertension,5, 9, 10 type 2 diabetes,11 dyslipidemia,12, 13 elevated body mass index (BMI), and insulin resistance.10, 12, 14, 15, 16 However, little has been reported on the prognosis of these diseases in the near future after delivery in Japanese women. We performed a double-cohort study, consisting of an HDP group and a group of women with normal blood pressure during pregnancy (control group), to assess the incidence of hypertension, type 2 diabetes mellitus, dyslipidemia and metabolic syndrome 5 years after the index delivery. We calculated the odds ratio (OR) for developing hypertension adjusted for age, BMI, salt intake, family history of hypertension.
Materials and methods
Study subjects
This double-cohort study recruited study subjects from the Tokyo Children’s Health, Illness and Development (T-CHILD) study being conducted by the National Center for Child Health and Development (NCCHD) and the Showa University Hospital Mother and Child Health Center (SUH) in Tokyo, Japan, from October 2003 to December 2005. Study subjects consisted of women who received antenatal care at NCCHD or SUH from the first trimester during this time period and delivered singletons. Apart from patients who changed to another hospital, had miscarriages or stillbirths, a total of 75 women with HDP complications were included in the HDP group, while 1466 women with normal deliveries were included in the control group. Based on the exclusion criteria described below, a total of 70 women in the HDP group and 1443 women in the control group were mailed information within 3 months of their child’s fifth birthday about receiving a medical checkup 5 years after delivery. Women who agreed to the medical checkup filled out a questionnaire and underwent a physical examination, blood testing, and urinalysis.
Exclusion criteria
Women who met the following criteria were excluded: chronic hypertension, diabetes mellitus, kidney disease before pregnancy, systolic blood pressure of 140 mm Hg or greater or diastolic blood pressure of 90 mm Hg or greater before 20 weeks of gestation, no documented blood pressure prior to 20 weeks of gestation. We also excluded a participant if we could not confirm that blood pressure was less than 140/90 mm Hg within 12 weeks after the index delivery.
Study participant characteristics
Clinical information on the participants such as birth date, underlying disease, past medical history, family history, obstetric history, as well as information on the course of the index pregnancy and the newborn, was obtained from electric medical records. Information on participants at 5 years after the index delivery such as underlying disease, family history, current smoking habits, and education level, was derived from the questionnaire filled out by participants.
Brief-type self-administered diet history questionnaire
Salt intake was calculated based on self-reported daily dietary data from the brief-type self-administered diet history questionnaire (BDHQ).17, 18
Medical checkup 5 years after the index delivery
At the medical checkup 5 years after the index delivery, the participant’s demographic characteristics were ascertained and urine and fasting blood samples were collected. Height, weight and waist circumference were measured according to guidelines issued by the Ministry of Health, Labour and Welfare of Japan.19 After a brief resting period upon arrival, blood pressure was measured twice with 1 min between measurements using an automated sphygmomanometer (Kentaro ADVANCE BP-203RV III, Colin, Tokyo, Japan).
Clinical criteria
In this study, we defined HDP as pre-eclampsia and gestational hypertension. The diagnosis of pre-eclampsia and gestational hypertension was made retrospectively based on the participant’s medical records. We diagnosed pre-eclampsia and gestational hypertension according to 2015 Best Practice Guide for Care and Treatment of Hypertension in Pregnancy.20 These criteria define pre-eclampsia as hypertension between 20 weeks of gestation to 12 weeks postpartum with proteinuria. Gestational hypertension was defined as hypertension during the same period without proteinuria. Hypertension was defined as systolic blood pressure of 140 mm Hg or greater or a diastolic blood pressure of 90 mm Hg or greater. Proteinuria was defined as 300 mg of urinary protein per 24 h, ≥2+ protein on a voided urine sample, or ⩾1+ protein measured on 2 separate occasions. Because the authors were focused on the HDP group, patients who experienced only labor onset hypertension which is related to the perinatal outcomes21 was not included in this study.
We defined the blood pressure in early pregnancy as the average before 16 weeks gestation. We defined the blood pressure in middle pregnancy as the nearest blood pressure to 20 weeks gestation from 18 to 22 weeks gestation.
