Abstract
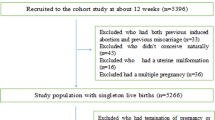
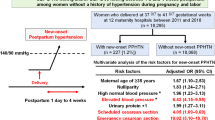
Hypertensive disorders of pregnancy (HDP) comprise a group of hypertension-related diseases and represent the most common medical disorders in pregnancy. The aim of this study was to investigate the risks of adverse pregnancy outcomes in patients with different types of HDP, including gestational hypertension, chronic hypertension, preeclampsia (PE, early or late onset), PE superimposed on chronic hypertension (superimposed PE), eclampsia, and HELLP syndrome. Data from a multicenter retrospective patient cohort in China were analyzed. Seventeen adverse maternal or perinatal outcomes were evaluated. Logistic regression was used to estimate the risk of adverse outcomes for each HDP subgroups, using the gestational hypertension group as the reference. The final analysis included 2368 patients with HDP. Of these, 39.9% of patients reported at least one adverse pregnancy outcome. Patients with early onset PE had the highest risk for having both adverse maternal and perinatal outcomes (OR = 7.28, 95% CI: 2.68, 19.79). The risk of perinatal death significantly increased in HELLP syndrome, superimposed PE, and early onset PE, (OR = 13.81, 6.32, and 4.84, respectively, p < 0.05) groups. This study highlights that among patients with HDP, those with early onset PE had the highest risk for having both adverse maternal and perinatal outcomes, and patients with HELLP syndrome had the highest risk for perinatal death.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet 2010;376:631–44.
Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet. 2011;25:391–403.
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res. 2017;40:213–20.
Brown MA, Lindheimer MD, de Swiet M, Assche AV, Moutquin J-M. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20:ix-xiv.
Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHP. Hypertens Pregnancy. 2014;4:97–104.
Lisonkova S, Joseph KS. Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol. 2013;209:544.e1–12.
Tuuli MG, Rampersad R, Stamilio D, Macones G, Odibo AO. Perinatal outcomes in women with preeclampsia and superimposed preeclampsia: do they differ? Am J Obstet Gynecol. 2011;204:e1–7.
Harmon AC, Cornelius DC, Amaral LM, Faulkner JL, Cunningham MW Jr., Wallace K, et al. The role of inflammation in the pathology of preeclampsia. Clin Sci. 2016;130:409–19.
Phipps E, Prasanna D, Brima W, Jim B. Preeclampsia: updates in pathogenesis, definitions, and guidelines. Clin J Am Soc Nephrol. 2016;11:1102–13.
Burton GJ, Redman CW, Roberts JM, Moffett A. Pre-eclampsia: pathophysiology and clinical implications. BMJ. 2019;366:l2381.
von Dadelszen P, Magee LA, Roberts JM. Subclassification of preeclampsia. Hypertens Pregnancy. 2003;22:143–8.
Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS. Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol. 2014;124:771–81.
Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai BM. The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens. 2013;3:44–7.
Yildirim G, Gungorduk K, Aslan H, Gul A, Bayraktar M, Ceylan Y. Comparison of perinatal and maternal outcomes of severe preeclampsia, eclampsia, and HELLP syndrome. J Turk Ger Gynecol Assoc. 2011;12:90–6.
Rahmayanti S, Nurdiati DS. HELLP syndrome in severe preeclampsia: the perinatal outcomes. Pregnancy Hypertens. 2017;7:61.
Group of Obstetrics and Gynecology Chinese Medical Association. Guidelines for the diagnosis and treatment of hypertensive disorder complicating pregnancy (2015). Chin J Obstet Gynecol. 2015;10:721–8. [in Chinese]
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on hypertension in pregnancy. Obstet Gynecol. 2013;122:1122–31.
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014;36:416–41.
Redman CW. Early and late onset preeclampsia: Two sides of the same coin. Pregnancy Hypertens. 2017;7:58. (Abstract)
Abildgaard U, Heimdal K. Pathogenesis of the syndrome of hemolysis, elevated liver enzymes, and low platelet count (HELLP): a review. Eur J Obstet Gynecol Reprod Biol. 2013;166:117–23.
John K, Wielgosz S, Schulze-Osthoff K, Bantel H, Hass R. Increased plasma levels of CK-18 as potential cell death biomarker in patients with HELLP syndrome. Cell Death Dis. 2013;4:e886.
Purwosunu Y, Sekizawa A, Okazaki S, Farina A, Wibowo N, Nakamura M, et al. Prediction of preeclampsia by analysis of cell-free messenger RNA in maternal plasma. Am J Obstet Gynecol. 2009;200:386.e1–7.
Ankumah NE, Sibai BM. Chronic hypertension in pregnancy: diagnosis, management, and outcomes. Clin Obstet Gynecol. 2017;60:206–14.
Ankumah NA, Cantu J, Jauk V, Biggio J, Hauth J, Andrews W, et al. Risk of adverse pregnancy outcomes in women with mild chronic hypertension before 20 weeks of gestation. Obstet Gynecol 2014;123:966–72.
von Dadelszen P, Ornstein MP, Bull SB, Logan AG, Koren G, Magee LA. Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis. Lancet. 2000;355:87–92.
Orbach H, Matok I, Gorodischer R, Sheiner E, Daniel S, Wiznitzer A, et al. Hypertension and antihypertensive drugs in pregnancy and perinatal outcomes. Am J Obstet Gynecol. 2013;208:301.e1–6.
Villar J, Carroli G, Wojdyla D, Abalos E, Giordano D, Ba’aqeel H, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194:921–31.
Tooher J, Thornton C, Makris A, Ogle R, Korda A, Hennessy A. All hypertensive disorders of pregnancy increase the risk of future cardiovascular disease. Hypertension. 2017;70:798–803.
Barton JR, O’Brien JM, Bergauer NK, Jacques DL, Sibai BM. Mild gestational hypertension remote from term: progression and outcome. Am J Obstet Gynecol. 2001;184:979–83.
Magee LA, von Dadelszen P, Chan S, Gafni A, Gruslin A, Helewa M, et al. The control of hypertension in pregnancy study pilot trial. BJOG. 2007;114:e13–20.
Silva LM, Coolman M, Steegers EA, Jaddoe VW, Moll HA, Hofman A, et al. Low socioeconomic status is a risk factor for preeclampsia: the Generation R Study. J Hypertens. 2008;26:1200–8.
Sibai B, Ewell M, Levine R, Klebanoff M, Esterlitz J, Catalano P, et al. Risk factors associated with preeclampsia in healthy nulliparous women. Am J Obstet Gynecol. 1997;177:1003–10.
Shen M, Smith GN, Rodger M, White RR, Walker MC, Wen SW. Comparison of risk factors and outcomes of gestational hypertension and pre-eclampsia. PLoS ONE. 2017;12:e0175914.
Cruz MO, Gao W, Hibbard JU. Obstetrical and perinatal outcomes among women with gestational hypertension, mild preeclampsia, and mild chronic hypertension. Am J Obstet Gynecol. 2011;205:260.e1–9.
Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, et al. Pregnancy outcomes in healthy nulliparas who developed hypertension. Calcium for Preeclampsia Prevention Study Group. Obstet Gynecol. 2000;95:24–8.
Funding
This work was supported by the National Key Research and Development Program of China (2016YFC1000206); the Science & Technology Project of Hunan Province (2017SK2151 and 2017SK1033); the National Science and Technology Pillar Program of China During the Twelfth Five-Year Plan Period (2014BAI 05B05); and the China Postdoctoral Science Foundation (2018M633000).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was reviewed and approved by the Medical Ethics Committee of the Xiangya Hospital, Center South University (reference number: 20170527). The requirement for written informed consent was waived by the Ethics Committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Zhang, W., Lin, J. et al. Hypertensive disorders of pregnancy and risks of adverse pregnancy outcomes: a retrospective cohort study of 2368 patients. J Hum Hypertens 35, 65–73 (2021). https://doi.org/10.1038/s41371-020-0312-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0312-x