Diagnostic criteria at the time of the medical checkup 5 years after the index delivery were as follows. Hypertension was defined as mean systolic blood pressure of 140 mm Hg or higher, mean diastolic blood pressure of 90 mm Hg or higher, or current antihypertensive therapy. Type 2 diabetes mellitus defined as either fasting blood glucose of 126 mgdl−1 or higher, hemoglobin A1c (HbA1c) of 6.5% or higher, or taking medication for diabetes mellitus. In addition, dyslipidemia was defined as high-density lipoprotein cholesterol (HDL-C) of 40 mg dl−1 or lower, triglycerides (TG) of 150 mg dl−1 or higher, or low-density lipoprotein cholesterol (LDL-C) of 140 mgdl−1 or higher while on medication for dyslipidemia. Finally, our definition of metabolic syndrome was based on the revised Japanese standards for abdominal girth in Asians.22, 23 Metabolic syndrome was defined as waist circumference greater than 80 cm with at least 2 of the following: (1) systolic blood pressure of 130 mm Hg or higher or diastolic blood pressure of 85 mm Hg or higher; (2) fasting TG greater than 150 mgdl−1, HDL-C of 40 mgdl−1 or less; and (3) fasting glucose greater than 110 mg dl−1.
Statistical analysis
The Mann–Whitney U-test was used to analyze differences between 2 continuous variables, while the χ2-test or Fisher’s exact test was used for discrete variables. Logistic regression was used to assess the influence of HDP on the development of subsequent hypertension, diabetes mellitus, dyslipidemia, and metabolic syndrome 5 years after delivery, respectively. For each OR, a 95% confidence interval (CI) was calculated. Independent variables used in the model were age at delivery (years), BMI (kg m−2), familial history of hypertension (yes or no), salt intake calculated based on BDHQ data during the medical checkup (g per day), kidney disease (yes or no), low maternal birth weight (yes or no), and maternal preterm birth (yes or no). P<0.05 was considered statistically significant. All analyses were performed with SPSS software, version 18 for Windows (SPSS, Chicago, IL, USA).
Results
Seventy women from the HDP group (NCCHD, 39; SUH, 31) were invited for a medical checkup 5 years after their index delivery, and 27 (NCCHD, 20; SUH, 7) underwent the checkup (38.6%). From the normotensive control group, 1,443 women were invited and 802 underwent the checkup (55.6%).
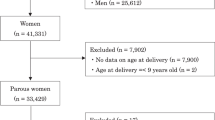
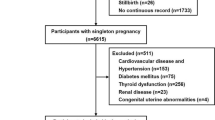
A total of 771 women were analyzed, after excluding 30 who were pregnant, 26 who were breast-feeding at the time of the medical checkup, and 2 who declined blood pressure measurement at the medical checkup. Of the 25 women with HDP, 11 had pre-eclampsia and 14 had gestational hypertension. In the normotensive control group, 746 women were analyzed (Figure 1).
Flow diagram showing sample selection. Seventy women from the HDP group were invited for a medical checkup, and 27 underwent a checkup (follow-up proportion, 38.6%). From the normotensive control group, 1443 women were invited and 802 received a checkup (follow-up proportion, 55.6%). A total of 771 women were analyzed, after excluding 30 who were pregnant and 26 who were breast-feeding at the time of the medical checkup and 2 who declined blood pressure measurement. A total of 25 women from the HDP group and 746 from the normotensive control group were analyzed.
Characteristics of the index pregnancy of the HDP and control groups were compared (Table 1). There were no significant differences in age at delivery, height, pre-pregnancy body weight, and BMI between the groups. Gestational weeks was significantly lower in the HDP group compared to the control group. The proportion of preterm births was significantly higher in the HDP group than in the control group. Mean birth weight was significantly lower in the HDP group than in the control group. The proportion of low birth weight was significantly higher in the HDP group than in the control group. Blood pressure in early and middle pregnancy and 1 month after delivery was significantly higher in HDP group. There was significant difference in the proportion of participants with a history of previous HDP.
Characteristics and current study of the women at the time of the medical checkup are shown in Table 2. There were no significant differences between the HDP and control groups in underlying disease; family history of hypertension, diabetes, or dyslipidemia; proportion of smokers, daily salt intake, and education. Furthermore, there were no significant differences between the groups in terms of body weight, BMI, and waist circumference.
Hypertension
The HDP group had significantly higher blood pressure than the control group (P<0.001) (Table 2). Six women in the HDP group (24.0%) and 19 women (2.5%) in the normotensive control group developed subsequent hypertension (P<0.001) (Table 3). One woman in the HDP group and 7 women in the control group were taking antihypertensive medication.
Diabetes mellitus
There was no significant difference in the glucose metabolism profile between the groups (Table 2). None of the women in the HDP group developed diabetes mellitus, compared to 6 (0.8%) in the normotensive control group. There was no significant difference in the proportion of participants with diabetes mellitus between the groups (Table 3). Five women in the control group were taking antidiabetic medication.
Dyslipidemia
There were no significant differences in the lipid profile between the groups (Table 2). Three women in the HDP group (12.0%) developed dyslipidemia, compared to 106 women (14.2%) in the control group. There was no significant difference in the proportion of participants with dyslipidemia between the groups (Table 3). One woman in the control group was taking medication for dyslipidemia.
Metabolic syndrome
Four women in the control group (0.5%) developed metabolic syndrome. There was no significant difference in the proportion of participants with metabolic syndrome between the groups (Table 3).
Risk for subsequent hypertension 5 years after the index delivery in the HDP group
The crude OR for subsequent hypertension 5 years after the index delivery in the HDP group was 12.1 (95% CI, 4.3–33.7; P<0.001). Multiple logistic regression analysis identified that HDP was associated with a 7.1–12.1-fold increased risk of subsequent hypertension after adjusting for confounding factors such as age, BMI, family history of hypertension, salt intake (Table 4).
There were no significant differences in blood pressure and the proportion of participants with hypertension between the pre-eclampsia group (n=11) and the gestational hypertension group (n=14). The blood pressure of the pre-eclampsia group and the gestational hypertension group was 112.3±10.9/73.0±9.3 mm Hg and 126.0±23.2/81.8±16.1 mm Hg, respectively. Two women in the pre-eclampsia group (18.2%) and 4 women in the gestational hypertension group (28.6%) developed subsequent hypertension. There were no significant differences in BMI, waist circumference and blood profile (HbA1c, glucose, insulin, HOMA-R, LDL-C, HDL-C and TG) between the groups (data not shown).
Discussion
Blood pressure
Our study revealed that the proportion of participants with subsequent hypertension 5 years after the index delivery is significantly higher among women with HDP. Watanabe et.al reported the positive relation between HDP and future hypertension in Japanese women retrospectively. Mean age of their study participants at the medical checkup was 46.5 years old and the diagnosis of HDP is from the Maternal and Child Health Handbook.24 In our study, the average age of the women at the medical checkup was 39.0 years old which was 5 years after the index delivery. This indicates the possibility of elevated blood pressure at an early stage of life after delivery.
Mangos et al.10 reported that women with a history of pre-eclampsia or gestational hypertension have significantly higher ambulatory blood pressure compared with women who have had normotensive pregnancies, although the period between the index pregnancy and blood pressure measurement ranges from 2 to 12 years. Moreover, BMI, which might affect blood pressure, was significantly higher in the HDP group. Hermes et al.25 reported that women with HDP during pregnancy had significantly higher blood pressure compared to women with normotensive pregnancies 2.5 years after the index pregnancy. The prevalence of hypertension was significantly higher in the HDP group, and BMI was higher in the same group as well. In studies from other countries, women with HDP tend to have subsequent hypertension and obesity. The average BMI of the women in our study was 20.1 kg m−2 before pregnancy and 20.6 kg m−2 at the 5 years after medical checkup. This study population was not affected by obesity but was prone to hypertension, which is a unique finding. In addition, we adjusted for salt intake. There is a positive correlation between sodium intake and blood pressure26 and Katsuya et al.reported that the Japanese have high salt sensitivity genetically.27 We added salt intake as a confounding factor and confirmed that higher blood pressure in the HDP group was not dependent on salt intake.
Parikh NI et.al reported that pre-eclampsia was independently associated with higher systolic and diastolic blood pressure levels at 40 years of age.28 Hypertension is a leading risk factor for CVD among women.29 HDP is recognized as a major risk factor for CVD in the guidelines for the prevention of CVD in women by the American Heart Association,30 but specific long-term postpartum management remains unclear.31 Pregnancy and childbirth represent an excellent chance to identify women who are at high risk of future hypertension and cardiovascular disease. As a next step, constructing appropriate follow-up systems after delivery for women with a history of HDP may be necessary.
Glucose metabolism and insulin resistance
Callaway et al.11 reported that HDP is associated with diabetes mellitus 21 years after delivery. However, BMI before pregnancy and 21 years after delivery attenuates this association. In their study, 33 women had hypertension before pregnancy or before 20 weeks of gestation. As such, the HDP group may already have higher BMI, insulin resistance, and blood pressure before pregnancy than the control group. Girouard et al.12 reported that women with previous HDP show signs of insulin resistance based on HOMA-R 7.8 years after delivery. However, women who developed HDP had significantly higher BMI at the beginning of the index pregnancy than control subjects, which might be associated with high insulin resistance in HDP. No significant difference in BMI at 5 years after the index delivery was observed between the HDP group and the normotensive control group. There was also no significant difference in the proportion of patients who developed diabetes mellitus or insulin resistance based on HOMA-R.
Lipid metabolism
Some researchers have reported a high prevalence of dyslipidemia after pregnancy among women with HDP.12, 13 On the other hand, there have been reports of no significant differences in the prevalence of dyslipidemia after pregnancy between women with HDP and women who were normotensive during pregnancy.4, 10, 14, 16 Our study did not find such a difference.
Metabolic syndrome
Women who develop HDP have been reported to have a high prevalence of metabolic syndrome.32 However, our study found no increase in the prevalence of metabolic syndrome among women with HDP.
Study limitations
The case group had a higher percentage of patients lost to follow-up. However, as there were no significant differences between those who participated in medical checkups and those who did not in terms of mean age at delivery, proportion of nulliparous women, mean duration of gestation and mean birth weight, our findings may be representative of the HDP group.
References
Hutcheon JA, Lisonkova S, Joseph KS . Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 2011; 25: 391–403.
Umesawa M, Kobashi G . Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res 2017; 40: 213–220.
McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ . Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J 2008; 156: 918–930.
Sattar N, Ramsay J, Crawford L, Cheyne H, Greer IA . Classic and novel risk factor parameters in women with a history of preeclampsia. Hypertension 2003; 42: 39–42.
Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, Hannaford P, Smith WC . Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. BMJ 2003; 326: 845–851.
Bellamy L, Casas JP, Hingorani AD, Williams DJ . Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007; 335: 974–985.
Arnadottir GA, Geirsson RT, Arngrimsson R, Jonsdottir LS, Olafsson O . Cardiovascular death in women who had hypertension in pregnancy: a case-control study. BJOG 2005; 112: 286–292.
Wikstrom AK, Haglund B, Olovsson M, Lindeberg SN . The risk of maternal ischaemic heart disease after gestational hypertensive disease. Bjog 2005; 112: 1486–1491.
Spaanderman ME, Ekhart TH, van Eyck J, Cheriex EC, de Leeuw PW, Peeters LL . Latent hemodynamic abnormalities in symptom-free women with a history of preeclampsia. Am J Obstet Gynecol 2000; 182: 101–107.
Mangos GJ, Spaan JJ, Pirabhahar S, Brown MA . Markers of cardiovascular disease risk after hypertension in pregnancy. J Hypertens 2012; 30: 351–358.
Callaway LK, Lawlor DA, O'Callaghan M, Williams GM, Najman JM, McIntyre HD . Diabetes mellitus in the 21 years after a pregnancy that was complicated by hypertension: findings from a prospective cohort study. Am J Obstet Gynecol 2007; 197: 492.e491–497.
Girouard J, Giguere Y, Moutquin JM, Forest JC . Previous hypertensive disease of pregnancy is associated with alterations of markers of insulin resistance. Hypertension 2007; 49: 1056–1062.
Magnussen EB, Vatten LJ, Smith GD, Romundstad PR . Hypertensive disorders in pregnancy and subsequently measured cardiovascular risk factors. Obstet Gynecol 2009; 114: 961–970.
Laivuori H, Tikkanen MJ, Ylikorkala O . Hyperinsulinemia 17 years after preeclamptic first pregnancy. J Clin Endocrinol Metab 1996; 81: 2908–2911.
Wolf M, Hubel CA, Lam C, Sampson M, Ecker JL, Ness RB, Rajakumar A, Daftary A, Shakir AS, Seely EW, Roberts JM, Sukhatme VP, Karumanchi SA, Thadhani R . Preeclampsia and future cardiovascular disease: potential role of altered angiogenesis and insulin resistance. J Clin Endocrinol Metab 2004; 89: 6239–6243.
Spaan JJ, Houben AJ, Musella A, Ekhart T, Spaanderman ME, Peeters LL . Insulin resistance relates to microvascular reactivity 23 years after preeclampsia. Microvasc Res 2010; 80: 417–421.
Kobayashi S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C . Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr 2011; 14: 1200–1211.
Kobayashi S, Honda S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C . Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol 2012; 22: 151–159.
The Ministry of Health, Labour and Welfare of Japan Statement on Special Medical Checkup. Medical Economics Division, Health Insurance Bureau, Ministry of Health, Labour and Welfare; 1 April 2008. http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/seikatsu/dl/hoken-program2.pdf. Accessed on 4 April 2016.
Takagi K, Yamasaki M, Nakamoto O, Saito S, Suzuki H, Seki H, Takeda S, Ohno Y, Sugimura M, Suzuki Y, Watanabe K, Matsubara K, Makino S, Metoki H, Yamamoto T . A Review of Best Practice Guide 2015 for care and treatment of hypertension in pregnancy. Hypertens Res Pregnancy 2015; 3: 65–103.
Ohno Y, Terauchi M, Tamakoshi K, Shiozaki A, Saito S . The risk factors for labor onset hypertension. Hypertens Res 2016; 39: 260–265.
Alberti KG, Zimmet P, Shaw J . Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 2006; 23: 469–480.
Doi Y, Ninomiya T, Hata J, Yonemoto K, Arima H, Kubo M, Tanizaki Y, Iwase M, Iida M, Kiyohara Y . Proposed criteria for metabolic syndrome in Japanese based on prospective evidence: the Hisayama study. Stroke 2009; 40: 1187–1194.
Watanabe K, Kimura C, Iwasaki A, Mori T, Matsushita H, Shinohara K, Wakatsuki A, Gosho M, Miyano I . Pregnancy-induced hypertension is associated with an increase in the prevalence of cardiovascular disease risk factors in Japanese women. Menopause 2015; 22: 656–659.
Hermes W, Tamsma JT, Grootendorst DC, Franx A, van der Post J, van Pampus MG, Bloemenkamp KW, Porath M, Mol BW, de Groot CJ . Cardiovascular risk estimation in women with a history of hypertensive pregnancy disorders at term: a longitudinal follow-up study. BMC Pregnancy Childbirth 2013; 13: 126.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24hour urinary sodium and potassium excretion. BMJ 1988; 297: 319–328.
Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T . Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res 2003; 26: 521–525.
Parikh NI, Norberg M, Ingelsson E, Cnattingius S, Vasan RS, Domellöf M, Jansson JH, Edstedt Bonamy AK . Association of Pregnancy Complications and Characteristics With Future Risk of Elevated Blood Pressure: The Vasterbotten Intervention Program. Hypertension 2017; 69: 475–483.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB . Heart Disease and Stroke Statistics-2016 Update: A report from the American Heart Association. Circulation 2016; 133: e38–360.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Piña IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D'Armiento J, Kris-Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK . Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. J Am Coll Cardiol 2011; 57: 1404–1423.
Spaan J, Peeters L, Spaanderman M, Brown M . Cardiovascular risk management after a hypertensive disorder of pregnancy. Hypertension 2012; 60: 1368–1373.
Giguere Y, Charland M, Thériault S, Bujold E, Laroche M, Rousseau F, Lafond J, Forest JC . Linking preeclampsia and cardiovascular disease later in life. Clin Chem Lab Med 2012; 50: 985–993.
Acknowledgements
We thank Shie Saito and Chiharu Matsuzawa for cohort data management. We also thank Dr Julian Tang of the Department of Education for Clinical Research, National Center for Child Health and Development, for proofreading, editing and rewriting parts of this manuscript. This work was supported in part by a Health and Labour Sciences Research Grant from the Ministry of Health, Labour and Welfare of Japan (No 09158522). This study was also supported by a grant from the National Center for Child Health and Development of Japan (20A-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mito, A., Arata, N., Qiu, D. et al. Hypertensive disorders of pregnancy: a strong risk factor for subsequent hypertension 5 years after delivery. Hypertens Res 41, 141–146 (2018). https://doi.org/10.1038/hr.2017.100
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.100
Keywords
This article is cited by
-
Postpartum and interpregnancy care of women with a history of hypertensive disorders of pregnancy
Hypertension Research (2024)
-
The joint effect of gestational diabetes mellitus and hypertension contribute to higher risk of diabetes mellitus after delivery: a nationwide population-based study
BMC Pregnancy and Childbirth (2023)
-
Protocol for an interventional study to reduce postpartum weight retention in obese mothers using the internet of things and a mobile application: a randomized controlled trial (SpringMom)
BMC Pregnancy and Childbirth (2021)
-
Gestational lipid profile as an early marker of metabolic syndrome in later life: a population-based prospective cohort study
BMC Medicine (2020)
-
Hypertensive disorders of pregnancy, obesity, and hypertension in later life by age group: a cross-sectional analysis
Hypertension Research (2020)